Abstract
The clinical features and risk factors for recurrence of Kawasaki disease (KD) remain unclear. In order to summarize clinical features of recurrent KD and identify risk factors associated with recurrence, we conducted a retrospective review of the medical records of consecutive cases of KD from January 2002 to December 2010. Demographic, clinical, laboratory, and echocardiographic data were analyzed. The maximum coronary artery Z score normalized against body surface area was assessed using coronary artery diameters. At the first onset of recurrent KD, children had longer durations of fever before intravenous immunoglobulin (IVIG) treatment and higher levels of alanine aminotransferase, serum aspartate aminotransferase (AST), and lower hemoglobin levels than those with a single episode of KD. Multivariate logistic regression analysis showed that long durations of fever before IVIG treatment, high AST levels, and reduced hemoglobin levels were significantly associated with recurrent KD. Ten of the 22 recurrent KD children had coronary artery complications during the first onset episode, and six (60 %) of these also had coronary artery complications during the recurrence. Children with longer durations of fever, lower hemoglobin levels, and higher AST levels may be at increased risk for KD and coronary artery complications are more likely to occur in children with recurrent KD if they were present during the first episode.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Kawasaki disease (KD) is a self-limiting systemic inflammatory illness, and coronary artery dilatation and/or aneurysm are a major complication of KD [9, 20]. Nowadays, coronary complication of KD represents the leading cause of acquired heart disease in children [21]. Epidemiological studies in Asian children suggest that the etiological agent underlying KD may be associated with environmental changes [14, 24]. It is well known that the disease recurs in some children. Previous surveys have shown that the proportion of recurrent KD ranges from 1.4 % in China to 3 % in Japan [4, 22, 23]. However, despite a considerable number of cases of recurrent disease, limited information exists regarding risk factors associated with recurrent KD.
Coronary artery complications of KD constitute one of the most serious problems associated with the disease, and some studies have reported the relationship between cardiac abnormalities and the recurrence of KD [7, 15, 16]. Data from a Japanese nationwide survey showed that coronary artery complications are more likely to be observed among children with recurrent disease than among patients with the first episode of recurrence KD. However, this study was limited as the data used to assess coronary artery abnormalities were derived from the Japanese Ministry of Health [18], whose definition contains subjective elements, incompletely accounts for patient size and ignores a time course. More recently, regression equations based on measurements from nonfebrile normal children have been used to calculate Z scores based on body surface area [3, 11]. These allow for the assessment of the involvement of a time course. However, no study has used measurements of Z scores to assess changes in the coronary arteries in children with recurrent KD.
The purposes of this study were to summarize the clinical features of recurrent KD, determine risk factors that may help to identify children with KD at risk of recurrence, and to clarify whether a more complicated course occurs in recurrent cases compared to single-onset cases. We hypothesized that recurrent acute KD would be associated with laboratory and clinical evidence of systemic inflammation and, furthermore, that both noncoronary artery cardiac abnormalities and coronary artery abnormalities are correlated with recurrent KD.
Subjects and methods
Subjects
We retrospectively reviewed the clinical records of consecutive KD children treated between January 2002 and December 2010 at the Beijing Children Hospital in China. The criteria for a diagnosis of KD included fever (temperature exceeding 38 °C) accompanied by at least four of the following five criteria: bilateral conjunctival injection, changes in the lips and oral cavity, nonpurulent cervical lymphadenopathy, polymorphous exanthema, and changes in the extremities. These diagnostic criteria were in compliant with the Diagnostic Guidelines for Kawasaki Disease (5th revision, issued by the Japan Kawasaki Disease Research Committee in 2002).
The management of KD has been standardized at Beijing Children Hospital through the use of a defined clinical pathway. Pediatric hospitalizations of children aged <18 years with an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for KD (446.1) listed as the major or the second diagnosis on the discharge record were selected. After discharge, they were followed up in our Kawasaki disease clinic, which is a multidisciplinary clinic that includes an infectious disease specialist and cardiologist. Echocardiograms were obtained by experienced personnel and interpreted by the same group of cardiologists during the acute phase and 6 to 8 weeks later.
Recurrent KD was defined as intervals between the first and second episodes of ≥2 months [7]. This time interval was chosen as by this time we would expect almost all of those children to have normalized levels of inflammatory markers, including the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
Children were excluded when clinical or laboratory evidence suggested any other disease that can to mimic KD, such as adenovirus, Epstein–Barr virus, scarlet fever, or bacterial cervical lymphadenitis. Children diagnosed after the first 10 days of the onset of fever, those who experienced recurrent KD within 2 months of the first episode and those who suffered three or more episodes were also excluded. Finally, children who lacked any of the individual data parameters that were required for the statistical analyses in this study were also removed from our dataset.
Data collection
According to the surveys, all children were divided into two groups: single-onset KD groups, n = 1,151 and recurrent KD groups, n = 22. Their medical records were then retrospectively reviewed for demographic information, clinical and laboratory findings, and echocardiography results. Laboratory tests were performed at least once weekly until the serum levels of ESR and CRP normalized. The highest value was selected for analysis in the case of white blood cell count (WBC), serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), CRP, ESR, and the lowest value in the case of hemoglobin concentration, platelet count, serum albumin concentration, and sodium concentration.
The coronary artery sizes in children with KD were evaluated by cardiac ultrasound studies. Two-dimensional echocardiographic measurements of coronary artery dimensions, the left main, proximal right and proximal left anterior descending coronary arteries (LMCA, RCA, and LAD, respectively), were obtained at least three times during the early phase: before treatment, after treatment for 7 days, and before discharge. The diameter of the coronary artery was expressed as a Z score and the value of the standard deviation (SD) from a standardized coronary artery dimension were calculated from the body surface area (BSA) [3]. The calculation of body surface area is based on the following equation:
Dilation of the coronary artery was defined as a Z score ≥ 2.5, which was calculated using the following equation:
Statistical analysis
All data were analyzed with the Statistical Package for the Social Sciences for Windows software version 12.0 (SPSS Inc., Chicago, IL, USA). Data are presented as either the mean ± SD for continuous variables or as the number (percentage) of children for categorical variables. Intragroup variables were compared using the paired t test, and intergroup variables were compared using the Students t test. Proportions were compared using the χ 2 test. To determine the cutoff value of each parameter that was found to be significant, relative operating characteristic (ROC) curves were used. A logistic regression analysis was used to determine independent parameters that predicted recurrent KD, and results were expressed as an odds ratio (OR) with 95 % confidence intervals (CI). A 95 % CI that did not include 1.0 was interpreted to indicate statistical significance. A level of p < 0.05 was considered statistically significant. All authors had full access to the data and take responsibility for its integrity. All authors have read and agreed to the manuscript as written.
Results
Demographic data
Over the 8-year period of observation, 1,484 children were admitted to the Beijing Children Hospital with a diagnosis of KD. Three hundred and eleven children were excluded from this study, including 181 children who were diagnosed after 10 days of illness and 126 with incomplete clinical or laboratory data. Thus, 1,173 children were included as the study subjects. Of them, 26 children were potential cases of recurrent KD. Three of them were excluded as they presented within 2 months of their original disease and were therefore defined as suffering from a re-exacerbation of the original disease rather than a true recurrence. One further child was excluded as this was their third episode of recurrent KD. Consequently, 22 children were defined in the present study as recurrent KD, and 1,151 single-episode KD children were used as the control group. The proportion of recurrent KD was 1.88 %.
The mean age of the single-episode KD groups was 2.5 years (range, 2.07–176.43 months). The male to female ratio of single-episode KD children was 1.72:1 (728 males and 423 females). The distributions of age at the first illness and recurrence and the interval between the two episodes of the 22 children with recurrent KDs are shown in Table 1. Of the 22 children with recurrent KDs, 9 were boys and 13 girls with a male/female ratio of 1:1.4. The age at the first onset of recurrent KD ranges from 4.0 months to 4.8 years (mean, 26.0 ± 16.9 months). The age at the second onset of recurrent KD ranges from 11.0 months to 6.0 years (mean, 39.5 ± 19.5 months). The average interval between the two episodes was 12.0 ± 2.0 months. Twenty-one children (95.5 %) suffered a recurrence within 2 years after the first episode and one case (4.5 %) developed a recurrence after 2 years. In a comparison between genders in the single-episode groups, female children were more likely to suffer a recurrence after the initial episode (P = 0.026).
Characteristics and clinical outcomes in recurrence KD
Table 2 compares the results between the first episode of recurrent KD groups and the single-episode KD groups' duration of fever and laboratory data. The mean duration of fever before intravenous immunoglobulin (IVIG) treatment in the first episode of recurrent KD groups was 8.1 ± 3.1 days, whereas it was 5.2 ± 2.7 days in the single-episode KD groups. The mean duration of fever before IVIG treatment during the first episode of recurrent KD groups was significantly longer than it was in the single-episode KD groups (P < 0.001). There were no statistically significant differences between the groups with respect to the duration of fever after IVIG treatment, WBC, platelet count, ESR, CRP, serum albumin, and sodium (all, p > 0.05). However, hemoglobin, ALT, and AST were significantly higher (P < 0.001, P = 0.032, P < 0.001, respectively) in the first episode of recurrent KD groups compared to the single-episode KD groups.
Table 2 compares the results between the group with the second episode of recurrent KD groups and the single-episode KD groups. The mean duration of fever before IVIG treatment was significantly longer in the second episode of recurrent KD groups compared to the single-episode KD groups (P < 0.001). There were no statistically significant differences between the groups with respect to the mean duration of fever after IVIG treatment, WBC, hemoglobin level, platelet count, ESR, CRP, ALT, AST, serum albumin, and sodium (all, p > 0.05).
Patient laboratory parameters of children with recurrent KD are summarized in Table 2. There were also no statistically significant differences between the second episode and the first episode with respect to the duration of fever, WBC count, hemoglobin level, platelet count, ESR, CRP, ALT, serum albumin, and sodium (all, p > 0.05).
Coronary arteries in the single-episode KD group
All coronary diameters at admission were transformed to Z scores; the maximum Z score of the left main coronary artery (LMCA) was 1.76 ± 2.39, 2.23 ± 2.10 for the RCA and 2.40 ± 2.49 for the left coronary artery (LCA). Coronary artery abnormalities were found in 417 out of 1,151 children (36.2 %) in the single-episode KD group (Table 2).
Coronary arteries in the group with recurrent KD
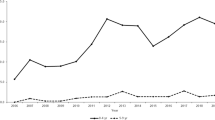
Figure 1 shows the distributions of the maximum Z score of the LMCA, RCA, and LAD over a time course. In the first episode of recurrent KD children, the Z scores for the LMCA, RCA, and LAD were 1.62 ± 0.93, 2.37 ± 1.33, and 2.87 ± 2.45, respectively. The maximum Z scores of all three coronary artery dimensions showed no significant differences between the first episode of recurrent KD group and the single-episode KD group. The incidence of coronary artery complications is summarized in Table 2. Ten out of 22 children (45.5 %) with the first episode of recurrent KD developed coronary artery abnormalities, which was higher than the single-episode KD group (417/1,151, 36.2 %), but this was not statistically significant (Table 2).
Maximum Z score of the a left main coronary artery (LMCA), b right coronary artery (RCA), and c left anterior descending coronary artery (LAD) branch diameters. Box encloses the 25th to 75th percentiles, line represents the median, and tails represent the 5th and 95th percentiles. Crosses represent the mean values. The maximum Z scores of all three coronary artery dimensions showed no significant differences among the three groups (the first episode of recurrent KD, the second episode of recurrent KD, and the single-episode KD groups)
In the second episode of recurrent KD children, the maximum Z scores were 1.71 ± 1.27, 2.03 ± 0.86, and 2.28 ± 1.42 for the LMCA, RCA, and LCA, respectively. The coronary artery dimensions showed no significant differences between the second episode of recurrent KD children and the single-episode KD groups, but there was a tendency for the scores to decrease compared to the first episode of recurrent KD children. The coronary artery abnormalities that developed were found in 8 (36.4 %) out of 22 children in the second episode of recurrent KD (Table 2).
Of note, 10 of the 22 recurrent KD children developed coronary artery abnormalities at the first episode, and 6 (60 %) of the 10 also experienced the abnormalities during the second episode of recurrent KD. However, 2 (16.6 %) of the 12 children that did not have coronary artery abnormalities at the first episode developed an abnormality during the second episode of recurrent KD. This was a significantly higher proportion than those who did not have coronary artery abnormalities at the first episode (p = 0.035).
Treatment in recurrence KD
Of 1,151 children in the single-episode KD group, 1,134 (98.5 %) received IVIG treatment in the acute febrile phase, 1,095(95.1 %)were treated with IVIG dose of 2 g/kg/day for 1 day, and 56 (4.9 %) were treated with IVIG dose of 1 g/kg/day for 2 consecutive days. Overall, 197 (96.2 %) IVIG-nonresponsive patients were treated by additional IVIG therapy, and 17 (1.5 %) out of 197 children were treated with steroids after additional IVIG treatment because of continuing fever.
In the first episode of recurrent KD children, all children (100 %) were administered IVIG at 2 g/kg/day for 1 day (n = 20; 91 %) or 1 g/kg/day for 2 days (n = 2; 9 %). Five (22.7 %) children were diagnosed as nonresponsive to IVIG, and one patient (4.5 %) was given steroids. There were no significant differences in the proportion of IVIG treatment or the number of nonresponsive children in the first episode group or those with recurrent KD (both, p > 0.05).
IVIG was also administered to all patients experiencing their second episode of recurrent KD. Of these, 21 (95.5 %) were treated with 2 g/kg/day IVIG for 1 day and one (4.5 %) was treated with 1 g/kg/day for 2 days. Four (18.1 %) were diagnosed as nonresponsive to IVIG, and steroids were not administered for recurrent KD in any patient. There also were no significant differences in the proportion of IVIG treatment and IVIG-nonresponsive between the second episode of recurrent KD and the single-episode KD groups (both, p > 0.05).
Risk factors of KD recurrence
To determine the relative effect of each risk factor in Kawasaki disease recurrence, we performed a logistic regression analysis. A comparison of the results between the first episode of recurrent KD groups and the single-episode KD groups for clinical and laboratory data showed that being female, the duration of fever before IVIG treatment, and ALT, AST, and hemoglobin levels were significant predictors of recurrent KD (P = 0.026, P < 0.001, P = 0.038, P < 0.001, P < 0.001, respectively). These five positive variables in addition to a single demographic variable (age in months) were included in the stepwise logistic regression analysis. Duration of fever before IVIG treatment (P = 0.009), AST level (P < 0.001), and hemoglobin level (P = 0.010) proved to be independent predictors of recurrent KD. ROC curves applied to each variable revealed the following cutoff values: duration of fever before IVIG treatment ≥10 days (sensitivity = 61 %, specificity = 81 %), AST ≥90 IU/L (sensitivity = 82 %, specificity = 71 %), and hemoglobin ≥9 g/dL (sensitivity = 42 %, specificity = 63 %) (Table 3). The area under the ROC curve for the duration of fever before IVIG treatment was 0.63, 0.77 for AST and 0.61 for hemoglobin.
Discussion
It is well known that KD recurs in some children. However, despite of a considerable number of recurrent cases, only a few detailed studies related to recurrent KD have been published. It has been reported that incidence of recurrent KD within 2 years from the first episode is higher than after 2 years have passed [7]. In this current study, many of the recurrent episodes were within 2 years from the first episode of the disease, after which the incidence decreased dramatically (Table 1). The results in the current study are comparable to the previous one. This may be a characteristic of the pattern of recurrence, which indicates that it is important to follow the patients carefully for 2 years following the initial episode.
In our study, the duration of fever before IVIG treatment was much longer in the first onset of recurrent KD than in the single-episode KD children. Fever that occurs as a result of cytokine release is a clinically useful index of systemic inflammation in KD [2]. This study mirrors the likelihood that the children that go on to develop recurrent KD have a higher severity of systemic inflammation.
Subclinical hepatic involvement is common in KD and tends to increase along with the natural course of inflammation [12, 25]. Our study shows that most of the single-episode KD children with elevated transaminases had only mild elevations. Children in the first onset episode of recurrent KD, however, had significant elevations in serum AST and ALT activity. We also observed that there was a relationship between the decreases in levels of hemoglobin in the first episode of children who went on to develop recurrent KD. Although the mechanism causing hemoglobin decrease in KD children is currently unknown, it may suggest that inflammation suppresses bone marrow function in children with KD [6]. The present data suggest that circulating levels of AST and hemoglobin are useful as a predictive marker for recurrence KD, and they may serve as a therapeutic target for prevention of recurrence KD in future.
It has been reported that the maximum serum CRP levels might have a prognostic significance for patients with KD [5, 8, 17], although this has been disputed by Hirata et al. [7]. Our findings show that there was no significant difference in CRP between recurrence KD children and the single-episode KD children.
Among children with recurrence KD, the laboratory parameters were not significantly different between the first onset and during the second onset. It is well known that KD is a self-limiting disease, and the inflammatory processes of KD progress to a peak during the acute period before regressing to a convalescent stage [12, 13]. Our current results corroborate this.
The most serious complication of KD is the development of coronary artery aneurysms. The proportion of coronary artery complications in this current study was much higher than that reported in the literature. This may because a large number of patients with severe KD or those in whom treatment had been unsuccessful was referred to our hospital. In addition, many previously reported studies used Japanese Ministry of Health established criteria for coronary abnormalities. It is recognized that these definitions are arbitrary, fail to account for patient size, and only reflect the time point of maximal dimension. For example, a 2.5-mm LCA might be normal in a 5-year-old child but is clearly dilated in a 3-month-old infant. Thus, the frequency of the occurrence of coronary artery abnormality may have been underestimated previously. De Zorzi et al. [3] explored the distribution of coronary artery dimensions in patients with KD whose arteries were classified as “normal” by Japanese Ministry of Health criteria, adjusted for body surface area as Z scores using linear regression analyses derived previously from a normal afebrile control population. They noted that 27 % of patients with no coronary artery involvement by Japanese Ministry of Health criteria had at least one coronary artery Z score > 2 or two standard deviations from the mean based on BSA [1, 11]. This was similar to the present findings and other reports.
The present findings suggest that the maximum Z scores of all three coronary artery dimensions and the proportion of coronary artery complications did not differ between the first onset and the second onset in recurrent KD children. It is well known that some coronary aneurysms are attributable to Kawasaki disease regression [10, 19], and our findings suggested that there was no increased risk of aneurysm with repeated episodes of vasculitis in the second-onset KD compared to single episodes. Nakamura et al. [16] reported that the coronary artery complications are more likely to be observed among the second-onset KD children than among the first onset of recurrent KD children. However, their studies also used Japanese Ministry of Health criteria for coronary abnormalities rather than the more sensitive BSA-adjusted coronary artery Z scores used in our current study. If a patient experiences a recurrence of KD long after the first episode, the patient will have advanced to an older age group. Thus, we hypothesize that coronary artery complications are more likely to be included among cases of recurrent KD.
Hirata et al. [7] reported that the incidence of recurrent KD was high for children with coronary artery complications at the first episode, and the presence of coronary artery complications at the first episode was a risk factor for recurrence. Our study also determined that coronary artery complications during the first episode in children who went on to develop recurrent KD were more frequent than the single-episode KD children, although this difference was not significantly different. In addition, we found that it was more likely for children who had developed coronary artery complications in the first onset episode to have them again during the recurrent episode of KD, compared to those who had normal coronary arteries on their first presentation. This indicates that children with coronary artery complications at the first episode have a greater risk of these complications recurring in future episodes of KD.
In our study, there was no difference in the proportion of patients that received IVIG treatment between those with the first episode of recurrent KD and a single episode of KD. This suggests a weak correlation between recurrence and IVIG therapy. Of note, although the results were not statistically significant, five (22.7 %) patients with their first episode of recurrent KD did not respond to IVIG, which indicated a tendency to develop recurrence in these patients. One explanation may be that the clinical condition of these nonresponsive children was more serious than the children that responded to IVIG therapy, as reflected by the significantly longer duration of fever. Therefore, more studies are required to assess the potential risk of recurrence in the IVIG-nonresponsive children with KD.
There were some limitations to the present study. Firstly, this is a retrospective study. There might be bias introduced in the results. Another drawback is the possibility of selection bias. This study included a relatively small number of patients with recurrent disease. For multiple reasons, complete data linkage was not possible, and some data were not available in some children; therefore, only 22 cases were available for inclusion.
In conclusion, although limited by its retrospective design, this study suggests that a longer duration of fever, lower levels of hemoglobin, and higher AST levels could help to identify children who are at an increased risk of recurrent KD. The risk of coronary artery complications in children with KD recurrence is probably higher in those children with coronary artery complications at their initial episode. These results provide important information that should be considered during the follow-up of children with KD, and further prospective studies will be conducted to confirm these findings.
Abbreviations
- AST:
-
Serum aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- BSA:
-
Body surface area
- CRP:
-
C-reactive protein
- CI:
-
Confidence interval
- ESR:
-
Erythrocyte sedimentation rate
- IVIG:
-
Intravenous immunoglobulin
- KD:
-
Kawasaki disease
- LMCA:
-
Left main coronary artery
- LAD:
-
Left anterior descending coronary artery
- OR:
-
Odds ratio
- RCA:
-
Right coronary artery
- WBC:
-
White blood cell count
References
Baer AZ, Rubin LG, Shapiro CA, Sood SK, Rajan S, Shapir Y, Romano A, Bierman FZ (2006) Prevalence of coronary artery lesions on the initial echocardiogram in Kawasaki syndrome. Arch Pediatr Adolesc Med 160:686–690
Brogan PA, Bose A, Burgner D, Shingadia D, Tulloh R, Michie C (2002) Kawasaki disease: an evidence based approach to diagnosis, treatment, and proposals for future research. Arch Dis Child 86(4):286–290
de Zorzi A, Colan SD, Gauvreau K, Baker AL, Sundel RP, Newburger JW (1998) Coronary artery dimensions may be misclassified as normal in Kawasaki disease. J Pediatr 133:254–258
Du ZD, Zhang YL, Zhao D, DU JB, Lu S, Yi JM, Hou AC, Zhou ZS, Ding GF (2007) The epidemiologic study on kawasaki disease in Beijing from 2000 through 2004. Pediatr Infect Dis J 26:449–451
Egami K, Muta H, Ishii M, Suda K, Sugahara Y, Iemura M, Matsuishi T (2006) Prediction of resistance to intravenous immunoglobulin treatment in patients with Kawasaki disease. J Pediatr 149:237–240
Eladawy M, Dominguez SR, Anderson MS, Glodé MP (2011) Abnormal liver panel in acute kawasaki disease. Pediatr Infect Dis J 30(2):141–144
Hirata S, Nakamura Y, Yanagawa H (2001) Incidence rate of recurrent Kawasaki disease and related risk factors:from the results of nationwide surveys of Kawasaki disease in Japan. Acta Pediatr 90:40–44
Jansson LT, Kling S, Dallman PR (1986) Anemia in children with acute infection seen in a primary care pediatric outpatient clinic. Pediat Infect Dis 5:424–427
Kato H, Ichinose E, Yoshioka F, Takechi T, Matsunaga S, Suzuki K, Rikitake N (1982) Fate of coronary aneurysms in Kawasaki disease: serial coronary angiography and long-term follow-up study. Am J Cardiol 49:1758–1766
Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, Kazue T, Eto G, Yamakawa R (1996) Long-term consequences of Kawasaki disease: a 10- to 20-year follow-up study of 594 patients. Circulation 94:1379–1385
Kurotobi S, Nagai T, Kawakami N, Sano T (2002) Coronary diameter in normal infants, children and patients with Kawasaki disease. Pediatr Int 44:1–4
Lee KY, Han JW, Hong JH, Lee HS, Lee JS, Whang KT (2004) Inflammatory processes in Kawasaki disease reach their peak at the sixth day of fever onset: laboratory profiles according to duration of fever. J Korean Med Sci 19:501–504
Lee KY, Rhim JW, Kang JH (2012) Kawasaki disease: laboratory findings and an immunopathogenesis on the premise of a “protein homeostasis system”. J Yonsei Med 53:262–275
Mason W (2007) Epidemiology and etiology of Kawasaki disease. Pediatr Infect Dis 2007:273–295
Nakamura Y, Hirose K, Yanagawa H, Kato H, Kawasaki T (1994) Incidence rate of recurrent Kawasaki disease in Japan. Acta Paediatr 83:104–106
Nakamura Y, Yanagawa H, Ojima T, Kawasaki T, Kato H (1998) Cardiac sequelae of Kawasaki disease among recurrent cases. Arch Dis Child 78:163–165
Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, Shulman ST, Bolger AF, Ferrieri P, Baltimore RS, Wilson WR, Baddour LM, Levison ME, Pallasch TJ, Falace DA, Taubert KA (2004) Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114:1708–1733
Research Committee on Kawasaki Disease (1984) Report of subcommittee on standardization of diagnostic criteria and reporting of coronary artery lesions in Kawasaki disease. Japanese Ministry of Health and Welfare, Tokyo
Sasaguri Y, Kato H (1982) Regression of aneurysms in Kawasaki disease: a pathologic study. J Pediatr 100:225–231
Suzuki A, Kamiya T, Kuwahara N, Ono Y, Kohata T, Takahashi O, Kimura K, Takamiya M (1986) Coronary arterial lesions of Kawasaki disease: cardiac catheterization findings of 1100 cases. Pediatr Cardiol 7:3–9
Taubert KA, Rowley AH, Shulman ST (1991) Nationwide survey of Kawasaki disease and acute rheumatic fever. J Pediatr 119:279–282
Yanagawa H, Nakamura Y, Yashiro M, Fujita Y, Nagai M, Kawasaki T, Aso S, Imada Y, Shigematsu I (1988) A nationwide incidence survey of Kawasaki disease 1985–1986 in Japan. J Infect Dis 158:1296–1301
Yanagawa H, Nakamura Y, Yashiro M, Kawasaki T, Kato H (1995) Epidemiologic pictures of Kawasaki disease in Japan: from the nationwide incidence survey in 1991 and 1992. Pediatrics 95:475–479
Yanagawa H, Yashiro M, Nakamura Y, Kawasaki T, Kato H (1995) Results of 12 nationwide epidemiological incidence surveys of Kawasaki disease in Japan. Arch Pediatr Adolesc Med 149:779–783
Zulian F, Falcini F, Zancan L, Martini G, Secchieri S, Luzzatto C, Zacchello F (2003) Acute surgical abdomen as presenting manifestation of Kawasaki disease. J Pediatr 142:731–735
Conflict of Interest
This study was supported by National Natural Science Foundation of China (81274109, 30973238), Key Research Project of Beijing Natural Science Foundation (B)/Beijing Education Committee (KZ201010025024), and Science and Technology Innovation Platform (PXM2011_014226_07_000085).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, Hm., Du, ZD. & Fu, Pp. Clinical features of recurrent Kawasaki disease and its risk factors. Eur J Pediatr 172, 1641–1647 (2013). https://doi.org/10.1007/s00431-013-2101-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-013-2101-9