Abstract
Polymerase chain reaction (PCR) techniques have been increasingly used to detect microbial DNA in cerebrospinal fluid (CSF) for the diagnosis of bacterial meningitis. In order to determine the rapidity, sensitivity and specificity of 16S rRNA-based fluorescence quantitative polymerase chain reaction (FQ-PCR), 16S rRNA-based FQ-PCR, CSF bacterial culture and CSF routine analysis were compared in the diagnosis of bacterial meningitis in children. Twenty children who were clinically suspected of bacterial meningitis were included in this study. A total of 2.0 ml of CSF was collected from every child and was subjected to 16S rRNA-based FQ-PCR, CSF culture and CSF routine analysis. Bacterial DNA copies and the cycle threshold (CT) value of the 16S rRNA-based FQ-PCR was recorded, and the results were compared with CSF culture and CSF routine analysis. Seven children were found to be positive with a rate of 35% (7/20) when detected with 16S rRNA-based FQ-PCR and four children displayed a positive rate of 20% (4/20) with the CSF culture method. These two groups displayed a significant difference, with a p-value of 0.002. The method of 16S rRNA-based FQ-PCR demonstrated a high specificity when compared to the standard microbes. A negative correlation was noted between the CT value and the bacteria DNA copies, and the CT value was indicative of the seriousness of bacterial meningitis. 16S rRNA-based FQ-PCR was proved to be a more rapid, sensitive and specific method compared with CSF culture and it should have promising usage in the diagnosis of bacterial meningitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial meningitis is a serious disease with high morbidity and mortality. To reduce death and permanent neurological sequellae (e.g. hearing loss, mental retardation, seizures and behavioural changes) as much as possible, a fast and accurate diagnosis is of utmost importance for the early targeting of antimicrobial and adjuvant therapy. In the diagnosis of bacterial meningitis, the current golden standard is cerebrospinal fluid (CSF) culture. Although it helps greatly in the clinical practice, such limitations as the long length of time required and a high negative rate in up to 13% of all cases make it difficult to suggest a rapid, sensitive and specific clinical diagnosis [4, 7, 10, 14]. Meningitis may also be caused by fastidious or slow-growing microorganisms that are difficult to be detected by CSF culture. Furthermore, the common practice of antibiotics therapy prior to CSF evaluation coupled with inconsistent laboratory support in developing countries makes aetiological diagnosis extremely difficult [2]. Prior antibiotics therapy 12 h or more before lumbar puncture can sterilise the CSF [8]. In addition, tuberculous meningitis, which resembles partially treated pyogenic meningitis in many respects, creates further diagnostic difficulties.
In recent years, polymerase chain reaction (PCR) techniques have been used increasingly to amplify and detect microbial organisms of bacterial meningitis. The PCR assay has been used for the identification of Streptococcus pneumoniae and for the simultaneous detection of Neisseria meningitidis, Haemophilus influenzae and streptococci as aetiological agents of bacterial meningitis. Use of broad-range bacterial primers in the diagnosis of bacterial meningitis has been reported in earlier studies. PCR-based assays have become available to provide an early and accurate diagnosis of bacterial meningitis [8].
Here, we found that amplification with fluorescence quantitative polymerase chain reaction (FQ-PCR) in the bacterial 16S rRNA gene of CSF could make a more rapid and reliable diagnosis in comparison with CSF culture and CSF routine analysis.
Materials and methods
Clinical specimens
Between October 2003 and May 2005, a total of 11 males and nine females who were clinically suspected of bacterial meningitis from the neonatal department and the intensive care unit of the Children’s Hospital, Zhejiang University, China, were evaluated. The diagnosis criteria of bacterial meningitis include pathogenic bacteria isolated from CSF or clinical meningitis with all of the following: lymphocytes and neutrophils, low concentration of glucose in CSF (<50% of that in blood), sterile blood and CSF cultures, full recovery (without antituberculosis chemotherapy) 3 months after admission [12]. The study was approved by the Medical Ethics Committee of the Medical College, and informed consent was obtained from the parents. The age of the patients ranged from 3 days to 11 years, in which 16 patients were 3 days to 6 months old and the other four patients were 3 years to 11 years old. Two millilitres of CSF was collected from every patient by lumbar puncture under sterile conditions before and after the antibiotics treatment. One millilitre of CSF was detected by CSF culture and CSF routine analysis, and the other 1.0 ml of CSF was determined by FQ-PCR.
The specificity of FQ-PCR was determined with Mycoplasma pneumoniae, Chlamydia trachomatis, three standard bacterial strains (Escherichia coli, Staphylococcus aureus, Streptococcus pneumoniae) and human genomic DNA. Mycoplasma pneumoniae, Chlamydia trachomatis and the three standard bacterial strains (Escherichia coli, Staphylococcus aureus, Streptococcus pneumoniae) were preserved by the Center Lab of the Children’s Hospital, Zhejiang University, China. Human genomic DNA was provided by the Chinese Academy of Preventive Medicine.
FQ-PCR amplification
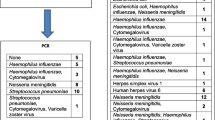
Oligonucleotide primers were designed to be complementary to conserved regions in the 16S rRNA gene of different kinds of bacteria. This was based on a computer alignment of 16S rRNA gene sequences of different kinds of bacteria available on GenBank. The universal fluorescent probe was designed in the region that was amplified by the synthesised primers. MegAlign was used to analyse the 16S rRNA gene sequences and to design the sequences of the oligonucleotide primers and the universal fluorescent probe. The sequences of primers were as follows: forward (P690F) 5′-TGTGTAGCGGTGAAATGCG-3′ (690–708 bp); reverse (P829R) 5′-CATCGTTTACGGCGTGGAC-3′ (829–811 bp). Sequences of the universal probe (UnProbe) were as follows: 5′-TCTAATCCTGTTTGATCCCCACG-3′ (800–778 bp). With these primers and universal probe, we could almost determine all of the common pathogenic bacteria of bacterial meningitis. The representative bacterial species that could be detected are shown in Table 1. Because Mycoplasma pneumoniae and Chlamydia trachomatis were not common pathogens of bacterial meningitis, we intended to apply them as a negative control in our study, and this strategy was deliberately planned during computer alignment. Subsequently, the primers we designed were not able to amplify Mycoplasma pneumoniae and Chlamydia trachomatis.
One millilitre of CSF specimen was moved into a 1.5-ml microcentrifuge aseptically and was centrifuged for 5 min. The supernatant was decanted and the cell pellets were suspended in 50 μl of lysis buffer, which contained 10 mmol/L Tris-HCL (pH 7.6), 5 mmol/L EDTA and 0.5% sodium dodecyl sulphate. The mixture was then boiled for 10 min. After the mixture was centrifuged at 4°C, 4 μl of supernatant served as the template in the FQ-PCR amplification. FQ-PCR was performed on an ABI 5700 thermocycler. The cycling parameters of PCR were initial preincubation at 94°C for 4 min and then 40 cycles consisting of 94°C for 20 s and 60°C for 60 s. A positive control with Escherichia coli ATCC11775 and Staphylococcus aureus ATCC25923 and a negative control with no DNA sample were used in every PCR reaction. Serial dilutions starting from 1 × 103 copies/μl to 1 × 106 copies/μl of standard plasmid DNA was used to create the external calibration curve to quantify the products load in FQ-PCR. The cycle threshold (CT) value, which was defined as the fractional cycle number at which the fluorescence signal passes the fixed threshold, was determined. Samples with CT value of 37.0 to 40.0 were quantified as 0 copies/μl; samples with CT value less than 35.0 were quantified with the actual CT value; but if the CT value was between 35.0 and 37.0, a second FQ-PCR was requested; if the CT value was not 37.0 to 40.0 in the second test, the actual CT value was used in the quantification.
FQ-PCR products sequencing
FQ-PCR products were delivered to Invitrogen for sequencing.
CSF culture
CSF specimens were first inoculated into 20.0 ml of blood enrichment medium. The culture bottle was incubated at 35.5°C. Subcultures were performed after 3 days of incubation. Samples were removed from each culture bottle aseptically to a blood agar plate and a chocolate agar plate. The positive growth was recorded at 24 h and biochemical tests were carried out to identify the bacteria by use of the VITEK-60 microorganism autoanalysis system. The culture bottle and VITEK-60 microorganism autoanalysis system were bought from bioMérieux Corporate, France.
CSF routine analysis
CSF was collected into sterile polystyrene tubes and immediately submitted for analysis. CSF glucose and lactate were determined using the Roche™ kit with Hitachi equipment. The total CSF protein was determined by the Hitachi equipment using the benzethonium chloride precipitation technique standardised to the biuret method. Cell counts were determined using a calibrated Fuchs-Rosenthal chamber after staining with toluidine blue. CSF analysis to distinguish polymorphonuclear leukocytes (PMNs) and lymphocytes was carried out using a Shandon Cytocentrifuge and Pappenheim stain.
Data analysis
The chi-square test was used to analyse all of the data with SPSS software (version 13.0). Statistical significance was recorded if the p-value was less than 0.01.
Results
Specificity of FQ-PCR
Three standard bacterial strains (Escherichia coli, Staphylococcus aureus, Streptococcus pneumoniae) were detected with FQ-PCR. Their results were demonstrated to be positive, with CT between 18.2 and 21.6. Mycoplasma pneumoniae, Chlamydia trachomatis and human genomic DNA were also detected with FQ-PCR. Their results were negative. This revealed that 16S rRNA gene FQ-PCR did not cross-react with DNA from humans, Mycoplasma pneumoniae and Chlamydia trachomatis, so our 16S rRNA gene FQ-PCR was highly specific for the common pathogen of bacterial meningitis.
Comparison of FQ-PCR, CSF culture and CSF routine analysis
During every FQ-PCR circulation, two groups of Escherichia coli ATCC11775 and Staphylococcus aureus ATCC25923 were used as positive controls. And two groups with no DNA template served as negative controls. If the CT value was less than 35.0, the result was positive. In the FQ-PCR amplification group, seven patients were found to be positive with a rate of 35% (7/20). In the CSF culture group, four patients showed a positive result with a rate of 20% (4/20). Therefore, the positive rate of the FQ-PCR group was higher than the CSF culture group. The chi-square test for paired counting data was used to calculate the p-value of the FQ-PCR group and the CSF culture group (χ2=9.286, p = 0.002). The results of these two groups were significantly different (p < 0.01, Table 2). All of the four positive patients in the CSF culture group showed positive results in the FQ-PCR group. The other three patients whose FQ-PCR results were positive did not show positive CSF culture results, but all three of these patients were diagnosed with bacterial meningitis based on clinical manifestations, CSF routine analysis and clinical prognosis, and none of the 13 patients with negative FQ-PCR results had positive CSF culture results.
The outcome of the CSF displayed different kinds of infectious diseases of the central nervous system [15]. FQ-PCR, CSF culture and CSF routine analysis were compared in consideration of these differences (Table 2). A total of six patients showed positive results both in CSF routine analysis and FQ-PCR. Four patients were found to be positive both in CSF culture and FQ-PCR. Three of these four cases were shown to be positive in FQ-PCR, CSF culture and CSF routine analysis. In the CSF culture group, Escherichia coli was the most common pathogen of bacterial meningitis (50%).
Relationship between CT value, bacteria DNA copies and the seriousness of bacterial meningitis
The CT value and number of bacteria DNA copies differed in patients with bacterial meningitis. Patients with more serious meningitis had lower CT values and more bacteria DNA copies, while patients with milder infections had higher CT values and fewer bacteria DNA copies (Table 3). Therefore, the CT value had a negative correlation with bacteria DNA copies. The hospitalisation period was shorter in patients with a higher CT value and fewer bacteria DNA copies. And given a lower CT value and more bacteria DNA copies, patients usually had a much longer hospital stay. There was a life-threatening case of bacterial meningitis with such complications as subdural effusion and acute bronchial pneumonia in our study. CSF was detected with FQ-PCR three times in the early phase of infection. The CT values were 18.5, 25.8 and 30.3, respectively. During this patient’s 58-day hospitalisation period, intravenous medications of ceftazidime, benzylpenicillin, ceftriaxone sodium and meropenem were administered. Preceding complications were cured finally and the patient recovered fully without any sequellae. Laboratory studies showed a normal CT value of 37.6, negative CSF culture and negative CSF routine analysis on his day of discharge.
Comparison of CSF FQ-PCR and bacterial DNA sequencing
All of the seven products which demonstrated positive FQ-PCR results were subjected to sequencing. Four specimens with CT values of 17.9, 18.5, 25.8 and 26.5 demonstrated a DNA sequence of Escherichia coli, Klebsiella pneumonia, Enterobacter cloacae and Escherichia coli, respectively. This was consistent with the positive CSF culture results. The CT values of the other three specimens was 28.9, 30.4 and 31.8. These high CT values indicated that bacteria copies of this CSF sample might be very low. Also, the DNA sequencing of these specimens failed, which was consistent with their low bacteria copies and negative CSF culture.
Comparison of FQ-PCR before and after therapy
These seven positive cases were all treated in time. FQ-PCR after therapy was negative in all of them (Table 2).
Discussion
Pathogen examination plays an extremely critical role in the diagnosis and antibiotics treatment of bacterial meningitis. Because of the high mortality of infection in the central nervous system [6], the early detection and rapid differentiation of bacteria in the central nervous system is extremely important.
However, such methods as CSF culture and CSF routine analysis cannot make a rapid, sensitive and specific result. Although CSF routine analysis is always required in bacterial meningitis, such parameters as cell counts, total protein concentration and glucose concentration vary over a wide range. And there are no microbiological and chemical findings in the CSF in a few patients whose clinical manifestation of bacterial meningitis are obvious. CSF culture is influenced by various factors and can reduce the chance of a positive result [13]. It requires at least 24–48 h of incubation and subsequent biochemical tests to identify the bacteria. Furthermore, classical clinical manifestations of bacterial meningitis are always difficult to be observed in infants and children because of delayed elevated intracranial pressure and the absence of meningeal irritation signs [16], so it is still difficult to obtain a rapid and specific identification of bacteria in the clinical practice of bacterial meningitis.
The 16S rRNA gene is the gene that encodes the sequences of rRNA. It presents in all bacteria and such prokaryotic organisms as chlamydia, mycoplasma and actinomycete, but not in the non-prokaryotic organisms, such as viruses and fungi. The 16S rRNA gene sequence is about 1,550 bp long and is composed of both conserved and variable regions. The conserved regions are highly conserved in all bacteria and the variable regions differ in different bacteria due to occasional mutations in the long evolutionary process. Therefore, different bacteria could be distinguished by the 16S rRNA analysis using special primers [11].
The FQ-PCR assay is a rapid, sensitive and specific method for the detection of microbial infection and has a high reproduction quality. It has been widely used in gene expression research and microbial detection [1, 9]. In this study, we introduced a fluorescent-labelled TaqMan probe into the PCR procedure. The fluorescent quencher, which is located in the 3′ end of the TaqMan probe, could efficiently inhibit the activity of the fluorescent reporter, which is located in the 5′ end of the TaqMan probe, without interfering the integrity of the probes. A fluorescent signal could be detected following the cleavage of the fluorescent-labelled probe by the 5′-exonuclease activity of the Taq polymerase. The release of the fluorescent signal during each round of amplification allows the rapid detection and quantification of DNA [3].
CSF, which is sterile in a healthy person, could be detected with 16S rRNA gene PCR to confirm bacterial infection just as blood samples [13, 18]. Not only is it more sensitive in identifying bacteria compared with CSF culture, FQ-PCR had a great advantage of time-saving, as it took only about 2–3 h in total. More importantly, this assay could not be interfered by antibiotics in CSF or blood, since both dead and viable microorganisms could be detected [10, 17]. In these 20 patients, a total of six patients demonstrated positive results in both CSF routine analysis and FQ-PCR, four positive patients in both CSF culture and FQ-PCR, and three positive patients in all of the FQ-PCR, CSF culture and CSF routine analysis. FQ-PCR products were further delivered to sequencing and the results revealed a good agreement with CSF cultures. CSF culture might be negative in some patients due to low bacteria DNA copies or antibiotics therapy prior to lumbar puncture, but FQ-PCR could report a positive result. So it was true that FQ-PCR was more sensitive than CSF culture. 16S rRNA gene FQ-PCR did not cross-react with DNA from humans, Mycoplasma pneumoniae and Chlamydia trachomatis. Our 16S rRNA gene FQ-PCR was highly specific for the common pathogen of bacterial meningitis. Therefore, 16S rRNA gene FQ-PCR was a rapid, sensitive and specific method for the diagnosis of bacterial meningitis compared with CSF culture and CSF routine analysis.
Attention should be paid to the negative correlation between the CT value and bacteria DNA copies. It has been demonstrated that the lower CT values corresponded with more bacteria DNA copies and more severe clinical manifestations. The higher CT values corresponded with fewer bacteria DNA copies and milder severe clinical manifestations. In patients who had long hospitalisation periods of between 47 and 58 days, their CT values were all less than 20.0. So the CT value was probably an indicator of the seriousness of bacterial meningitis.
In patient 18, the FQ-PCR and CSF culture were positive, but the CSF routine analysis was negative. The values of the CSF routine analysis were usually characteristic of meningitis. However, the values elicited by different aetiological agents often overlapped by as much as 30 to 40%, and might be relatively normal in some patients [5]. CSF routine analysis was relatively normal in patient 18; this may be due to the different aetiological agents and patient idiosyncrasy.
In conclusion, our16S rRNA gene FQ-PCR was proved to be a valuable supplementary test in clinical practice. The bacterial culture of CSF remains the cornerstone in the diagnosis of bacterial meningitis. However, especially when antimicrobial therapy has already been started at the time of lumbar puncture, conventional methods should always be accompanied by molecular detection, because the sensitivity of direct CSF routine analysis and bacterial culture drops substantially when therapy has started. The FQ-PCR assay took only 2–3 h from the time of sample collection to the results analysis, and it was proved to be a sensitive and specific method. So, FQ-PCR could help greatly in the pathogen identification of bacterial meningitis and it has a promising perspective in clinical practice.
Abbreviations
- PCR:
-
Polymerase chain reaction
- CSF:
-
Cerebrospinal fluid
- FQ-PCR:
-
Fluorescence quantitative polymerase chain reaction
- CT:
-
Cycle threshold
References
Bièche I, Onody P, Laurendeau I, Olivi M, Vidaud D, Lidereau R, Vidaud M (1999) Real-time reverse transcription-PCR assay for future management of ERBB2-based clinical applications. Clin Chem 45:1148–1156
Cartwright K, Reilly S, White D, Stuart J (1992) Early treatment with parenteral penicillin in meningococcal disease. BMJ 305:143–147
Corless CE, Guiver M, Borrow R, Edwards-Jones V, Kaczmarski EB, Fox AJ (2000) Contamination and sensitivity issues with a real-time universal 16S rRNA PCR. J Clin Microbiol 38:1747–1752
Durand ML, Calderwood SB, Weber DJ, Miller SI, Southwick FS, Caviness VS Jr, Swartz MN (1993) Acute bacterial meningitis in adults. A review of 493 episodes. N Engl J Med 328:21–28, correction 1712–1713
Gray LD, Fedorko DP (1992) Laboratory diagnosis of bacterial meningitis. Clin Microbiol Rev 5:130–145
Greisen K, Loeffelholz M, Purohit A, Leong D (1994) PCR primers and probes for the 16S rRNA gene of most species of pathogenic bacteria, including bacteria found in cerebrospinal fluid. J Clin Microbiol 32:335–351
Janner DL, Probert WS, McClure CD (2007) Ribosomal DNA assay of culture-negative Streptococcus pneumoniae meningitis. Pediatr Neurol 37(1):55–58
Pandit L, Kumar S, Karunasagar I, Karunasagar I (2005) Diagnosis of partially treated culture-negative bacterial meningitis using 16S rRNA universal primers and restriction endonuclease digestion. J Med Microbiol 54:539–542
Pas SD, Fries E, De Man RA, Osterhaus AD, Niesters HG (2000) Development of a quantitative real-time detection assay for hepatitis B virus DNA and comparison with two commercial assays. J Clin Microbiol 38:2897–2901
Schuurman T, de Boer RF, Kooistra-Smid AM, van Zwet AA (2004) Prospective study of use of PCR amplification and sequencing of 16S ribosomal DNA from cerebrospinal fluid for diagnosis of bacterial meningitis in a clinical setting. J Clin Microbiol 42(2):734–740
Shang SQ, Hong WL, Yu HM (1999) Detection of bacterial DNA with polymerase chain reaction and reverse hybridization of 16SrRNA gene. Chin J Infect Dis 17:30–32
Thwaites GE, Chau TTH, Stepniewska K, Phu NH, Chuong LV, Sinh DX, White NJ, Parry CM, Farrar JJ (2002) Diagnosis of adult tuberculous meningitis by use of clinical and laboratory features. Lancet 360(9342):1287–1292
Tong MQ, Shang SQ, Wu YD, Zhao ZY (2004) Rapid diagnosis of neonatal sepsis by 16SrRNA genes PCR amplification and genechip hybridization. Chin J Pediatr 42:663–667
Tunkel AR, Scheld WM (1995) Acute bacterial meningitis. Lancet 346:1675–1680
Wu XR (2002) Pyogenic meningitis. In: Wang MD (ed) Pediatrics, 5th edn. People’s Health Publishing House, Beijing
Wu SX (2005) Study on newborns with intracranial infection. J Appl Clin Dis 20:97–99
Xu J, Millar BC, Moore JE, Murphy K, Webb H, Fox AJ, Cafferkey M, Crowe MJ (2003) Employment of broad-range 16S rRNA PCR to detect aetiological agents of infection from clinical specimens in patients with acute meningitis—rapid separation of 16S rRNA PCR amplicons without the need for cloning. J Appl Microbiol 94:197–206
Zheng JY, Shang SQ, Wu YD, Xu YP, Du LZ (2005) Use of 16S rRNA gene chip hybridization in the diagnosis of neonatal sepsis. Chin J Infect Dis 23:187–190
Acknowledgement
This study was supported by a grant from the Zhejiang Province Great Science Foundation (no. 001103059-01).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duan, QJ., Shang, SQ. & Wu, YD. Rapid diagnosis of bacterial meningitis in children with fluorescence quantitative polymerase chain reaction amplification in the bacterial 16S rRNA gene. Eur J Pediatr 168, 211–216 (2009). https://doi.org/10.1007/s00431-008-0747-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-008-0747-5