Abstract
We compared the characteristics, clinical behavior, and biomarker profile between HER2 positive (HER2+) and triple-negative (TN) ductal carcinoma in situ (DCIS) which are considered more aggressive than other DCIS subtypes. In addition, we explored the impact of these features on its potential of progression to invasive breast carcinomas. Cases of DCIS diagnosed at the Department of Pathology, Singapore General Hospital from 1994 to 2010 were identified. TN and HER2+ DCIS cases formed the study cohort. Immunohistochemistry (IHC) was performed for ER, PR, HER2, CK14, EGFR, and p53. Comparisons of clinicopathological features, IHC results, and clinical outcomes were performed between the two groups. We evaluated 145 HER2+ and 85 TN DCIS cases. HER2 positive DCIS had significantly higher nuclear grade (p < 0.001) and more frequent necrosis (p < 0.001) than TN DCIS. HER2 positive DCIS also harbored significantly higher rates of nuclear p53 immunoreactivity (p = 0.002) than TN DCIS. Younger patients (age < 40) with HER2+ and TN DCIS demonstrated statistically significant worse invasive DFS than older women (p < 0.001). Multivariate cox regression analysis (HR 15.08, 95% CI 12.79–81.45, p = 0.002) also confirmed these findings. In addition, younger patients (age < 40) with HER2+ DCIS experienced significantly poorer prognosis when p53 was also positive (p = 0.033). HER2+ DCIS had more aggressive pathological characteristics compared to TN DCIS; accumulation of mutant p53 could possibly be contributory. Age was an independent predictor of aggressive biological behavior of HER2+ and TN DCIS. We demonstrated that younger patients with p53 positive HER2+ DCIS had significantly adverse clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ductal carcinoma in situ (DCIS) is a heterogeneous disease arising from the terminal duct lobular unit, composed of a clonal proliferation and accumulation of malignant breast epithelial cells within the lobule [1]. DCIS is also considered a non-obligate precursor of invasive breast carcinoma [2,3,4] and numerous studies have been reported in this regard [5,6,7]. DCIS is primarily classified based on its nuclear grade, while in terms of molecular expression, it could be divided according to the status of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) in carcinoma cells, akin to invasive breast cancer [8].
Molecular subtyping by immunohistochemistry (IHC) surrogates could generally classify breast cancer into four broad categories—namely, Luminal A, Luminal B, HER2 positive (HER2+) type, and triple-negative (TN). Breast cancers that fall under the non-luminal categories (HER2+ and TN) tend to have a less favorable prognosis compared to luminal breast cancers [9], although one study [10] reported that long-term survival at 15 years was poorest for patients with luminal HER2+ breast cancer.
HER2+ DCIS may be defined by an overexpression of the HER2 receptor and the lack of hormonal receptors [11]. HER2 positivity has been reported to be generally associated with a significantly higher risk of recurrence [12,13,14,15]. Recently, Mustafa et al. described HER2+ DCIS to have significantly higher rates of upstaging to invasive breast carcinoma than HER2- DCIS [16]. Similarly, HER2 status in invasive breast carcinoma is also considered a significant predictor of prognosis [17,18,19].
In contrast, TN DCIS is characterized by the lack of ER, PR, and HER2 receptors. TN invasive breast carcinoma has more aggressive clinical behavior, distinctive metastatic patterns, and poorer prognosis than other subtypes [20,21,22,23]. However, few studies have characterized the biological behavior and biomarker profiles of TN DCIS to date [24,25,26]. TN DCIS can also develop into invasive disease [27, 28]. A previous study established TN DCIS (basal-like) as a precursor of the corresponding invasive counterpart [29] but much has still remained unknown at this juncture.
We previously compared clinicopathological parameters, IHC characteristics, and clinical outcomes of screen-detected and symptomatic DCIS, which included 145 HER2+ and 85 TN DCIS cases out of 1202 DCIS cases [30]. Therefore, in this study, we compared the clinical and biological characteristics, behavior, and biomarker profiles in these two subtypes of DCIS derived from our previous cohort.
Materials and methods
Patients
Two hundred and thirty cases of HER2+ and TN DCIS were evaluated in this study. All the cases were diagnosed at the Department of Pathology, Singapore General Hospital (SGH) from 1994 to 2010. Clinical and pathological findings including age, ethnicity, screen-detected/symptomatic, laterality, tumor size, nuclear grade, necrosis, microinvasion, and morphological subtypes were retrieved from pathology records. Nuclear grade was categorized as low, intermediate, or high based on the degree of nuclear pleomorphism [31]. Microinvasion was defined as the presence of invasion not exceeding 1 mm in extent [31]. Morphological subtypes were classified into comedo, cribriform, papillary, solid, and mixed groups.
Immunohistochemistry
Archival formalin-fixed paraffin-embedded (FFPE) tissue blocks were retrieved. Four-micrometer tissue sections were cut from the FFPE blocks and placed onto positively charged Bond Plus glass slides (Leica Biosystems, Inc., Richmond, IL, USA). These slides were incubated in an oven overnight at 80 °C to increase adhesion of the sections to the slides. Antibodies to ER, PR, HER2 (c-erbB2), CK14, epidermal growth factor receptor (EGFR), and p53 were applied to the sections. Details of the antibodies and dilution were summarized in Table 1. An appropriate positive control was run with each immunostaining batch, and specificity was confirmed in these controls.
Nuclear ER, PR, and p53 immunoreactivity, cytoplasmic membranous HER2 and EGFR immunoreactivity, and cytoplasmic CK14 immunoreactivity were assessed. The relative immunointensity and percentage of positively stained tumor cells were recorded. The relative immunointensity was categorized as 0, 1+, 2+, and 3+, denoting no staining, weak, moderate, and strong staining, respectively [32]. For ER, PR, CK14, and EGFR, a positive result was defined by the presence of at least 1% of tumor cells displaying positive staining [33]. For HER2, positive expression was defined as > 10% of tumor cells exhibiting 3+ membrane staining [34].
Molecular subtypes of DCIS were classified, based on IHC status of receptors, as Luminal A (ER+, and/or PR+, HER2−), Luminal B (ER+, and/or PR+, HER2+), triple-negative (ER−, PR−, HER2−), and HER2 type (ER−, PR−, and HER2+), adapted from Carey et al.’s classification in 2006 [9]. Although Ki-67 is also used to differentiate between Luminal A and B according to the 2011 St Gallen classification [11], only ER, PR, and HER2 were applied for the purposes of this study.
Follow-up
Follow-up data were obtained from clinical charts. Recurrences included in situ and invasive local relapses. Events were categorized as ipsilateral DCIS recurrence, contralateral DCIS occurrence, ipsilateral invasive recurrence, and contralateral invasive occurrence. Disease-free survival (DFS) was defined overall as time from the date of diagnosis to the date of ipsilateral in situ or invasive recurrence, or to the date of last follow-up [35]. We used the terms in situ and invasive DFS to refer to the period from diagnosis of DCIS to ipsilateral in situ and ipsilateral invasive disease recurrence respectively.
Statistical analysis
Results were analyzed using SPSS for Windows, Version 18 (SPSS, Inc., Chicago, IL, USA). χ2 and Fisher’s exact tests were used to evaluate the relationship of clinicopathological characteristics between HER2+ and TN DCIS. Survival outcomes were evaluated using the Kaplan-Meier estimator and compared by the log-rank test. Multivariate cox regression analysis (adjusted for age, tumor size, and grade) was performed to examine the impact of the characteristics of DCIS on survival outcomes. A p value of < 0.05 defined statistical significance.
Results
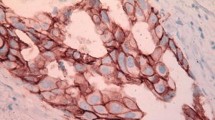
Among 230 DCIS cases in our study cohort, 145 were HER2+ and 85 cases TN DCIS. Results of comparison of clinicopathological characteristics between TN and HER2+ DCIS were summarized in Table 2 with the IHC illustrations in Fig. 1. HER2+ DCIS was more likely to be symptomatic than TN DCIS although this difference did not reach statistical significance (p = 0.062). HER2+ DCIS was more frequently detected in the left than right breast (p = 0.024). HER2+ DCIS had statistically significantly higher nuclear grade (p < 0.001) and more frequently harbored foci of necrosis (p < 0.001) than TN DCIS. However, there were no other differences in the remaining clinicopathological parameters between HER2+ and TN DCIS.
We evaluated the expression of CK14, EGFR, and p53 in this study and results were summarized in Table 3. The patterns of IHC expression of these biomarkers were also illustrated in Fig. 2. The status of CK14 and EGFR was not significantly different between HER2+ and TN DCIS (p = 0.972 and p = 0.342 respectively). However, HER2+ DCIS had significantly higher rates of mutant p53 positivity than TN DCIS (p = 0.002).
Patient follow-up ranged from 4 to 229 months (mean and median 101 months). One hundred and forty-seven (63.9%) women underwent breast conserving surgery, while the remaining 83 (36.1%) had mastectomy. Twenty-eight patients (12.2%) developed a subsequent breast cancer; 17 (7.4%) were in situ, and 11 (4.8%) were invasive. Details were summarized in Table 4. There were no significant differences between HER2+ and TN DCIS with regard to subsequent occurrence of breast cancer. There was a trend for more favorable ipsilateral invasive DFS (p = 0.082) in patients who underwent a mastectomy than those who had breast conserving surgery, although the difference was not statistically significant. Adjusting the multivariate analysis for surgical treatment did not yield any statistical significance (p = 0.234, HR 3.09, 95% CI 0.48–19.85). Five- and ten-year DFS were summarized in Table 5. A total of three patients died, but none were due to breast cancer.
In the entire study cohort (N = 230), younger patients (age < 40) with HER2+ and TN DCIS harbored significantly unfavorable invasive DFS (p < 0.001) (Fig. 3a). This was subsequently confirmed by multivariate cox regression analysis (p = 0.002, HR = 15.08, 95% CI 2.79–81.45).
Survival analysis in whole series, TN series, and HER2 positive series. a In the whole series, younger patients (age < 40) had significantly poorer invasive DFS than older patients. Multivariate cox regression analysis confirmed this finding (p = 0.002, HR = 15.08, 95% CI 2.79–81.45). b In TN DCIS, younger patients (age < 40) also had significantly poorer invasive DFS. This was also confirmed by multivariate cox regression analysis (p = 0.009, HR = 30.40, 95% CI 2.34–395.45). c In the HER2 positive cohort, younger patients (age < 40) disclosed a trend for unfavorable invasive DFS. d Also, in the HER2 positive DCIS series, younger patients (age < 40) with p53 positivity had significantly poorer prognosis (invasive DFS) compared to other patients. Multivariate cox regression analysis affirmed this finding (p = 0.011, HR = 23.48, 95% CI 2.08–264.83)
In TN DCIS, younger patients (age < 40) also had significantly poorer invasive DFS than older ones (p < 0.001) (Fig. 3b). This finding was subsequently confirmed by multivariate cox regression analysis (p = 0.009, HR = 30.34, 95% CI 2.34–395.45).
In HER2+ DCIS, younger patients showed a trend for unfavorable invasive DFS than older ones (p = 0.078) (Fig. 3c). Of particular interest, also within the HER2+ DCIS cohort, younger patients with p53 positive DCIS had significantly poorer DFS (p = 0.033) (Fig. 3d), which was subsequently confirmed by multivariate analysis (p = 0.011, HR = 23.48, 95% CI 2.08–264.83). All survival analyses shown were performed with ipsilateral invasive recurrences or the last follow-up as the endpoint. Analyses with in situ recurrences or a combination of in situ and invasive recurrences did not yield any statistically significant results.
Discussion
We previously compared characteristics and behavior of screen-detected and symptomatic DCIS in a large series diagnosed at our institution [30], including 7.6% of TN and 12.9% of HER2 phenotypes, both of which were more commonly observed in symptomatic disease. In this study, we found that women with the HER2 DCIS phenotype harbored higher nuclear grade and necrosis, as well as more frequently expressed p53 protein when compared to TN DCIS.
The association of nuclear grade with HER2+ or HER2 amplified DCIS has been previously reported [15, 36]. Van Bockstal and colleagues [36] found that 63.0% of their HER2 amplified DCIS cases were high grade, compared to 22.0% of non-HER2 amplified DCIS (p < 0.001). Similarly, Di Cesare et al. [15] also reported a significant association between HER2+ DCIS and high nuclear grade (p = 0.001). High nuclear grade has been well known as an indicator for poorer prognosis, including higher risk for local recurrence and progression to invasive disease compared to low nuclear grade DCIS [15, 37,38,39]. Therefore, this suggests that patients with HER2+ DCIS could be at a higher risk for recurrent disease.
Consistent with our findings regarding the presence of necrosis, the same study by Van Bockstal [36] also found extensive comedo necrosis to be independently associated with HER2 amplified DCIS. As it is with high nuclear grade, necrosis, especially comedo necrosis, is another factor that has been found to correlate with an increased risk of local recurrence [39, 40], which therefore could hint at a poorer prognosis for these particular groups of patients.
On IHC, we found that a higher proportion of HER2+ DCIS expressed p53 compared to TN DCIS. Kaplan-Meier analyses also revealed that younger women with DCIS harboring p53 protein expression displayed an independent risk of developing ipsilateral invasive disease among HER2 DCIS cases. In line with our findings, a study investigating the expression of p53 in DCIS by Kikuchi and colleagues [41] found a significant association between the overexpression of p53 and HER2 positivity (p < 0.0001).
The p53 gene is well known to function as a tumor suppressor, and aberrations in its expression have been implicated in many cancers. Although wild-type p53 can diminish or even eliminate the tumorigenic potential of normal cells, the presence of excessive mutant p53 protein could hamper this function. p53 protein abnormalities can exist at the in situ phase and are present throughout the stages of breast cancer progression from in situ to invasive disease and/or metastatic disease [42]. Overexpression of p53 is also considered an indicator of higher risk of recurrence in invasive breast cancers [43, 44]. Recently, there has been renewed interest in mutant p53 as a potential therapeutic target in cancer via reactivation of wild-type transcriptional function of mutant p53 or restoration of its native protein structure or activity [45]. The p53 gene product regulates a wide range of biological functions, including DNA repair, cell cycle progression, differentiation, cell proliferation, and cell death [46, 47]. Studies of interactions and the prognostic value of the relationship between HER2 and p53 in DCIS lesions are potentially attractive research areas as there are scant data concerning the accumulation of mutant p53 protein in DCIS lesions. Both HER2 and p53 protein expression can be routinely established in the laboratory for identification of high risk patients with pure DCIS for appropriate treatment strategies.
In our present study, we were unable to determine if HER2+ or TN DCIS could better predict disease progression. In our previous study, 870 (77.3%) DCIS cases were ER positive [30]. Among these, 27 (3.1%) had an ipsilateral invasive recurrence. Although we were not able to establish any association between the different molecular types and recurrence risk, the rate of ipsilateral invasive recurrence among luminal DCIS (3.1%) was also comparable to non-luminal DCIS in this study (3%, Table 4). The reasons are uncertain, and may be related to sample size. However, we were able to demonstrate that younger women (age < 40 years) with HER2+ or TN DCIS in the entire cohort, as well as only among the TN cases, disclosed poorer invasive DFS. Younger age has been shown to be associated with a higher risk of local recurrence for patients with DCIS [48, 49]. In Singapore, while the National Breast Screening program targets women aged 50 years and above, it is to be noted that DCIS in younger patients are more commonly symptomatic, and therefore more aggressive with poorer prognosis [30].
In our series, 5-year invasive DFS rate in the TN cohort was slightly lower than that of the HER2+ phenotype (72.9 vs 75.2% respectively). However, after 10 years of follow-up, the difference in the invasive DFS rate of patients with HER2+ DCIS became greater when compared to that of patients with TN DCIS (27.6 vs 34.1% respectively). This suggests that TN DCIS appears to progress to invasive carcinoma at a faster rate than HER2+ DCIS initially, but that in the long run, the proportion of HER2+ DCIS that eventually upstages from in situ to invasive carcinoma exceeds TN DCIS. In his review, Kurbel [28] calculated the relative t1/2 durations (time needed for 50.0% of DCIS to become invasive) using simulated probabilities of tumor progression in a modeled population of DCIS and invasive breast cancers and disclosed that TN DCIS cases had the fastest tumor progression among all subtypes. In fact, its rate of progression was three times that of HER2+ tumors and nearly twice that of luminal A tumors. However, it is to be noted that the number of cases that progressed from DCIS to invasive carcinoma in our cohort is very limited, and a larger cohort would be helpful in validating this finding.
Other studies have proposed that HER2 overexpression in DCIS is of major importance for tumor progression toward invasive cancer [12, 50, 51]. Roses et al. [50], Harada et al. [51], and Liao et al. [12] all reported that HER2 overexpression or positivity was significantly associated with DCIS that harbored invasive foci compared to DCIS without. This suggests that HER2 overexpression could indicate or predict the presence of invasive disease and potentially identify patients at risk of developing invasive cancer.
Additionally, there were reports of HER2 overexpression being associated with tumor cell migration, expression of proangiogenic factors and cyclooxygenase-2 (COX-2), suggesting a potentially significant role in inducing invasion, or the elaboration of a stroma that supports tumor growth [52, 53]. All these factors favor the importance of recognizing HER2+ DCIS as a high-risk factor.
In summary, our present study demonstrated that HER2+ DCIS had more aggressive pathological characteristics than TN DCIS. Younger women (age < 40 years) have poorer invasive DFS and increased risk of upstaging in the whole series as well as among TN cases. Younger age together with p53 expression independently predicted disease progression in HER2+ DCIS. Therefore, age at diagnosis, HER2 overexpression, triple negativity, and accumulation of mutant p53 were all considered important in identifying those at higher risk of developing invasive cancer and tailoring the management of DCIS lesions. Currently, there is no widely accepted molecular panel to separate DCIS lesions into those with low risk or high risk for subsequent development of recurrence, with or without invasive progression. Our study may lend insights into promising panels of markers for identifying high-risk patients with DCIS.
References
Tan PH (2001) Pathology of ductal carcinoma in situ of the breast: a heterogeneous entity in need of greater understanding. Ann Acad Med Singap 30:671–676 quiz 677
Sanders ME, Schuyler PA, Dupont WD, Page DL (2005) The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer 103:2481–2484. https://doi.org/10.1002/cncr.21069
Boughey JC, Gonzalez RJ, Bonner E, Kuerer HM (2007) Current treatment and clinical trial developments for ductal carcinoma in situ of the breast. Oncologist 12:1276–1287. https://doi.org/10.1634/theoncologist.12-11-1276
Cowell CF, Weigelt B, Sakr RA, Ng CKY, Hicks J, King TA, Reis-Filho JS (2013) Progression from ductal carcinoma in situ to invasive breast cancer: revisited. Mol Oncol 7:859–869. https://doi.org/10.1016/j.molonc.2013.07.005
Williams KE, Barnes NLP, Cramer A, Johnson R, Cheema K, Morris J, Howe M, Bundred NJ (2015) Molecular phenotypes of DCIS predict overall and invasive recurrence. Ann Oncol 26:1019–1025. https://doi.org/10.1093/annonc/mdv062
Buerger H, Otterbach F, Simon R, Schäfer KL, Poremba C, Diallo R, Brinkschmidt C, Dockhorn-Dworniczak B, Boecker W (1999) Different genetic pathways in the evolution of invasive breast cancer are associated with distinct morphological subtypes. J Pathol 189:521–526. https://doi.org/10.1002/(SICI)1096-9896(199912)189:4<521::AID-PATH472>3.0.CO;2-B
Buerger H, Otterbach F, Simon R, Poremba C, Diallo R, Decker T, Riethdorf L, Brinkschmidt C, Dockhorn-Dworniczak B, Boecker W (1999) Comparative genomic hybridization of ductal carcinoma in situ of the breast-evidence of multiple genetic pathways. J Pathol 187:396–402. https://doi.org/10.1002/(SICI)1096-9896(199903)187:4<396::AID-PATH286>3.0.CO;2-L
Zhou W, Jirström K, Amini R-M, Fjällskog ML, Sollie T, Lindman H, Sørlie T, Blomqvist C, Wärnberg F (2013) Molecular subtypes in ductal carcinoma in situ of the breast and their relation to prognosis: a population-based cohort study. BMC Cancer 13:512. https://doi.org/10.1186/1471-2407-13-512
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MCU, Nielsen TO, Moorman PG, Earp HS, Millikan RC (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502. https://doi.org/10.1001/jama.295.21.2492
Blows FM, Driver KE, Schmidt MK, Broeks A, van Leeuwen FE, Wesseling J, Cheang MC, Gelmon K, Nielsen TO, Blomqvist C, Heikkilä P, Heikkinen T, Nevanlinna H, Akslen LA, Bégin LR, Foulkes WD, Couch FJ, Wang X, Cafourek V, Olson JE, Baglietto L, Giles GG, Severi G, McLean CA, Southey MC, Rakha E, Green AR, Ellis IO, Sherman ME, Lissowska J, Anderson WF, Cox A, Cross SS, Reed MWR, Provenzano E, Dawson SJ, Dunning AM, Humphreys M, Easton DF, García-Closas M, Caldas C, Pharoah PD, Huntsman D (2010) Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med 7:e1000279. https://doi.org/10.1371/journal.pmed.1000279
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, Panel members (2011) Strategies for subtypes--dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747. https://doi.org/10.1093/annonc/mdr304
Liao N, Zhang G, Liu Y, Li XR, Yao M, Xu FP, Li L, Wu YL (2011) HER2-positive status is an independent predictor for coexisting invasion of ductal carcinoma in situ of the breast presenting extensive DCIS component. Pathol Res Pract 207:1–7. https://doi.org/10.1016/j.prp.2010.08.005
Curigliano G, Disalvatore D, Esposito A, Pruneri G, Lazzeroni M, Guerrieri-Gonzaga A, Luini A, Orecchia R, Goldhirsch A, Rotmensz N, Bonanni B, Viale G (2015) Risk of subsequent in situ and invasive breast cancer in human epidermal growth factor receptor 2-positive ductal carcinoma in situ. Ann Oncol 26:682–687. https://doi.org/10.1093/annonc/mdv013
Nofech-Mozes S, Spayne J, Rakovitch E, Kahn HJ, Seth A, Pignol JP, Lickley L, Paszat L, Hanna W (2008) Biological markers predictive of invasive recurrence in DCIS. Clin Med Oncol 2:7–18
Di Cesare P, Pavesi L, Villani L et al (2017) The relationships between HER2 overexpression and DCIS characteristics. Breast J 23:307–314. https://doi.org/10.1111/tbj.12735
Mustafa RE, DeStefano LM, Bahng J et al (2017) Evaluating the risk of upstaging HER2-positive DCIS to invasive breast cancer. Ann Surg Oncol 24:2999–3003. https://doi.org/10.1245/s10434-017-5941-0
Cheang MCU, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS, Perou CM, Ellis MJ, Nielsen TO (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750. https://doi.org/10.1093/jnci/djp082
Muñoz M, Fernández-Aceñero MJ, Martín S, Schneider J (2009) Prognostic significance of molecular classification of breast invasive ductal carcinoma. Arch Gynecol Obstet 280:43–48. https://doi.org/10.1007/s00404-008-0867-1
Caldarella A, Crocetti E, Bianchi S, Vezzosi V, Urso C, Biancalani M, Zappa M (2011) Female breast cancer status according to ER, PR and HER2 expression: a population based analysis. Pathol Oncol Res 17:753–758. https://doi.org/10.1007/s12253-011-9381-z
Nielsen TO, Hsu FD, Jensen K et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5374. https://doi.org/10.1158/1078-0432.CCR-04-0220
Fulford LG, Reis-Filho JS, Ryder K, Jones C, Gillett CE, Hanby A, Easton D, Lakhani SR (2007) Basal-like grade III invasive ductal carcinoma of the breast: patterns of metastasis and long-term survival. Breast Cancer Res 9:R4. https://doi.org/10.1186/bcr1636
Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, Hess KR, Stec J, Ayers M, Wagner P, Morandi P, Fan C, Rabiul I, Ross JS, Hortobagyi GN, Pusztai L (2005) Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res 11:5678–5685. https://doi.org/10.1158/1078-0432.CCR-04-2421
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, Ollila DW, Sartor CI, Graham ML, Perou CM (2007) The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 13:2329–2334. https://doi.org/10.1158/1078-0432.CCR-06-1109
Zhou W, Jirström K, Johansson C, Amini RM, Blomqvist C, Agbaje O, Wärnberg F (2010) Long-term survival of women with basal-like ductal carcinoma in situ of the breast: a population-based cohort study. BMC Cancer 10:653. https://doi.org/10.1186/1471-2407-10-653
Bryan BB, Schnitt SJ, Collins LC (2006) Ductal carcinoma in situ with basal-like phenotype: a possible precursor to invasive basal-like breast cancer. Mod Pathol 19:617–621. https://doi.org/10.1038/modpathol.3800570
Sarode VR, Han JS, Morris DH, Peng Y, Rao R (2011) A comparative analysis of biomarker expression and molecular subtypes of pure ductal carcinoma in situ and invasive breast carcinoma by image analysis: relationship of the subtypes with histologic grade, Ki67, p53 overexpression, and DNA ploidy. Int J Breast Cancer 2011:217060–217067. https://doi.org/10.4061/2011/217060
Ishikawa Y, Horiguchi J, Toya H, Nakajima H, Hayashi M, Tagaya N, Takeyoshi I, Oyama T (2011) Triple-negative breast cancer: histological subtypes and immunohistochemical and clinicopathological features. Cancer Sci 102:656–662. https://doi.org/10.1111/j.1349-7006.2011.01858.x
Kurbel S (2013) In search of triple-negative DCIS: tumor-type dependent model of breast cancer progression from DCIS to the invasive cancer. Tumour Biol 34:1–7. https://doi.org/10.1007/s13277-012-0602-1
Thike AA, Iqbal J, Cheok PY et al (2013) Ductal carcinoma in situ associated with triple negative invasive breast cancer: evidence for a precursor-product relationship. J Clin Pathol 66:665–670. https://doi.org/10.1136/jclinpath-2012-201428
Koh VCY, Lim JCT, Thike AA et al (2015) Characteristics and behaviour of screen-detected ductal carcinoma in situ of the breast: comparison with symptomatic patients. Breast Cancer Res Treat 152:293–304. https://doi.org/10.1007/s10549-015-3472-6
Lakhani SR, Ellis IO, Schnitt SJ, et al (2012) WHO classification of tumours of the breast, 4th ed. IARC, Lyon
Thike AA, Cheok PY, Jara-Lazaro AR et al (2010) Triple-negative breast cancer: clinicopathological characteristics and relationship with basal-like breast cancer. Mod Pathol 23:123–133. https://doi.org/10.1038/modpathol.2009.145
Allred DC, Harvey JM, Berardo M, Clark GM (1998) Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol 11:155–168
Wolff AC, Hammond MEH, Hicks DG et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31:3997–4013. https://doi.org/10.1200/JCO.2013.50.9984
Thike AA, Iqbal J, Cheok PY et al (2010) Triple negative breast cancer: outcome correlation with immunohistochemical detection of basal markers. Am J Surg Pathol 34:956–964. https://doi.org/10.1097/PAS.0b013e3181e02f45
Van Bockstal M, Lambein K, Denys H et al (2014) Histopathological characterization of ductal carcinoma in situ (DCIS) of the breast according to HER2 amplification status and molecular subtype. Virchows Arch 465:275–289. https://doi.org/10.1007/s00428-014-1609-3
Evans AJ, Pinder SE, Ellis IO, Wilson AR (2001) Screen detected ductal carcinoma in situ (DCIS): overdiagnosis or an obligate precursor of invasive disease? J Med Screen 8:149–151. https://doi.org/10.1136/jms.8.3.149
Roka S, Rudas M, Taucher S et al (2004) High nuclear grade and negative estrogen receptor are significant risk factors for recurrence in DCIS. Eur J Surg Oncol 30:243–247. https://doi.org/10.1016/j.ejso.2003.11.004
Shamliyan T, Wang S-Y, Virnig BA et al (2010) Association between patient and tumor characteristics with clinical outcomes in women with ductal carcinoma in situ. J Natl Cancer Inst Monogr 2010:121–129. https://doi.org/10.1093/jncimonographs/lgq034
Bijker N, Peterse JL, Duchateau L et al (2001) Risk factors for recurrence and metastasis after breast-conserving therapy for ductal carcinoma-in-situ: analysis of European Organization for Research and Treatment of Cancer Trial 10853. J Clin Oncol 19:2263–2271. https://doi.org/10.1200/JCO.2001.19.8.2263
Kikuchi S, Osako T, Nishiyama Y et al (2014) P53 overexpression in ductal carcinoma in situ of the breast. J Cytol Histol 5. https://doi.org/10.4172/2157-7099.1000269
Rajan PB, Scott DJ, Perry RH, Griffith CD (1997) p53 protein expression in ductal carcinoma in situ (DCIS) of the breast. Breast Cancer Res Treat 42:283–290
Jasar D, Smichkoska S, Kubelka K et al (2015) Expression of p53 protein product in triple negative breast cancers and relation with clinical and histopathological parameters. Pril (Makedon Akad Na Nauk Umet Oddelenie Za Med Nauki) 36:69–79
de Roos MA, de Bock GH, de Vries J et al (2007) p53 overexpression is a predictor of local recurrence after treatment for both in situ and invasive ductal carcinoma of the breast. J Surg Res 140:109–114. https://doi.org/10.1016/j.jss.2006.10.045
Muller PAJ, Vousden KH (2013) p53 mutations in cancer. Nat Cell Biol 15:2–8. https://doi.org/10.1038/ncb2641
Vogelstein B, Lane D, Levine AJ (2000) Surfing the p53 network. Nature 408:307–310. https://doi.org/10.1038/35042675
Oren M (2003) Decision making by p53: life, death and cancer. Cell Death Differ 10:431–442. https://doi.org/10.1038/sj.cdd.4401183
Vicini FA, Shaitelman S, Wilkinson JB et al (2013) Long-term impact of young age at diagnosis on treatment outcome and patterns of failure in patients with ductal carcinoma in situ treated with breast-conserving therapy. Breast J 19:365–373. https://doi.org/10.1111/tbj.12127
Kong I, Narod SA, Taylor C et al (2014) Age at diagnosis predicts local recurrence in women treated with breast-conserving surgery and postoperative radiation therapy for ductal carcinoma in situ: a population-based outcomes analysis. Curr Oncol 21:e96–e104. https://doi.org/10.3747/co.21.1604
Roses RE, Paulson EC, Sharma A et al (2009) HER-2/neu overexpression as a predictor for the transition from in situ to invasive breast cancer. Cancer Epidemiol Biomark Prev 18:1386–1389. https://doi.org/10.1158/1055-9965.EPI-08-1101
Harada S, Mick R, Roses RE et al (2011) The significance of HER-2/neu receptor positivity and immunophenotype in ductal carcinoma in situ with early invasive disease. J Surg Oncol 104:458–465. https://doi.org/10.1002/jso.21973
Wolf-Yadlin A, Kumar N, Zhang Y et al (2006) Effects of HER2 overexpression on cell signaling networks governing proliferation and migration. Mol Syst Biol 2:54. https://doi.org/10.1038/msb4100094
Subbaramaiah K, Howe LR, Port ER et al (2006) HER-2/neu status is a determinant of mammary aromatase activity in vivo: evidence for a cyclooxygenase-2-dependent mechanism. Cancer Res 66:5504–5511. https://doi.org/10.1158/0008-5472.CAN-05-4076
Acknowledgements
Satoshi Takahashi is a medical student intern on an elective posting from Tohoku University, Sendai, Japan.
Contributions
ST took part in the study design, analyzed the data, and wrote the manuscript. AAT took part in the study design, collected the clinicopathological data, evaluated the IHC stains, analyzed the data, and edited the manuscript. VCYK performed the experiments (tissue sectioning and IHC staining), assisted in data collection, and critically revised the manuscript. HS contributed substantially to the study design and critically reviewed and edited the manuscript. PHT conceived the study and critically reviewed and revised the manuscript. All authors gave final approval for publication.
Funding
This study was funded by the Health Services Research Competitive Research Grant, HSRG/0009/2010, from the Ministry of Health, Singapore.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This is a retrospective study involving human FFPE tissues and has been approved by the SingHealth Centralised Institutional Review Board (CIRB) (Ref: 2010/610/F). This article does not contain any studies with animals performed by any of the authors. A waiver for informed consent was approved by the SingHealth CIRB.
Conflict of interest
The authors declare that they no conflict of interest.
Rights and permissions
About this article
Cite this article
Takahashi, S., Thike, A.A., Koh, V.C.Y. et al. Triple-negative and HER2 positive ductal carcinoma in situ of the breast: characteristics, behavior, and biomarker profile. Virchows Arch 473, 275–283 (2018). https://doi.org/10.1007/s00428-018-2416-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-018-2416-z