Abstract
The primary objective was to study agreement between X-rays and point of care ultrasound (POC-US) in determining central venous line (CVL) tip position. The secondary objective was to examine malposition rates over time using POC-US. Fifty-six neonates were enrolled who had a CVL placed. Initial X-rays and POC-US were obtained. POC-US was performed daily thereafter for the total of 6 days. US video clips were acquired in four standard echocardiographic views: subcostal, four-chamber, and short- and long-axis parasternal views. Gwet’s agreement coefficient (AC1) for agreement measured inter-rater reliability of X-rays and POC-US (correct position/malposition). A generalized linear mixed model for binary clustered data estimated malposition rate over time. All analyses were conducted using SAS version 9.4 and Agree Stat. The study included 108 “pairs” of X-rays and POC-US images. Agreement coefficient (AC1), with respect to correct position/malposition of CVL tip, was high AC1 = 0.872 (UVC-AC1 = 0.814, PICC-AC1 = 0.94). Among birth weight (BW) < 1000 g, 1000–1499 g, and BW > 1500 g, AC1 values were 0.922, 0.774, and 0.873, respectively. CVL tip malposition rate decreased over time.
Conclusions: Agreement between POC-US and X-rays for CVL tip position was high, with the highest in BW < 1000 g. The data suggest that POC-US can be used for initial confirmation and follow up of CVL tip position.
What is Known • X-ray is currently the gold standard for localizing central venous line (CVL) tip position. • Malposition of CVL tip can lead to life-threatening complications. | |
What is New • POC-US is superior to X-ray as it can follow CVL tip position over time, detecting malpositioned lines, adjusting them in a timely manner thus preventing complications. • Standardizing CVL placement, X-ray acquisition, POC-US acquisition with four views with video clips and ultrasound operator training increases accuracy and thus agreement between X-ray and POC-US. • UVC tip is more likely to be malpositoned than PICC tip. Malposition of UVC tip using POC-US decreased over time due to shrinking of the umbilical cord in the first 48 of life. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Central venous lines (CVL) including umbilical venous catheter (UVC) and peripherally inserted central catheters (PICC) are routinely used in the neonatal intensive care unit (NICU) for administration of fluid and medications. Each UVC is inserted blindly and advanced based on the shoulder-umbilicus length graph or a weight-based equation (Shukla’s formula) [6, 23]. Alternatively, PICC is advanced to a length based on the external anatomic measurements. X-ray is the standard method used for evaluation of the CVL tip position. CVL tip at the cavoatrial junction (CAJ) is considered as the optimal target position.
X-rays identify location of the UVC tip in relation to bony vertebral column, liver shadow, and cardiac silhouette. Studies that included more than 100 neonates have examined concordance between X-ray and ultrasound (US) in examining the exact UVC tip position [1, 7]. They found ultrasound (US) to be more accurate with relatively low concordance between the two. Similarly, rays that locate PICC tip in the inferior vena cava (IVC) or superior vena cava (SVC) but not in the heart are considered adequate. Several recent studies examining PICC tip location, performed in more than 350 neonates, found concordance between X-ray and US to be 59–80% [12, 17, 20, 24]. In these studies, 5–25% of PICC tips were in the heart even though they looked to be appropriately positioned on the X-rays. Correspondingly, comparable data have been found in adult studies that examined PICC tip position with X-rays and US [11, 25]. Hence, the use of X-ray analysis may be misleading, and the use of US in determination of the CVL tip position has been recommended [1, 7, 12, 17, 20, 24]. A recent study in neonates found that point of care ultrasound (POC-US) used in PICC placement is associated with fewer catheter manipulations, fewer X-rays needed, and decreased time required for the catheter insertion [14]. In the adult population, POC-US use has been well studied and established in the protocols that guide CVL insertion, confirm CVL tip position, and detect complications in a timely manner [10, 15, 16].
In neonates, appropriate CVL tip position is very important. Malposition may lead to life-threatening complications including pleural effusion, liver hematoma, and injury. Intra-atrial positioning of either UVC or PICC is associated with increased occurrence of arrhythmia, thrombosis, pericardial effusion, cardiac tamponade, and death [4, 9, 13, 21].
Study aims
In this study, our primary aim was to examine agreement between X-rays and POC-US for checking CVL tip position (correct position/malposition), with a secondary aim to examine malposition rates by POC-US during the first 6 days of CVL placement.
Study methods
Patients and setting
We conducted a prospective observational study on 56 infants who needed central venous line (UVC or PICC). They were admitted to the level III NICUs at two academic medical centers, Cohen’s Children Medical Center and Northshore University Hospital (Northwell Health). The study was approved by the Institutional Review Board of the Northwell Health System as a quality improvement study; therefore, informed consent was not needed. Study patients were recruited between December 2015 and December 2016. Neonates with congenital anomalies were not included in the study. All central lines were placed by neonatal fellows and neonatal nurse practitioners. The length of the central venous line insertion was determined by Shukla’s formula for UVC and by external anatomical measurement for PICCs as directed by our unit protocol. Umbilical venous catheters were sutured to the umbilical stump and secured by taping with a NeoBridge®. On the other hand, PICCs were properly secured by Tegaderm™ and Steri-strip™. Central line insertion was performed under standard sterile precautions.
The goal for the optimal UVC tip placement is at the junction of the IVC and the right atrium (RA). The upper extremity PICC tip was placed ideally in the SVC at the CAJ. Similarly, the lower extremity PICC tip was placed in the IVC at the junction of the IVC and the RA. Verification of the catheter placement was performed with chest or chest and abdomen X-rays with limbs in the standard resting semi-flexed position. For the upper extremity PICC, the shoulder was minimally abducted and elbows flexed. Having upper extremity in this particular position assures the deepest possible position of the PICC tip regardless of whether the central line was placed in the basilic or cephalic vein [19]. For the lower extremity, PICC hips were slightly abducted and knees flexed 45°. Two views anteroposterior (AP) and lateral were obtained. Catheters with malpositioned tips were adjusted to the appropriate position.
Catheters were removed either after completion of intravenous therapy or if patient developed complications. After initial X-ray verification of the line placement, further X-ray images were obtained only as clinically indicated. The decision to remove UVC was mandatory after 7 days post-insertion, or earlier at the discretion of the attending neonatologist. In addition, PICCs were removed when the patient reached 100 cc/kg/day in enteral feeds and no intravenous medication was needed.
POC-US and X-ray protocol for CVL tip position
All infants enrolled in the study had CVL tip position examined by a neonatologist who had formal training in POC-US. Training included attending two workshops given by physician experts in ultrasound. Proper performance of 40 point of care ultrasounds under expert supervision was required before the start of the study.
On the day of insertion (day 0), CVL tip position was examined in the same limb position as soon as X-ray was completed. All CVLs were followed with POC-US exams daily to confirm their satisfactory position. A 10-Hz curved phased array neonatal US probe was used (Zonare, Z.One Pro Ultrasound System, Mindray, China). Ultrasound gel was warmed before every examination. A pacifier was offered to the babies with mature suck reflex. To confirm the position of the CVL tip, each neonate had a 10-s video clip recorded for each of the following views: sagittal subcostal view of the IVC and right atrium (RA), parasternal short-axis view of the RA at the aortic level, parasternal long-axis view of the RA inflow, and apical four-chamber view. The video clips were obtained to assure the correct line tip identification as some babies had US “noise” coming from the lungs.
During POC-US scanning, if an ultrasound operator located a malpositioned line tip, the NICU team was notified. The decision to correct the line position based on the POC-US findings, or following further X-ray image analysis, was made by the attending physician. Every effort was made to scan the babies in the standard resting position identical to the position that the X-rays were taken. Official radiology department X-ray reports of the line tip position were recorded in our data sheet. A radiologist and pediatric critical care physician (ECHO-certified) independently reviewed ultrasound scans. They were blinded to the readings obtained by the US operator. The results of the POC-US scans were correlated with X-ray images.
Statistical methods
Gwet’s agreement coefficient (AC1) coefficient for agreement was used to measure inter-rater reliability of X-ray and POC-US in checking CVL position (correct position/malposition). Subjects were followed for 6 days during their NICU stay. For the purpose of examining agreement, only days when both measures (X-ray and POC-US) were available were included in the statistical analysis (referred to as an X-ray/POC-US “pair”).
A generalized linear mixed model (GLMM) for binary clustered (i.e., hierarchical) data was used to estimate malposition rate during the first 6 days of catheter life, along with their corresponding 95% confidence intervals (CIs). All analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC) and Agree Stat (Advanced Analytics, LLC 2015. Agree Stat Software for Windows, Version 2015.1. Gaithersburg, MD: Advanced Analytics, LLC.).
Results
There were 56 subjects with POC-US and X-ray performed. An aggregate of 108 X-rays and 306 POC-US were obtained. A total of 108 X-ray/POC-US “pairs” were included for the agreement analysis.
Among the studied population, there were 34 UVCs (60.71%) and 22 PICCs (39.29%). The mean birth weight (BW) was 1900 ± 1200 g. The distribution was as follows: 12 neonates with BW ranged between 500 and 999 g (23.12%), 12 neonates with BW 1000–1499 g (21.43%), and 31 neonates with BW > 1500 g (55.36%).
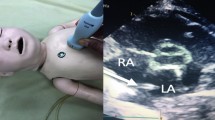
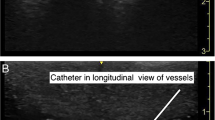
As described above, ultrasound operators saved the images as 10-s video clips of each of the four scanned views. Video clips of one patient are demonstrated (online resource 1–4) All CVL tips were visualized. Figure 1 shows examples of different UVC tip ultrasound views. Figure 2 shows examples of different PICC tip ultrasound views. Availability of POC-US has a huge advantage regarding the time needed to complete all four views taking 4 min on average (range 2–10 min). On the contrary, the time frame from ordering the X-ray to its execution ranged between 10 and 45 min.
Examples of different UVC tip ultrasound views. a Subcostal sagittal view of the heart. UVC tip at the junction of IVC and the right atrium (red arrow) (correct position). b Short-axis parasternal view of the heart. UVC tip in the left atrium (red arrow) (malposition). c Subcostal sagittal view of the heart. UVC tip in ductus venosus (red arrow) (malposition). d Four chamber view of the heart. UVC tip in the right atrium (red arrow). (malposition). e Four chamber view of the heart. UVC tip in the right atrium touching atrial septum (red arrow) (malposition). f Short-axis parasternal view of the heart. UVC line tip at junction of IVC and RA (red arrow) (correct position). RA right atrium, TV tricuspid valve, RV right ventricle, RVOT right ventricular outflow tract, PV pulmonary valve, PA pulmonary artery, LA left atrium, AV aortic valve, MV mitral valve, LV left ventricle, AS atrial septum. VS ventricular septum, SVC superior vena cava, IVC inferior vena cava, PFO Patent foramen ovale
Examples of different PICC tip ultrasound views. a Long-axis parasternal right inflow view of the heart. Lower extremity PICC tip in the right atrium (red arrow) (malposition). b High parasternal view of SVC and subclavian vein. PICC tip in the subclavian vein (red arrow) (malposition). c Subcostal sagittal view of IVC. PICC tip in IVC (red arrow) (correct position). RA right atrium, TV tricuspid valve, RV right ventricle. SVC superior vena cava, IVC inferior vena cava
(MP4 5784 kb)
(MP4 6162 kb)
(MP4 6207 kb)
(MP4 5605 kb)
The agreement between POC-US and X-ray with respect to position of the CVL tip was high (AC1 = 0.872). Thirty three UVCs were assessed with 65 POC-US and X-rays “pairs.” This represents about 60% of the total CVLs evaluated in this study. The agreement coefficient for UVCs was 0.814. Twenty-three PICCs were evaluated with 43 POC-US and X-rays “pairs.” This represents about 40% of the total CVL assessed. The agreement coefficient for PICCs was 0.940 (Table 1). In our opinion, the agreement between POC-US and X-ray was higher in PICCs than UVCs due to the fact that PICCs may have less migration.
Based on BW, in neonates with BW ranging between 500 and 999 g, the agreement coefficient between POC-US and X-ray was 0.922; in neonates with BW of 1000–1499 g, the agreement coefficient between POC-US and X-ray was 0.774; and for those infants with BW > 1500 g, the agreement coefficient was 0.873. The agreement coefficient between POC-US and X-ray was the highest among the lowest BW infants (< 1000 g) (Table 2).
Our results showed that the malposition rate of UVCs as examined by POC-US decreased over time (p < 0.0287). Malposition rate of UVCs was 30% on day 0 of catheter life. In the first 48 h of the UVC life, the rates were around 20% and then decreased over time reaching 10% on day 5 (Fig. 3a). On the contrary, malposition rates of PICCs were consistently low over time (Fig. 3b).
Central venous line malposition rates. a UVC tip malposition rate. The graph displays UVC tip malposition rate and corresponding 95% confidence intervals from day 0 to day 5 of the catheter life. The x-axis displays the days of UVC life and y-axis displays the percentage of malpositioned lines. p = 0.0287 using a generalized linear mixed model (GLMM) for binary clustered data. b PICC tip malposition rate. The graph displays PICC tip malposition rate and corresponding 95% confidence intervals from day 0 to day 5 of the catheter life. The x-axis displays the days of PICC life and y-axis displays the percentage of malposition lines. p = 0.1052 using a generalized linear mixed model (GLMM) for binary clustered data
Discussion
To the best of our knowledge, this is the first prospective study that assesses the agreement between X-rays (AP and lateral view) and POC-US (4-views) in localizing CVL tip (both UVC and PICC) over time. Moreover, we describe UVC migration by using serial POC-US exams over the course of the first six catheter days. We examined both types of CVLs, AP, and cross-table lateral X-ray views, as well as the recording of POC-US video clips in four standard views, which altogether increase the accuracy of CVL tip localization.
This is also the first study using POC-US in comparing the identification of the tip of UVC and PICC lines as they are both made of different material and have different diameters. PICC lines are more difficult to identify due to their smaller diameter (1F–1.9F vs 3.5F–5F for UVC) and occasional position in SVC or subclavian vein needing a high parasternal view to identify the tip. PICC lines are less likely to be malpositioned than UVC. PICC tip has a wider anatomic range within the SVC or IVC for it to be deemed well positioned while UVC tip is often displaced deeper in the RA (malpositioned) due to the shrinking of the umbilical cord stump as Wharton’s jelly dries up.
Neonates have good acoustic windows for examination of the RA and large portion of SVC and IVC. Therefore, the relation of CVL tip to the CAJ can be accurately assessed. Therefore, malpositioning could be suspected if the tip is not visualized at the CAJ. As previously described, verification of the CVL tip location by ultrasound requires significantly less time [14, 22]. This is relevant in urgent CVL placements and in unstable patients in whom rapid and safe catheter use is necessary. The use of POC-US has significant impact in decreasing the number of X-rays needed [14]. Exposure to ionizing radiation is well known for its short- and long-term sequelae [22]. In a recent survey of PICC practices in level III NICUs in the USA, 80% routinely obtained additional films after any repositioning of the catheter.
We had strict criteria for optimal UVC tip position. Malposition was defined by having the UVC tip either “inside the liver” or above the CAJ rather than the tip projecting outside the range of T8–10 vertebral body space. We also had strict criteria for PICC tip positioning at CAJ. In addition, every effort was made to have the limbs in a consistent position for both X-ray and POC-US exams. Both AP and cross table lateral X-ray views were done. We believe that these details and ultrasound scanning strategy of using four standard ECHO views together with recording and analyzing sweeping video clips improve the accuracy of the CVL tip localization. Moreover, no adverse effects from POC-US examinations were noted in the studied neonates.
Verification of CVL tip position is essential to prevent catheter-related complications. Radiography is still considered as the gold standard exam used for this purpose. Our study demonstrates good agreement between POC-US and X-ray in identifying malpositioned CVL tips. The agreement coefficient between POC-US and X-ray was highest among the lowest BW infants (Table 2). We believe this is the result of the better penetrance of both US and X-ray in smaller neonates. Our results are in agreement with Alonso-Quintela et al. who analyzed 51 CVLs and found that X-ray and ultrasound results agreed 94% of the time in determining intra-atrial and extra-atrial locations and 92% of the time in diagnosing CVL malposition defined by CVL tip being out of the vena cava [2]. On the other hand, few studies have found lower agreement between X-rays and ultrasound. Ades et al. examined 53 UVCs and found that the sensitivity and specificity of chest X-ray in evaluating inappropriate UVC position were 32% and 89%, respectively. They concluded that the chest X-ray is inaccurate in confirming UVC tip position [1]. Similarly, another study that examined 109 PICCs found that echocardiography used to confirm PICC tip location, after it was confirmed as appropriate with X-ray, identified 25% of these PICC tips to actually be in the heart [24]. Michel et al. found that for CVL tip position localization, sensitivity and specificity were 93.3 and 95.6% for US and 66.7 and 63.0% for X-ray confirming the superiority of US over X-ray [18].
We have shown that UVC tip malposition rate decreases over time (Fig. 3a). This can be explained by the fact that the umbilical cord stump shrinks due to the drying of the Wharton’s jelly, until it reaches its final length. As the stump shrinks, UVC moves inward towards the heart with the tip often found deep in the RA. Shrinking of the umbilical stump causes most UVC tips to be malpositioned in the first 48 h even though they were initially in the correct position. Nevertheless, with time, the rate of UVC tip malposition decreases. Therefore, we recommend that POC-US should be regularly obtained for the first 2–3 days after UVC placement and the catheter tip adjusted accordingly if migrated past CAJ. There is no need for further X-rays if POC-US is available in NICU. Correspondingly, POC-US is helpful in ongoing surveillance of the CVL tip position in infants with long-term PICCs as they can be malpositioned as infants grow and have a higher likelihood of complications like thrombosis. In addition, with different arm positioning, PICCs placed in upper extremity can move substantially towards the heart (up to 1.5 cm with shoulder adduction and elbow flexion). Similarly, PICCs made of different materials (silicone vs. polyurethane) may move in different fashion [5]. These facts are very important as PICC tips deep in the RA can erode through myocardium into pericardial space causing catastrophic pericardial effusion.
Our data support previously published literature that highlights safety, efficiency, and superiority of POC-US. We question the use of X-ray as the gold standard for CVL tip location assessment. Our POC-US study operators had extensive formal training, which adds strength to our study. Also, we acquired 10-s video clips of each of the four views. The clips are superior to static images, as “sweeping” clips eliminate the false localization of catheter tip and reverberation artifacts that may occasionally occur with static images. Video clips were further reviewed by ECHO-certified physician blinded to the US operator’s read. In addition, a different radiologist who was on clinical service at the time reads X-rays. All our video clips were acquired almost immediately after X-ray was done which decreases the chance CVL inadvertently moved.
Our study is limited by its moderate sample size. We had 108 pairs of POC-US and X-rays. This fact makes it difficult to analyze UVC and PICC tip positions separately in different BW categories. Even though POC-US was done daily for the first 6 days of the CVL life, X-rays were ordered only when deemed necessary by the clinical team. Catheter tips “within the liver,” outside of IVC or SVC may pose diagnostic challenges to an inexperienced POC-US examiner [3, 18]. Hyper-inflated lungs, pneumothorax, and gaseous abdomens may obscure CVL tip position localization [17]. Finally, one of the barriers to the widespread use of ultrasound is the highly operator-dependent nature of this technology. As with other technical skills, appropriate training and credentialing is essential.
Conclusions
We found that POC-US has a good agreement with X-rays for the detection of malpositioned CVL tip. Ultrasound appears to be a superior method to X-rays for routine verification of the CVL tip position in neonates. Further, it can be used to monitor UVC tip migration over time, especially in the first 48 h post-line insertion. Therefore, POC-US has the potential to decrease the need for daily or repetitive X-rays. Finally, POC-US can aid in avoiding complications resulting from the CVL tip malposition in a timely manner.
Abbreviations
- AC1:
-
Agreement coefficient
- AP:
-
Anteroposterior
- BW:
-
Birth weight
- CAJ:
-
Cavoatrial junction
- CVL:
-
Central venous line
- CIs:
-
Confidence intervals
- GLMM:
-
Generalized linear mixed model
- IVC:
-
Inferior vena cava
- LA:
-
Left atrium
- NICU:
-
Neonatal intensive care unit
- PICC:
-
Peripherally inserted central catheter
- POC-US:
-
Point of care ultrasound
- RA:
-
Right atrium
- SVC:
-
Superior vena cava
- US:
-
Ultrasound
- UVC:
-
Umbilical venous catheter
References
Ades A, Sable C, Cummings S, Cross R, Markle B, Martin G (2003) Echocardiographic evaluation of umbilical venous catheter placement. J Perinatol 23:24–28
Alonso-Quintela P, Oulego-Erroz I, Rodiguez-Blanco S, Muñiz-Fontan M, Lapeña-López-de Armentia S, Rodriguez-Nuñez A (2015) Location of the central venous catheter tip with bedside ultrasound in young children: can we eliminate the need for chest radiography? Pediatr Crit Care Med 16(9):e340–e345. https://doi.org/10.1097/PCC.0000000000000491
Brissaud O, Harper L, Lamireau D, Jouvencel P, Fayon M (2010) Sonography- guided positioning of intravenous long lines in neonates. Eur J Radiol 74(3):e18–e21. https://doi.org/10.1016/j.ejrad.2009.03.017
Collier PE, Goodman GB (1995) Cardiac tamponade caused by central venous catheter perforation of the heart: a preventable complication. J Am Coll Surg 181:459–463
Connolly B, Amaral J, Walsh S, Temple M, Chait P, Stephens D (2006) Influence of arm movement on central tip location of peripherally inserted central catheters (PICCs). Pediatr Radiol 36(8):845–850
Dunn PM (1966) Localization of the umbilical catheter by post-mortem measurement. Arch Dis Child 4:69–75
George L, Waldman JD, Cohen ML, Segall ML, Kirkpatrick SE, Turner SW, Pappelbaum SJ (1982) Umbilical vascular catheters: localization by two-dimensional echocardio/aortography. Pediatr Cardiol 2:237–243
Gnannt R, Connolly BL, Parra DA, Amaral J, Moineddin R, Thakor AS (2016) Variables decreasing tip movement of peripherally inserted central catheters in pediatric patients. Pediatr Radiol 46(11):1532–1538. https://doi.org/10.1007/s00247-016-3648-1. Epub 2016 Jun 7
Green C, Yohannan MD (1998) Umbilical arterial and venous catheters: placement, use, and complications. Neonatal Netw 17(6):23–28
Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C (2003) Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 16:327–361
Hsu JH, Wang CK, Chu KS, Cheng KI, Chuang HY, Jaw TS, Wu JR (2006) Comparison of radiographic landmarks and the echocardiographic SVC/RA junction in the positioning of long-term central venous catheters. Acta Anaesthesiol Scand 50:731–735
Jain A, McNamara PJ, Ng E, El-Khuffash A (2012) The use of targeted neonatal echocardiography to confirm placement of peripherally inserted central catheters in neonates. Am J Perinatol 29:101–106. https://doi.org/10.1055/s-0031-1295649
Jain A, Deshpande P, Shah P (2013) Peripherally inserted central catheter tip position and risk of associated complications in neonates. J Perinatol 33(4):307–312. https://doi.org/10.1038/jp.2012.112
Katheria AC, Fleming SE, Kim JH (2013) A randomized controlled trial of ultrasound-guided peripherally inserted central catheters compared with standard radiograph in neonates. J Perinatol 33(10):791–794. https://doi.org/10.1038/jp.2013.58
Matsushima K, Frankel HL (2011) Detection of central venous catheter insertion-related complication using bedside ultrasound: the CVC sono. J Trauma 70:1561–1563. https://doi.org/10.1097/TA.0b013e3182128546
Maury E, Guglielminotti J, Alzieu M, Guidet B, Offenstadt G (2001) Ultrasonic examination: an alternative to chest radiography after central venous catheter insertion? Am J Respir Crit Care Med 164:403–405
McGee WT, Mailloux PT, Martin RT (2011) Safe placement of central venous catheters: a measured approach. J Intensive Care Med 26:392–396. https://doi.org/10.1177/0885066610392895
Michel F, Brévaut-Malaty V, Pasquali R, Thomachot L, Vialet R, Hassid S, Nicaise C, Martin C, Panuel M (2012) Comparison of ultrasound and X-ray in determining the position of umbilical venous catheters. Resuscitation 83:705–709. https://doi.org/10.1016/j.resuscitation.2011
Nadroo AM, Glass RB, Lin J, Green RS, Holzman IR (2002) Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics 110(1 Pt 1):131–136
Ohki Y, Tabata M, Kuwashima M, Takeuchi H, Nako Y, Morikawa A (2000) Ultrasonographic detection of very thin percutaneous central venous catheter in neonates. Acta Paediatr 89:1381–1384
Racadio JM, Doellman DA, Johnson ND, Bean JA, Jacobs BR (2001) Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 107(2):E28
Sharpe E, Pettit J, Ellsbury DL (2013) A national survey of neonatal peripherally inserted central catheter (PICC) practices. Adv Neonatal Care 13(1):55–74. https://doi.org/10.1097/ANC.0b013e318278b907
Shukla H, Ferrara A (1986) Rapid estimation of insertional length of umbilical catheters in newborns. Am J Dis Child 140:786–788
Tauzin L, Sigur N, Joubert C, Parra J, Hassid S, Moulies M (2013) Echocardiography allows more accurate placement of peripherally inserted central catheters in low birthweight infants. Acta Paediatr 102:703–706. https://doi.org/10.1111/apa.12245
Wirsing M, Schummer C, Neumann R, Steenbeck J, Schmidt P, Schummer W (2008) Is traditional reading of the bedside chest radiograph appropriate to detect intraatrial central venous catheter position? Chest 134:527–533. https://doi.org/10.1378/chest.07-2687
Funding
This research was funded by Department of Pediatrics at Cohen Children’s Medical Center of NY given to NZ.
Author information
Authors and Affiliations
Contributions
NZ contributed to the conception, organization, and oversight of the study, data analysis and interpretation, the writing of the original manuscript draft, and final approval of the version to be published.
LW contributed to data analysis and interpretation, critical manuscript revision, and final approval of the version to be published.
JCR contributed to data analysis and interpretation, critical manuscript revision, and final approval of the version to be published.
SP contributed to critical manuscript revision and final approval of the version to be published.
DK contributed to the oversight of the study, data analysis and interpretation, critical manuscript revision, and final approval of the version to be published.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 2013 Helsinki declaration.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was not available as the study was approved by the Institutional Review Board as a quality improvement study and informed consent was not needed.
Additional information
Communicated by Patrick Van Reempts
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Zaghloul, N., Watkins, L., Choi-Rosen, J. et al. The superiority of point of care ultrasound in localizing central venous line tip position over time. Eur J Pediatr 178, 173–179 (2019). https://doi.org/10.1007/s00431-018-3269-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3269-9