Abstract
The frequency and morphological spectrum of gastrointestinal peripheral nerve sheath tumors (PNSTs) from consecutive case material has not been studied in the c-KIT era. We reviewed all mesenchymal gastrointestinal (GI) lesions at our departments according to current diagnostic criteria. PNSTs formed the third commonest group of mesenchymal GI tumors with a lower frequency (≤5%) compared to gastrointestinal stromal tumors (GISTs; ∼50%) and smooth muscle neoplasms (∼30%). Granular cell tumors (GCTs; n = 31) and schwannomas (n = 22) were the most common types of PNSTs encountered. Rare tumors included neurofibromatosis 1 (NF1)-associated PNSTs (n = 5) and gastric perineurioma (n = 1). Thirteen schwannomas (including also some recent cases) were initially diagnosed as GIST, leiomyoma, or neurofibroma. Unusual histological variants included sigmoid GCT with prominent lipomatous component (n = 1), reticular–microcystic schwannoma of small (n = 1) and large (n = 1) bowel, NF1-associated gastric schwannoma (the first case to date), and psammomatous melanotic colonic schwannoma unrelated to Carney complex (n = 1). PNSTs coexisted with GIST in four patients (three had definite NF1). In conclusion, PNSTs of the GI tract are rare uniformly benign neoplasms that may show schwannian, perineurial, fibroblastic, or mixed differentiation. Most of them (92%) occurred sporadically unassociated with NF1 or NF2. Gastrointestinal PNSTs are still underrecognized by general pathologists. Awareness of their diverse morphology will help to avoid confusing them with smooth muscle neoplasms and GIST that they may closely mimic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following the seminal discovery of activating KIT mutations in mesenchymal gastrointestinal tumors formerly classified as “smooth muscle” or “neurogenic neoplasms,” the term “gastrointestinal stromal tumor” (GIST) has been redefined as a specific clinicopathologic and molecular diagnostic entity with implications for therapy and prognosis [1]. According to current diagnostic criteria, a majority of primary mesenchymal neoplasms of the gastrointestinal tract (GI tract) represent GISTs [1]. Although the existence of GI neoplasms with true neural differentiation has been long recognized [2, 3], only a few selective series describing the clinicopathologic characteristics of one tumor type of peripheral nerve sheath tumors (PNSTs) from specific GI site have been published in the c-KIT era [4–8]. Thus, the frequency and full spectrum of gastrointestinal PNSTs from a consecutive case material has not been covered in a single study. In our experience, gastrointestinal PNSTs are still underrecognized by general pathologists and may be the source of diagnostic confusion as many of them may be mistaken for smooth muscle neoplasms and GISTs. Because of the completely different therapeutic options and biological potentials of the different categories of mesenchymal GI neoplasms, a precise histological diagnosis is mandatory.
The aim of this study was to analyze the frequency and morphologic diversity of PNSTs in the GI tract, thereby looking for unusual and possibly underrecognized variants that might represent a diagnostic challenge.
Material and method
All mesenchymal lesions of the GI tract from the esophagus to the anorectum at our departments (1997–2009) were retrieved by a computerized search for tumors classified as “neurofibroma, schwannoma, neurinoma, spindle cell tumor, peripheral nerve sheath tumor, neurofibromatosis, GIST, stromal tumor, leiomyoma, leiomyoblastoma, or leiomyosarcoma.” Hematoxylin and Eosin (H&E)-stained slides have been reviewed by two experienced pathologists (A.A. & R.C.). One case has been reported previously [9], but more extended follow-up was obtained. Immunohistochemistry (IHC) was performed on 5-µm sections using a polymer Kit purchased from Zytomed systems Ltd., Berlin, Germany according to the manufacturer’s instructions and the following antibodies: protein S100 (polyclonal, 1:2,500, DakoCytomation, Glostrup, Denmark), CD56 (1:100, Novocastra), desmin (1:250, DakoCytomation), α-smooth muscle actin (α-SMA; 1:200, DakoCytomation), CD34 (1:200, DakoCytomation), CD117 (polyclonal, 1:200, DakoCytomation), glial fibrillary acidic protein (GFAP; 1:50, DakoCytomation), calretinin (1:2, Zytomed), and α-inhibin (1:100, Serotec, UK). Schwannomas were also stained with a monoclonal antibody recognizing the antigen DOG-1 (1:200, Novocastra). In addition, further markers were applied selectively in some cases, based on relevant differential diagnoses (antibody sources and protocols are available upon request). Follow-up data were obtained from clinical records, from pathology reports, and from treating doctors.
Results
Frequency and distribution of gastrointestinal PNSTs
A total of 58 patients were recovered. PNSTs represented 5% of all mesenchymal tumors of the GI tract in our case material contrasting a percentage of ∼50% for GISTs and ∼30% for smooth muscle neoplasms. Five patients (8%) were known to have neurofibromatosis 1 (NF1), but none had features of NF2 or other tumor syndrome. Patients were 34 women and 24 men with a mean age of 52 years (range, 17–87). Histologically, tumors were classified as granular cell tumor (n = 31), gastrointestinal schwannoma (n = 22), gastric perineurioma (n = 1), and NF1-associated PNSTs (n = 5). Several fibroblastic colorectal polyps were seen but excluded from further analysis due to the controversy regarding their neoplastic nature and relationship to peripheral nerve sheath tumors. No case of sporadic solitary neurofibroma, “epithelioid Schwann cell hamartoma,” or conventional malignant PNST (MPNST) was found. The clinicopathologic features of the individual tumor types are discussed in detail below.
Granular cell tumors (Table 1)
These affected 19 women and 12 men aged 17–87 years (mean, 50 years). All were incidental findings during endoscopic investigation for other diseases or for nonspecific upper GI symptoms. Three tumors were ulcerated. Most tumors originated in the distal esophagus/gastroesophageal junction (n = 24). Two involved the mid-esophagus. One tumor each originated in the cardia, body, cecum, sigmoid colon, and rectum. Treatment was endoscopic biopsy or marginal polypectomy in almost all cases. In five of ten patients who underwent a control endoscopic biopsy at 8–52 months (mean, 21 months), tumor cells were detected, probably indicating residual tumor, but none showed progressive growth or metastasis. However, most patients were lost to follow-up due to the benign nature of the lesion. Size of the tumors ranged from 2 to 20 mm (mean, 6 mm). Multiple tumors were not observed. Pseudoepitheliomatous squamous hyperplasia of overlying mucosa was a common feature of esophageal lesions (Fig. 1a). All but one tumor were centered in the lamina propria mucosae/submucosa. Tumors revealed typical sheets of large polyhedral cells having granular PAS-positive cytoplasm with hyaline droplets and small centrally located nuclei. All tumors but one showed infiltrating borders, and three have infiltrated into the muscularis propria (Fig. 1b). Focal spindling was seen in two cases (Fig. 1c). One tumor from the sigmoid colon combined features of granular cell tumors (GCT) and submucosal lipoma with a peculiar nodule-in-nodule pattern and predominance of fatty component (Fig. 1d, e). The largest tumor (20 mm) originated in the muscularis propria of the rectum and presented clinically as a “rectovaginal septum mass.” This tumor blended with the Auerbach plexus in a manner reminiscent of GIST (Fig. 1f, g) and showed focal peritumoral lymphoid cuffs. In tumors with available paraffin blocks or unstained slides, IHC revealed strong expression of protein S100 (17/17; Fig. 1g), CD56 (17/17), and variable expression of calretinin (11/14) and α-inhibin (11/14; Fig. 1h). Four cases stained variably with CD34 in the granular tumor cells as well as in slender bipolar mesenchymal cells scattered between them. CD34 was more prominent toward infiltrating tumor borders (Fig. 1i). All tumors were negative for CD117, desmin, and α-SMA.
Representative images of GCTs in the GI tract with subepithelial growth in the esophagus associated with pseudoepitheliomatous hyperplasia (b) and infiltration of the muscularis propria (b). Prominent spindling mimicking GIST was seen in two cases (c). Whole-mount section of lipomatous cecal GCT with nodule-in-nodule pattern (d), paucity of tumor cells toward the mucosa contrasts with conventional GCT. Almost equal proportions of fat cells and granular cells were seen at higher magnification (e). Rectal GCT (f, lower left) arising from Auerbach plexus (upper right) highlighted with protein S100 immunostaining in g. α-Inhibin showed a moderate staining that was less intense than in adjacent nerve on the right (h). CD34 reactivity was more prominent at the tumor periphery (i, lower field)
Gastrointestinal schwannomas (Table 2)
Patients were 14 women and 8 men aged 38–86 (mean age, 63 years). Sixteen tumors (73%) originated in the stomach, four (18%) in the large bowel (one each in cecum, descendosigmoidal junction, sigmoid colon, and rectum), one in the mid-jejunum, and one at an unspecified intestinal site. Symptoms were nonspecific upper abdominal symptoms or epigastric mass for symptomatic gastric tumors, but many were incidental findings during investigation or at surgery for other diseases. One patient had definite NF1 (see also Table 3). Three patients had one or more other tumors unrelated to NF1: colorectal adenoma/cancer (n = 2), breast cancer (n = 2), papillary thyroid carcinoma (n = 1), and small lymphocytic lymphoma/chronic lymphocytic leukemia (CLL; n = 1). Clinical diagnosis was uniformly “gastric wall tumor, most probably GIST.” Gastric tumors involved predominantly the body (n = 12), two originated in the antrum, and two at unspecified gastric sites. Tumor size ranged from 0.7 to 15.5 cm (mean, 3.5 cm). Ten patients had a mean follow-up of 31.7 months (range, 2–77 months); none had evidence of progressive disease or new tumors. Extended follow-up was obtained for the previously reported patient with melanotic psammomatous schwannoma (48 months); there was no evidence of recurrence or development of new tumors.
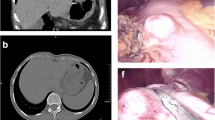
Grossly, the majority showed a homogenous tan-yellow or whitish cut surface with strikingly firm to hard consistency so that diagnosis was suspected in some cases upon bisecting the tumor (Fig. 2a). Only nine tumors were initially correctly diagnosed histologically. Initial diagnoses included GIST/sclerosing GIST (n = 9), neurofibroma (n = 3), and involuted leiomyoma (n = 1). Two recent gastric tumors were correctly diagnosed by core needle biopsy. The jejunal tumor (reticular variant) was coincidental to a huge extramural gastric GIST leading to misinterpretation of the large GIST as peritoneal metastasis of the small mural jejunal tumor. All gastric tumors were moderately cellular throughout with abundant wavy collagen fibers. Prominent lymphoid cuffs were seen in all cases (Fig. 2b) but were less prominent in the reticular variant. Of interest, one patient with a gastric schwannoma had a history of small lymphocytic lymphoma/CLL. His tumor displayed extensive lymphoid cuffing that turned out to be neoplastic on IHC and molecular analysis (Fig. 2c). He also had perigastric lymph nodes involved by the CLL. Most tumors showed a variable mixture of microtrabecular, macrotrabecular, nested, storiform, and cellular patterns (Fig. 2d–h). Antoni A and B areas were lacking in all cases as well as true nuclear palisading. However, three tumors including the NF1 associated one had foci of nuclear crowding reminiscent of palisading. Three tumors showed areas of sclerosis and confluent dystrophic calcification superficially reminiscent of calcifying fibrous tumors, but these were usually focal findings in otherwise typical schwannomas. One multifocal sigmoid schwannoma showed sheets of plump to spindled cells, scattered psammoma bodies, and occasional pigmentation consistent with psammomatous melanotic schwannoma. The histologic features of this tumor have been reported in more details previously [9]. One cecal tumor and one jejunal tumor revealed a reticular–microcystic pattern that is reminiscent of perineurioma of soft tissue. The cecal tumor showed slender bipolar cells infiltrating between the mucosal crypts with scattered eosinophils and prominent CD34 reactivity superficially mimicking inflammatory fibroid polyp (Fig. 2i). However, the deeper portion of the tumor within the submucosa showed typical reticular–microcystic pattern (Fig. 2j) with prominent protein S100 expression in all tumor cells (Fig. 2k). IHC revealed a strong expression of protein S100 in all schwannomas (Fig. 2l) and variable usually focal expression of CD56 (11/11) and GFAP (9/9). CD34 was detectable in the stromal cells in areas of sclerosis, but not in tumor cells, except for the cecal reticular schwannoma. Scattered epithelial membrane antigen (EMA)-positive perineurial cells were seen in several cases. All six cases examined were negative for calretinin and α-inhibin. All of the schwannomas have been stained with CD117, and 12 cases were also stained with the antibody DOG-1 and were found completely negative for both markers.
Gross and microscopic features of gastrointestinal schwannomas: Gastric schwannomas were well circumscribed intramural masses with homogeneous tan-yellow cut surface (a). Prominent submucosal lymphoid cuffs were seen in sigmoid schwannoma (b). Neoplastic (CLL) lymphoid cuffs in gastric schwannoma showed irregular infiltration into subserosal fat. Microtrabecular (d), macrotrabecular (e), nested (f), storiform (g), and cellular (h) histologic patterns. Cecal reticular schwannoma infiltrated into both mucosa and submucosa (i) with prominent reticular–microcystic pattern in deeper portion of the tumor (j) and diffuse S100 expression (k). S100 expression in gastric schwannoma was typically diffuse and strong with wavy pattern (l)
Gastric perineurioma
The patient was a 58-year-old man who presented with epigastric pain without relevant clinical history or signs of NF1 or NF2. A 5 × 3 × 2 cm measuring mass was excised from the stomach. The patient was alive and well 5 years after surgery. The tumor was well circumscribed but nonencapsulated and was centered in the submucosa (Fig. 3a). It was composed of slender cells with wavy nuclei and long bipolar cytoplasmic extensions arranged in diffuse pattern with intervening thin capillaries (Fig. 3b). Onion skin pattern and eosinophil-rich infiltrate typically seen in inflammatory fibroid polyp were lacking. Tumor cells expressed diffusely EMA (Fig 3c) and variably CD34, but were negative for S100, CD117, desmin, α-SMA, and h-caldesmon. This tumor lacked the organoid biphasic pattern of the recently described hybrid schwannoma/perineurioma [10].
Gastrointestinal manifestation of NF1 (Table 3)
Five patients presented with GI manifestations of NF1 (other than GIST) at a mean age of 39 years. All had clinical features of NF1. One patient had multiple minute neurofibromas in the gastric fundus and in the vermiform appendix associated with multiple minute gastric fundus GISTs, all diagnosed at autopsy (Fig. 4a, b). He died of locally advanced mediastinal MPNST. Another had a plexiform neurofibroma of ileum/mesentery accompanied by diffuse mucosal neurofibromatosis in the ileum (Fig. 4c–e). One patient had multiple plexiform neurofibromas in stomach and small bowel, in addition to a large gastric GIST and a duodenal somatostatinoma. Another patient presented with stenosing diffuse mucosal neurofibromatosis in the rectosigmoid colon and small bowel at ages 11 and 14 years, respectively. She had no circumscribed tumors. Histologically, GI neurofibromatosis manifested either as diffuse spindle cell proliferation displacing mucosal crypts apart or as a ganglioneuromatous proliferation involving the submucosa (Fig. 4f). The fifth patient, a 75-year-old man, presented with concurrent gastric schwannoma (Fig. 4g–i) and a diffuse neurofibroma in the appendix/mesoappendix in addition to microscopic appendiceal carcinoid. He had a 1-mm microscopic GIST detected incidentally in the gastric specimen intimately associated with the gastric schwannoma (Fig. 4j–l). This patient had multiple cutaneous neurofibromas in the whole body. He died postoperatively of nontumor-related cause.
Spectrum of NF1-associated peripheral nerve sheath tumors of the GI tract. Autopsy specimen showed multiple minute plaque-like nodules on the gastric serosa that turned out to be either minute GISTs or neurofibromas (a). Three minute neurofibromas in the appendix from same patient protruded from the serosa (b). Large plexiform neurofibroma in the ileal wall/mesentery from another patient formed multiple nodules (c, d). Reticular perineurioma-like component (between arrows) was a common finding at the periphery of neurofibromatous nodules (e). Diffuse neurofibromatosis was composed of dense S100-positive spindle cell proliferation separating mucosal crypts (right) associated with submucosal ganglioneuromatous hyperplasia (left; f). NF1-associated sclerosing gastric schwannoma with prominent lymphoid cuffs (g), occasional fascicular growth (h), and strong diffuse S100 staining (i). Microscopic GIST in the midfield separated from sclerosing schwannoma (lower right) by muscle bundles (between arrows) from same patient (j). Higher magnification of the GIST is shown in k. Protein S100 staining highlighted prominent neural hyperplasia accompanying the GIST (l). The GIST coexpressed CD117 and CD34 (not shown)
Discussion
In this study, we reviewed the spectrum of PNSTs of the GI tract in a consecutive case material, demonstrating that PNSTs encompass a heterogeneous group of rare uniformly benign GI tumors that may differentiate along any of the cellular components of the peripheral nerves. PNSTs with schwannian differentiation (GCTs and schwannomas) comprised 91% of all GI PNSTs. The majority occurred sporadically unrelated to NF1 or NF2.
A neurogenic derivation of GCTs has been demonstrated in several studies, and a schwannian line of differentiation is currently widely accepted [11]. GCTs have been documented in the setting of NF1 [12] and as a novel component in hybrid PNSTs of soft tissue [13]. However, their distinct histology warrants their separation from neurofibroma and schwannoma. GCTs of the GI tract comprised ≤5% of all GCTs [11]. The esophagus (80%) and large bowel (10%) are predilection sites in our study and in previous series [14, 15]. Diagnosis of GCTs is usually not problematic. Rare GCTs with prominent spindling may mimic GIST [15, 16], but more typical diagnostic areas are usually present. GCTs are negative for CD117, desmin, α-SMA, and h-caldesmon. They are uniformly S100-positive, and they stain variably with CD56, calretinin, α-inhibin, and CD34 [17, 18]. Infiltration of the muscularis propria may be seen and does not indicate malignancy. Two GCTs in our series displayed unusual features. The sigmoid colon tumor showed a prominent lipomatous component similar to a recently described cecal tumor [19]. The nature of the adipocytic component (pre-existing submucosal lipoma versus adipocytic differentiation) remains obscure. The uniform distribution of adipocytes and absence of stromal reaction suggested a dual differentiation, but this remains speculative. Adipocytic differentiation has been rarely documented in PNSTs of the soft tissue [20]. Furthermore, rare GCTs have shown hyalinization/calcification [21] and osseous metaplasia [22]. The largest GCT in this study originated from the rectal Auerbach plexus as a rectovaginal septum mass. This unusual intramural variant should be distinguished from GIST, in particular from epithelioid GIST with granular cytoplasmic change [23].
Schwannomas comprise 2–7% of mesenchymal GI neoplasms. To date, less than 200 cases have been reported [3–8, 24]. The stomach was the most common site involved followed by the large bowel. The esophagus and the small bowel are only rarely affected. The age distribution, origin in the muscularis propria, and predilection for gastric body are features shared with GISTs. Grossly, schwannomas lack cystic changes and hemorrhages commonly seen in GISTs. A thin marginal halo (corresponding to lymphoid cuffs) seen on endoscopic ultrasound is a helpful feature in their preoperative evaluation [25]. Schwannomas show a mixture of diverse histological patterns. Their separation from GISTs and smooth muscle tumors is facilitated by the typical histology of the latter and by lower cellularity and the prominent lymphoid cuffs in schwannomas. By IHC, schwannomas are uniformly S100-positive, and they do not stain with CD117 [5, 8] and DOG-1 [26], features that help to separate them from GISTs.
Reticular–microcystic schwannoma is a recently defined rare variant with a predilection for visceral sites [27]. Including our two cases, a total of eight cases of this rare variant were reported in the GI tract; three from the large bowel, three from the small bowel, and two from the stomach [27, 28]. The striking predilection of this variant for the intestine contrasts with its rarity in the stomach where most GI schwannomas occur. Compared to usual GI schwannomas, the reticular–microcystic variant presented at higher mean age (75.8 versus 63 years) and showed higher female predilection (3:1 versus 1.5:1). Seven of the eight patients had a median follow-up of 13 months; none developed progressive disease or recurrence.
In this study, we documented the first NF1-associated GI schwannoma. Although it is possible that this might represent a mere coincidence, the occurrence of a neurogenic neoplasm in an NF1-patient is most likely to be considered a manifestation of the disorder. Given the overlapping features of gastric schwannoma with neurofibroma, the fact that many schwannomas in the current study were initially considered neurofibromas, and the high suspicion of neurofibroma in NF1 patients, it is possible that some GI schwannomas in NF1 patients might have been interpreted as neurofibroma [29, 30]. Of interest, intratumoral axons and perineurial cells were detected in GI schwannomas, supporting a neurofibroma-like histogenesis [31]. Moreover, the study by Lasota et al [32] has shown that loss of heterozygosity (LOH) at NF2 was rare in GI schwannomas (5%), and no NF2 mutations could be detected in 13 cases analyzed. Instead, LOH on 17q involving NF1 occurred frequently in GI schwannomas (50%), suggesting a distinct molecular pathogenesis that is more akin to that of plexiform neurofibroma [32]. However, a recent case of gastric schwannoma harbored a mutation in NF2 [33], suggesting that the molecular pathogenesis of GI schwannoma is probably heterogeneous. The absence of calretinin and α-inhibin as additional markers of schwannian differentiation [18, 34] in six of our GI schwannomas represents a further argument for a neurofibroma-like histogenesis.
Although ∼25% of digestive schwannomas were associated with coincidental GI malignancies [3], the concurrence of GI PNSTs with clinically meaningful GISTs seems to be rare with only two previously reported cases [5, 35] and two other cases in the current study including one patient with NF1. However, coexistence of minute incidental gastric GISTs with PNSTs in two of our NF1 patients might represent a mere coincidence, given the high prevalence of incidental gastric GISTs in the general population [36].
Conventional (soft tissue type) perineurioma is rare in the GI tract. Including our case, five GI neoplasms with features of soft tissue perineuriomas [37] have been reported: two in stomach and one each in jejunum, colon, and esophagus [38–40]. Two cases with follow-up (54 and 60 months) showed a benign course [39]. Two further cases with hybrid features of schwannoma–perineurioma were reported from the colon [10, 41]. However, a group of small polypoid mucosal lesions presumed to show peripheral nerve sheath differentiation was the subject of controversy in several recent reports in the literature. They have been reported as mucosal perineurioma [39], fibroblastic polyps [42], mucosal epithelioid nerve sheath tumor [43], and mucosal Schwann cell hamartoma [44]. The nature and the pathogenesis of these lesions and their relationship, if any, to perineurioma remain currently controversial.
MPNST are quite rare in the GI tract, but their real frequency is unknown. We encountered no MPNST in our cases. Recent case reports (∼10 cases) contained no detailed histologic descriptions or microphotographs, making it difficult to rule out sarcomatoid carcinoma and other spindle cell neoplasms [45]. Moreover, it is appreciated that most malignant GI schwannomas preceding the c-KIT era probably represented GIST.
In summary, we reported on a series of PNSTs of the GI tract demonstrating a wider variation in their clinicopathologic profiles and histology including the first NF1-associated GI schwannoma and other unusual histological variants that posed diagnostic challenge. Awareness of the diverse histologic appearance of these mostly benign rare tumors should facilitate their recognition and separation from the more common GI stromal tumors and smooth muscle neoplasms that they may closely mimic both grossly and histologically.
References
Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 23:70–83
Yagihashi S, Kimura M, Kurotaki H et al (1987) Gastric submucosal tumours of neurogenic origin with neuroaxonal and Schwann cell elements. J Pathol 153:41–50
Daimaru Y, Kido H, Hashimoto H et al (1988) Benign schwannoma of the gastrointestinal tract: a clinicopathologic and immunohistochemical study. Hum Pathol 19:257–264
Sarlomo-Rikala M, Miettinen M (1995) Gastric schwannoma—a clinicopathological analysis of six cases. Histopathology 27:355–360
Miettinen M, Shekitka KM, Sobin LH (2001) Schwannomas in the colon and rectum: a clinicopathologic and immunohistochemical study of 20 cases. Am J Surg Pathol 25:846–855
Kwon MS, Lee SS, Ahn GH (2002) Schwannomas of the gastrointestinal tract: clinicopathological features of 12 cases including a case of esophageal tumor compared with those of gastrointestinal stromal tumors and leiomyomas of the gastrointestinal tract. Pathol Res Pract 198:605–613
Goh BK, Chow PK, Kesavan S et al (2008) Intraabdominal schwannomas: a single institution experience. J Gastrointest Surg 12:756–760
Hou YY, Tan YS, Xu JF et al (2006) Schwannoma of the gastrointestinal tract: a clinicopathological, immunohistochemical and ultrastructural study of 33 cases. Histopathology 48:536–545
Chetty R, Vajpeyi R, Penwick JL (2007) Psammomatous melanotic schwannoma presenting as colonic polyps. Virchows Arch 451:717–720
Hornick JL, Bundock EA, Fletcher CD (2009) Hybrid schwannoma/perineurioma: clinicopathologic analysis of 42 distinctive benign nerve sheath tumors. Am J Surg Pathol 33:1554–1561
Scheithauer BW, Woodruff JM, Erlandson RA (1999) Tumors of the peripheral nervous system. In: Rosai J, Sobin LH (eds) Atlas of tumor pathology, 3rd series, fascicle 24. Armed Forces Institute of Pathology, Washington DC
Finkel G, Lane B (1982) Granular cell variant of neurofibromatosis: ultrastructure of benign and malignant tumors. Hum Pathol 13:959–963
Zarineh A, Costa ME, Rabkin MS (2008) Multiple hybrid granular cell tumor-perineuriomas. Am J Surg Pathol 32:1572–1577
Johnston MJ, Helwig EB (1981) Granular cell tumors of the gastrointestinal tract and perianal region: a study of 74 cases. Dig Dis Sci 26:807–816
Parfitt JR, McLean CA, Joseph MG et al (2006) Granular cell tumours of the gastrointestinal tract: expression of nestin and clinicopathological evaluation of 11 patients. Histopathology 48:424–430
Prematilleke IV, Sujendran V, Warren BF et al (2004) Granular cell tumour of the oesophagus mimicking a gastrointestinal stromal tumour on frozen section. Histopathology 44:502–503
Maiorano E, Favia G, Napoli A et al (2000) Cellular heterogeneity of granular cell tumours: a clue to their nature? J Oral Pathol & Med 29:284–290
Fine SW, Li M (2003) Expression of calretinin and the alpha-subunit of inhibin in granular cell tumors. Am J Clin Pathol 119:259–264
Mori T, Orikasa H, Shigematsu T et al (2006) An Ultrastructural and immunohistochemical study of a combined submucosal granular cell tumor and lipoma of the colon showing a unique nodule-in-nodule structure: putative implication of CD34 or prominin-2-positive stromal cells in its histopathogenesis. Virchows Arch 449:137–139
Plaza JA, Wakely PE Jr, Suster S (2006) Lipoblastic nerve sheath tumors: report of a distinctive variant of neural soft tissue neoplasm with adipocytic differentiation. Am J Surg Pathol 30:337–344
Hong R, Lim SC (2009) Granular cell tumor of the cecum with extensive hyalinization and calcification: a case report. World J Gastroenterol 15:3315–3318
Lee KH, Cho JH, Han YW et al (2006) A rare case of ossifying granular cell (Abrikossoff) tumour. Acta Derm Venereol 86:548–549
Adamiak A, Lee CH, Nielsen TO et al (2009) Duodenal epithelioid gastrointestinal stromal tumor with prominent granular cell features. Hum Pathol 40:599–602
Hirasaki S, Kanzaki H, Fujita K et al (2008) Ileal schwannoma developing into ileocolic intussusception. World J Gastroenterol 14:638–640
Jung MK, Jeon SW, Cho CM et al (2008) Gastric schwannomas: endosonographic characteristics. Abdom Imaging 33:388–390
Miettinen M, Wang ZF, Lasota J (2009) DOG1 antibody in the differential diagnosis of gastrointestinal stromal tumors: a study of 1840 cases. Am J Surg Pathol 33:1401–1408
Liegl B, Bennett MW, Fletcher CD (2008) Microcystic/reticular schwannoma: a distinct variant with predilection for visceral locations. Am J Surg Pathol 32:1080–1087
Tozbikian G, Shen R, Suster S (2008) Signet ring cell gastric schwannoma: report of a new distinctive morphological variant. Ann Diagn Pathol 12:146–152
Fuller CE, Williams GT (1991) Gastrointestinal manifestations of type 1 neurofibromatosis (von Recklinghausen's disease). Histopathology 19:1–11
Basile U, Cavallaro G, Polistena A et al (2010) Gastrointestinal and retroperitoneal manifestations of type 1 neurofibromatosis. J Gastrointest Surg 14:186–194
Zámecník M, Mukensnabl P, Sokol L et al (2004) Perineurial cells and nerve axons in gastrointestinal schwannomas: a similarity with neurofibromas. An immunohistochemical study of eight cases. Cesk Patol 40:150–153
Lasota J, Wasag B, Dansonka-Mieszkowska A et al (2003) Evaluation of NF2 and NF1 tumor suppressor genes in distinctive gastrointestinal nerve sheath tumors traditionally diagnosed as benign schwannomas: a study of 20 cases. Lab Invest 83:1361–1371
Ogasawara N, Sasaki M, Ishiguro H et al (2009) Gastric schwannoma with adjacent external progression harbored aberrant NF2 gene. Dig Endosc 21:192–195
Fine SW, McClain SA, Li M (2004) Immunohistochemical staining for calretinin is useful for differentiating schwannomas from neurofibromas. Am J Clin Pathol 122:552–559
Ince AT, Yavuzer D, Kiliç G et al (2008) Coincidental occurrence of granular cell tumor and gastrointestinal stromal tumor in a patient. Turk J Gastroenterol 19:135–136
Agaimy A, Wünsch PH, Hofstaedter F et al (2007) Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. Am J Surg Pathol 31:113–120
Hornick JL, Fletcher CD (2005) Soft tissue perineurioma: clinicopathologic analysis of 81 cases including those with atypical histologic features. Am J Surg Pathol 29:845–858
Agaimy A, Wünsch PH (2005) Perineurioma of the stomach: a rare spindle cell neoplasm that should be distinguished from gastrointestinal stromal tumor. Pathol Res Pract 201:463–467
Hornick JL, Fletcher CD (2005) Intestinal perineuriomas: clinicopathologic definition of a new anatomic subset in a series of 10 cases. Am J Surg Pathol 29:859–865
Kelesidis T, Tarbox A, Lopez M et al (2009) Perineurioma of esophagus: a first case report. Am J Med Sci 338:230–232
Emanuel P, Pertsemlidis DS, Gordon R et al (2006) Benign hybrid perineurioma-schwannoma in the colon. A case report. Ann Diagn Pathol 10:367–370
Groisman GM, Polak-Charcon S (2008) Fibroblastic polyp of the colon and colonic perineurioma: 2 names for a single entity? Am J Surg Pathol 32:1088–1094
Lewin MR, Dilworth HP, Abu Alfa AK et al (2005) Mucosal benign epithelioid nerve sheath tumors. Am J Surg Pathol 29:1310–1315
Gibson JA, Hornick JL (2009) Mucosal Schwann cell "hamartoma": clinicopathologic study of 26 neural colorectal polyps distinct from neurofibromas and mucosal neuromas. Am J Surg Pathol 33:781–787
Telem DA, Pertsemlidis D (2008) Malignant peripheral nerve sheath tumor: an unusual cause of intussusception. J Gastrointest Surg 12:1609–1611
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agaimy, A., Märkl, B., Kitz, J. et al. Peripheral nerve sheath tumors of the gastrointestinal tract: a multicenter study of 58 patients including NF1-associated gastric schwannoma and unusual morphologic variants. Virchows Arch 456, 411–422 (2010). https://doi.org/10.1007/s00428-010-0886-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-010-0886-8