Abstract
Multiple voltage-gated calcium channels (VGCCs) contribute to the processing of nociceptive signals in primary afferent fibers. In addition, alteration of calcium channel activity is associated with a number of chronic pain conditions. Therefore, VGCCs have emerged as prime target for the management of either neuropathic or inflammatory pain, and selective calcium channel blockers have been shown to have efficacy in animal models and in the clinic. However, considering that multiple calcium channels contribute pain afferent signaling, broad-spectrum inhibitors of several channel isoforms may offer a net advantage in modulating pain. Here, we have analyzed the ability of the compound surfen to modulate calcium channels, and assessed its analgesic potential. We show that surfen is an equipotent blocker of both low- and high-voltage-activated calcium channels. Furthermore, spinal (intrathecal) delivery of surfen to mice produces sustained analgesia against both acute and chronic pain. Collectively, our data establish surfen as a broad-spectrum calcium channel inhibitor with analgesic potential, and raise the possibility of using surfen-derived compounds for the development of new pain-relieving drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Voltage-gated calcium channels (VGCCs) are essential contributors to the processing of peripheral nociceptive information within neurons of the dorsal root ganglion (DRG) [4, 60]. Among the various VGCCs expressed in DRG neurons [33, 47, 57, 67], the high-voltage-activated (HVA) Cav2.2 (N-type) and low-voltage-activated (LVA) Cav3.2 (T-type) channels are the main calcium channels isoforms that mediate processing of the pain signals. For instance, Cav2.2 channels are predominantly expressed in presynaptic terminals of afferent nerve fibers where they support evoked release of pronociceptive neurotransmitters such as glutamate, substance P and calcitonin gene-related peptide (CGRP) [7, 29, 45, 49]. In contrast, Cav3.2 channels are expressed along axons where they possibly regulate the excitability of afferent fibers via their electrogenic function that may facilitate the opening of voltage-gated sodium channels [16]. In addition, Cav3.2 channels expressed in nerve endings in skin hair follicles [42] are essential for mechanotransduction [8, 15], and contribute to mechanical allodynia [35]. Finally, Cav3.2 channels also contribute to excitatory synaptic transmission in the dorsal horn of the spinal cord [19], possibly by supporting low-threshold release of neurotransmitters by virtue of their interaction with the synaptic vesicle release machinery [61, 62]. Consequently, Cav2.2 and Cav3.2 channels play a major role in the development and maintenance of neuropathic pain, and have thus emerged as prime targets for its treatment [38, 68]. In addition, there is also evidence for a role of other VGCC members. For instance, Cav1.2 and Cav1.3 channels (L-type) are present in neurons of the dorsal horn of the spinal cord [6, 52] where they contribute to sensitization to pain [41]. Moreover, a role for Cav2.3 channels (R-type) in the spinal transmission of the pain signal was also reported [31, 55], along with a role for Cav3.3 channels [64]. Given that multiple calcium channels contribute to the processing of peripheral pain signaling, broad-spectrum inhibitors of VGCCs may represent an effective mean of mediating analgesia.
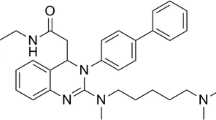
Surfen (bis-2-methyl-4-amino-quinolyl-6-carbamide) was first described in the late thirties as a byproduct in the production of depot insulin [58], and was later reported to block C5a receptor binding [24] and to inhibit anthrax lethal factor [36]. More recently, surfen was shown to inhibit heparan sulfate [46, 63]. Here, we report that surfen is a potent, broad-spectrum inhibitor of VGCCs. An electrophysiological analysis indicates that surfen effectively inhibits recombinant and native VGCC channels in DRG neurons. In addition, our results reveal that surfen produces sustained analgesia when delivered intrathecally in mouse models of acute and chronic inflammatory pain.
Materials and methods
Cell culture and heterologous expression
Human embryonic kidney tsA-201 cells were gown in DMEM medium supplemented with 10% fetal bovine serum (FBS) and 1% streptomycin/penicillin (all media from Invitrogen), and maintained under standard conditions at 37 °C in a humidified atmosphere containing 5% CO2. Cells were plated out onto 60 mm dishes and transfected using the calcium/phosphate method with cDNAs encoding human Cav1.2 or Cav2.1 channels along with β1b and α2δ-1. Human Cav3.2 and Cav3.3 channels were expressed alone as previously described [25]. The CHO cell line stably transfected with rat Cav2.2-EGFP/α2δ-1/β was previously described [30] and grown in MEM alpha medium supplemented with 10% FBS, 200 mM L-glutamine, 0.7 mg/ml G418, 0.25 mg/ml hygromycin B and 0.005 mg/ml blasticidin.
DRG neuron culture
DRG neurons from 5- to 6-week-old mice were dissociated enzymatically with 0.7 mg/ml collagenase (Sigma-Aldrich) and 5 mg/mL trypsin-EDTA (Thermo-Fisher) in HBSS for 1 h at 37 °C, followed by mechanical trituration with fire-polished Paster pipette. Cells were seeded in 35 mm dishes coated with Poly-L-Lysine (Sigma-Aldrich) in DMEM medium supplemented with 10% FBS and penicillin-streptomycin (Thermo-Fisher).
Patch-clamp electrophysiology
Recording of barium currents in the whole-cell configuration of the patch-clamp technique in tsA-201 cells expressing various calcium channels was performed 72 h after transfection in a bath solution containing (in millimolar): 5 BaCl2, 5 KCl, 1 MgCl2, 128 NaCl, 10 TEA-Cl, 10 D-glucose, 10 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) (pH 7.2 with NaOH). Patch pipettes had a resistance of 2–4 MΩ when filled with a solution containing (in millimolar): 110 CsCl, 3 Mg-ATP, 0.5 Na-GTP, 2.5 MgCl2, 5 D-glucose, 10 EGTA, and 10 HEPES (pH 7.4 with CsOH). Whole-cell patch-clamp recordings were performed using an Axopatch 200B amplifier (Axon Instruments). Acquisition and analysis were performed using pClamp 10 and Clampfit 10 software, respectively (Axon Instruments). Ba2+ currents were recorded in response to depolarizing steps to various potentials applied every 5 or 10 s from a holding potential of −100 or −80 mV for LVA and HVA channels, respectively. The linear leak component of the current was corrected online and current traces were digitized at 10 kHz, and filtered at 2 kHz. The voltage dependence of the peak Ba2+ current density was fitted with the following modified Boltzmann equation:
with I(V) being the peak current amplitude at the command potential V, Gmax the maximum conductance, Vrev the reversal potential, V 0.5 the half-activation potential, and k the slope factor.
The steady-state voltage dependence of inactivation of the Ba2+ current was determined by measuring the peak current amplitude in response to a 150 ms-long depolarizing step to +10 mV (Cav2.2) or −20 mV (Cav3.2) applied after a 5-s-long conditioning prepulse at various voltages. The current amplitude obtained during each test pulse was normalized to the maximum at −80 mV (Cav2.2) or −100 mV (Cav3.2) and plotted as a function of the prepulse potential. The voltage dependence of the steady-state inactivation was fitted with the following two-state Boltzmann function:
with I max corresponding to the maximal peak current amplitude and V 0.5 to the half-inactivation voltage.
Recording of calcium currents in primary DRG neurons was performed after 24 h in culture and elicited with a ramp command (0.5 V/s) from a holding potential of −90 mV as previously described [5]. For recording of Nav currents, the bath solution contained (in millimolar): 35 NaCl, 30 TEA-Cl, 65 choline-Cl, 5 MgCl2, 10 HEPES, 10 D-glucose, and 0.05 CdCl2 (pH 7.2). The pipette solution contained (in millimolar): 100 CsCl, 40 TEA-Cl, 5 NaCl, 1 CaCl2, 2 MgCl2, 11 EGTA, 10 HEPES, 2 Mg-ATP, and 1 Li2GTP (pH 7.2). For recording of K v currents, the bath solution contained (in millimolar): 140 choline-Cl, 4 KCl, 1 MgCl2, 1.8 CaCl2, 0.1 CdCl2, 10 D-glucose, and 10 HEPES (pH 7.2). The pipette solution contained (in millimolar): 140 KCl, 4 NaCl, 1 MgCl2, 10 EGTA, 2 Na2-ATP, and 10 HEPES (pH 7.2). All experiments were performed at room temperature (22–24 °C).
Animals and surfen treatment
All experiments were approved by the Institutional Care and Use Committee and carried out according the guidelines of the Internal Association for the Study of Pain. Efforts were made to minimize animal suffering and distress. Adult (7–9 weeks old) male C57BL/6 J mice were kept on a 12 h light/dark cycle at a maximum of five per cage in a room maintained at 23 ± 1 °C with ad libitum access to food and water. To verify if surfen produces antinociception when delivered spinally to mice, intrathecal (i.t.) injections were performed using volumes of 10 μl and according the method described by Hilden and Wilcox [18] and as routinely performed in our laboratory [10, 11]. Control groups were assessed simultaneously. Surfen was dissolved in 1% or less DMSO, whereas control animals received PBS +1% DMSO (which was the concentration of DMSO in the highest dose delivered to mice in the formalin test). Each mouse was tested only once.
Formalin test
Formalin-induced acute pain was performed as originally described [17]. After a period of at least 60 min acclimation, mice were injected intraplantarily (i.pl.) in the ventral surface of the right hindpaw with 20 μL of a formalin solution (1.25%) prepared in PBS. Immediately after intraplantarily injection of formalin, mice were placed individually into observation chambers and monitored for the time spent licking of biting the injected paw as a mean to assess nocifensive response. Animals were observed from 0 to 5 min and 15 to 30 min to assess acute nociceptive and inflammatory phases, respectively. Surfen was delivered intrathecally (i.t.) 20 min prior injection of formalin and its effect against both nociceptive and inflammatory phases was evaluated.
Persistent inflammatory pain induced by CFA
To induce thermal hyperalgesia caused by peripheral inflammation, animals received 20 μl of CFA injected i.pl. in the right hind paw as performed previously [10]. Sham groups received 20 μl of PBS in the ipsilateral paw. Animals were treated with either surfen (10 μg/i.t.) or vehicle (10 μl/i.t.) 2 days following CFA injection and their thermal withdrawal threshold was subsequently tested.
Measurement of thermal hyperalgesia
Immediately before receiving CFA (baselines) and 2 days after CFA injection (time-course testing day), animals were accessed on a plantar test apparatus (Hargreaves, UgoBasile, Varese, Italy) and the latency to withdrawal the right hindpaws from an infra-red radiant heat (IR = 30%) was scored. Mice were kept individually in enclosed testing chambers (10 cm × 10 cm × 13 cm, length × width × height) placed on top of a glass floor and were allowed to acclimate before testing for at least 120 min. The infra-red heat source was placed underneath the right hind paw and three measurements were taken for each mouse. The cut-off time was set at 30 s to avoid tissue damage.
Chemicals
All chemicals were purchased from Sigma-Aldrich. Surfen (Sigma S6951) was dissolved in DMSO to prepare a stock solution of 10 mM, and was diluted in the external recording solution prior to the experiments so that the final concentration of DMSO was 0.1% or less. Pertussis toxin (PTX) was dissolved in distilled water and applied to the cell at 1 μg/ml for 24 h. The PLC inhibitor U73122 was dissolved in DMSO to prepare a stock solution of 5 mM and applied to the cells at 10 μM for 30 min.
Statistical analysis
Statistical significance for electrophysiology data was determined using a paired or unpaired Student’s t test. For behavioral analysis, data were evaluated by one-way or two-way ANOVA followed by Tukey’s test. All data are presented as mean ± standard error. Value of p ≤ 0.05 was considered to be significant (*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001).
Results
Surfen is an effective inhibitor of voltage-gated calcium channels
We performed whole-cell patch-clamp recordings to assess the ability of surfen to mediate tonic block of various recombinant VGCCs involved in pain transmission. Representative current traces recorded for HVA channels (Cav1.2, Cav2.1, and Cav2.2) and LVA channels (Cav3.2 and Cav3.3) are shown in Fig. 1b before (black traces) and after (gray traces) application of 10 μM surfen. Application of surfen produced robust current inhibition of all calcium channels tested (ranging from 69 ± 2% for Cav2.2 to 84 ± 2% for Cav3.2) (Fig. 1c). We next further analyzed the blocking properties of surfen on the two main calcium channel isoforms (Cav2.2 and Cav3.2) involved in the processing of peripheral nociceptive information. The dose-response relation for block of Cav2.2 and Cav3.2 channels is shown in Fig. 2a, b, respectively. The IC50 values obtained from the fit of the dose-response curves were 1.3 and 2.7 μM for Cav2.2 and Cav3.2 channels, respectively, and did not significantly differ (p = 0.2564). The Hill coefficients were 0.6 and 0.4 for Cav2.2 and Cav3.2 (p = 0.5796), respectively, and in both cases (and in particular for Cav2.2) block appeared to be incomplete at a saturating concentration. The effect of surfen on the voltage dependence of Cav2.2 and Cav3.2 is shown in Fig. 2c, d, respectively. At a concentration of 10 μM, surfen blocked Cav2.2 and Cav3.2 channels at all test potentials, but did not significantly alter the mean half-activation potential (−6.5 ± 0.5 mV versus 0.9 ± 1.6 mV, n = 10 for Cav2.2 channels, and −47.1 ± 1.9 mV versus − 45.6 ± 6.5 mV, n = 9 for Cav3.2 channels). Similarly, there was no significant difference in the mean half-steady-state inactivation potential (−26.3 ± 0.5 mV versus − 26.5 ± 1.0 mV, n = 7 for Cav2.2 channels, and −71.7 ± 0.8 mV versus − 70.7 ± 0.9 mV, n = 10 for Cav3.2 channels) (Fig. 2e, f, respectively). The time course of inhibition at 10 μM for both Cav2.2 and Cav3.2 channels is presented in Fig. 2g, h, respectively, and required approximately 3–4 min to reach a steady-state block. The inhibition was irreversible and we did not observe obvious differences in the time course of inhibition at lower concentrations of surfen (data not shown).
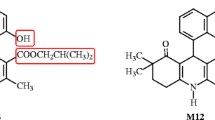
Surfen blocks multiple recombinant voltage-gated calcium channels. a Molecular structure of surfen. b Representative whole-cell current traces recorded from cells expressing recombinant HVA (Cav1.2, Cav2.1, and Cav2.2) and LVA (Cav3.2 and Cav3.3) in response to a step depolarization to −20 mV (LVA) or +10 mV (HVA) from a holding potential of −90 mV, before (black traces) and after external application of 10 μM surfen (gray traces). Scale 20 ms (x-axis)/200 pA (y-axis). c Corresponding mean percentage of tonic current inhibition
Pharmacological properties of surfen on Cav2.2 and Cav3.2 channels. a, b Dose-response relation for surfen inhibition of Cav2.2 (a) and Cav3.2 (b) channels. Fits of the Hill equation gave mean values for IC50 and Hill coefficient of 1.3 μM, 0.6 and 2.7 μM, 0.4 for Cav2.2 and Cav3.2 channels, respectively. c, d Mean current-voltage relation for Cav2.2 (c) and Cav3.2 (d) channels before (filled circles) and after application of 10 μM surfen (open circles). e, f Ensemble steady-state inactivation curves for Cav2.2 (e) and Cav3.2 (f) channels before (filled circles) and after application of 10 μM surfen (open circles). g, h Time course of Cav2.2 (c) and Cav3.2 (f) channel inhibition during external application of 10 μM surfen
To analyze the pharmacological properties of surfen under more physiological conditions, we assessed the ability of surfen to block native calcium channels in adult mouse DRG neurons. Patch-clamp recordings were performed on small DRG neurons (15–30 μm diameter) corresponding to unmyelinated nociceptive C fibers [65]. Representative current traces elicited by a ramp command (0.5 V/s) from a holding potential of −90 mV are shown in Fig. 3a before (black traces) and after application of 10 μM surfen (gray traces). Consistent with previous studies [3], we observed different electrophysiological profiles of small DRG neurons. A subset of cells displayed a combination of LVA and HVA currents (Fig. 3a, left panel), and application of surfen potently blocked both current components by 58 ± 4% (n = 7) and 69 ± 7% (n = 7), respectively (Fig. 3b, left side). The remaining cells exclusively expressed HVA currents (Fig. 3a, right panel) that were blocked by 64 ± 3% (n = 9) (Fig. 3b, right side). In contrast, we observed only a moderate block of voltage-gated sodium currents (Nav) by 20 ± 5% (n = 5) (Fig. 3c, left panel, and Fig. 3d) and of voltage-gated potassium currents (Kv) by 11 ± 4% (n = 5) (Fig. 3c, right panel, and Fig. 3d).
Surfen blocks native calcium channels in DRG neurons. a Representative calcium current traces recorded from small DRG neurons in response to a ramp command (0.5 V/s) from a holding potential of −90 mV before (black trace) and after application of 10 μM surfen (gray trace). A subset of neurons displayed both LVA and HVA currents (left panel) while the remaining cells presented only HVA currents (right panel). b Corresponding mean percentage of tonic current inhibition for cells displaying LVA and HVA currents (left side) and cells displaying HVA current only (right side). c Representative sodium (Nav, left panel) and potassium (K v , right panel) current traces elicited by a step depolarization from a holding potential of −90 mV before (black traces) and after application of 10 μM surfen (gray trace). d Corresponding mean percentage of tonic block of Nav and K v currents
Altogether, these results indicate that surfen is a preferential broad-spectrum inhibitor of recombinant and native voltage-gated calcium channels in nociceptive neurons, with comparatively moderate effects on voltage-gated sodium and potassium channels.
Surfen-mediated inhibition of calcium channels does not rely on G-protein signaling
We next conducted a series of analysis in order to investigate the mechanisms behind surfen-induced imbibition of calcium channels. It was previously reported that surfen triggers Gβγ- and phospholipase C (PLC)-depend signaling by releasing Gβγ dimers from Gα-bound GDP without activating either G-protein coupled receptors (GPCRs) or Gα subunits and their downstream pathways [53]. Considering that one of the main mechanisms by which GPCRs modulate neuronal Cav2 calcium channels involves the activation of Gβγ [39], we explored the possibility that this regulation could support surfen-mediated inhibition of the channels. Direct inhibition of neuronal calcium channels by Gβγ dimers is typically assessed with a double pulse protocol where a conditioning prepulse to depolarized potentials relieves most of the inhibition (facilitation) [39]. Hence, we recorded Cav2.2 currents before (P1) and after (P2) application of a depolarizing prepulse (PP) to +100 mV to assess the implication of Gβγ in surfen-mediated inhibition of the channel. Representative current traces before (black trace) and after application of 10 μM surfen (gray trace) are shown in Fig. 4a. In control condition, application of a depolarizing prepulse produced a small current facilitation suggesting the existence of a slight tonic blockade of the channel likely caused by basal G-protein activity (Fig. 4a black trace and Fig. 4b). However, we did not observe any prepulse facilitation under surfen inhibition indicating that surfen-induced inhibition of Cav2.2 is voltage-independent ruling out a direct G-protein βγ-mediated inhibition of the channel (Fig. 4a gray trace and Fig. 4b). Consistent with this notion, pre-treatment of cells with pertussis toxin (PTX) for 24 h did not alter the ability of surfen to block Cav2.2 channels (Fig. 4c, d), indicating that Gi/o-coupled receptor signaling is not involved in surfen-mediated inhibition of the channels. Furthermore, pre-treatment of cells with the PLC inhibitor U73122 for 30 min had no effect on surfen-mediated inhibition of Cav2.2 channels (Fig. 4c, d).
Surfen-mediated inhibition of calcium channels does not involved Gβγ- and PLC-dependent signaling. a Representative Cav2.2 current traces recorded before (P1) and after (P2) application of a depolarizing prepulse (PP) to +100 mV in control (black trace) and surfen condition (10 μM). b Corresponding mean P2/P1 current ratios. c Representative current traces before (black traces) and after application of 10 μM surfen (gray traces) in control cells (left panel) and in cells pre-treated with PTX (middle panel) and PLC inhibitor U73122 (right panel). d Corresponding mean percentage of tonic current inhibition
Surfen mediates analgesia in acute and chronic inflammatory pain models
To evaluate the analgesic potential of surfen, we assessed the effect of the molecule against both nociceptive (phase 1) and inflammatory (phase 2) responses after formalin injection. Intrathecal (i.t.) injection of surfen produced effective and dose-dependent inhibition of nocifensive responses in both phases of the formalin test, such that injection of 10 μg/i.t. of surfen, 20 min before the injection of formalin, caused significant inhibition of the first phase by 55 ± 5% (Fig. 5a), and second phase by 77 ± 6% (Fig. 5b). Considering that surfen was highly effective in inhibiting the acute nocifensive response in the inflammatory phase of the formalin test, we further analyzed the analgesic potential of surfen on CFA-induced persistent inflammatory nociception. The ability of surfen to modulate CFA-induced hypersensitivity was assessed by thermal paw withdrawal latency (in seconds) in response to thermal stimulation. As shown in Fig. 6a, intrathecal injection of 10 μg/i.t of surfen produced a significant and long-lasting attenuation of CFA-induced thermal hyperalgesia (open circle) when compared with control animals who received intrathecal injection of PBS + 1% DMSO (dark circles). Notably, this effect was apparent as early as 20 min after the injection of surfen (p < 0.05), and remained sustainable up to over 180 min (p < 0.01).
Surfen inhibits nocifensive responses during formalin-induced pain. a, b Effect of increasing doses of surfen delivered intrethecally on the first (nociceptive, a) and second (inflammatory, b) phases of the formalin test. Control values are from animals injected with 1% DMSO. Note the efficacy of surfen on both the nociceptive and inflammatory responses in animal injected intrathecally with 10 μg/i.t. of surfen
Surfen reduces persistent inflammatory pain induced by CFA. a Time course of analgesic action of surfen delivered intrathecally (10 μg/i.t.) against thermal hyperalgesia induced by CFA (open circles) compared to control animals that received PBS (dark circles). Note the ability of surfen to increase thermal withdrawal latency as early as 20 min after injection and for a sustained period of time up to over 180 min
Altogether, these data demonstrate the analgesic potential of surfen when injected intrathecally in mouse models of acute and chronic inflammatory pain.
Discussion
Initially described in the late thirties as a byproduct in the production of depot insulin [58], the therapeutic potential of surfen in the treatment of various chronic disorders has gained increasing attention. For instance, surfen and derivatives have been proposed as potential antibacterial agents (patent US20070112048) [2], and more recently for the treatment of tauopathies including Alzheimer’s disease (patent WO2013020909) [1]. Here, we report new pharmacological properties of surfen and demonstrate its analgesic potential in mouse models of acute and chronic inflammatory pain.
A number of voltage-gated calcium channels have been implicated in the processing of the pain signal with specific subcellular expression patterns and function [4]. Among them, Cav2.2 and Cav3.2 channels are validated drug targets for the management of pain in the clinic [37, 56, 59, 60, 68]. For instance, inhibition of Cav2.2 channels by opioid receptors represents one of the mechanisms by which morphine mediates analgesia [20]. In addition, the gabapentinoid drugs gabapentin (Neurontin™) and pregabaline (Lyrica™) that target the Cavα2δ-1 ancillary subunit to modulate Cav2.2 channels have shown clinical efficacy in patients with neuropathic pain [23]. Small peptide inhibitors of Cav2.2 channels isolated from cone snails toxins have also shown analgesic potential in animal pain models, and the ω-conotoxin MVIIA (Prialt™) was approved for the management of refractory chronic pain in patients [44, 51]. More recently, Cav3.2 channels have emerged as clinically relevant drug targets for the management of neuropathic pain. For instance, inhibition of Cav3.2 channels by intrathecal delivery of ethosuximide (Zarontin™) has shown clinical efficacy [21]. Furthermore, the T-type channel inhibitor Z944 is currently assessed in Phase II clinical trials for pain [26]. In addition to Cav2.2 and Cav3.2 channels that are validated clinical targets, there is evidence that spinal modulation other calcium channel members, including Cav1.2/Cav1.3 [66], Cav2.1 [9, 28, 34], Cav2.3 [31, 55], and Cav3.3 [64], can produce analgesia in animal pain models. Considering that a variety of calcium channels participate in the transmission and processing of pain signals, targeting multiple channels with broad-spectrum inhibitors may represent an effective avenue to mediate analgesia.
Here, we showed that surfen effectively blocks multiple voltage-gated calcium channels including L-type (Cav1.2), P/Q-type (Cav2.1), N-type (Cav2.2), and T-type (Cav3.2 and Cav3.3) channels, without apparent selectivity. Furthermore, surfen was also effective in blocking native LVA and HVA channels in small DRG neurons in culture, with only minimal blocking activity on Nav and K v channels. The ability of surfen to block LVA currents in small DRG neurons implies that this compound acts on native Cav3.2 channels as it is the only channel isoform to carry T-type currents in these neurons [3]. In contrast, our observation that surfen blocked up to 65% of the HVA current suggests that multiple HVA channel isoforms were blocked as none of the HVA channels expressed in small DRG neurons account for more than 30% of the whole HVA current [33].
Previous studies have suggested that surfen modulates neutrophil chemotaxis via a Gβγ- and PLC-dependent signaling pathway [53]. Here, we did not observe any evidence for the implication of Gβγ or PLC in surfen-mediated inhibition of the calcium channels. On the other hand, the observation that inhibition of Cav2.2 and Cav3.2 channels plateaued at 80% inhibition with similar pharmacological properties (IC50 values and Hill coefficients) may be consistent with a diffuse, but common effect by which surfen indirectly modulates the calcium channels rather than a direct block of the channel itself, although we cannot rule out the latter mechanism. Along these lines, surfen was recently reported as an antagonist of cell-surface heparan sulfate with the potential to prevent glycosaminoglycan (GAG)-protein interaction [46, 63]. Although not studied here, it is a possibility that surfen could modulate calcium channels by altering GAG-channel interactions. Consistent with this idea, reduced calcium influx in pyramidal hippocampal neurons after enzymatic removal of heparan sulfate was recently documented [32]. Consistent with this notion, direct binding of heparin to exofacial Cav1.2 channel regions such as the pore-forming loop connecting transmembrane segments S5 and S6 of the first domain was reported to modulate channel activity [12]. It is possible that binding of surfen to heparan sulfate could disrupt this interaction and alter channel activity. Further studies will be needed to uncover the role of heparan sulfate in functioning of calcium channels.
Regardless of the mechanism behind surfen-induced inhibition of calcium channels, our in vivo data revealed that inthrathecal delivery of surfen results in long-lasting analgesic effects in rodent models of acute and persistent inflammatory pain. These data are consistent with previous studies reporting analgesic effects of calcium channel blockers on inflammatory hyperalgesia. For instance, and consistent with the notion that Cav2.2 channels are up-regulated in CFA-induced inflammatory pain model [27], inhibition of Cav2.2 by aminopiperidine sulfonamide reduced inflammatory hyperalgesia [48]. Reduced inflammatory pain was also documented in mice lacking Cav2.2 channels [43]. Along these lines, inhibition of T-type channel activity using pharmacological blockers [40, 54] or small interfering peptides to reduce surface expression of the channel [13, 14] also produced marked analgesic effect on mouse models of inflammatory pain. Hence, it is reasonable to propose that reduced inflammatory hyperalgesia observed during the second phase of the formalin test and in CFA-induced inflammatory pain model was at least partly mediated by the ability of surfen to block calcium channels. It is worth noting that surfen was also reported to have anti-inflammatory activity [24] that could have contributed to the analgesic effect in the CFA model. In addition, and although our data indicate that surfen has only a minor blocking activity on Nav and K v channels that is unlikely to have had a major contribution to its analgesic properties (the slight blockade of K v channels would actually have a pronociceptive effect), we cannot rule out the possibility that surfen may have affected the functioning of other channels and receptors by virtue of its pharmacological activity on heparan sulfate which in turn may have contributed to the observed analgesic effect. For instance, modulation of angiotensin II-mediated signaling by heparan sulfate glycosaminoglycans has been reported [22] and the angiotensin II type 2 receptor is a potential target to modulate pain [50]. Yet, our pain data are consistent with numerous reports showing that blockade of calcium channels in vivo supports analgesia in various animal pain models.
Although selective inhibitors are usually preferred in order to limit the risk of side effects, broad-spectrum blockers may have an advantage especially for disorders like neuropathic pain where multiple channels are implicated. Hence, our data raise the possibility of using surfen-type compounds for the development of new analgesic drugs.
References
Alavi NSM, Soussi-Yanicostas N, Yanicostas C (2013) Materials and methods for the treatment of tauopathies. https://www.google.com/patents/WO2013020909A1?cl=no
Bavari S, Panchal R, Gussio R (2007) Broad spectrum antibacterial compounds. https://www.google.com/patents/WO2008041966A2?cl=en&dq=Broad+spectrum+antibacterial+compounds&hl=en&sa=X&ved=0ahUKEwjol7_t2crUAhVB7hoKHYoFDYsQ6AEIJjAA
Bourinet E, Alloui A, Monteil A, Barrère C, Couette B, Poirot O, Pages A, McRory J, Snutch TP, Eschalier A, Nargeot J (2005) Silencing of the Cav3.2 T-type calcium channel gene in sensory neurons demonstrates its major role in nociception. EMBO J 24(2):315–324
Bourinet E, Altier C, Hildebrand ME, Trang T, Salter MW, Zamponi GW (2014) Calcium-permeable ion channels in pain signaling. Physiol Rev 94(1):81–140
Comunanza V, Carbone E, Marcantoni A, Sher E, Ursu D (2011) Calcium-dependent inhibition of T-type calcium channels by TRPV1 activation in rat sensory neurons. Pflugers Arch 462(5):709–722
Dobremez E, Bouali-Benazzouz R, Fossat P, Monteils L, Dulluc J, Nagy F, Landry M (2005) Distribution and regulation of L-type calcium channels in deep dorsal horn neurons after sciatic nerve injury in rats. Eur J Neurosci 21(12):3321–3333
Evans AR, Nicol GD, Vasko MR (1996) Differential regulation of evoked peptide release by voltage-sensitive calcium channels in rat sensory neurons. Brain Res 712(2):265–273
François A, Schüetter N, Laffray S, Sanguesa J, Pizzoccaro A, Dubel S, Mantilleri A, Nargeot J, Noël J, Wood JN (2015) The low-threshold calcium channel Cav3. 2 determines low-threshold mechanoreceptor function. Cell Rep 10(3):370–382
Fukumoto N, Obama Y, Kitamura N, Niimi K, Takahashi E, Itakura C, Shibuya I (2009) Hypoalgesic behaviors of P/Q-type voltage-gated Ca2+ channel mutant mouse, rolling mouse Nagoya. Neuroscience 160(1):165–173
Gadotti VM, Caballero AG, Berger ND, Gladding CM, Chen L, Pfeifer TA, Zamponi GW (2015) Small organic molecule disruptors of Cav3.2—USP5 interactions reverse inflammatory and neuropathic pain. Mol Pain 11:12
Gadotti VM, You H, Petrov RR, Berger ND, Diaz P, Zamponi GW (2013) Analgesic effect of a mixed T-type channel inhibitor/CB2 receptor agonist. Mol Pain 9:–32
Garau G, Magotti P, Heine M, Korotchenko S, Lievens PM, Berezin V, Dityatev A (2015) Heparin/heparan sulfates bind to and modulate neuronal L-type (Cav1. 2) voltage-dependent Ca(2+) channels. Exp Neurol 274(Pt B):156–165
Garcia-Caballero A, Gadotti VM, Chen L, Zamponi GW (2016) A cell-permeant peptide corresponding to the cUBP domain of USP5 reverses inflammatory and neuropathic pain. Mol Pain 12. doi:10.1177/1744806916642444
García-Caballero A, Gadotti VM, Stemkowski P, Weiss N, Souza IA, Hodgkinson V, Bladen C, Chen L, Hamid J, Pizzoccaro A, Deage M, François A, Bourinet E, Zamponi GW (2014) The deubiquitinating enzyme USP5 modulates neuropathic and inflammatory pain by enhancing Cav3.2 channel activity. Neuron 83(5):1144–1158
Heppenstall PA, Lewin GR (2006) A role for T-type Ca 2+ channels in mechanosensation. Cell Calcium 40(2):165–174
Hildebrand ME, Smith PL, Bladen C, Eduljee C, Xie JY, Chen L, Fee-Maki M, Doering CJ, Mezeyova J, Zhu Y (2011) A novel slow-inactivation-specific ion channel modulator attenuates neuropathic pain. Pain 152(4):833–843
Hunskaar S, Fasmer OB, Hole K (1985) Formalin test in mice, a useful technique for evaluating mild analgesics. J Neurosci Methods 14(1):69–76
Hylden JL, Wilcox GL (1980) Intrathecal morphine in mice: a new technique. Eur J Pharmacol 67(2–3):313–316
Jacus MO, Uebele VN, Renger JJ, Todorovic SM (2012) Presynaptic Cav3. 2 channels regulate excitatory neurotransmission in nociceptive dorsal horn neurons. J Neurosci 32(27):9374–9382
Jiang YQ, Andrade A, Lipscombe D (2013) Spinal morphine but not ziconotide or gabapentin analgesia is affected by alternative splicing of voltage-gated calcium channel CaV2.2 pre-mRNA. Mol Pain 9:67
Kerckhove N, Mallet C, Pereira B, Chenaf C, Duale C, Dubray C, Eschalier A (2016) Assessment of the effectiveness and safety of Ethosuximide in the Treatment of non-Diabetic Peripheral Neuropathic Pain: EDONOT-protocol of a randomised, parallel, controlled, double-blinded and multicentre clinical trial. BMJ Open 6(12):e013530
Köppel H, Yard BA, Christ M, Wehling M, van der Woude FJ (2003) Modulation of angiotensin II-mediated signalling by heparan sulphate glycosaminoglycans. Nephrol Dial Transplant 18(11):2240–2247
Kremer M, Salvat E, Muller A, Yalcin I, Barrot M (2016) Antidepressants and gabapentinoids in neuropathic pain: mechanistic insights. Neuroscience 338:183–206
Lanza TJ, Durette PL, Rollins T, Siciliano S, Cianciarulo DN, Kobayashi SV, Caldwell CG, Springer MS, Hagmann WK (1992) Substituted 4,6-diaminoquinolines as inhibitors of C5a receptor binding. J Med Chem 35(2):252–258
Lazniewska J, Rzhepetskyy Y, Zhang FX, Zamponi GW, Weiss N (2016) Cooperative roles of glucose and asparagine-linked glycosylation in T-type calcium channel expression. Pflugers Arch 468(11–12):1837–1851
Lee M (2014) Z944: a first in class T-type calcium channel modulator for the treatment of pain. J Peripher Nerv Syst 19(Suppl 2):S11–S12
Lu SG, Zhang XL, Luo ZD, Gold MS (2010) Persistent inflammation alters the density and distribution of voltage-activated calcium channels in subpopulations of rat cutaneous DRG neurons. Pain 151(3):633–643
Luvisetto S, Marinelli S, Panasiti MS, D’Amato FR, Fletcher CF, Pavone F, Pietrobon D (2006) Pain sensitivity in mice lacking the Ca(v)2. 1 alpha 1 subunit of P/Q-type Ca2+ channels. Neuroscience 142(3):823–832
Maggi CA, Tramontana M, Cecconi R, Santicioli P (1990) Neurochemical evidence for the involvement of N-type calcium channels in transmitter secretion from peripheral endings of sensory nerves in guinea pigs. Neurosci Lett 114(2):203–206
Mallmann RT, Wilmes T, Lichvarova L, Bührer A, Lohmüller B, Castonguay J, Lacinova L, Klugbauer N (2013) Tetraspanin-13 modulates voltage-gated CaV2. 2 Ca2+ channels. Sci Rep 3:1777
Matthews EA, Bee LA, Stephens GJ, Dickenson AH (2007) The Cav2. 3 calcium channel antagonist SNX-482 reduces dorsal horn neuronal responses in a rat model of chronic neuropathic pain. Eur J Neurosci 25(12):3561–3569
Minge D, Senkov O, Kaushik R, Herde MK, Tikhobrazova O, Wulff AB, Mironov A, van Kuppevelt TH, Oosterhof A, Kochlamazashvili G, Dityatev A, Henneberger C (2017) Heparan sulfates support pyramidal cell excitability, synaptic plasticity, and context discrimination. Cereb Cortex 27(2):903–918
Murakami M, Nakagawasai O, Suzuki T, Mobarakeh II, Sakurada Y, Murata A, Yamadera F, Miyoshi I, Yanai K, Tan-No K, Sasano H, Tadano T, Iijima T (2004) Antinociceptive effect of different types of calcium channel inhibitors and the distribution of various calcium channel alpha 1 subunits in the dorsal horn of spinal cord in mice. Brain Res 1024(1–2):122–129
Nebe J, Vanegas H, Neugebauer V, Schaible HG (1997) Omega-agatoxin IVA, a P-type calcium channel antagonist, reduces nociceptive processing in spinal cord neurons with input from the inflamed but not from the normal knee joint—an electrophysiological study in the rat in vivo. Eur J Neurosci 9(10):2193–2201
Obradovic AL, Hwang SM, Scarpa J, Hong SJ, Todorovic SM, Jevtovic-Todorovic V (2014) Ca V 3.2 T-Type calcium channels in peripheral sensory neurons are important for mibefradil-induced reversal of hyperalgesia and allodynia in rats with painful diabetic neuropathy. PLoS One 9(4):e91467
Panchal RG, Hermone AR, Nguyen TL, Wong TY, Schwarzenbacher R, Schmidt J, Lane D, Mc Grath C, Turk BE, Burnett J, Aman MJ, Little S, Sausville EA, Zaharevitz DW, Cantley LC, Liddington RC, Gussio R, Bavari S (2004) Identification of small molecule inhibitors of anthrax lethal factor. Nat Struct Mol Biol 11(1):67–72
Perret D, Luo ZD (2009) Targeting voltage-gated calcium channels for neuropathic pain management. Neurotherapeutics 6(4):679–692
Pexton T, Moeller-Bertram T, Schilling JM, Wallace MS (2011) Targeting voltage-gated calcium channels for the treatment of neuropathic pain: a review of drug development. Expert Opin Investig Drugs 20(9):1277–1284
Proft J, Weiss N (2015) G protein regulation of neuronal calcium channels: back to the future. Mol Pharmacol 87(6):890–906
Pudukulatham Z, Zhang FX, Gadotti VM, M’Dahoma S, Swami P, Tamboli Y, Zamponi GW (2016) Synthesis and characterization of a disubstituted piperazine derivative with T-type channel blocking action and analgesic properties. Mol Pain 12. doi:10.1177/1744806916641678
Radwani H, Lopez-Gonzalez MJ, Cattaert D, Roca-Lapirot O, Dobremez E, Bouali-Benazzouz R, Eiríksdóttir E, Langel Ü, Favereaux A, Errami M, Landry M, Fossat P (2016) Cav1. 2 and Cav1. 3 L-type calcium channels independently control short- and long-term sensitization to pain. J Physiol 594(22):6607–6626
Rose KE, Lunardi N, Boscolo A, Dong X, Erisir A, Jevtovic-Todorovic V, Todorovic SM (2013) Immunohistological demonstration of Ca V 3.2 T-type voltage-gated calcium channel expression in soma of dorsal root ganglion neurons and peripheral axons of rat and mouse. Neuroscience 250:263–274
Saegusa H, Kurihara T, Zong S, Kazuno A, Matsuda Y, Nonaka T, Han W, Toriyama H, Tanabe T (2001) Suppression of inflammatory and neuropathic pain symptoms in mice lacking the N-type Ca2+ channel. EMBO J 20(10):2349–2356
Sanford M (2013) Intrathecal ziconotide: a review of its use in patients with chronic pain refractory to other systemic or intrathecal analgesics. CNS Drugs 27(11):989–1002
Santicioli P, Del Bianco E, Tramontana M, Geppetti P, Maggi CA (1992) Release of calcitonin gene-related peptide like-immunoreactivity induced by electrical field stimulation from rat spinal afferents is mediated by conotoxin-sensitive calcium channels. Neurosci Lett 136(2):161–164
Schuksz M, Fuster MM, Brown JR, Crawford BE, Ditto DP, Lawrence R, Glass CA, Wang L, Tor Y, Esko JD (2008) Surfen, a small molecule antagonist of heparan sulfate. Proc Natl Acad Sci U S A 105(35):13075–13080
Scroggs RS, Fox AP (1992) Calcium current variation between acutely isolated adult rat dorsal root ganglion neurons of different size. J Physiol 445:639–658
Shao PP, Ye F, Chakravarty PK, Varughese DJ, Herrington JB, Dai G, Bugianesi RM, Haedo RJ, Swensen AM, Warren VA, Smith MM, Garcia ML, Mc Manus OB, Lyons KA, Li X, Green M, Jochnowitz N, Mc Gowan E, Mistry S, Sun SY, Abbadie C, Kaczorowski GJ, Duffy JL (2012) Aminopiperidine sulfonamide Cav2. 2 channel inhibitors for the treatment of chronic pain. J Med Chem 55(22):9847–9855
Smith MT, Cabot PJ, Ross FB, Robertson AD, Lewis RJ (2002) The novel N-type calcium channel blocker, AM336, produces potent dose-dependent antinociception after intrathecal dosing in rats and inhibits substance P release in rat spinal cord slices. Pain 96(1):119–127
Smith MT, Muralidharan A (2015) Targeting angiotensin II type 2 receptor pathways to treat neuropathic pain and inflammatory pain. Expert Opin Ther Targets 19(1):25–35
Staats PS, Yearwood T, Charapata SG, Presley RW, Wallace MS, Byas-Smith M, Fisher R, Bryce DA, Mangieri EA, Luther RR, Mayo M, Mc Guire D, Ellis D (2004) Intrathecal ziconotide in the treatment of refractory pain in patients with cancer or AIDS: a randomized controlled trial. JAMA 291(1):63–70
Sukiasyan N, Hultborn H, Zhang M (2009) Distribution of calcium channel Ca(V)1. 3 immunoreactivity in the rat spinal cord and brain stem. Neuroscience 159(1):217–235
Surve CR, Lehmann D, Smrcka AV (2014) A chemical biology approach demonstrates G protein βγ subunits are sufficient to mediate directional neutrophil chemotaxis. J Biol Chem 289(25):17791–17801
Teleb M, Zhang FX, Huang J, Gadotti VM, Farghaly AM, OM AW, Zamponi GW, Fahmy H (2017) Synthesis and biological evaluation of novel N3-substituted dihydropyrimidine derivatives as T-type calcium channel blockers and their efficacy as analgesics in mouse models of inflammatory pain. Bioorg Med Chem 25(6):1926–1938
Terashima T, Xu Q, Yamaguchi S, Yaksh TL (2013) Intrathecal P/Q- and R-type calcium channel blockade of spinal substance P release and c-Fos expression. Neuropharmacology 75:1–8
Todorovic SM, Jevtovic-Todorovic V (2011) T-type voltage-gated calcium channels as targets for the development of novel pain therapies. Br J Pharmacol 163(3):484–495
Tsien RW, Lipscombe D, Madison DV, Bley KR, Fox AP (1988) Multiple types of neuronal calcium channels and their selective modulation. Trends Neurosci 11(10):431–438
Umber F, Stoerring FK, Foellmer W (1938) Erfolge mit einem neuartigen Depotinsulin ohne Protaminzusatz (Surfen-Insulin). Klin Wochenschr 17(13):443–446
Vink S, Alewood PF (2012) Targeting voltage-gated calcium channels: developments in peptide and small-molecule inhibitors for the treatment of neuropathic pain. Br J Pharmacol 167(5):970–989
Waxman SG, Zamponi GW (2014) Regulating excitability of peripheral afferents: emerging ion channel targets. Nat Neurosci 17(2):153–163
Weiss N, Hameed S, Fernández-Fernández JM, Fablet K, Karmazinova M, Poillot C, Proft J, Chen L, Bidaud I, Monteil A, Huc-Brandt S, Lacinova L, Lory P, Zamponi GW, De Waard M (2012) A Ca(v)3. 2/syntaxin-1A signaling complex controls T-type channel activity and low-threshold exocytosis. J Biol Chem 287(4):2810–2818
Weiss N, Zamponi GW (2013) Control of low-threshold exocytosis by T-type calcium channels. Biochim Biophys Acta 1828(7):1579–1586
Weiss RJ, Gordts PL, Le D, Xu D, Esko JD, Tor Y (2015) Small molecule antagonists of cell-surface heparan sulfate and heparin-protein interactions. Chem Sci 6(10):5984–5993
Wen XJ, Li ZJ, Chen ZX, Fang ZY, Yang CX, Li H, Zeng YM (2006) Intrathecal administration of Cav3. 2 and Cav3. 3 antisense oligonucleotide reverses tactile allodynia and thermal hyperalgesia in rats following chronic compression of dorsal root of ganglion. Acta Pharmacol Sin 27(12):1547–1552
Woolf CJ, Ma Q (2007) Nociceptors—noxious stimulus detectors. Neuron 55(3):353–364
Yamamoto S, Suzuki Y, Ono H, Kume K, Ohsawa M (2016) N- and L-type calcium channels blocker cilnidipine ameliorates neuropathic pain. Eur J Pharmacol 793:66–75
Yusaf SP, Goodman J, Pinnock RD, Dixon AK, Lee K (2001) Expression of voltage-gated calcium channel subunits in rat dorsal root ganglion neurons. Neurosci Lett 311(2):137–141
Zamponi GW (2016) Targeting voltage-gated calcium channels in neurological and psychiatric diseases. Nat Rev Drug Discov 15(1):19–34
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Financial support
Work in the Weiss laboratory is supported by the Czech Science Foundation (grant 15-13556S), the Czech Ministry of Education Youth and Sports (grant 7AMB15FR015), and the Institute of Organic Chemistry and Biochemistry (IOCB). GWZ is a Canada Research Chair and supported by the Canadian Institutes of Health Research.
Rights and permissions
About this article
Cite this article
Rivas-Ramirez, P., Gadotti, V.M., Zamponi, G.W. et al. Surfen is a broad-spectrum calcium channel inhibitor with analgesic properties in mouse models of acute and chronic inflammatory pain. Pflugers Arch - Eur J Physiol 469, 1325–1334 (2017). https://doi.org/10.1007/s00424-017-2017-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-017-2017-8