Abstract
The purpose of this study is to evaluate whether activating mutations of the p110α catalytic subunit of class A phosphoinositide 3-kinases (PI3KCA) or complete loss of phosphatase and tensin homolog (PTEN) is associated with response to anti-human epidermal growth factor receptor 2 (Her2) treatment in breast cancer (BC). We analysed PI3KCA hot-spot mutations and PTEN immunohistochemical expression in 129 Her2-positive infiltrating BC treated with trastuzumab, including 26 cases treated with neoadjuvant therapy, 48 metastatic infiltrating breast cancer (IBC; MBC) and 55 early-stage IBC, with complete clinical information (mean follow-up 37, 66 and 32 months, respectively). PI3KCA hot-spot mutations were observed in 25 cases (19 %): 12 (9 %) in exon 9 and 13 (10 %) in exon 20. No correlations were observed between mutations and pathological and biological parameters. In patients treated with neoadjuvant therapy and in MBC, we did not observe any relationship with response to trastuzumab-based therapy. PTEN loss was observed in 24 out of 86 informative cases (28 %), 3 (13 %) of which were also mutated for PI3KCA. PI3K pathway activation, defined as PI3KCA mutation and/or PTEN loss, was not associated with response to treatment or clinical outcome in MBC. PI3KCA mutation and/or PTEN loss should not exclude patients from potentially beneficial anti-Her2 therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human epidermal growth factor receptor 2 (Her2) is a tyrosine kinase receptor, which is overexpressed or amplified in 20 to 25 % of infiltrating breast carcinomas (IBC), which may behave more aggressively. Her2 overexpression may lead to increased receptor homo/heterodimerization, which induces phosphorylation of the intracellular domain, leading in turn to activation of many downstream signalling molecules, including class A phosphoinositide 3-kinases (PI3K)/AKT. Activated PI3K catalyzes the phosphorylation of inositol lipids to produce phosphatidylinositol-3,4,5-trisphosphate (PIP3), which in turn, as a negative feedback mechanism, is dephosphorylated to PIP2 by phosphatase and tensin homolog (PTEN). PIP3 activates the serine/threonine kinase AKT which in turn phosphorylates and regulates the mammalian target of rapamycin (mTOR).
Trastuzumab, a humanized monoclonal antibody targeting the extracellular domain of Her2, has good therapeutic efficacy in patients with Her2-positive IBC. Trastuzumab is effective in neoadjuvant therapy, in cases of metastatic breast cancer (MBC) and in the adjuvant setting in early-stage IBC. However, not all patients benefit from trastuzumab-based therapy, and a relevant percentage shows an initial resistance to trastuzumab.
The underlying antitumoural mechanisms of trastuzumab are complex and not completely understood [1]. The hypothesized mechanisms include inhibition of Her2 homo/heterodimerization, Her2 endocytosis and degradation or reduced shedding of the extracelluar domain, leading to downregulation of downstream signalling through the PI3K–AKT pathway. An alternative mechanism of action could be related to the fact that trastuzumab, being an intact monoclonal antibody, may recruit Fc-competent immune effector cells and the other components of antibody-dependent cell-mediated cytotoxicity, leading to tumour cell death [2].
Several lines of evidence suggest that Her2-independent activation of the PI3K–AKT pathway may be related to resistance to trastuzumab [3–5]. Aberrations of the components of the PI3K–AKT pathway are frequent in IBC, including activating mutations of the p110α catalytic subunit of PI3K (PI3KCA) and PTEN loss, which have been described in 9 to 45 % of cases [6–17] and 4 to 28 % of cases [18–21], respectively. The vast majority of PIK3CA mutations, comprising approximately 90 % of cases, are clustered at two hot-spot regions in exon 9 (E542K and E545K) and exon 20 (H1047R and H1047L) encoding the helical and kinase domains, respectively [6–17]. PI3KCA mutations are among the most common genetic aberrations in human IBC and have generally been reported as more frequent in node-negative [8, 17], estrogen receptor (ER)-positive and Her2-negative IBC [8–10, 14, 22–24], but data are not consistent. Controversies exist also concerning the prognostic value of PI3KCA mutations: most authors report favourable relation with survival [9, 10, 25, 26] but again data are not consistent [14, 27, 28] probably due to the heterogeneity of the investigated series and to possible different pathogenetic significance of mutations occurring at different sites in the molecule [7]. PI3KCA mutations have also been indicated as possible markers for poor response to trastuzumab [21, 27–29], but data are still not conclusive [5, 27, 30, 31]. Preclinical studies also suggest that the PI3KCA gene could be a target for new drugs [32] suggesting the possibility to combine anti-Her2 therapy with different inhibitors targeting PI3K, TORC1, AKT or EGFR [33, 34].
In the present study, we analyse PI3KCA mutations at hot-spots in exon 9 and exon 20 and PTEN expression in a retrospective series of Her2-positive IBC treated with trastuzumab (26 cases treated with neoadjuvant therapy, 48 metastatic IBC and 55 early-stage IBC), investigating their frequency and their relationship with clinical and pathological parameters and response to trastuzumab treatment.
Material and methods
Patients and tumour samples
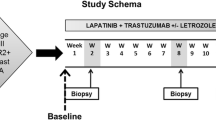
We retrospectively evaluated 129 Her2-positive IBC which had been treated with trastuzumab at the Santa Chiara Hospital of Trento Italy between 2000 and 2010. The study has been approved by the ethical committee of the Santa Chiara Hospital. The investigated cases include three groups of patients: 26 primary IBC treated with neoadjuvant trastuzumab therapy, 48 advanced MBC and 55 early-stage IBC treated with adjuvant therapy. Complete follow-up information was available for all cases; mean follow-up was 37, 66 and 32 months for the above three groups of patients. Neoadjuvant therapy consisted of doxorubicin and trastuzumab for three courses followed by paclitaxel and trastuzumab for 4 cycles followed by cyclophosphamide, methotrexate, fluorouracil associated with trastuzumab (according to NOAH trial regimen). In MBC patients, the first-line therapy consisted of trastuzumab associated with taxanes (weekly paclitaxel or docetaxel). All early-stage IBC patients received adjuvant trastuzumab for 1 year after surgery. All patients showing positive estrogen receptors also received hormonal therapy with tamoxifen ± ovarian ablation if in pre-menopausal status and with aromatase inhibitors if in post-menopausal status. All cases were reviewed by a pathologist (MB). For each case, one representative tissue block was selected for further analyses. The percentage of tumour cells in each block was visually estimated, and only cases with more that 50 % of tumour cell content were included in the study.
For patients affected by primary IBC treated with neoadjuvant trastuzumab, pathological response at surgery was scored as: (a) complete, if no invasive residual disease in breast and axilla was found, (b) partial, if the residual tumour burden was inferior to the clinically estimated tumour diameter and (c) absent, if the residual tumour burden was identical or higher than the clinically estimated tumour diameter (stable or progressive disease). For MBC, response to therapy was evaluated clinically. The different pathological characteristics of the whole group of cases are shown in Table 1, and the characteristics of the three different series are illustrated in Tables 2, 3 and 4.
Her2 immunoreactivity was evaluated using the HercepTest kit (DakoCytomation, Glostrup, Denmark) according to the manufacturer’s FDA-approved procedures, using manual or computer-assisted assessment [35]. All cases with Her2 score 2+ were further investigated with fluorescent in situ hybridization using the HER2 FISH pharmDx™ kit (DakoCytomation). Tumours with a HER2/Cep17 ratio ≥2.2 were considered as amplified.
In all cases, ER, progesterone receptor (PgR) and Ki67 were evaluated using 6 F11 (Leica, Novocastra, Newcastle, UK), Pgr636 (DakoCytomation) and MIB1 (Leica, Novocastra) antibodies, respectively [36]. Ki67 labelling index was evaluated manually in the peripheral areas of all tumours. In case of marked heterogeneity, Ki67 labelling was also evaluated using computer-assisted image analysis [37]. Cases with at least 1 % reactive cells were considered positive for ER and PgR. Ki67 labelling was scored as high if at least 25 % reactive cells were counted. A subset of 34 cases out of the series of advanced MBC and 52 out of 55 cases treated with adjuvant therapy were immunostained for PTEN, using the 138G6 antibody (Cell Signaling Technology, Celbio, Italy). PTEN immunohistochemistry was scored as absent (complete PTEN loss) when no immunostaining was observed in spite of positive internal controls, or positive, if any degree of cytoplasmic and nuclear staining was observed. In 14 cases, PTEN could not be evaluated because of lack of available histological samples or inadequate internal control immunostaining.
Mutational analysis
Sample DNA extraction
Five 10-μm sections were cut from each paraffin-embedded tumour block. Slides were deparaffinized twice with 1 mL of xylene, vortexed and centrifuged. The supernatant was removed and then washed with 1 mL absolute ethanol. The samples were resuspended in 180 μl lysis buffer containing 20 μl proteinase K. DNA was isolated with the Qiamp DNA mini-kit (Qiagen, Valencia, CA) and was incubated overnight at 56 °C at 300 rpm.
Real-time polymerase chain reaction amplification
Briefly, DNA fragments were amplified using RT-PCR with primers specific for exon 9 and exon 20 of the PI3KCA gene, designed to allow the identification of the following mutations: E542K, E545K and Q546K in exon 9 and M1043I, H1047R, H1047L, G1049S and G1049R in exon 20 (Diatech Pharmacogenetics, Jesi, Italy). Each mix contained 5× buffer Mg2+-free, 50 mM Mg2+ solution, 10 mM of each dNTP, 1 μl of specific primers, EvaGreen dye (20× in water), 5 U/μl Hot Star Taq DNA Polymerase and 100 ng genomic DNA in a 50-μl final volume. The mixture was denatured for 3 min at 95 °C and underwent 40 cycles: at 95 °C for 20 s, at 57 °C for 30 s and at 72 °C for 30 s, followed by a final step for 6 min at 60 °C for the acquisition the green signal.
Pyrosequencing
Each sample submitted for pyrosequencing was prepared utilizing 3 μl streptavidin sepharose (GE Healthcare, Buckinghamshire, UK), 37 μl PyroMark binding buffer (Qiagen), 20 μl MB water (Qiagen) and 20 μl biotinylated PCR product. The plate was mixed and incubated for 15 min on a shaking table at 1,400 rpm. In the second step, the binding solutions were released into 40 μl of annealing buffer containing the respective sequencing primer. Primers were annealed to the target after incubation at 80 °C for 2 min and allowed to cool to room temperature prior to pyrosequencing. PyroGold reagents were used for the pyrosequencing reaction, and the signal was analysed using the PyroMark Q96 ID system (Qiagen). The software analyses the bioluminescence produced at the end of the enzymatic reactions, of which the intensity is proportional to the number of incorporated nucleotides. Positive controls were cases with known PI3KCA mutational status. The results of the experiments were interpreted according to the cutoffs provided by the manufacturer (Diatech Pharmacogenetics). For exon 9 mutations, the cutoff nucleotide substitution values to define a case as mutated were: E542K A > 5 %, E545K A >10 %, Q546K G > 10 % and Q546K A > 5 %. For exon 20 mutations, the cut-off nucleotide substitution values to define a case as mutated were: M1043I T > 10 %, M1043I A > 10 %, H1047R C > 12 %, H1047L A > 10 %, G1049S G > 6 % and G1049R T > 5 %.
Statistical methods
Statistical analysis was performed using the SPSS 15.0 software for Windows (SPSS Inc., Chicago, IL). In the groups of primary IBC treated with neoadjuvant trastuzumab therapy and MBC groups, we evaluated the possible association of PI3KCA mutations/PTEN loss with response to therapy; in the series of MBC, we evaluated also their relation with overall and disease-free survival (DFS). No survival analysis was performed in early IBC because of the short follow-up (all patients are alive and disease free).
Contingency tables were used to analyse the relationships between the categorical variables: absence/presence of mutation/loss of PTEN vs. pathological and biological parameters. Fisher’s exact test (2 × 2 tables) and chi-square test (general contingency tables) were used to test the significance of the association between two classifications. Kaplan–Meier survival analysis with log-rank test was used to determine the difference in DFS and overall survival between groups. All tests were two sided. The statistical significance level was chosen at 5 %. All analyses were performed blinded to the study endpoints.
Results
Clinical outcome of the patients
In the series of patients treated with neoadjuvant trastuzumab therapy, 11 (42 %) showed complete pathological response, 14 (54 %) partial pathological response and 1 (4 %) showed stable disease. At a mean follow-up of 37 months, 3 patients died of disease, 3 were alive with relapsing disease and 20 were alive without evidence of disease.
In the series of patients affected by MBC treated with trastuzumab therapy, 4 (8 %) showed complete clinical response, 18 (38 %) partial clinical response with more than 50 % reduction of the tumour, 14 (29 %) partial clinical response with less than 50 % reduction of the tumour, 8 (17 %) stable disease and 3 (6 %) showed progressive disease. In responsive cases (complete and partial responses), median response duration was 9.5 months with two patients having durable complete response over 3 years of trastuzumab treatment. At a mean follow-up of 66 months, 39 patients died of disease, 7 were alive with disease and 2 were alive without evidence of disease. In the series of 55 early-stage IBC treated with adjuvant therapy at a mean follow-up of 32 months, all patients were alive without evidence of relapse.
Frequency of PI3KCA mutations and relationships with pathological and biological characteristics
In the whole series of 129 IBC, PI3KCA mutations were observed in 25 cases (19 %): 12 (9 %) in exon 9 (2 Q546K and 10 E545K) and 13 (10 %) in exon 20 (1 H1047L and 12 H1047R; Fig. 1). PI3KCA mutations were observed in 15 % of locally advanced IBC treated with neoadjuvant therapy, in 10 % of MBC and in 29 % of early-stage IBC treated with adjuvant trastuzumab therapy. The relationships between PI3KCA mutation and pathological and biological characteristics are shown in Table 1 for the whole series and in Tables 2, 3 and 4 for the three different groups of patients. No statistically significant correlations were observed between mutations and pathological and biological parameters. In particular, we did not observe any relationship with histological type, nodal status and hormone receptor status.
Association of PI3KCA mutation with response to therapy and clinical outcome
In the series of patients treated with neoadjuvant therapy, PI3KCA mutations were observed in 3 out of the 11 cases with complete pathological response (three exon 20 H1047R mutations with 14.1, 33.9 and 71.2 % substitution frequency, respectively) and in 1 out of 14 cases with partial response (one exon 9 Q546K mutation with 19.5 % substitution frequency) (Table 5). These data suggest that PI3KCA mutations are not a major determinant of trastuzumab resistance because even cases with very high percentages of the mutated allele showed complete pathological response.
In the series of metastatic breast carcinomas, PI3KCA mutations were observed in 3 out of the 29 cases with partial clinical response (two exon 9 E545K mutations with substitution frequency of 11.6 and 38.4 % respectively, and one exon 20 H1047R mutation with 28.1 % substitution frequency) and in 1 out of 10 cases with stable/progressive disease (exon 20 H1047R mutation with 21.1 % substitution frequency; Table 6). No gene mutations were observed in the four patients showing complete clinical responses. These data suggest that PI3KCA mutations are not a major determinant of trastuzumab resistance in metastatic IBC treated with trastuzumab. Survival analysis in metastatic IBC showed that PI3KCA mutations are not related to adverse clinical outcome. However, the survival analysis has limited statistical power due to the limited number of investigated cases.
PTEN expression and PI3K mutation
PTEN immunohistochemical expression was evaluable in 86 cases and ranged from complete loss of reactivity in tumour cells, in spite of positive internal controls, to various degrees of immunoreactivity (Fig. 2). PTEN loss was observed in 24 (28 %) cases, 3 (13 %) of which were also mutated for PI3KCA. PTEN immunostaining was observed in 62 (72 %) cases, 17 (27 %) of which showed PI3K mutation. These data show that in the present series of IBC, PTEN loss, although less frequent in cases with concurrent PI3KCA mutation (13 versus 27 %), was not mutually exclusive with PI3KCA mutation.
Combined evaluation of PI3KCA mutation and PTEN loss in relation to clinical outcome in metastatic breast carcinomas
PTEN immunostaining could be evaluated in 34 of the 48 MBC, 10 of which showed complete PTEN loss. PI3KCA mutations were observed in 1 out of these 10 cases with complete PTEN loss and in 3 of the 24 cases with PTEN expression. PI3K pathway activation, defined as PTEN loss and/or PI3KCA mutation, was seen in 13 out of these 34 cases, including 1 case with complete clinical response, 5 cases with prominent clinical response (>50 % reduction in tumour burden) and 5 cases with partial clinical response (<50 % reduction in tumour burden), and in 2 cases with stable disease (Table 7). These data suggest that PI3K pathway activation is not a major determinant of trastuzumab resistance in MBC.
Discussion
Our present study on 129 Her2-positive IBC treated with trastuzumab, analysed with the highly specific and sensitive pyrosequencing technique, shows that PI3KCA mutations occur in 19 % of cases and are not related to pathological features of the tumours. In retrospective analyses of small groups of MBC and locally advanced IBC treated with neoadjuvant trastuzumab, we show that PI3KCA mutations are not related to response to treatment. In a subset of cases, we also show that PI3KCA mutations are not mutually exclusive with PTEN expression loss, and that, in MBC, PI3K pathway activation, defined as PI3KCA mutation and/or PTEN loss, is not associated with response to treatment. Survival analysis in the group of MBC shows that neither PI3KCA mutations nor PI3K/PTEN pathway activation is related to clinical outcome, but the limited number of investigated cases could have precluded the study to reach statistical significance.
The reported frequency of PI3KCA mutation in literature is quite variable, ranging from 15 [30] to 29 % [38]. This wide range of frequencies in Her2-positive IBC could in part be related to the limited number of investigated cases in some studies, to the different analytical methods used, or could be related to differences between population groups. The latter is a well-known phenomenon, which has been observed not only between different ethnic groups, such as for example frequency of EGFR mutations lung carcinoma in Western and Japanese populations, but also within the same ethnic group, such as B-raf mutations and PTC/Ret translocations in thyroid carcinomas [38, 39]. In a previous study of a consecutively collected series of IBC from the same geographical area (Trentino, Northeast Italy), we observed a frequency of PI3KCA mutation (26 % mutated cases) which is slightly higher than the one observed in the present study [7]. This difference might be related to the different composition of the two series, as the previous series included mainly Her2-negative ER-positive IBC, while the present one includes only Her2-positive cases, with a higher percentage of ER-negative cases. Several studies have indeed shown that PI3KCA mutation is more frequent in ER-positive and Her2-negative IBC [8–10, 14, 22–24] suggesting that in these cases PI3K/AKT pathway activation occurs through a Her2-independent mechanism. However, discordances exist, and other studies have either not found such associations or even provided opposite results, such as an association between PI3KCA mutations and Her2 overexpression [13]. Comparison between the different studies is extremely difficult as the inclusion criteria are different. Moreover, since the pathogenetic role of mutations in different regions of the PI3KCA gene could provide different activating effects, with potentially different pathogenetic and clinic relevance [7], further studies, and possibly a meta-analysis of currently available data, should further investigate these relationships.
The most intriguing aspect of the study of PI3KCA mutations is their possible role as predictive markers of resistance to anti-Her2 therapy, either using trastuzumab or the reversible dual kinase inhibitor lapatinib, which is active also against EGFR. Preclinical and preliminary data suggest that PI3KCA mutations might predict resistance to anti-Her2 therapy [5, 21, 27–29]. The study of Razis et al. [28] is of particular interest as it includes a series of partly Her2-positive and partly Her2-negative metastatic IBC treated with trastuzumab: in Her2-negative cases, PI3KCA mutations were not related to time to progression, while in the Her2-positive group, a strong and independent association between PI3KCA mutations and worse prognosis was found. However, data are still not conclusive, and some studies suggest that PI3KCA mutations are not associated with response or clinical outcome [31, 39] or are of limited predictive value [5, 30]. Our present study shows that PI3KCA mutations occur in patients responding to trastuzumab treatment (i.e. four neoadjuvant patients and five MBC patients), further supporting the hypothesis that PI3KCA mutations do not exclude the possibility of clinical benefit to trastuzumab therapy.
Previous reports suggested that PI3KCA mutation and PTEN loss are mutually exclusive [13]. However, in our study 3 (12.5 %) out of 24 PTEN-negative IBC showed also PI3KCA mutation, as also reported by Perez-Tenor et al. [10] and Wang et al. [31]. The reason for this redundancy in the activation of the PI3K pathway is not clear, but could be related to different yet unknown cross-talk mechanisms between different pathways, or to an additive effect of these two activating hits along the same metabolic pathway.
The lack of a clear-cut relationship between PI3KCA mutation and therapeutic response to anti-Her2 agents can be interpreted in the light of the complex and poorly understood mechanisms of action of trastuzumab. First, resistance could be related to the fact that the PI3K/AKT signalling pathway is very complex and may be improperly constitutionally activated at several levels with different mechanisms, which, beside PI3KCA mutation, potentially include loss of PTEN expression, PI3KCA gene amplification, mutations or amplification of AKT, deregulation of mTOR activity, altered expression of p70S6K, etc. In particular, PTEN loss has been associated with resistance to anti-Her2 therapy in cell lines and patients [21, 27, 28, 30, 38]. The combined evaluation of alterations of the PI3K/AKT pathway at several levels could provide a rationale for combining anti-Her2 therapy with PI3K/AKT inhibitors [29, 40]. Preliminary data indeed show that concurrent evaluation of PI3KCA mutations and PTEN and p70S6K expression may identify patients without PI3K/AKT pathway activation who could benefit more from trastuzumab-based therapy [27, 28, 30, 31]. However, in our small series of MBC, PI3K/PTEN pathway activation was not related to clinical response to trastuzumab, and further studies are needed to clarify this issue. Alternatively, the fact that PI3KCA mutated cases may respond to trastuzumab therapy could be interpreted in the light of the possible role of trastuzumab in determining antibody-dependent cell-mediated cytotoxicity. Trastuzumab is an intact monoclonal antibody which, binding to the Her2 molecule, could elicit antibody-dependent cellular cytotoxicity which could lead to tumour cell necrosis and hence clinical/pathological response [41–43].
In conclusion, our study shows that PI3KCA mutations are frequent in Her2-positive breast cancer and that there is no significant correlation with response to trastuzumab-based therapy. The study also shows that PI3K pathway activation, defined as PTEN loss and/or PI3KCA mutation, is not associated with response to treatment or with clinical outcome. Since most reported series of IBC treated with anti-Her2 treatment are small and the possible variables influencing the results are many, including the confounding effects of the patients’ background treatments [5], an effort should be undertaken to pool all data together to perform a meta-analysis and possibly to study PI3K pathway activation mechanisms in a more comprehensive way, including also less frequently studied biomarkers such as AKT mutation and phosphorylation status, mTOR and p70S6K expression levels. More importantly, the value of the combined use of trastuzumab with different inhibitors targeting the PI3K pathway at different levels needs to be tested. Finally, our data show that PI3KCA mutation and/or PTEN loss are not criteria to exclude patients from potentially beneficial anti-Her2 therapy.
References
Clifford A, Hudis MD (2007) Trastuzumab—mechanism of action and use in clinical practice. N Engl J Med 357:39–51
Bailey TA, Luan H, Clubb RJ, Naramura M, Band V, Raja SM, Band H (2011) Mechanisms of Trastuzumab resistance in ErbB2-driven breast cancer and newer opportunities to overcome therapy resistance. J Carcinog 10:28
Yakes FM, Chinratanalab W, Ritter CA, King W, Seelig S, Arteaga CL (2002) Herceptin-induced inhibition of phosphatidylinositol-3 kinase and Akt is required for antibody-mediated effects on p27, cyclin D1, and antitumor action. Cancer Res 62:4132–4141
Mills GB, Kohn E, Lu Y, Eder A, Fang X, Wang H, Bast RC, Gray J, Jaffe R, Hortobagyi G (2003) Linking molecular diagnostics to molecular therapeutics: targeting the PI3K pathway in breast cancer. Semin Oncol 30(5 Suppl 16):93–104
Esteva FJ, Guo H, Zhang S, Santa-Maria C, Stone S, Lanchbury JS, Sahin AA, Hortobagyi GN, Yu D (2010) PTEN, PIK3CA, p-AKT, and p-p70S6K status: association with trastuzumab response and survival in patients with HER2-positive metastatic breast cancer. Am J Pathol 177:1647–1656
Lopez-Knowles E, O'Toole SA, McNeil CM, Millar EK, Qiu MR, Crea P, Daly RJ, Musgrove EA, Sutherland RL (2010) PI3K pathway activation in breast cancer is associated with the basal-like phenotype and cancer-specific mortality. Int J Cancer 126:1121–1131
Barbareschi M, Buttitta F, Felicioni L, Cotrupi S, Barassi F, Del GM, Ferro A, Dalla PP, Galligioni E, Marchetti A (2007) Different prognostic roles of mutations in the helical and kinase domains of the PIK3CA gene in breast carcinomas. Clin Cancer Res 13:6064–6069
Kalinsky K, Heguy A, Bhanot UK, Patil S, Moynahan ME (2011) PIK3CA mutations rarely demonstrate genotypic intratumoral heterogeneity and are selected for in breast cancer progression. Breast Canc Res Treat 129:635–643
Maruyama N, Miyoshi Y, Taguchi T, Tamaki Y, Monden M, Noguchi S (2007) Clinicopathologic analysis of breast cancers with PIK3CA mutations in Japanese women. Clin Cancer Res 13:408–414
Perez-Tenorio G, Berglund F, Esguerra MA, Nordenskjold B, Rutqvist LE, Skoog L, Stal O (2006) Cytoplasmic p21WAF1/CIP1 correlates with Akt activation and poor response to tamoxifen in breast cancer. Int J Oncol 28:1031–1042
Stemke-Hale K, Gonzalez-Angulo AM, Lluch A, Neve RM, Kuo WL, Davies M, Carey M, Hu Z, Guan Y, Sahin A, Symmans WF, Pusztai L, Nolden LK, Horlings H, Berns K, Hung MC, van de Vijver MJ, Valero V, Gray JW, Bernards R, Mills GB, Hennessy BT (2008) An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res 68:6084–6091
Lerma E, Catasus L, Gallardo A, Peiro G, Alonso C, Aranda I, Barnadas A, Prat J (2008) Exon 20 PIK3CA mutations decreases survival in aggressive (HER-2 positive) breast carcinomas. Virchows Arch 453:133–139
Saal LH, Holm K, Maurer M, Memeo L, Su T, Wang X, Yu JS, Malmstrom PO, Mansukhani M, Enoksson J, Hibshoosh H, Borg A, Parsons R (2005) PIK3CA mutations correlate with hormone receptors, node metastasis, and ERBB2, and are mutually exclusive with PTEN loss in human breast carcinoma. Cancer Res 65:2554–2559
Li SY, Rong M, Grieu F, Iacopetta B (2006) PIK3CA mutations in breast cancer are associated with poor outcome. Breast Canc Res Treat 96:91–95
Buttitta F, Felicioni L, Barassi F, Martella C, Paolizzi D, Fresu G, Salvatore S, Cuccurullo F, Mezzetti A, Campani D, Marchetti A (2007) PIK3CA mutation and histological type in breast carcinoma: high frequency of mutations in lobular carcinoma. J Pathol 208:350–355
Benvenuti S, Frattini M, Arena S, Zanon C, Cappelletti V, Coradini D, Daidone MG, Pilotti S, Pierotti MA, Bardelli A (2008) PIK3CA cancer mutations display gender and tissue specificity patterns. Hum Mutat 29:284–288
Liedtke C, Cardone L, Tordai A, Yan K, Gomez HL, Figureoa LJ, Hubbard RE, Valero V, Souchon EA, Symmans WF, Hortobagyi GN, Bardelli A, Pusztai L (2008) PIK3CA-activating mutations and chemotherapy sensitivity in stage II–III breast cancer. Breast Canc Res 10:R27
Tsutsui S, Inoue H, Yasuda K, Suzuki K, Higashi H, Era S, Mori M (2005) Reduced expression of PTEN protein and its prognostic implications in invasive ductal carcinoma of the breast. Oncology 68:398–404
Gonzalez-Angulo AM, Ferrer-Lozano J, Stemke-Hale K, Sahin A, Liu S, Barrera JA, Burgues O, Lluch AM, Chen H, Hortobagyi GN, Mills GB, Meric-Bernstam F (2011) PI3K pathway mutations and PTEN levels in primary and metastatic breast cancer. Mol Cancer Ther 10:1093–1101
Gori S, Sidoni A, Colozza M, Ferri I, Mameli MG, Fenocchio D, Stocchi L, Foglietta J, Ludovini V, Minenza E, De Angelis V, Crino L (2009) EGFR, pMAPK, pAkt and PTEN status by immunohistochemistry: correlation with clinical outcome in HER2-positive metastatic breast cancer patients treated with trastuzumab. Ann Oncol 20:648–654
Berns K, Horlings HM, Hennessy BT, Madiredjo M, Hijmans EM, Beelen K, Linn SC, Gonzalez-Angulo AM, Stemke-Hale K, Hauptmann M, Beijersbergen RL, Mills GB, van de Vijver MJ, Bernards R (2007) A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Canc Cell 12:395–402
Bachman KE, Argani P, Samuels Y, Silliman N, Ptak J, Szabo S, Konishi H, Karakas B, Blair BG, Lin C, Peters BA, Velculescu VE, Park BH (2004) The PIK3CA gene is mutated with high frequency in human breast cancers. Canc Biol Ther 3:772–775
Boyault S, Drouet Y, Navarro C, Bachelot T, Lasset C, Treilleux I, Tabone E, Puisieux A, Wang Q (2012) Mutational characterization of individual breast tumors: TP53 and PI3K pathway genes are frequently and distinctively mutated in different subtypes. Breast Canc Res Treat 132:23–39
Michelucci A, Di CC, Lami A, Collecchi P, Caligo A, Decarli N, Leopizzi M, Aretini P, Bertacca G, Porta RP, Ricci S, Della RC, Stanta G, Bevilacqua G, Cavazzana A (2009) PIK3CA in breast carcinoma: a mutational analysis of sporadic and hereditary cases. Diagn Mol Pathol 18:200–205
Ellis MJ, Lin L, Crowder R, Tao Y, Hoog J, Snider J, Davies S, DeSchryver K, Evans DB, Steinseifer J, Bandaru R, Liu W, Gardner H, Semiglazov V, Watson M, Hunt K, Olson J, Baselga J (2010) Phosphatidyl-inositol-3-kinase alpha catalytic subunit mutation and response to neoadjuvant endocrine therapy for estrogen receptor positive breast cancer. Breast Canc Res Treat 119:379–390
Dupont JJ, Laenkholm AV, Knoop A, Ewertz M, Bandaru R, Liu W, Hackl W, Barrett JC, Gardner H (2011) PIK3CA mutations may be discordant between primary and corresponding metastatic disease in breast cancer. Clin Cancer Res 17:667–677
Lai YL, Mau BL, Cheng WH, Chen HM, Chiu HH, Tzen CY (2008) PIK3CA exon 20 mutation is independently associated with a poor prognosis in breast cancer patients. Ann Surg Oncol 15:1064–1069
Razis E, Bobos M, Kotoula V, Eleftheraki AG, Kalofonos HP, Pavlakis K, Papakostas P, Aravantinos G, Rigakos G, Efstratiou I, Petraki K, Bafaloukos D, Kostopoulos I, Pectasides D, Kalogeras KT, Skarlos D, Fountzilas G (2011) Evaluation of the association of PIK3CA mutations and PTEN loss with efficacy of trastuzumab therapy in metastatic breast cancer. Breast Canc Res Treat 128:447–456
Junttila TT, Akita RW, Parsons K, Fields C, Lewis Phillips GD, Friedman LS, Sampath D, Sliwkowski MX (2009) Ligand-independent HER2/HER3/PI3K complex is disrupted by trastuzumab and is effectively inhibited by the PI3K inhibitor GDC-0941. Canc Cell 15:429–440
Dave B, Migliaccio I, Gutierrez MC, Wu MF, Chamness GC, Wong H, Narasanna A, Chakrabarty A, Hilsenbeck SG, Huang J, Rimawi M, Schiff R, Arteaga C, Osborne CK, Chang JC (2011) Loss of phosphatase and tensin homolog or phosphoinositol-3 kinase activation and response to trastuzumab or lapatinib in human epidermal growth factor receptor 2-overexpressing locally advanced breast cancers. J Clin Oncol 29:166–173
Wang L, Zhang Q, Zhang J, Sun S, Guo H, Jia Z, Wang B, Shao Z, Wang Z, Hu X (2011) PI3K pathway activation results in low efficacy of both trastuzumab and lapatinib. BMC Canc 11:11
Brunner-Kubath C, Shabbir W, Saferding V, Wagner R, Singer CF, Valent P, Berger W, Marian B, Zielinski CC, Grusch M, Grunt TW (2011) The PI3 kinase/mTOR blocker NVP-BEZ235 overrides resistance against irreversible ErbB inhibitors in breast cancer cells. Breast Canc Res Treat 129:387–400
Miller TW, Rexer BN, Garrett JT, Arteaga CL (2011) Mutations in the phosphatidylinositol 3-kinase pathway: role in tumor progression and therapeutic implications in breast cancer. Breast Canc Res 13:224
Eichhorn PJ, Gili M, Scaltriti M, Serra V, Guzman M, Nijkamp W, Beijersbergen RL, Valero V, Seoane J, Bernards R, Baselga J (2008) Phosphatidylinositol 3-kinase hyperactivation results in lapatinib resistance that is reversed by the mTOR/phosphatidylinositol 3-kinase inhibitor NVP-BEZ235. Cancer Res 68:9221–9230
Cantaloni C, Tonini RE, Eccher C, Morelli L, Leonardi E, Bragantini E, Aldovini D, Fasanella S, Ferro A, Cazzolli D, Berlanda G, Dalla PP, Barbareschi M (2011) Diagnostic value of automated Her2 evaluation in breast cancer: a study on 272 equivocal (score 2+) Her2 immunoreactive cases using an FDA approved system. Appl Immunohistochem Mol Morphol 19:306–312
Barbareschi M, Girlando S, Mauri FM, Forti S, Eccher C, Mauri FA, Togni R, Dalla PP, Doglioni C (1994) Quantitative growth fraction evaluation with MIB1 and Ki67 antibodies in breast carcinomas. Am J Clin Pathol 102:171–175
Fasanella S, Leonardi E, Cantaloni C, Eccher C, Bazzanella I, Aldovini D, Bragantini E, Morelli L, Cuorvo LV, Ferro A, Gasperetti F, Berlanda G, Dalla PP, Barbareschi M (2011) Proliferative activity in human breast cancer: Ki-67 automated evaluation and the influence of different Ki-67 equivalent antibodies. Diagn Pathol 6(Suppl 1):S7
Xu BH, Jiang ZF, Chua D, Shao ZM, Luo RC, Wang XJ, Liu DG, Yeo W, Yu SY, Newstat B, Preston A, Martin AM, Chi HD, Wang L (2011) Lapatinib plus capecitabine in treating HER2-positive advanced breast cancer: efficacy, safety, and biomarker results from Chinese patients. Chin J Canc 30:327–335
Girlando S, Cuorvo LV, Bonzanini M, Morelli L, Amadori P, Dalla PP, Barbareschi M (2011) High prevalence of B-RAF mutation in papillary carcinoma of the thyroid in north-east Italy. Int J Surg Pathol 8:173–176
Lu CH, Wyszomierski SL, Tseng LM, Sun MH, Lan KH, Neal CL, Mills GB, Hortobagyi GN, Esteva FJ, Yu D (2007) Preclinical testing of clinically applicable strategies for overcoming trastuzumab resistance caused by PTEN deficiency. Clin Cancer Res 13:5883–5888
Park S, Jiang Z, Mortenson ED, Deng L, Radkevich-Brown O, Yang X, Sattar H, Wang Y, Brown NK, Greene M, Liu Y, Tang J, Wang S, Fu XY (2010) The therapeutic effect of anti-HER2/neu antibody depends on both innate and adaptive immunity. Canc Cell 18:160–170
Mohsin SK, Weiss HL, Gutierrez MC, Chamness GC, Schiff R, DiGiovanna MP, Wang CX, Hilsenbeck SG, Osborne CK, Allred DC, Elledge R, Jenny C, Chang JC (2005) Neoadjuvant Trastuzumab induces apoptosis in primary breast cancers. J Clin Oncol 23:2460–2468
Varchetta S, Gibelli L, Oliviero V, Nardini E, Gennari R, Gatti G, Silva LS, Villani N, Tagliabue E, Menard S, Costa A, Fannioni FF (2007) Element related to enterogenity of antibody-dependent cell cytotoxicity in patients under Trastuzumab therapy for primary operable breast cancer overexpressing Her2. Cancer Res 67:11991–11999
Acknowledgments
This study has been supported by grants of the Provincia Autonoma di Trento, Italy and of the Fondazione Cassa di Risparmio di Trento e Rovereto, Italy.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barbareschi, M., Cuorvo, L.V., Girlando, S. et al. PI3KCA mutations and/or PTEN loss in Her2-positive breast carcinomas treated with trastuzumab are not related to resistance to anti-Her2 therapy. Virchows Arch 461, 129–139 (2012). https://doi.org/10.1007/s00428-012-1267-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-012-1267-2