Abstract
Secondary sclerosing cholangitis (SSC) is a chronic cholestatic disorder caused by mechanical, infectious, toxic, or ischemic factors. A new variant of SSC occurring after long-term treatment in intensive care units (ICU) has been recently described and characterized from the clinical point of view. The aim of this study was the histomorphological characterization of ICU-treatment-related SSC (ICU-SSC) and the definition of histological changes occurring over time based on the morphological findings. Liver biopsies of ten patients affected by ICU-SSC obtained at different time points (1.5 to 57 months) after the initial injury were analyzed. The main morphological alterations included degenerative changes of portal bile ducts, portal edema, inflammation, and fibrosis as well as biliary interface activity and bilirubinostasis. Perivenular necroses and bile infarcts were found in eight and six patients, respectively. Bile duct loss was not observed. No correlation between morphological features of biopsies and liver chemistry tests or outcome could be established. Based on the morphological observation, a possible disease-progression model starting with an initial damage of portal bile ducts (primary insult) with associated portal/periportal changes (inflammation, ductular reaction) and resulting in secondary parenchymal changes is proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sclerosing cholangitis is a chronic, variably progressive cholestatic disease affecting the extra- and/or intrahepatic biliary tree with evolution into biliary cirrhosis and cholestatic liver failure [1]. A primary or idiopathic form and a less common secondary, acquired form of sclerosing cholangitis are known, which share similar radiological, morphological, and clinical features. In addition, primary sclerosing cholangitis (PSC) and some forms of secondary sclerosing cholangitis (SSC) belong to the spectrum of liver diseases associated with progressive intrahepatic bile duct loss or ductopenia, usually developing over decades. Most common causes of SSC include infectious, toxic, or ischemic injuries of the biliary tree. Long-standing biliary obstruction of diverse etiologies (stones, benign strictures), often with superimposed suppurative cholangitis, also causes morphological alterations that resemble PSC and may rarely evolve into secondary biliary cirrhosis [2]. Furthermore, autoimmune pancreatocholangitis is an immune-mediated disorder characterized by a PSC-like involvement of the extra- and intrahepatic biliary tract [3]. Recently, a new variant of SSC occurring after long treatment in intensive care units has been described and characterized, mostly from the clinical point of view [4–9]. In the present study, the histomorphological features of rapid-onset secondary sclerosing cholangitis after long-term intensive care unit (ICU) treatment are described. A possible progression model is suggested, and criteria for the histopathological differential diagnosis are proposed.
Materials and methods
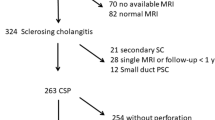
Ten patients (nine men, one woman; median age at diagnosis 52.5, range 16–68 years) affected by ICU-SSC with available needle biopsies of the liver were retrospectively analyzed in this study. The main clinical data are summarized in Table 1. All patients were treated in an intensive care unit for septic shock after an initial insult, and they all required long-term ventilation, catecholamines, total parenteral nutrition, and antibiotics. The alterations in the liver function did not resolve despite successful treatment of the sepsis. The complete clinical characterization of the patients’ collective has been previously published [9]. None of the patients showed elevation of the cholestasis parameters [bilirubin, serum alkaline phosphatase, and γ-glutamyltransferase (GGT)] prior to their admission or on the initial laboratory tests in the ICU.
Liver biopsies had been obtained at admission to the Department of Gastroenterology of the University of Heidelberg 1.5 to 6.5 months (median, 2 months) after injury from patients 1 and 3–10. The liver biopsy of patient 2 was obtained 57 months after injury. A follow-up biopsy was obtained from patient 5 2 weeks after the first one.
Tissue sections obtained from the liver biopsies were retrieved from the archive of the Institute of Pathology of the University of Heidelberg and analyzed for the purposes of the present study by two pathologists (I.E. and P.S.) experienced in biliary and hepatic pathology blinded to detailed clinical information. In addition to conventional hematoxylin and eosin sections, periodic acid–Schiff (PAS)-diastase staining, Gomori’s silver impregnation for reticulin, and Van Gieson’s or Masson’s trichrome staining for connective tissue were available in all cases. Rhodamine-staining for copper was used as a marker of chronic cholestasis. For better demonstration of bile duct status (ductular reaction and metaplasia), immunostaining for cytokeratin (CK) 7 (Dakocytomation, Glostrup, Denmark) was performed according to standard protocols.
The following parameters were taken into account for the histopathological evaluation: total numbers of portal tracts (PT), number of affected PT, portal changes (edema, inflammation, bile duct changes, and fibrosis), acinar changes (hepatocellular changes, necrosis, inflammation, cholestasis, and fibrosis).
All morphological parameters were semiquantitatively assessed on a three-point scale (0 = absent; + = mild/weak; ++ = moderate; +++ = heavy/strong). Continuous variables were stratified according to their median and percentile values for comparison purposes.
Results
Morphological spectrum of ICU-related SSC
The quality of the biopsy material was good in all but one case (patient 3), where significant autolytic changes were present. The median number of portal tracts was 20 (3–28), and in all cases, the majority of them (76–100%) showed histopathological changes. In all cases, mild to moderate portal inflammation was observed. The inflammatory infiltrate mostly consisted of lymphocytes, less frequently of plasma cells and neutrophil granulocytes, which showed preferential periductal localization. In four cases, eosinophils were present. Portal inflammation was accompanied in all cases by edema with portal enlargement, as well as by a number of alterations of the interlobular bile duct epithelium, which included cytoplasmic vacuolization, loss of cellular polarity, cellular drop-out, and irregularities of the basal membrane. Mild to heavy ductular reaction—that is, the presence of numerous ductular-shaped structures at the margins of the portal tracts—was found in all cases, together with a mostly mild to moderate ductular metaplasia of the periportal hepatocytes [10], as demonstrated in eight of ten cases by means of immunostaining for CK7. Mild to moderate portal fibrosis was present in all cases, but it was never concentric around ducts or ductules. There was no evidence of definite bile duct loss or even ductopenia. Lymph follicles, granulomas, or lymphocytic interface activity was not observed. Portal changes were associated with mild to strong hepatocellular bilirubinostasis in nine of ten cases, canalicular bilirubinostasis in six of ten cases, perivenular hepatocyte ballooning in four of ten cases, focal perivenular necroses in eight of ten cases, and preferentially periportal bile infarcts in six of ten cases. Periportal hepatocytes showed morphological features of cholate stasis. However, rhodamine staining did not show copper accumulation (not shown). Broad fibrous septa linking portal tracts were found in four of ten cases. No patient showed overt liver cirrhosis. The observed changes are shown in detail in Table 2 and are illustrated in Fig. 1.
Morphological characteristics of ICU-associated secondary sclerosing cholangitis. a–d Portal changes. a (Case 5) Low-power view of a portal tract showing marked enlargement due to edema, mild inflammation, and mild fibrosis. At the periphery of the portal tract, dilated cholangioli are seen (arrows), some of them containing yellow bile plugs (×25). b (Case 5) Higher magnification of a portal tract illustrating the relatively mild inflammatory infiltrate contrasting with the striking degenerative changes of the interlobular bile duct (arrow; ×100). c (Case 5) Degenerative changes of the bile duct epithelium are shown in detail (×400). d (Case 4) Another example of portal tract changes in ICU-related SSC. Portal tract expansion with mild inflammation, degenerative changes of the interlobular bile duct, and beginning ductular reaction are shown (×100). e–h Parenchymal changes. e (Case 3) Hepatocellular and canalicular cholestasis (×200). f (Case 6) Periportal bile infarct (arrows; ×100). g and h (Cases 5 and 7) Perivenular loss of hepatocytes. The central vein is indicated with an asterisk (×100). i–l Later stages. i–k (Case 2) Extensive fibrosis with bridges linking portal tracts is evident in the Masson’s trichrome staining (i ×25). The prominent ductular reaction is highlighted in the PAS staining (j ×100) and in the immunostaining for CK7 (k ×100). l (Case 8) Immunostaining for CK7 showing extensive ductular reaction and ductular metaplasia of periportal hepatocytes (×25)
Clinicopathological correlations
First, possible correlations between liver chemistry values and morphological changes were analyzed. Liver chemistry tests suggested a predominant cholestatic or a mixed cholestatic/hepatocellular damage [11]. In general, no definitive correlation was observed between serological cholestasis parameters and the morphological representation of cholestasis. For instance, patient 2 had a strong increase in the serum levels of alkaline phosphatase but no morphological evidence of cholestasis, whereas patient 10 had only a modest to moderate increase in the level of total bilirubin and alkaline phosphatase, but the liver biopsy showed a moderate to severe hepatocellular and canalicular cholestasis. Also, no evident correlation was found between the hepatocellular damage expressed by the elevation in the serum transaminases and the morphological evidence of liver cell damage (ballooning, necrosis). For instance, patients 6 and 10 had the lowest transaminase levels of the whole cohort at the time of biopsy, but the examination of the liver tissue revealed the presence of perivenular necroses and bile infarcts in both cases. On the other hand, patient 3 had a significant increase in the serum transaminases [alanine aminotransferase (ALT) seven times the upper limit of the normal value] but only mild (+) perivenular necroses.
Since biopsies from different patients were obtained at different time intervals from the injury event that caused ICU treatment, we next sought to determine if a correlation between morphological changes and clinical progression/outcome existed. For this purpose, liver biopsies were classified as “early” when obtained <1.8 months from the injury event (<25th percentile, patients 5, 6, and 7), as “intermediate” when obtained between 1.8 and 4.6 months from the injury event (26–74th percentile, patients 3, 4, 9, and 10) and as “late” when obtained later than 4.6 months from the injury event (>75th percentile, patients 1, 2, and 8). All patients displayed evident alterations of the portal bile ducts and some degree of portal inflammation, together with mild to moderate portal fibrosis. Instead, morphological evidence of cholestasis and necrosis was not a constant finding, but no clear correlation with the clinical evolution and/or the outcome was found. However, most of the tissue probes were obtained between 1.5 and 6.5 months from the injury event, a time span which could be too short to detect any clear morphological markers of disease progression and outcome. Nevertheless, the analysis of the liver tissues of patient 5, which were obtained with a 2-week interval from each other, revealed signs of progression in the cholestatic and necrotic features (appearance of ductular metaplasia, as shown in the CK7 staining, and of bile infarcts) as well as in the fibrotic reaction (bridges) in the later biopsy. Moreover, the analysis of a “very late” biopsy, like that of patient 2, which was obtained almost 6 years after the injury event, shows that slow progression to liver cirrhosis of biliary type can be one possible outcome of the disease, which otherwise rapidly progresses to cholestatic liver insufficiency.
Discussion
Secondary sclerosing cholangitis occurring in critically ill patients after ICU treatment is a recently described, still not well-characterized entity [5–8] that has to be included in the differential diagnosis of chronic cholestatic diseases. In the reported series, including our present, patients affected by ICU-SSC have a history of long-term intensive care treatment with necessity of mechanical ventilation and catecholamine therapy as a consequence of trauma, severe burning, cardiovascular accidents, or major cardiovascular and abdominal surgery. Hypoxic/ischemic, toxic (infectious and drug-related), and obstructive factors are likely to play a role in the multifactorial pathogenesis of ICU-SSC [12], but the contribution of primary and secondary causative factors remains difficult and eventually impossible to evaluate in a given case. The formation of biliary casts with subsequent bacterial infection has been reported as one of the earliest events in ICU-SSC, but its cause remains still elusive. One of the most accredited hypotheses identifies the hypoxic/ischemic damage of the intrahepatic biliary tree, following hypotension, reduced arterial blood oxygenation, and infusion of high doses of vasoconstrictors as the most probable etiologic factor [6, 8]. All these factors are also involved in the pathogenesis of sepsis-associated cholestasis, which is attributed to functional alterations of the hepatocytes and/or the bile ducts and is reversible after successful therapy [12]. ICU-SSC is instead a progressive disease, where an anatomical—and not merely functional—damage of the biliary tree is possibly perpetuated by (auto)immunological mechanisms that become activated only in a subset of patients. Since ICU-SSC has been described only in recent years, it is possible that modern measures of intensive care treatment play a role in the etiopathogenesis of this disorder, but specific factors have not been identified yet [8].
In this study, we focused on the morphological characterization of ICU-SSC, aiming at defining criteria supporting the histopathological differential diagnosis, a possible progression model, and potential clinicopathological correlations that may be of relevance for the clinical management. The observed morphological changes can be divided in those affecting the portal/periportal and the acinar areas. The portal alterations include: (1) inflammatory-degenerative changes of the bile duct; (2) mild to moderate, often periductal inflammatory infiltrate; (3) portal edema with moderate portal enlargement; (4) cholestatic features with ductular reaction and cholate stasis; and (5) mild to moderate fibrosis without a specific periductal pattern. The acinar changes appear to be secondary and include: hepatocellular and/or canalicular cholestasis, perivenular necroses potentially attributable to ischemia, and bile infarcts. The alterations of portal bile ducts, together with a certain degree of portal inflammation and ductular reaction, were a constant finding, being already detectable in early biopsies and uniformly distributed within a biopsy. On the other hand, periportal and acinar changes, such as cholate stasis, bilirubinostasis, necroses, and (bridging) fibrosis were more inconstant and possibly (for example in patient 5) progressive events. Based on this morphological observation, a disease-progression model, starting with an initial damage of portal bile ducts (primary insult) with associated portal/periportal changes (inflammation, ductular proliferation) and evolving with secondary cholestatic parenchymal changes, is suggested (Fig. 2). However, larger numbers of patients and examination of tissue specimens at different time points in the evolution of ICU-SSC are surely needed to give further support to this hypothesis.
Schematic representation of the proposed disease progression model. An initial insult to the portal bile ducts (flash) causes degenerative changes of the bile duct epithelium (e.g., cytoplasmic vacuolization, loss of nuclear polarization) and portal changes (enlargement due to edema and inflammation, ductular proliferation) and progresses to secondary parenchymal changes, such as bilirubinostasis, hepatocellular rosette formation, and cholestatic necroses
Some morphologic characteristics associated with ICU-SSC have in part been described in previous studies and correlate well with our findings. In two of the three cases reported by Scheppach et al., a liver biopsy was performed 8 and 11 months after initial symptoms, respectively, and in both cases, ductular proliferation and bridging fibrosis were present. The third patient underwent liver transplantation, and the examination of the explanted organ showed PSC-like changes, including ulceration of the epithelium of large intrahepatic bile ducts, which were filled with bile plugs [4]. Engler et al. reported ductular proliferation, minimal portal inflammatory infiltrates, and portal fibrosis in the biopsies of seven patients; in three of them, micronodular cirrhosis was found [5]. Liver biopsies were performed at different time points in the series of Benninger et al. Four to 6 months after clinical presentation, morphological signs of chronic cholestasis and fibrosis were present, whereas later biopsies (12–24 months after injury) showed overt cirrhosis in two out of three patients [6]. Changes consistent with chronic bile duct obstruction have been described in four patients already 1–3 months after clinical presentation by Gelbmann et al., and incomplete liver cirrhosis was present in one of two patients, who were biopsied >12 months after injury. Moreover, liver explants examined 1, 2, 9, and 16 months after injury showed morphological alterations suggesting secondary biliary cirrhosis [8]. All together, our and previous data show that morphological changes associated with ICU-SSC are comparable, with signs of bile duct damage and chronic cholestasis being already evident shortly after the clinical presentation. The evolution of the disease remains, however, quite unpredictable, with some cases rapidly developing into cholestatic liver failure and death and others more slowly progressing into secondary biliary cirrhosis. The factors that influence the outcome are not completely clarified, but comorbidities surely play an important role in these seriously ill patients. The absence of a correlation between laboratory values and morphological evidence of cholestasis is a known phenomenon in primary biliary diseases, such as PSC or primary biliary cirrhosis, where—especially in early stages—morphological changes can be focal and unevenly distributed.
Patients’ history and clinical presentation are certainly fundamental for the diagnosis of ICU-SSC and for the exclusion of pre-existent liver disease (e.g., PSC) as well as of other systemic conditions (e.g., AIDS, neoplastic diseases) that can cause SSC. Nevertheless, morphology is helpful in distinguishing ICU-SSC from other disorders. Septicemia-associated cholestasis is an important differential diagnosis of ICU-SSC, since the clinical context of the two conditions can be the same. Histological changes associated with sepsis-induced cholestasis can be unspecific (portal inflammation, perivenular bilirubinostasis) and therefore indistinguishable from early stages of ICU-SSC, as those described by Gelbmann et al. [8]. However, the so-called cholangiolitis lenta, arising in patients with severe septic/endotoxic shock, usually shows a predominantly peri- and intraductular neutrophilic infiltrate and a rapid and extensive ductular reaction with prominent ductular bilirubinostasis [13], features that are usually not observed in ICU-SSC. Large bile duct obstruction also shares similar morphological features with ICU-SSC, but the primary bile duct damage (i.e., with no or only mild inflammation) is usually not as prominent as in ICU-SSC, while portal edema and ductular reaction are typical, and suppurative cholangitis of pre-existing bile ducts may occur. Drug-induced bile duct injury may be difficult to distinguish from ICU-SSC, since drugs may actually contribute to the severity and progression of this disorder. An accurate clinical evaluation of ICU patients with signs of cholestasis should therefore always take into consideration the possibility of drug-induced bile duct damage.
Other chronic cholestatic conditions that might be distinguished from ICU-SSC are autoimmune pancreatocholangitis/IgG4-hepatopathy and idiopathic adulthood ductopenia. Intrahepatic manifestations of autoimmune pancreatocholangitis/IgG4-hepatopathy, in particular those patterns with features of large bile duct obstruction or canalicular cholestasis [14], can be excluded by the absence of an infiltrate rich in IgG4-bearing plasma cells and of prominent periductal sclerosis. Idiopathic adulthood ductopenia is characterized by bile duct loss, a feature that is not observed early on in ICU-SSC.
In conclusion, ICU-SSC is a chronic cholestatic disease characterized by relatively specific morphological changes of the liver, consisting of degenerative changes of the interlobular bile duct epithelium with only mild accompanying chronic inflammatory reaction and usually severe cholestasis. Liver biopsy is useful in the differential diagnosis of ICU-SSC in the appropriate clinical context. Possible correlation between morphological changes and outcome should be verified on a larger number of patients.
References
Maggs JR, Chapman RW (2007) Sclerosing cholangitis. Curr Opin Gastroenterol 23:310–316
Abdalian R, Heathcote EJ (2006) Sclerosing cholangitis: a focus on secondary causes. Hepatology 44:1063–1074
Bjornsson E, Chari ST, Smyrk TC et al (2007) Immunoglobulin G4 associated cholangitis: description of an emerging clinical entity based on review of the literature. Hepatology 45:1547–1554
Scheppach W, Druge G, Wittenberg G et al (2001) Sclerosing cholangitis and liver cirrhosis after extrabiliary infections: report on three cases. Crit Care Med 29:438–441
Engler S, Elsing C, Flechtenmacher C et al (2003) Progressive sclerosing cholangitis after septic shock: a new variant of vanishing bile duct disorders. Gut 52:688–693
Benninger J, Grobholz R, Oeztuerk Y et al (2005) Sclerosing cholangitis following severe trauma: description of a remarkable disease entity with emphasis on possible pathophysiologic mechanisms. World J Gastroenterol 11:4199–4205
Jaeger C, Mayer G, Henrich R et al (2006) Secondary sclerosing cholangitis after long-term treatment in an intensive care unit: clinical presentation, endoscopic findings, treatment, and follow-up. Endoscopy 38:730–734
Gelbmann CM, Rummele P, Wimmer M et al (2007) Ischemic-like cholangiopathy with secondary sclerosing cholangitis in critically ill patients. Am J Gastroenterol 102:1221–1229
Kulaksiz H, Heuberger D, Engler S et al (2008) Poor outcome in progressive sclerosing cholangitis after septic shock. Endoscopy 40:214–218
Van Eyken P, Sciot R, Desmet VJ (1989) A cytokeratin immunohistochemical study of cholestatic liver disease: evidence that hepatocytes can express ‘bile duct-type’ cytokeratins. Histopathology 15:125–135
Green RM, Flamm S (2002) AGA technical review on the evaluation of liver chemistry tests. Gastroenterology 123:1367–1384
Geier A, Fickert P, Trauner M (2006) Mechanisms of disease: mechanisms and clinical implications of cholestasis in sepsis. Nat Clin Pract Gastroenterol Hepatol 3:574–585
Lefkowitch JH (1982) Bile ductular cholestasis: an ominous histopathologic sign related to sepsis and "cholangitis lenta". Hum Pathol 13:19–24
Umemura T, Zen Y, Hamano H et al (2007) Immunoglobin G4-hepatopathy: association of immunoglobin G4-bearing plasma cells in liver with autoimmune pancreatitis. Hepatology 46:463–471
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Esposito, I., Kubisova, A., Stiehl, A. et al. Secondary sclerosing cholangitis after intensive care unit treatment: clues to the histopathological differential diagnosis. Virchows Arch 453, 339–345 (2008). https://doi.org/10.1007/s00428-008-0654-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-008-0654-1