Abstract
Both human and animal studies indicate that alcohol withdrawal following chronic alcohol consumption (CAC) impairs many of the cognitive functions which rely on the prefrontal cortex (PFC). A candidate signaling cascade contributing to memory deficits during alcohol withdrawal is the protein kinase A (PKA)/cAMP-responsive element binding (CREB) cascade, although the role of PKA/CREB cascade in behavioral and molecular changes during sustained withdrawal period remains largely unknown. We demonstrated that 1 week (1W) or 6 weeks (6W) withdrawal after 6-month CAC impairs working memory (WM) in a T-maze spontaneous alternation task and reduces phosphorylated CREB (pCREB) in the PFC but not the dorsal CA1 region (dCA1) of the hippocampus compared with CAC and water conditions. In contrast, both CAC-unimpaired and withdrawn-impaired mice exhibited decreased pCREB in dCA1 as well as reduced histone H4 acetylation in PFC and dCA1, compared with water controls. Next, we showed that enhancing CREB activity through rolipram administration prior to testing improved WM performance in withdrawn mice but impaired WM function in water mice. In addition, WM improvement correlates positively with increased pCREB level selectively in the PFC of withdrawn mice. Results further indicate that direct infusion of the PKA activator (Sp-cAMPS) into the PFC significantly improves or impairs, respectively, WM performance in withdrawn and water animals. In contrast, Sp-cAMPS had no effect on WM when infused into the dCA1. Collectively, these results provide strong support that dysregulation of PKA/CREB-dependent processes in prefrontal neurons is a critical molecular signature underlying cognitive decline during alcohol withdrawal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cessation of chronic ethanol consumption is often accompanied by several withdrawal symptoms such as increased anxiety, difficulties of concentration and cognitive deficits (Voltaire-Carlsson et al. 1996; Watanabe et al. 2001). Clinical studies have shown that poorer cognitive performance in alcoholic patients was related to severe withdrawal bouts and heavy alcohol consumption (Errico et al. 2002). In line with these observations, both human and animal studies indicate that alcohol withdrawal following chronic alcohol consumption (CAC) impairs many of the cognitive functions which rely on the prefrontal cortex (PFC) (Moselhy et al. 2001; Pfefferbaum et al. 2001; Chanraud et al. 2010). Alterations of the PFC in ethanol-withdrawn animals produced deficits in spatial working memory (WM), a task that depends on the functional integrity of the PFC and its interaction with the hippocampus (HPC) (Beracochea et al. 1987; George et al. 2012).
A prime mechanism that could underlie the actions of CAC and alcohol withdrawal on PFC cognitive function is dysregulation of cAMP-dependent events based on animal (Szabo et al. 1988; Dar, 1997; Meng et al. 1998) and clinical studies (Tabakoff and Hoffman 1988). Alterations in cAMP-protein kinase A (PKA) activity and downstream cAMP-responsive element binding (CREB) phosphorylation have been observed in various brain regions during alcohol exposure and its withdrawal (for reviews, (Tabakoff and Hoffman 1988; Moonat et al. 2010). However, the regulation of activated/phosphorylated CREB (pCREB) by alcohol appeared to differ depending on the brain region examined. For example, in contrast to the HPC, ethanol withdrawal but not treatment decreased pCREB levels in cortical structures (Pandey et al. 1999, 2001; Bison and Crews 2003). Furthermore, prefrontal CREB function was affected to a greater extent in ethanol-treated adolescent mice than in adults whereas the opposite was seen in the HPC (Faria et al. 2008; Soares-Simi et al. 2013).
The ability of pCREB to initiate gene transcription is achieved via the recruitment of a coactivator which has intrinsic histone acetyltransferase (HAT) activity and can acetylate histones at promoters, resulting in chromatin relaxation and thus enabling gene expression (Chrivia et al. 1993). Histone acetylation has been implicated in activity-dependent gene expression in the HPC (for reviews, (Day and Sweatt 2011; Peixoto and Abel 2013) and the PFC (Bredy et al. 2007; Stafford et al. 2012; Sui et al. 2012; Wang et al. 2012). Reduced HAT activity and histone acetylation patterns in cortical and hippocampal structures have been shown to correlate with persistently altered behavior during withdrawal after CAC in rats (Pascual et al. 2011). Others studies suggested a role for histone acetylation in the development of anxiety-like behaviors and deficits in activity-regulated genes during abstinence (Pandey et al. 2008; Mizuo et al. 2012), as they were abolished after blockade of histone deacetylase (HDAC) activity (Arora et al. 2013; Moonat et al. 2013; You et al. 2014).
However, despite the aforementioned observations that support critical roles for CREB and histone acetylation in alcohol withdrawal-mediated memory deficits, the vast majority of these studies have focused on elucidating behavioral and molecular changes associated with short-term withdrawal periods but not of sustained withdrawal periods. In addition, it has not been directly tested whether WM deficits during alcohol withdrawal are potentially reversible through treatments that activate cAMP-PKA-CREB cascade in the PFC and/or the HPC. To address these questions, we exposed mice to a 6-month CAC period and assessed the effects of 1 week (1W) or 6 weeks (6W) withdrawal on WM and levels of pCREB and histone acetylation in these structures. We then examined the behavioral and molecular consequences of PKA activation, via systemic phosphodiesterase-IV inhibition by rolipram, in water and withdrawn mice. Finally, to identify specific contribution of PFC and HPC function, we studied whether direct infusion of PKA activator Sp-cAMPS into the PFC or the CA1 region of the dorsal HPC (dCA1) differentially influences WM performance in withdrawn mice.
Experimental procedures
Animals
Male C57/BL6 mice were purchased from Charles River (L’Arbresle, France) at 6 weeks of age. Upon arrival, they were group housed (20 mice) in standard laboratory cages until they were 10 months old. They were maintained in a temperature-controlled colony room (22 ± 1 °C) under a 12:12 light–dark cycle and given ad lib access to food and water or alcohol. Food pellets (Pietrement, France) were enriched with vitamin supplement to avoid nutritional disturbances. Two weeks before the experiments, the mice were housed individually and were daily handled (2 min/day) for 5 days before training. All experimental procedures were carried out during the light phase of the cycle. The experimental protocols were conducted in accordance with the European Communities Council Directive of 24 November 1986 (86/609/EEC) and approved by a local bioethical committee (N°A5012089).
Alcohol administration
The procedure has been described elsewhere (Celerier et al. 2000). At 4-month-old, mice were given as their sole source of liquid increasing concentration of ethanol solution (V/V) (Prochilab) as follows: 1st week, 4 %; 2nd week, 8 and 12 % for six consecutive months. At the end of this period, alcohol mice (n = 118) were randomly assigned to one of the two withdrawal conditions, under which ethanol was progressively replaced by water only at 1 week (n = 58) or 6 weeks (n = 60) before behavioral testing as follows: 8 % v/v for 3 days followed by 4 % v/v for 3 days, then water. The remaining alcohol mice (n = 16) have no restriction to alcohol access. Alcohol and withdrawn mice were compared to a water group constituted by mice having drunk water only (n = 71). Blood alcohol concentration (BAC) was determined using an EnzyChrom™ Ethanol Assay Kit (ECET-100, BioAssay Systems, Hayward, CA, USA).
Working memory task
The mice were trained on a sequential alternation task over a series of successive trials run in a T-maze as previously described (Beracochea et al. 1987; Pierard et al. 2006; Vandesquille et al. 2013). Indeed, to alternate over a series from trial to trial, animals have both to remember at a given N trial the choice made at the N − 1 trial, and to reset the interfering information (trials N − 2, N − 3,..), which is a main aspect of WM (Kesner 2005).
Training session
Animals were initially habituated to the T-maze and allocentric cues during two 10 min-free exploration sessions on two successive days. The mice were then subjected to a training phase [seven successive trials separated by 30-s inter-trial interval (ITI)] to familiarize them with the experimental procedure (opening and closing of doors and confinement into the arms). At the beginning of each trial, the mouse was placed in the start box for 30-s ITI delay. Then, the door was opened and the mouse was allowed to enter one of the goal arms, the door to that arm was closed, and the choice was recorded. After a 30-s confinement period into the chosen arm, the mouse was removed and placed back in the start box for a 2nd trial, identical to the first one. To avoid olfactory cues in the apparatus, visible traces of urine and feces were washed with water.
Test session
Mice were submitted 24 h later to same procedure but the ITI delay was increased to 90 s. An alternation response was considered each time the subject entered the arm opposite to the one visited on the immediately previous trial. Alternation rate was calculated taking into account the seven successive trials, and expressed in percentage relative to the maximal alternation rate of 100 % (obtained when the subject never returned into the same arm over two consecutive trials). The chosen arm and the time that elapsed between opening the door and the arrival to the end of the chosen arm were registered, allowing calculation of the mean choice latency. Following a 30-s confinement period in the chosen arm, the animal was removed and placed in the start box for a new trial. To dissociate memory deficit from an eventual progressive loss of motivation to alternate over the series, an 8th trial was added which was separated by a shorter ITI (5 s) from the 7th trial.
Immunohistochemistry
All mice were deeply anesthetized (Pentobarbital®, 40 mg/kg i.p.) and perfused transcardially with 4 % paraformaldehyde fixative. Coronal sections (50 µm) were taken using a vibratome (Leica) and processed for immunohistochemistry as described previously (Dagnas et al. 2013). The antibodies for phospho(ser133)CREB and acetylated histones H3 (lys9) and H4 (lys5,8,12,16) (Upstate Biotechnology, Lake placid, NY) were used. After washing with Tris buffer (0.1 M), the sections were incubated with biotinylated goat anti-rabbit IgG secondary antibodies (Jackson Immunoresearch) followed by an avidin-biotinylated horseradish peroxidase complex (Vectastain Elite kit, Vector Laboratories). The peroxidase reaction was visualized using diaminobenzidine tetrahydrochloride and hydrogen peroxide. Digital images of each side of the dorsal HPC (from bregma: −1.70 to −2.30 mm), ventral HPC (from bregma: from −2.80 to −3.08 mm) and PFC (from bregma: +1.98 to +1.50 mm), as defined by the mouse stereotaxic brain atlas of Franklin and Paxinos (1997), were captured at 10× magnification using an Olympus (BX50) and an imaging analysis system (Biocom Visiolab 2000, V4.50). At all stages, the experimenter was blind to the experimental groups. For each animal, three to four consecutive sections (every first section in each set of four 50 µm-sections) were examined bilaterally and the number of positive nuclei/mm2 was averaged to produce a mean.
Experimental designs
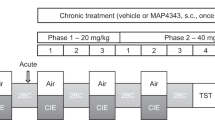
Experiment 1: effects of alcohol and alcohol withdrawal on WM-related changes in pCREB and histone acetylation in the PFC and the HPC
Experimental design is described in Fig. 1a. Cohorts of 10-month-old mice from the water (n = 11), alcohol (n = 10) and withdrawal 1W (n = 9) and 6W (n = 10) groups together with a 4-month-old cohort of mice (n = 7) were trained on a WM task. The 10-month-old mice were killed for immunohistochemistry 30 min after the beginning of the test session. An additional control naive group was sacrificed directly from their home cage (water: n = 10; alcohol: n = 6; withdrawal 1W: n = 8 and 6W: n = 7).
Alcohol withdrawal impairs WM in a long-delay alternation T-maze task. a Experimental design of the working memory testing session, in which mice from the water (n = 11), alcohol (n = 10), and withdrawal 1W (n = 9) and 6W (n = 10) groups were given seven successive trials separated by a 90-s inter-trial interval (ITI) followed by an additional trial with a 5-s ITI. b Alternation performance expressed as mean + SEM percentage of correct responses and c choice latencies expressed as mean time (in sec) to make arm choice were calculated during Trials 2–7 for each experimental condition. d Alternation performance on Trial 8th with 5-s ITI. Dashed lines for b and d represent chance level. Bars represent mean + SEM. **p < 0.01 vs. water. ## p < 0.01 and ### p < 0.001 vs. alcohol
Experiment 2: effects of systemic PKA activation on WM performance and levels of pCREB and histone acetylation in water and withdrawn mice
Rolipram (0.1 mg/kg/body weight; Sigma-Aldrich) was dissolved in 1 % DMSO (Zhang et al. 2000; Reneerkens et al. 2009). Thirty minutes before testing, water and withdrawal mice were randomly given a single i.p. injection of rolipram (water: n = 10; 1W: n = 8; 6W: n = 9) or vehicle (water: n = 9; 1W: n = 8; 6W: n = 8). All mice were killed 30 min after the beginning of WM testing for immunohistochemistry. Naive controls were treated identically except that they were sacrificed directly from their home cage for every conditions (vehicle: water: n = 6; 1W: n = 4; 6W: n = 4 and rolipram: water: n = 6; 1W: n = 4; 6W: n = 5).
Experiment 3: effect of bilateral intra-PFC or intra-dCA1, infusion of Sp-cAMPS on WM in withdrawn mice
Surgical procedure
Water and withdrawn mice were anesthetized with ketamine (100 mg/Kg; body weight, i.p.) and xylasine (10 mg/kg; body weight, i.p.) (Bayer, Wuppertal, Germany) and implanted bilaterally with guide cannulae (26 gauge, 8-mm length) above the PFC (anteroposterior +1.9 mm, lateral ±0.3 mm and depth 1.2 mm; relative to bregma) and the dCA1 (anteroposterior −2 mm, mediolateral ±1.4 mm, dorsoventral −0.9 mm; relative to bregma). Mice were allowed to recover for 2 weeks before WM testing. Water (n = 10) and withdrawal 1W and 6W (n = 9 for each) mice were infused 15 min before WM testing with the PKA activator Sp-cAMPS (Punch et al. 1997) (Sp-diastereomer of cAMP; Tocris Bioscience) into the PFC (0.1 µl/min for 2.5 min) or the dCA1 (0.1 µl/min for 5 min). The dose of Sp-cAMPS (1 µg/µl) was based on preliminary experiments (data not shown). Other mice (water: n = 9; 1W and 6W: n = 8 for each) received artificial cerebrospinal fluid (ACSF; vehicle) infusions. For each mouse, the same injection procedure was replicated 72 h later but the locus of injection was alternated, i.e. mice that had been infused into the PFC at the earlier time point were injected into the dCA1 and vice versa. The cannulae were left in place for an additional 1 min before removal to allow for diffusion. After WM testing, animals were sacrificed and cannulae placements were verified on 30-µm coronal sections stained with thionine blue coloration and visualized under an optical microscope.
Statistical analysis
Behavioral data were analyzed using three-way factorial analyses of variance (ANOVAs) to highlight between-groups differences and to determine the effect of treatment, when adequate, with post hoc comparisons. Comparisons of retrieval performances with chances level were calculated with one-sample t test (with hypothesized mean = chances level = 50 % for correct responses). Statistical analyses were performed using ANOVAs (StatView® statistical software) followed by appropriate post hoc tests set to reliability level of p < 0.05. For correlation analyses, the Spearman’s correlation coefficient, R, was determined and a probability level of p < 0.05 was accepted as statistically significant.
Results
Experiment 1: alcohol withdrawal was associated with impaired WM and reduced CREB phosphorylation and histone H4 acetylation in the PFC
Blood alcohol levels and cell death
In the present study, we subjected a cohort of 4-month-old mice to a regimen of 6-month CAC period and assessed behavioral and molecular changes induced by 1W or 6W withdrawal (Fig. 1a). When blood samples were taken just before the beginning of the memory test, very low levels of ethanol were detected in the blood of alcohol-treated mice (CAC: 0.58 ± 0.17 mg/dl; water: 0 ± 0 mg/dl). Moreover, upon thionin staining of the PFC, a weak neuronal cell death occurred in the alcohol (−5.75 % ± 3.09) and withdrawal 1W mice (−8.52 % ± 3.49) and no apparent neuronal loss was found in withdrawal 6W mice −0.89 % ± 1.59), compared with water controls. The results are in agreement with our previous observations using the same alcoholization procedure in Balb/c mice (Lescaudron et al. 1984; Beracochea et al. 1987).
Withdrawal effects on WM performance
Both water and alcohol animals alternated significantly above the chance level of 50 % (water: 75.76 ± 4.12 %; t(10) = 6.25; p < 0.001 and alcohol: 80.0 ± 6.48 %; t(9) = 4.63; p = 0.0012; Fig. 1b). The two groups did not differ from 4-month-old mice (69.04 ± 5.66 %; t(7) = 3.01; p = 0.018; data not shown. One-way ANOVA, group effect: F (2,25) = 0.88; p = 0.42), indicating that 10-month-old water and alcohol mice showed no WM deficits. By contrast, mice from withdrawal 1W and 6W groups responded at chance (1W: 50.0 ± 3.93 %; p = NS and 6W: 53.33 ± 4.84 %, p = NS). Analysis of variance yielded a significant between-groups difference (F (3,36) = 9.34; p < 0.001), with both withdrawal groups exhibiting lower alternation rates compared with water (both p < 0.01) and alcohol groups (1W: p < 0.001; 6W: p < 0.01). Further analyses per block of trials (Block A, trials 2–4 and Block B, trials 5–7) revealed a significant Block effect (F (1,36) = 4.64; p = 0.037, data not shown). Indeed, whereas no significant between-group differences were observed at Block A (F (1,36) = 1.02; p = NS), the Block B resulted in a significant impairment of alternation rates in the withdrawn groups (group effect (F (3,36) = 12.24; p < 0.001); vs. water and alcohol: p < 0.001 in all comparisons).
The WM deficits in withdrawn mice did not result from motivational or other factors unrelated to WM because the mean choice latency did not differ among the groups, whatever the factor considered (p > 0.05 in all comparisons; Fig. 1c). Moreover, all groups exhibited similar short-term alternation rates under 5-sec ITI delay condition (F (3,36) = 0.40; NS; Fig. 1d).
Withdrawal effects on CREB phosphorylation
We next determined the levels of pCREB in the PFC and the HPC (dCA1 and vCA1) of mice from the four experimental groups using immunohistochemistry. Animals were sacrificed 30 min after the end of the WM testing session. The results were expressed as percentage changes in pCREB levels relative to naive controls sacrificed just before testing (Fig. 2).
Effects of alcohol withdrawal on CREB phosphorylation in the PFC and the HPC. a Withdrawal 1W and 6W mice showed significantly lower pCREB levels in the PFC than water and alcohol mice after WM testing. b Representative 50-μm coronal sections of the PFC that show pCREB immunoreactivities in Naive controls (top) and in mice sacrificed 30 min after the beginning of WM testing (bottom) for the four experimental groups. c In the dCA1, water mice exhibited higher pCREB levels than both alcohol and withdrawal mice after WM testing. d There was no between-group difference in pCREB levels in the vCA1. The data represent mean ± SEM percentage of changes after WM testing relative to naive controls. e Summary of the mean number of positive pCREB nuclei per mm2 found in the PFC, dCA1 and vCA1 of the four experimental groups after WM testing. *p < 0.05, **p < 0.01 and ***p < 0.001 vs. water. # p < 0.05 vs. alcohol
In the PFC, pCREB levels were significantly increased after WM testing in the water and alcohol groups, but not the withdrawal groups, compared with respective naive controls (Fig. 2a, e). This observation was supported by a one-way ANOVA which yielded a significant between-group difference (F (3,36) = 5.79; p = 0.0024). Post hoc comparisons indicated significant differences between both water and alcohol groups and withdrawal 6W mice (both p < 0.01) as well as between water and withdrawal 1W groups (p < 0.05). Figure 2b shows representative pCREB immunoreactivity in the PFC for each of the experimental groups under naive (top) and trained (bottom) conditions.
In the dCA1, differential CREB activation was also observed after WM testing as a function of the group examined (Fig. 2c, e; ANOVA, F (3,36) = 4.658; p < 0.0075). Specifically, the water group displayed higher pCREB level after WM testing than respective naive controls (p < 0.001), whereas no training effects were observed in other groups (all p > 0.1). Levels of pCREB in the water group significantly differed from those of the withdrawal groups (1W and 6W: both p < 0.001), which otherwise did not differ from each other.
In the vCA1, there was no effect of WM testing on pCREB levels, whichever experimental group was considered (F (3,36) = 1.04; p = 0.38; Fig. 2d, e).
Effects of withdrawal on histone acetylation
We determined whether alcohol withdrawal after CAC produces changes in histone acetylation status in the PFC and the dHPC.
After WM testing, only the water group exhibited significant WM-related increase in Ac-H4 in the PFC (Fig. 3a left; ANOVA, significant between-group differences, F (3,36) = 6.78; p < 0.0001) and dCA1 (Fig. 3b left; ANOVA, significant between-group differences, F (3,36) = 6.15; p < 0.01). Post hoc analyses confirmed significantly higher Ac-H4 levels in the water vs. alcohol or withdrawn mice in the PFC (alcohol: p < 0.01; 1 and 6W: both p < 0.0001) and the dCA1 (alcohol: p < 0.05; 1 and 6W: both p < 0.01). In contrast, no between-group differences were found for Ac-H4 in the vCA1 (all F > 1; NS; data not shown).
Effects of alcohol withdrawal on histone acetylation in the PFC and the HPC. a, b After WM testing, the water mice showed greater levels of Ac-H4 than alcohol and withdrawal 1W and 6W mice in the PFC (a left) and the dCA1 (b left). In contrast, no changes in Ac-H3 were observed in the PFC and dCA1 (a, b right) in any of the experimental groups. The data represent mean ± SEM percentage of changes in Ac-H4 or Ac-H3 in mice sacrificed 30 min after the beginning of WM testing relative to respective naive controls. *p < 0.05, **p < 0.01 vs. water
No WM-related changes were detected for Ac-H3, irrespective of region and condition analyzed (Fig. 3, right).
Experiment 2: rolipram alleviates WM deficits and restores levels of pCREB and Ac-H4 in withdrawn mice
We next compared the effects of increasing CREB function on WM performance in water and withdrawn mice by administrating a single, i.p. injection of rolipram or vehicle 30 min before testing (Fig. 4a). As expected, performance during the test session was above chance level in the vehicle-water group (74.07 ± 4.04 %; t(8) = 5.96; p < 0.001) but not in vehicle-withdrawal groups (1W: 58.33 ± 5.45 %; t(7) = 1.53; p = 0.17; 6W: 54.17 ± 2.73 %; t(7) = 1.53; p = 0.17) (Fig. 4b). ANOVAs confirmed a significant between-groups difference (F (2,22) = 6.42; p = 0.006), alternation rates being significantly greater in water mice compared with withdrawn mice (p ≤ 0.01 in all comparisons). Systemic administration of rolipram improved performance in both withdrawal groups (1W: 75.0 ± 5.45 %; t(7) = 4.58; p = 0.0025; 6W: 79.63 ± 3.70 %; t(8) = 8.0; p < 0.001). Both rolipram-withdrawn groups showed much higher alternation rates than respective vehicle groups (1W: t(14) = 2.16; p < 0.05 and 6W: t(15) = 5.41; p < 0.001). In contrast, rolipram-water mice responded at chance (48.33 ± 3.89 %; t(9) = −0.43; NS). One-way ANOVA confirmed a significant between-group effect (F (2,24) = 16.22; p < 0.0001) with rolipram-water mice performing significantly worse than rolipram-withdrawn mice (p < 0.001 in both comparisons).
Systemic administration of rolipram reverses working memory impairments and rescues the deficits in pCREB and Ac-H4 in the PFC during alcohol withdrawal. a Experimental design. Thirty minutes before WM testing, mice from the water, withdrawal 1W and 6W groups received i.p. injection of rolipram (0.1 mg/kg) or vehicle. They were then submitted to WM testing and sacrificed 30 min later for pCREB and Ac-H4 immunohistochemistry. For comparison, rolipram- and vehicle-injected Naive mice that remained in the home cage were killed for immunohistochemistry. b Systemic rolipram had opposite effects on WM in water group (impairment) and withdrawal 1W and 6W groups (improvement). The data represent mean percentage of alternation performance during Trials 2–7 (90-s ITI). c Compared with vehicle, rolipram enhanced (water) or rescued to normal level (withdrawal 1W and 6W) pCREB (left) and Ac-H4 (right) immunoreactivities in the PFC of mice subjected to WM testing. d rolipram had no effect on pCREB (left) and Ac-H4 (right) immunoreactivities in the dCA1. The data represent mean ± SEM percentage of changes relative to respective naive controls. e, f Correlations between alternation performance and changes in pCREB after WM testing for the water (e; R = −0.42; p = 0.09) and withdrawal 6W (f; R = 0.82; p < 0.001) groups when all vehicle (open circles) and rolipram (black circles) mice were pooled together. p < 0.05, °° p < 0.01, °°° p < 0.001 vs. vehicle
No such effects were observed on the 8th trial of the test session (data not shown), indicating that withdrawal and/or treatment did not affect motivation to alternate during the testing session.
To test the region-specific effects of i.p. rolipram injection, we measured levels of pCREB and Ac-H4 in the PFC (Fig. 4c) and the dCA1 (Fig. 4d) of vehicle- and rolipram-treated groups killed 30 min after the beginning of the test session.
The ANOVAs for both pCREB and Ac-H4 data in the PFC revealed significant between-groups differences (pCREB: F (2,46) = 10.63; p < 0.001; Ac-H4: F (2,46) = 8.75; p < 0.001) as well as a significant “treatment” effect (pCREB: F (1,46) = 20.52; p < 0.001; Ac-H4: F (1,46) = 15.20; p < 0.001) without significant between-factors interaction (both F (2,46) < 1; both p: NS). Specifically, withdrawn mice exhibited significantly reduced pCREB and Ac-H4 levels relative to water mice, regardless of whether they were treated with vehicle (pCREB: all p < 0.05 except p: 0.078 for Ac-H4 in withdrawal 1W) or rolipram (all p < 0.01 except p < 0.05 for pCREB in withdrawal 6W). However, the factor “treatment” indicated significantly higher pCREB and Ac-H4 levels in rolipram vs. vehicle groups (all p < 0.05 except for Ac-H4 in withdrawal 1W: p = 0.06). In the dCA1 (Fig. 4d), there was a significant between-group difference for pCREB (F (2,46) = 13.79; p < 0.001) and Ac-H4: (F (2,46) = 8.88; p < 0.001) but no “treatment” or “factors interaction” effects (all F < 1; NS). Overall, these results suggest that improved or impaired WM performance in rolipram-treated mice arose from changes in pCREB and Ac-H4 specifically in the PFC.
Correlation analyses were applied to confirm relationships between individual WM performance and prefrontal pCREB levels in water and withdrawal groups. Overall, when vehicle- and rolipram-treated mice were pooled together, individual percent alternation rates correlated positively with pCREB levels in withdrawn mice (R = 0.57; p < 0.001) whereas a negative, non-significant, correlation was found between behavioral performance and pCREB in water mice (R = −0.42; p > 0.5; Fig. 4e). When each withdrawal group was considered separately, we found a strong positive correlation for withdrawal 6W mice (R = 0.82; p < 0.001; Fig. 4f), but not for 1W mice (R = 0.2; p > 0.5). In withdrawal 6W mice, there were also positive correlations between individual performance vs. Ac-H4 in the PFC (R = 0.673; p < 0.01) or between pCREB vs. Ac-H4 in the PFC (R = 0.6; p = 0.01). No such correlations were found in dCA1 region, providing more support for the hypothesis that prefrontal CREB plays a key role in alcohol withdrawal-related memory deficits.
Experiment 3: direct infusion of Sp-cAMPS into the PFC, but not dCA1, alleviates withdrawal-associated WM deficits
To complement the above findings, we next tested the effects of acutely increasing CREB activity into the PFC or the dCA1 on WM performance in water and withdrawal mice. To that aim, bilateral infusions of Sp-cAMPS or vehicle into either the PFC or dCA1 were performed 15 min before the test session (Fig. 5a). As expected, Fig. 5b shows that, when vehicle was infused into the PFC, water mice exhibited alternation rates that were significantly above chance (74.07 ± 4.90 %; t(8) = 4.92; p = 0.001) whereas withdrawn animals did not (1W: 47.92 ± 7.99 %; t(7) = −0.26; NS; 6W: 50.0 ± 5.45 %; t(7) = −0.001; NS). ANOVAs yielded a significant between-groups difference (F (2,22) = 5.76; p < 0.01), alternation rates being significantly greater in water mice compared with withdrawn mice (p ≤ 0.01 in all comparisons). In contrast, acute intra-PFC infusion of Sp-cAMPS improved performance in withdrawal groups (1W: 68.52 ± 4.34 %; t(8) = 4.26; p < 0.01; 72.22 ± 3.93 %; t(8) = 5.66; p < 0.001) but impaired performance in water group (51.66 ± 2.99 %; t(9) = 0.55; NS). This was confirmed by a significant between-group difference (F (2,25) = 8.82; p = 0.0013), with both Sp-cAMPS-withdrawal groups showing significantly higher percentage of alternation rates than Sp-cAMPS-water group (vs 1W: p < 0.01; vs 6W: p < 0.001). Here again, choice latencies did not significantly differ among the groups, whatever the factor considered (p > 0.5 in all comparisons; data not shown).
Acutely increasing cAMP-PKA-CREB in the PFC but not the dCA1 is sufficient to rescue withdrawal-associated WM deficits. Mice from the water, withdrawal 1W and 6W groups received acute, bilateral infusion of vehicle or the selective PKA activator Sp-cAMPS into the PFC (0.25 μg in 0.25 μl) or the dCA1 (0.5 μg in 0.5 μl) 15 min prior to WM testing. a Representative views of injection sites in the PFC (top) and the dCA1 (bottom) showing tracks of guide cannulae (arrows). b Compared with vehicle, Sp-cAMPS into the PFC impaired and improved working memory performance in water and withdrawal groups, respectively. c Sp-cAMPS into the dCA1 had no effect on working memory, in any of the groups examined. The data represent mean + SEM percentage of alternation performance during Trials 2–7 (90-s inter-trial interval). ° p < 0.05, °° p < 0.01, °°° p < 0.001 vs. vehicle
Intra-dCA1 infusion of Sp-cAMPS had no effect on WM performance in water and withdrawal groups (Fig. 5c). Water animals exhibited sequential alternation rates that were above chance level, regardless of whether they received vehicle (74.07 ± 2.93 %; t(8) = 8.22; p < 0.001) or Sp-cAMPS (71.67 ± 3.56 %; t(9) = 6.09; p < 0.001) whereas withdrawn mice responded at chance (vehicle 1W: 58.33 ± 5.45 %; t(7) = 1.53; NS; 6W: 56.25 ± 4.38 %; t(7) = 1.43; NS; Sp-cAMPS 1W: 44.44 ± 4.81 %; t(8) = −1.15; NS; 6W: 51.85 ± 6.48 %; t(8) = 0.29; NS). Whatever the treatments, performance was higher in water vs. withdrawn mice (all p < 0.05). Overall, the findings indicate that acutely enhancing PKA/CREB activity selectively in the PFC (but not the dCA1) is sufficient to rescue withdrawal-associated WM deficits.
Discussion
To sum up our findings, we have shown that alcohol withdrawal produces long-term WM impairments in a T-maze sequential alternation task that are associated with decreased CREB phosphorylation selectively in the PFC. The behavioral and molecular deficits appeared to be selectively related to alcohol withdrawal since no such changes were observed in CAC mice. In contrast, both CAC-unimpaired and withdrawn-impaired mice exhibited decreased pCREB level in the dCA1 as well as altered histone H4 acetylation in both structures, compared with water controls. Systemic administration of rolipram before WM testing was effective in either enhancing (in water mice) or rescuing to normal levels (in withdrawal mice) pCREB in the PFC, but did not affect the dCA1 region. Importantly, rolipram-induced increase in pCREB level in the PFC had bidirectional effects on spontaneous alternation performance in water (impairment) and withdrawal (improvement) groups. Finally, locally increasing cAMP-PKA activity into the PFC, but not dCA1, was sufficient to rescue withdrawal-related WM deficits, supporting a role for deregulated PKA/CREB signaling in mediating prefrontal cognitive declines during alcohol withdrawal.
Our data indicated that both short (1 week) or prolonged (6 weeks) alcohol withdrawal periods significantly impair WM performance (mainly on the three last trials) in the T-maze spontaneous alternation task whereas six months of alcohol consumption did not. The data confirmed previous results obtained in Balb/c strain mice indicating that WM deficits are observed after 12 months, but not 6 months, of CAC (Beracochea et al. 1987). The low alternation rates observed in withdrawn mice were not attributable to decreased motivation or capacity to alternate during trial series, as performances were not compromised when the ITI was shortened from 90 s to 5 s. Thus, the withdrawal-associated WM deficits resulted in increased vulnerability to delay-dependent proactive interference over a series. Both human and rodent studies have reported enhanced anxiety-like behaviors in various tests during ethanol withdrawal (for review, Kliethermes 2005). In our experimental conditions, increased anxiety in an elevated plus maze and in exploratory patterns in a 9-hole board was observed in withdrawn 1W mice that did not persist in withdrawn 6W mice (data not shown). Thus, the prolonged WM deficits seen in both withdrawn 1W and 6W mice cannot be the result of withdrawal-induced anxiety-like behavior but must be considered as particularly long-lasting impairments caused by CAC. Previous studies also demonstrated that alcohol withdrawal consistently potentiates memory deficits in spatial and non-spatial tasks induced by several weeks/months of CAC (Melis et al. 1996; Lukoyanov et al. 1999; Farr et al. 2005). Data from rodent studies on adaptive changes after prolonged ethanol exposure have suggested that cognitive deficits and development of neuronal damage during alcohol withdrawal are mediated, at least in part, through enhanced glutamatergic neurotransmission and excessive Ca2+ influx. Such imbalance particularly within the cortex and the HPC are believed to underlie withdrawal-induced seizure, neuronal cell loss and cognitive deficits in rodents and humans (For reviews, Ward et al. 2009; Prendergast and Mulholland 2012). Although we did not find any evidence of obvious neuronal cell loss in the PFC of withdrawn mice, considering the importance of glutamate in regulating PFC function and connectivity (Blot et al. 2013) it is conceivable that enhanced prefrontal glutamatergic activity during alcohol withdrawal contributes to impaired WM performance.
In withdrawn animals, WM impairments were associated with reduced pCREB levels in PFC and dCA1 regions whereas the CAC (unimpaired) mice showed reduced pCREB levels in the dCA1 only. Thus, the current results suggest that altered CREB phosphorylation specifically in the PFC is involved in the withdrawal-associated WM deficits. In this respect, decreased CREB phosphorylation and reduced expression of CREB target genes have been observed in cortical structures of ethanol-withdrawn rats (Pandey et al. 1999; 2001). Both alcohol and withdrawal groups displayed reduced dCA1 CREB phosphorylation compared with water controls, suggesting that altered hippocampal CREB function may contribute to behavioral deficits commonly observed during alcohol exposure and “early abstinence”. Indeed, anatomical and neurochemical changes occurring in the HPC during alcohol exposure are considered as major mechanism that underlie hippocampus-dependent spatial/contextual memory loss [for review, (Matthews and Morrow 2000)]. Moreover, repeated ethanol produced greater decreases in pCREB, CREB-DNA binding activity and CREB target gene expression in the HPC compared with the PFC (Faria et al. 2008, Soares-Simi et al. 2013). Importantly, our results indicated that CAC and its withdrawal affected specifically pCREB in the PFC and the dHPC, as no changes were found in the vCA1 region. These results fit well with current literature assigning a “cognitive” role for the dHPC and a more important implication of the vHPC in emotional behavior (Fanselow and Dong 2010; Segal et al. 2010).
Decreased histone acetylation, resulting from decreased CBP activity but increased HDAC activity, has been reported during withdrawal after chronic ethanol exposure (Pandey et al. 2008; Sakharkar et al. 2012) and these events have been associated with abnormal expression of plasticity/memory-related genes (Pandey et al. 2008; Qiang et al. 2011; Pascual et al. 2012). Here, we found that withdrawal after prolonged alcohol exposure robustly and selectively reduced the learning-related acetylation of H4, but not H3, in the PFC and dCA1, suggesting that altered H4 acetylation could be involved in mediating withdrawal-related WM deficits. Indeed, altered histone H4 acetylation in the dHPC has been implicated in impaired hippocampus-dependent contextual/spatial memories in mice (Peleg et al. 2010; Dagnas et al. 2013; Dagnas and Mons 2013) and rats (Bousiges et al. 2010; Zeng et al. 2011; Castellano et al. 2012). In our study, however, levels of Ac-H4 were also reduced in the PFC and the dCA1 of alcohol-treated mice. The data suggest that altered H4 acetylation in the PFC and dHPC may be related to adaptive changes that develop with CAC. Indeed, previous studies showed that chronic alcohol exposure leads to widespread changes in brain gene expression both in humans and animal models (Pandey et al. 2008; Qiang et al. 2011; Pascual et al. 2012; Ponomarev et al. 2012), and many of these gene expression changes including genes critical in neural transmission and related brain functions were involved in homeostatic adaptation in multiple regions of the brain that contribute to alcohol dependence (Mayfield et al. 2008; Zhou et al. 2011). Future studies will provide important insight regarding the contribution of epigenetic regulatory changes on gene networks involved in alcohol tolerance and dependence in our CAC model.
In the second experiment, we tested whether withdrawal-associated WM impairments could be rescued by restoration of prefrontal CREB function through i.p. injection of the specific phosphodiesterase-IV inhibitor rolipram prior to testing session. We found that rolipram bidirectionally influenced WM performances in water (impairment) and withdrawal (improvement) groups. In addition, rolipram was effective in either enhancing (in water mice) or rescuing to normal levels (in withdrawal mice) pCREB in the PFC, but not the dCA1 region. These results strongly suggest that an optimal window of PKA-CREB activation selectively in the PFC is necessary for normal WM function. Consistently, WM impairment or improvement in aged mice also depends on the level (reduction or over-expression) of pCREB in the PFC but not the dCA1 (Vandesquille et al. 2013). In agreement with our observation that rolipram-impaired WM in water mice with intact CREB function, we and others have shown that aberrant and sustained activation of cAMP-PKA signaling can lead to cognitive deficiencies (Belanoff et al. 2002; Ramos et al. 2003; Giralt et al. 2011). For instance, desinhibition of cAMP/PKA signaling exacerbated prefrontal cognitive deficits in aged animals and infusion of drugs that enhance prefrontal CREB activity worsened WM in young-adults (Ramos et al. 2003; Runyan and Dash 2005; Vandesquille et al. 2013). Remarkably, rolipram also reversed the deficits in prefrontal Ac-H4 in withdrawn mice, while having no effect in the dCA1 region. Moreover, the increases in pCREB and Ac-H4 in the PFC correlated positively with enhanced WM performance in rolipram-withdrawal mice, suggesting that CREB and H4 acetylation are parts of the same withdrawal-sensitive signaling cascade which contributes to disruption of PFC functioning. A mechanism has been proposed in which CBP, when recruited by CREB, modulates both ethanol and cocaine-associated behaviors through increased acetylation of histones and up-regulation of genes such as c-fos and NPY (Pandey et al. 2008; Malvaez et al. 2011). Future studies will be aimed at examining the changes in CREB target genes attributable to altered H4 acetylation in the PFC and other regions during CAC and alcohol withdrawal.
Using direct intra-PFC or intra-dCA1 infusion of the PKA activator Sp-cAMPS before testing, we confirmed that local PKA activation occurring selectively in the PFC is sufficient to reverse WM deficits in withdrawal mice but impairs WM in water mice. Furthermore, activating hippocampal PKA activity had no effect on WM performance both in withdrawn and water animals. Together, these findings not only demonstrate that alcohol withdrawal after CAC did not affect the PFC and dHPC functioning in the same manner but also strengthened the role of PFC-specific cAMP-PKA-CREB signaling cascade in mediating the observed withdrawal-associated WM impairments.
In conclusion, our data provide direct evidence that WM deficits during alcohol withdrawal correlated with deficiencies in CREB phosphorylation and H4 acetylation specifically in the PFC. The results further revealed that systemic or direct intra-PFC activation of cAMP-PKA pathway, by normalizing the reductions in both pCREB and Ac-H4 in the PFC, improved WM performance during alcohol withdrawal. These findings may have important implications for the development of effective strategies aimed at preventing the deleterious impact of withdrawal on PFC-dependent cognitive function and delayed neurobiological alterations.
References
Arora DS, Nimitvilai S, Teppen TL, McElvain MA, Sakharkar AJ, You C, Pandey SC, Brodie MS (2013) Hyposensitivity to gamma-aminobutyric acid in the ventral tegmental area during alcohol withdrawal: reversal by histone deacetylase inhibitors. Neuropsychopharmacology 38:1674–1684
Belanoff JK, Jurik J, Schatzberg LD, DeBattista C, Schatzberg AF (2002) Slowing the progression of cognitive decline in Alzheimer’s disease using mifepristone. J Mol Neurosci 19:201–206
Beracochea D, Lescaudron L, Tako A, Verna A, Jaffard R (1987) Build-up and release from proactive interference during chronic ethanol consumption in mice: a behavioral and neuroanatomical study. Behav Brain Res 25:63–74
Bison S, Crews F (2003) Alcohol withdrawal increases neuropeptide Y immunoreactivity in rat brain. Alcohol Clin Exp Res 27:1173–1183
Blot K, Kimura SI, Bai J, Kemp A, Manahan-Vaughan D, Giros B, Tzavara E, Otani S (2013) Modulation of hippocampus-prefrontal cortex synaptic transmission and disruption of executive cognitive functions by MK-801. Cereb Cortex
Bousiges O, Vasconcelos AP, Neidl R, Cosquer B, Herbeaux K, Panteleeva I, Loeffler JP, Cassel JC, Boutillier AL (2010) Spatial memory consolidation is associated with induction of several lysine-acetyltransferase (histone acetyltransferase) expression levels and H2B/H4 acetylation-dependent transcriptional events in the rat hippocampus. Neuropsychopharmacology 35:2521–2537
Bredy TW, Wu H, Crego C, Zellhoefer J, Sun YE, Barad M (2007) Histone modifications around individual BDNF gene promoters in prefrontal cortex are associated with extinction of conditioned fear. Learn Mem 14:268–276
Castellano JF, Fletcher BR, Kelley-Bell B, Kim DH, Gallagher M, Rapp PR (2012) Age-related memory impairment is associated with disrupted multivariate epigenetic coordination in the hippocampus. PLoS One 7:e33249
Celerier A, Ognard R, Decorte L, Beracochea D (2000) Deficits of spatial and non-spatial memory and of auditory fear conditioning following anterior thalamic lesions in mice: comparison with chronic alcohol consumption. Eur J Neurosci 12:2575–2584
Chanraud S, Pitel AL, Rohlfing T, Pfefferbaum A, Sullivan EV (2010) Dual tasking and working memory in alcoholism: relation to frontocerebellar circuitry. Neuropsychopharmacology 35:1868–1878
Chrivia JC, Kwok RP, Lamb N, Hagiwara M, Montminy MR, Goodman RH (1993) Phosphorylated CREB binds specifically to the nuclear protein CBP. Nature 365:855–859
Dagnas M, Guillou JL, Prevot T, Mons N (2013) HDAC inhibition facilitates the switch between memory systems in young but not aged mice. J Neurosci 33:1954–1963
Dagnas M, Mons N (2013) Region- and age-specific patterns of histone acetylation related to spatial and cued learning in the water maze. Hippocampus 23:581–591
Dar MS (1997) Mouse cerebellar adenosinergic modulation of ethanol-induced motor incoordination: possible involvement of cAMP. Brain Res 749:263–274
Day JJ, Sweatt JD (2011) Cognitive neuroepigenetics: a role for epigenetic mechanisms in learning and memory. Neurobiol Learn Mem 96:2–12
Errico AL, King AC, Lovallo WR, Parsons OA (2002) Cortisol dysregulation and cognitive impairment in abstinent male alcoholics. Alcohol Clin Exp Res 26:1198–1204
Fanselow MS, Dong HW (2010) Are the dorsal and ventral hippocampus functionally distinct structures? Neuron 65:7–19
Faria RR, Lima Rueda AV, Sayuri C, Soares SL, Malta MB, Carrara-Nascimento PF, da Silva Alves A, Marcourakis T, Yonamine M, Scavone C, Giorgetti Britto LR, Camarini R (2008) Environmental modulation of ethanol-induced locomotor activity: correlation with neuronal activity in distinct brain regions of adolescent and adult Swiss mice. Brain Res 1239:127–140
Farr SA, Scherrer JF, Banks WA, Flood JF, Morley JE (2005) Chronic ethanol consumption impairs learning and memory after cessation of ethanol. Alcohol Clin Exp Res 29:971–982
Franklin KBJ, Paxinos G (1997) The mouse brain in stereotaxic coordinates. Academic Press, San Diego
George O, Sanders C, Freiling J, Grigoryan E, Vu S, Allen CD, Crawford E, Mandyam CD, Koob GF (2012) Recruitment of medial prefrontal cortex neurons during alcohol withdrawal predicts cognitive impairment and excessive alcohol drinking. Proc Natl Acad Sci USA 109:18156–18161
Giralt A, Saavedra A, Carreton O, Xifro X, Alberch J, Perez-Navarro E (2011) Increased PKA signaling disrupts recognition memory and spatial memory: role in Huntington’s disease. Hum Mol Genet 20:4232–4247
Kesner RP (2005) Temporal processing of information: the role of the medial prefrontal cortex and hippocampus: theoretical comment on Gilmartin and McEchron. Behav Neurosci 119:1705–1709
Kliethermes CL (2005) Anxiety-like behaviors following chronic ethanol exposure. Neurosci Biobehav Rev 28:837–850
Lescaudron L, Beracochea D, Verna A, Jaffard R (1984) Chronic ethanol consumption induces neuronal loss in mammillary bodies of the mouse: a quantitative analysis. Neurosci Lett 150:151–155
Lukoyanov NV, Madeira MD, Paula-Barbosa MM (1999) Behavioral and neuroanatomical consequences of chronic ethanol intake and withdrawal. Physiol Behav 66:337–346
Malvaez M, Mhillaj E, Matheos DP, Palmery M, Wood MA (2011) CBP in the nucleus accumbens regulates cocaine-induced histone acetylation and is critical for cocaine-associated behaviors. J Neurosci 31:16941–16948
Matthews DB, Morrow AL (2000) Effects of acute and chronic ethanol exposure on spatial cognitive processing and hippocampal function in the rat. Hippocampus 10:122–130
Mayfield RD, Harris RA, Schuckit MA (2008) Genetic factors influencing alcohol dependence. Br J Pharmacol 154:275–287
Melis F, Stancampiano R, Imperato A, Carta G, Fadda F (1996) Chronic ethanol consumption in rats: correlation between memory performance and hippocampal acetylcholine release in vivo. Neuroscience 74:155–159
Meng ZH, Pennington SN, Dar MS (1998) Rat striatal adenosinergic modulation of ethanol-induced motor impairment: possible role of striatal cyclic AMP. Neuroscience 85:919–930
Mizuo K, Katada R, Okazaki S, Tateda K, Watanabe S, Matsumoto H (2012) Epigenetic regulation of MIR-124 under ethanol dependence and withdrawal. Nihon Arukoru Yakubutsu Igakkai Zasshi 47:155–163
Moonat S, Sakharkar AJ, Zhang H, Tang L, Pandey SC (2013) Aberrant histone deacetylase2-mediated histone modifications and synaptic plasticity in the amygdala predisposes to anxiety and alcoholism. Biol Psychiatry 73:763–773
Moonat S, Starkman BG, Sakharkar A, Pandey SC (2010) Neuroscience of alcoholism: molecular and cellular mechanisms. Cell Mol Life Sci 67:73–88
Moselhy HF, Georgiou G, Kahn A (2001) Frontal lobe changes in alcoholism: a review of the literature. Alcohol Alcohol 36:357–368
Pandey SC, Roy A, Mittal N (2001) Effects of chronic ethanol intake and its withdrawal on the expression and phosphorylation of the creb gene transcription factor in rat cortex. J Pharmacol Exp Ther 296:857–868
Pandey SC, Ugale R, Zhang H, Tang L, Prakash A (2008) Brain chromatin remodeling: a novel mechanism of alcoholism. J Neurosci 28:3729–3737
Pandey SC, Zhang D, Mittal N, Nayyar D (1999) Potential role of the gene transcription factor cyclic AMP-responsive element binding protein in ethanol withdrawal-related anxiety. J Pharmacol Exp Ther 288:866–878
Pascual M, Do Couto BR, Alfonso-Loeches S, Aguilar MA, Rodriguez-Arias M, Guerri C (2012) Changes in histone acetylation in the prefrontal cortex of ethanol-exposed adolescent rats are associated with ethanol-induced place conditioning. Neuropharmacology 62:2309–2319
Pascual M, Fernandez-Lizarbe S, Guerri C (2011) Role of TLR4 in ethanol effects on innate and adaptive immune responses in peritoneal macrophages. Immunol Cell Biol 89:716–727
Peixoto L, Abel T (2013) The role of histone acetylation in memory formation and cognitive impairments. Neuropsychopharmacology 38:62–76
Peleg S, Sananbenesi F, Zovoilis A, Burkhardt S, Bahari-Javan S, Agis-Balboa RC, Cota P, Wittnam JL, Gogol-Doering A, Opitz L, Salinas-Riester G, Dettenhofer M, Kang H, Farinelli L, Chen W, Fischer A (2010) Altered histone acetylation is associated with age-dependent memory impairment in mice. Science 328:753–756
Pfefferbaum A, Desmond JE, Galloway C, Menon V, Glover GH, Sullivan EV (2001) Reorganization of frontal systems used by alcoholics for spatial working memory: an fMRI study. Neuroimage 14:7–20
Pierard C, Liscia P, Valleau M, Drouet I, Chauveau F, Huart B, Bonneau D, Jouanin JC, Beaumont M, Beracochea D (2006) Modafinil-induced modulation of working memory and plasma corticosterone in chronically-stressed mice. Pharmacol Biochem Behav 83:1–8
Ponomarev I, Wang S, Zhang L, Harris RA, Mayfield RD (2012) Gene coexpression networks in human brain identify epigenetic modifications in alcohol dependence. J Neurosci 32:1884–1897
Prendergast MA, Mulholland PJ (2012) Glucocorticoid and polyamine interactions in the plasticity of glutamatergic synapses that contribute to ethanol-associated dependence and neuronal injury. Addict Biol 17:209–223
Punch LJ, Self DW, Nestler EJ, Taylor JR (1997) Opposite modulation of opiate withdrawal behaviors on microinfusion of a protein kinase A inhibitor versus activator into the locus coeruleus or periaqueductal gray. J Neurosci 17:8520–8527
Qiang M, Denny A, Lieu M, Carreon S, Li J (2011) Histone H3K9 modifications are a local chromatin event involved in ethanol-induced neuroadaptation of the NR2B gene. Epigenetics 6:1095–1104
Ramos BP, Birnbaum SG, Lindenmayer I, Newton SS, Duman RS, Arnsten AF (2003) Dysregulation of protein kinase a signaling in the aged prefrontal cortex: new strategy for treating age-related cognitive decline. Neuron 40:835–845
Reneerkens OA, Rutten K, Steinbusch HW, Blokland A, Prickaerts J (2009) Selective phosphodiesterase inhibitors: a promising target for cognition enhancement. Psychopharmacology 202:419–443
Runyan JD, Dash PK (2005) Distinct prefrontal molecular mechanisms for information storage lasting seconds versus minutes. Learn Mem 12:232–238
Sakharkar AJ, Zhang H, Tang L, Shi G, Pandey SC (2012) Histone deacetylases (HDAC)-induced histone modifications in the amygdala: a role in rapid tolerance to the anxiolytic effects of ethanol. Alcohol Clin Exp Res 36:61–71
Segal M, Richter-Levin G, Maggio N (2010) Stress-induced dynamic routing of hippocampal connectivity: a hypothesis. Hippocampus 20:1332–1338
Soares-Simi SL, Pastrello DM, Ferreira ZS, Yonamine M, Marcourakis T, Scavone C, Camarini R (2013) Changes in CREB activation in the prefrontal cortex and hippocampus blunt ethanol-induced behavioral sensitization in adolescent mice. Front Integr Neurosci 7:94
Stafford JM, Raybuck JD, Ryabinin AE, Lattal KM (2012) Increasing histone acetylation in the hippocampus-infralimbic network enhances fear extinction. Biol Psychiatry 72:25–33
Sui L, Wang Y, Ju LH, Chen M (2012) Epigenetic regulation of reelin and brain-derived neurotrophic factor genes in long-term potentiation in rat medial prefrontal cortex. Neurobiol Learn Mem 97:425–440
Szabo G, Hoffman PL, Tabakoff B (1988) Forskolin promotes the development of ethanol tolerance in 6-hydroxydopamine-treated mice. Life Sci 42:615–621
Tabakoff B, Hoffman PL (1988) Genetics and biological markers of risk for alcoholism. Public Health Rep 103:690–698
Vandesquille M, Baudonnat M, Decorte L, Louis C, Lestage P, Beracochea D (2013) Working memory deficits and related disinhibition of the cAMP/PKA/CREB are alleviated by prefrontal alpha4beta2*-nAChRs stimulation in aged mice. Neurobiol Aging 34:1599–1609
Voltaire-Carlsson A, Hiltunen AJ, Koechling UM, Borg S (1996) Effects of long-term abstinence on psychological functioning: a prospective longitudinal analysis comparing alcohol-dependent patients and healthy volunteers. Alcohol 13:415–421
Wang WS, Kang S, Liu WT, Li M, Liu Y, Yu C, Chen J, Chi ZQ, He L, Liu JG (2012) Extinction of aversive memories associated with morphine withdrawal requires ERK-mediated epigenetic regulation of brain-derived neurotrophic factor transcription in the rat ventromedial prefrontal cortex. J Neurosci 32:13763–13775
Ward RJ, Lallemand F, de Witte P (2009) Biochemical and neurotransmitter changes implicated in alcohol-induced brain damage in chronic or ‘binge drinking’ alcohol abuse. Alcohol Alcohol 44:128–135
Watanabe KI, Ogihara-Hashizume A, Kobayashi Y, Mitsushio H, Komiyama T (2001) Impaired sleep during the post-alcohol withdrawal period in alcoholic patients. Addict Biol 6:163–169
You C, Zhang H, Sakharkar AJ, Teppen T, Pandey SC (2014) Reversal of deficits in dendritic spines, BDNF and Arc expression in the amygdala during alcohol dependence by HDAC inhibitor treatment. Int J Neuropsychopharmacol 17:313–322
Zeng Y, Tan M, Kohyama J, Sneddon M, Watson JB, Sun YE, Xie CW (2011) Epigenetic enhancement of BDNF signaling rescues synaptic plasticity in aging. J Neurosci 31:17800–17810
Zhang HT, Crissman AM, Dorairaj NR, Chandler LJ, O’Donnell JM (2000) Inhibition of cyclic AMP phosphodiesterase (PDE4) reverses memory deficits associated with NMDA receptor antagonism. Neuropsychopharmacology 23:198–204
Zhou Z, Yuan Q, Mash DC, Goldman D (2011) Substance-specific and shared transcription and epigenetic changes in the human hippocampus chronically exposed to cocaine and alcohol. Proc Natl Acad Sci USA 108:6626–6631
Acknowledgments
This study was supported by the Centre National de la Recherche Scientifique and IREB (Institut de Recherches Scientifiques sur les Boissons).
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
D. Béracochéa and N. Mons contributed equally to this study.
Rights and permissions
About this article
Cite this article
Dominguez, G., Dagnas, M., Decorte, L. et al. Rescuing prefrontal cAMP-CREB pathway reverses working memory deficits during withdrawal from prolonged alcohol exposure. Brain Struct Funct 221, 865–877 (2016). https://doi.org/10.1007/s00429-014-0941-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00429-014-0941-3