Abstract
Prolactin (PRL) is reported to stimulate calcium absorption in the rat’s small intestine. However, little is known regarding its effects on the cecum, a part of the large intestine with the highest rate of intestinal calcium transport. We demonstrated herein by quantitative real-time polymerase chain reaction and Western blot analysis that the cecum could be a target organ of PRL since cecal epithelial cells strongly expressed PRL receptors. In Ussing chamber experiments, PRL enhanced the transcellular cecal calcium absorption in a biphasic dose–response manner. PRL also increased the paracellular calcium permeability and passive calcium transport in the cecum, which could be explained by the PRL-induced decrease in transepithelial resistance and increase in cation selectivity of the cecal epithelium. PRL actions in the cecum were abolished by inhibitors of phosphoinositide 3-kinase (PI3K), protein kinase C (PKC), and RhoA-associated coiled-coil forming kinase (ROCK), but not inhibitors of gene transcription and protein biosynthesis. In conclusion, PRL directly enhanced the transcellular and paracellular calcium transport in the rat cecum through the nongenomic signaling pathways involving PI3K, PKC, and ROCK.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
During pregnancy and lactation, prolactin (PRL) serves as a calcium-regulating hormone which markedly stimulates intestinal calcium absorption to help alleviate negative calcium balance due to massive calcium loss for fetal growth and milk production [5]. The PRL-enhanced calcium absorption has been intensively investigated in the small intestine [6, 25], especially in the duodenum, where the transcellular active calcium transport is prominent [11, 29]. However, the effects of PRL on the large intestine as well as its mechanisms were largely unknown.
It is widely known that, in monogastric herbivores, rats and humans, the cecum is for absorption of fluids and salts and is the site for luminal microfloral production of short-chain fatty acids, folate, and vitamin K [16, 32, 33]. Studies on the intestinal calcium absorption demonstrated that, besides the duodenum, the proximal part of the large intestine, particularly the cecum, is another important site for the transcellular active calcium transport [40]. Moreover, experiments in rats showed that when compared to other intestinal segments, cecum has the highest rate of calcium transport [28, 39]. Under normal conditions, it was suggested that the cecal epithelium absorbs a significant amount of free calcium which is released during microbial fermentation of the cecal contents through production of short-chain fatty acids and other acidic molecules, such as lactic acid, butyric acid, and succinic acid, as well as calcium released from the degradation of dietary fiber [10, 36]. Accumulation of free calcium in the cecal lumen may also be enough to increase the paracellular passive calcium transport [28]. Since PRL plays an important role in supplying additional calcium to the body, we postulated that it may increase the cecal calcium absorption via both transcellular and paracellular routes as seen in the small intestine [5].
Generally, the transcellular calcium transport is a three-step metabolically energized process, consisting of the apical uptake via the transient receptor potential vanilloid family calcium channel 5 and 6 (TRPV5/6) and l-type calcium channel Cav1.3, cytoplasmic translocation in a calbindin-D9k-bound form, and the basolateral extrusion via the plasma membrane Ca2+-ATPase 1b (PMCA1b) and Na+/Ca2+ exchanger 1 (NCX1) [20, 30, 49]. In contrast, the paracellular passive calcium transport is dependent on the transepithelial calcium gradient and is absent when both sides of the epithelium have equal calcium concentration [29]. Paracellular calcium movement is regulated by the tight junction, which contains several charge-selective proteins, particularly claudin-2, claudin-3, and claudin-12, arranged in the arrays of channel-like paracellular pores [14, 30]. Besides, the integrity of the tight junction is regulated by tight junction proteins, such as zonula occludens-1 (ZO-1) and occludin [50].
It is apparent that the paracellular calcium transport is predominant in the small intestine [10, 29]. However, when calcium demand is markedly increased, such as during pregnancy and lactation, contribution from the transcellular transport component to the total calcium absorption becomes more significant, in part, as a result of the stimulatory action of PRL [3, 5]. Recently, we demonstrated in the duodenum and Caco-2 monolayer that PRL enhanced both transcellular active and paracellular passive calcium transport through the phosphoinositide 3-kinase (PI3K), protein kinase C (PKC), and RhoA-associated coiled-coil forming kinase (ROCK) pathways [25, 48, 49]. However, PRL signaling in the large intestine, including the cecum, had never been investigated.
Therefore, the objectives of the present study were (a) to demonstrate that the cecum was a target organ of PRL, (b) to investigate the effects of PRL on the cecal calcium transport, and (c) to investigate the mechanisms of the PRL-enhanced calcium absorption in the cecum.
Materials and methods
Animals
Female Sprague–Dawley rats (8 weeks old, weighing 180–200 g) were obtained from the National Laboratory Animal Centre, Thailand. They were placed in hanging stainless steel cages, fed with standard pellets containing 1% wt/wt calcium and 100 IU vitamin D per 100 g of diet (Perfect Companion, Bangkok, Thailand), and provided with distilled water ad libitum under 12:12 h light/dark cycle. The room had temperature of 20–25°C, humidity of 50–60%, and average illuminance of 150–200 lux in the daytime. Body weight and food intake were recorded daily. This study has been approved by the Institutional Animal Care and Use Committee of the Faculty of Science, Mahidol University, Bangkok, Thailand.
Tissue preparation
After 7-day acclimatization, the rat was anesthetized by administering 50 mg/kg sodium pentobarbitone i.p. (Abbott, North Chicago, IL, USA). Thereafter, median laparotomy was performed. Duodenum (10 cm), proximal and distal jejunum (10 cm each), ileum (8 cm), cecum (4 cm), and proximal and distal colon (8 cm each) were removed and cut longitudinally to expose the mucosa. In the calcium transport experiments, the muscularis proper was stripped off before the tissue was mounted in a modified Ussing chamber as described previously [25]. The tissue was incubated for 20 min in the chamber before the 60-min experiment was carried out. As for the mRNA and protein expression studies, epithelial cells were collected by scraping the mucosal surface with an ice-cold glass slide [8].
Total RNA preparation and cDNA synthesis
Total RNA was extracted from mucosal scrapings by using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) and purified with RNeasy Mini kit (Qiagen, Valencia, CA, USA). Purity and integrity of RNA were determined by 260/280 nm absorbance and denaturing agarose gel electrophoresis, respectively [8]. One microgram of the total RNA was then reverse-transcribed to cDNA with the oligo-dT20 primer and the iScript kit (Bio-Rad, Hercules, CA, USA). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH), a housekeeping gene, served as a control gene to check the consistency of the reverse transcription.
Quantitative real-time PCR and sequencing
Primers used in this study were shown in Table 1. Quantitative real-time polymerase chain reaction (qRT-PCR) and melting curve analysis were performed by the Bio-rad MiniOpticon with the iQ SYBR Green SuperMix (Bio-rad) as previously described [8]. Relative expression of PRL receptor (PRLR) over GAPDH was calculated from the threshold cycle (C t) values by using \( 2^{{\Delta }{{C_{\text{t}}} }} \) method. The PCR products were also visualized on a 1.5% agarose gel stained with 1.0 μg/mL ethidium bromide under a UV transilluminator (Alpha Innotech, San Leandro, CA, USA). After electrophoresis, all PCR products were purified from a gel by the HiYield Gel/PCR DNA Extraction kit (Real Biotech Corporation, Taipei, Taiwan) and sequenced by the ABI Prism 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA, USA).
Western blot analysis
As previously described [25], scraped mucosal cells were lysed in lysis buffer (0.5 mmol/L Tris pH 7.5, 1.5 mol/L NaCl, 10% NP-40, 5% DOC, 10 mmol/L Na ethylenediaminetetraacetic acid, 1 mmol/L phenylmethylsulfonyl fluoride, 1 μg/mL leupeptin, 1 μg/mL aprotinin, 1 μg/mL pepstatin A; all purchased from Sigma, St. Louis, MO, USA). Lysates were sonicated at 4°C and centrifuged at 20,000×g for 10 min. One hundred micrograms proteins were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis and transferred to a nitrocellulose membrane (Amersham, Buckinghamshire, UK) by electroblotting. Membranes were blocked at 25°C for 4 h with 5% nonfat milk and were probed overnight at 4°C with 1:500 rabbit antirat PRLR polyclonal antibodies (catalog no. sc-30225; Santa Cruz Biotechnology, Santa Cruz, CA, USA) raised against the conserved extracellular domain. Membranes were later reprobed with 1:5,000 mouse antirat β-actin monoclonal antibodies (catalog no. sc-47778; Santa Cruz). After 2-h incubation at 25°C with 1:20,000 goat antirabbit (catalog no. sc-2004) or antimouse (catalog no. sc-2005) secondary antibodies (Santa Cruz), blots were visualized by enhanced chemiluminescence kit (Amersham).
Bathing solution for Ussing chamber study
The bathing solution continuously gassed with humidified 5% CO2 in 95% O2, contained (in mmol/L) 118 NaCl, 4.7 KCl, 1.1 MgCl2, 1.25 CaCl2, 23 NaHCO3, 12 d-glucose, and 2 mannitol (all purchased from Sigma). The solution was maintained at 37°C, pH 7.4, and had an osmolality of 290–293 mmol kg−1 water as measured by a freezing point-based osmometer (model 3320; Advanced Instruments, Norwood, MA, USA).
Measurement of epithelial electrical parameters
Three electrical parameters, i.e., potential difference (PD), short-circuit current (Isc), and transepithelial resistance (TER), were determined according to the method of Charoenphandhu et al. [6]. In brief, a pair of Ag/AgCl electrodes connected to agar bridges was placed near each surface of the mounted tissue for PD measurement. The other ends of the PD-sensing electrodes were connected to the EVC-4000 pre-amplifier (World Precision Instruments, Sarasota, FL, USA) and finally to a PowerLab 4/30 operated with the software Chart 5.2.2 for Mac OS X (ADInstruments, Colorado Springs, CO, USA). Another pair of Ag/AgCl electrodes was placed at the end of each hemichamber to supply external current, which was also measured by a PowerLab 4/30 connected in series to the EVC-4000 current-generating unit. TER and conductance (G; G = 1/TER) were calculated by Ohm’s equation. Fluid resistance was automatically subtracted by the EVC-4000 system. In some experiments, Isc was continuously applied to nullify PD, i.e., the experiments were performed under short-circuit condition. Unless otherwise specified, the experiments were normally performed under open-circuit condition since the absence of PD did not significantly affect calcium flux (Supplemental Figure S1). In other words, the voltage-dependent calcium transport in the cecum could be considered negligible, similar to that observed in the duodenum [6].
Measurement of calcium flux
Transepithelial calcium flux was determined by the method of Charoenphandhu et al. [6]. In brief, after 20-min incubation, Ussing chamber was filled on one side with 45CaCl2-containing bathing solution (specific activity of 500 mCi/mol; Amersham). Unidirectional flux (J H→C) from the hot side (H) to the cold side (C) was calculated with Eqs. 1 and 2.
where R H→C was the rate of tracer appearance in the cold side (counts per minute per hour), S H was the specific activity in the hot side (counts per minute per nanomole) and did not vary with time (a constant value), A was the surface area of the tissue (0.69 cm2), C H was the radioactivity in the hot side (counts per minute), and C T was the total calcium in the hot side (nanomole). Radioactivity of 45Ca in counts per minute was analyzed by liquid scintillation spectrophotometry (model Tri-Carb 3100; Packard Instruments, Meriden, CT, USA). Total calcium concentration in the hot side was determined by atomic absorption spectrophotometry (model SpectrAA-300; Varian Techtron, Springvale, Australia).
Calcium fluxes in the absence of transepithelial calcium gradient, i.e., bathing solution in both hemichambers containing equal calcium concentration, represented the active calcium transport [6]. The calcium gradient-dependent paracellular passive fluxes were measured by determining the calcium fluxes in the presence of varying apical calcium concentrations [48], i.e., 1.25, 2.5, 5, 10, and 20 mmol/L (n = 4 per each concentration).
Unless otherwise specified, the measured calcium fluxes represented calcium transport in mucosa-to-serosa direction. The serosa-to-mucosa calcium flux in the cecum was relatively small and had no significant influence on the net calcium transport (Supplemental Figure S2). In addition, PRL did not enhance calcium transport in serosa-to-mucosa direction (Supplemental Figure S2).
Determination of the epithelial permeability and Na+/Cl− selectivity
Permeability of sodium (P Na) and chloride (P Cl) which are indicative of the epithelial charge selectivity were measured by the dilution potential technique [21, 26]. The mounted cecum was equilibrated for 20 min in bathing solution containing 145 mmol/L NaCl before the apical solution was replaced with 72.5 mmol/L NaCl-containing solution. Osmolality of the solution was maintained by an equivalent amount of mannitol. Changes in the electrical parameters before and after fluid replacement were continuously recorded by PowerLab 4/30 until stable. The ion permeability ratio (P Na/P Cl) was calculated from the dilution potential (V δ) using the modified Goldman–Hodgkin–Katz equation (Eq. 3).
where ρ = P Na/P Cl; ϕ = C b/C a; ν = FV δ/RT; P Na was the absolute permeability of sodium; P Cl was the absolute permeability of chloride; C a was the mucosal NaCl concentration; C b was the serosal NaCl concentration; and R, T, and F had their conventional meanings.
Thereafter, P Na and P Cl were calculated from the conductance (G) and P Na/P Cl using Kimizuka–Koketsu equations [31], as follows:
The paracellular calcium permeability (P Ca) was calculated from Eq. 6 [48].
where J Ca was the paracellular passive calcium flux and ΔC was the difference between the apical and basolateral calcium concentrations.
Experimental protocol
To demonstrate the effects of PRL on calcium transport, electrical parameters, and epithelial permeability, the mounted cecal tissue was directly exposed on the serosal side to 200, 400, 600, 800, or 1,000 ng/mL PRL (catalog no. L6520; Sigma) during the 80-min experiment. In some experiments, the most efficient dose of PRL (i.e., 800 ng/mL) plus RNA polymerase II inhibitor (50 μmol/L 5,6-dichloro-1-β-D-ribofuranosylbenzimidazole (DRB); Calbiochem, San Diego, CA, USA), protein synthesis inhibitor (70 μmol/L cycloheximide (CCH); Sigma), Janus kinase (JAK) 2 inhibitor (50 μmol/L AG490; Calbiochem), PI3K inhibitors (75 μmol/L LY294002 or 200 nmol/L wortmannin; Tocris Bioscience, Bristol, UK), pan-specific PKC inhibitor (1 μmol/L GF109203X; A.G. Scientific, San Diego, CA, USA), selective ROCK inhibitor (1 μmol/L Y27632; Calbiochem), or myristoylated protein kinase A inhibitor 14–22 amide (10 µmol/L PKAI 14–22; Calbiochem) were added to the serosal solution to identify possible PRL signaling pathways. Wortmannin was more potent but less specific than LY294002 [18, 23]. PKAI 14–22 was first dissolved in distilled water, while other inhibitors were dissolved in DMSO (Sigma). Concentration of dimethyl sulfoxide (DMSO) in the bathing solution was 0.3% vol/vol, which did not affect the viability of cells [6]. To verify that PRL was able to stimulate the transcellular calcium transport, the cecal tissue was directly exposed to inhibitors of apical calcium uptake (50 µmol/L ruthenium red; Sigma) or calmodulin-dependent PMCA (100 μmol/L trifluoperazine; TFP; Sigma). Polyclonal antibody against PRLR (1 μg/mL; catalog no. sc-30225; Santa Cruz) was directly added in bathing solution to confirm that PRLR mediated PRL actions.
Statistical analysis
Results are expressed as means ± standard error (SE). Two sets of data were compared by using the unpaired Student’s t test. Multiple comparisons were performed by one-way analysis of variance with Dunnett’s multiple comparison test. Linear regression was used to demonstrate the relationships between mucosal calcium and paracellular calcium flux, and mucosal calcium and TER. The level of significance for all statistical tests was p < 0.05. All data were analyzed by GraphPad Prism 4.0 for Mac OS X (GraphPad Software, San Diego, CA, USA).
Results
Cecal epithelial cells expressed PRLRs and essential calcium transporters
As shown in Fig. 1a, b, both short (-S) and long (-L) isoforms of PRLR mRNAs and proteins were expressed in the duodenum, proximal and distal jejunum, ileum, cecum, and proximal and distal colon of rats. In the cecum (Fig. 1c–e), PRLR-L was more abundant than PRLR-S. Although calcium absorption has been demonstrated in cecum [28], the expression of calcium transport genes has not been completely investigated in cecal epithelial cells. Therefore, we used PCR to show that cecal cells strongly expressed all essential genes required for the transcellular calcium transport, i.e., TRPV5, TRPV6, Cav1.3, calbindin-D9k, PMCA1b, and NCX1, and for the paracellular calcium transport, i.e., claudin-2, claudin-3, claudin-12, ZO-1, and occludin (Fig. 1f). Thus, the results suggested that the cecal epithelium of female rats could absorb calcium via both transcellular and paracellular pathways. Calcium transport in the cecum may be of importance since the cecal calcium flux was ∼1.5-fold higher than that in the duodenum even in the absence of calcium concentration gradient (Fig. 1g).
a, b Expression of short (-S) and long (-L) isoforms of PRLRs in the duodenum (D), proximal (PJ) and distal jejunum (DJ), ileum (I), cecum (CE), and proximal (PC) and distal colon (DC) as demonstrated by qRT-PCR (a; n = 8 per segment) and Western blot analysis (b; n = 8 per segment). qRT-PCR data expressed as log means ± SE were normalized by GAPDH expression, while PRLR protein expression was normalized by β-actin expression. c Normalized expression of PRLR-S and PRLR-L in the cecum of female rats. PRLR-L expression appears as fold difference from PRLR-S expression, while setting PRLR-S expression as 1. **p < 0.01 PRLR-S expression vs. PRLR-L expression. d Representative electrophoretic bands of PRLR-S and PRLR-L mRNAs in duodenum (D) and cecum (CE). Gastrocnemius muscle (M) and liver (L) were used as negative and positive controls, respectively. e Representative bands of PRLR-S and PRLR-L proteins in duodenum (D) and cecum (CE). Gastrocnemius muscle (M) and liver (L) were negative and positive controls, respectively. f Electrophoretic bands of genes related to the transcellular and paracellular calcium transport in the cecum (n = 10). GAPDH was used as a housekeeping gene. g Normalized transepithelial calcium fluxes in the duodenum and cecum as determined by Ussing chamber technique. Calcium concentration on both sides was 1.25 mmol/L. ***p < 0.001 cecal flux vs. duodenal flux. Numbers in parentheses (c and g) represent the number of experimental animals
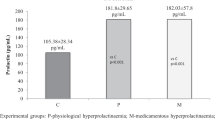
PRL stimulated the cecal calcium transport in a biphasic dose–response manner
Dose–response study demonstrated that high physiological concentrations of PRL of 600 and 800 ng/mL, which were comparable to the levels observed during suckling in lactating rats [1], markedly enhanced the transcellular calcium transport by ∼1.5- and ∼2-fold, respectively, while 200 and 400 ng/mL PRL were without effects (Fig. 2a). Interestingly, the pathological concentration of 1,000 ng/mL, as seen in prolactinomas, only slightly increased calcium transport in the cecum (Fig. 2a). Since such PRL effect was not observed in the presence of apical calcium uptake inhibitor (50 µmol/L ruthenium red) or basolateral calcium extrusion inhibitor (100 µmol/L trifluoperazine), the PRL-stimulated calcium transport in this experiment was confirmed to occur via the transcellular pathway (Fig. 2b). The fact that the PRL-enhanced cecal calcium transport occurred rapidly within 60 min after exposure and was not abolished by inhibitors of gene transcription (50 µmol/L DRB) or protein biosynthesis (70 µmol/L cycloheximide; Fig. 2b), suggesting that the stimulatory actions of PRL was exerted via the nongenomic signaling pathways. Direct exposure to DRB and cycloheximide alone did not affect the basal rate of the transcellular calcium transport (Fig. 2b). PRL-stimulated calcium transport was absent when the cecum was continuously exposed to 1 μg/mL PRLR antibody, indicating that PRLR mediated PRL actions in this intestinal segment (Fig. 2b). Moreover, the decrease in TER by 600, 800, and 1,000 ng/mL PRL (Table 2) suggested the PRL-induced increase in paracellular permeability. Since 800 ng/mL was the maximal effective concentration of PRL for stimulation of calcium transport, this concentration was used in the subsequent experiments.
a Dose-dependent effect of PRL on the transcellular calcium transport in the cecum. b Transcellular calcium transport in the cecum directly exposed to inhibitors of RNA polymerase II (50 μmol/L DRB), protein synthesis (70 µmol/L CCH), apical calcium uptake (50 µmol/L ruthenium red (Ruth.); apical side), basolateral calcium extrusion (100 µmol/L trifluoperazine (TFP); basolateral side), or 1 µg/mL PRLR antibody (Ab; basolateral side) with (+PRL) and without (−PRL) 800 ng/mL PRL (maximal effective concentration). DMSO was a vehicle for preparation of DRB and CCH. Numbers in parentheses represent the number of animals. *p < 0.05, **p < 0.01 compared with its respective control group
The PRL-enhanced transcellular calcium transport in cecum was mediated by PI3K, PKC, and ROCK signaling pathways
Previous investigations showed that PRL signaling in mammary epithelium was mediated by JAK2, whereas that in the duodenum and Caco-2 monolayer was mediated by PI3K, PKC, and ROCK [25, 48]. Moreover, an increase in intestinal calcium absorption via the transcellular route was also reported to be protein kinase A (PKA)-dependent [9, 30]. Herein, we found that the PRL-enhanced transcellular calcium transport in cecum was completely abolished by inhibitors of PI3K (75 µmol/L LY294002 and 200 nmol/L wortmannin), PKC (1 µmol/L GF109203X), and ROCK (1 µmol/L Y27632), but not inhibitors of JAK2 (50 µmol/L AG490) and PKA (10 µmol/L PKAI 14–22; Fig. 3). Exposure to inhibitors alone did not affect the calcium flux. The data, therefore, indicated that PRL exerted its stimulatory actions on the cecal calcium transport via the PI3K, PKC, and ROCK signaling pathways.
Transcellular calcium transport in the cecum exposed to JAK2 inhibitor (50 µmol/L AG490), PI3K inhibitors (75 µmol/L LY294002 and 200 nmol/L wortmannin), PKC inhibitor (1 µmol/L GF109203X), ROCK inhibitor (1 µmol/L Y27632), or myristoylated PKA inhibitor 14–22 amide (10 µmol/L PKAI 14–22) with (+PRL) and without (−PRL) 800 ng/mL PRL. PKAI 14–22 was dissolved in water, whereas other inhibitors were dissolved in DMSO (vehicle). All experiments were performed under open-circuit condition. Numbers in parentheses represent the number of animals. **p<0.01, ***p < 0.001 compared with the control group
PRL increased the paracellular calcium transport and calcium permeability in cecum via PI3K and ROCK pathways
Paracellular calcium transport and calcium permeability were evaluated in the presence of the transepithelial calcium gradient. Under normal conditions (Fig. 4a–d), the paracellular cecal calcium transport increased linearly with the mucosal calcium concentration (r 2 = 0.86). After exposure to PRL (Fig. 4a–d), the paracellular calcium fluxes were markedly enhanced, and the correlation between mucosal calcium concentrations and calcium fluxes still showed linearity (r 2 = 0.93). The slopes of the regression lines were significantly increased by 2.4-fold, i.e., from the control value of 63.06 ± 5.95 to 152.62 ± 9.67 cm h−1 (p < 0.001). PRL also increased calcium permeability of the cecal epithelium as demonstrated in Fig. 4e–h. The PRL-induced increases in the paracellular calcium transport and calcium permeability in the cecum were totally abolished by inhibitors of PI3K (Fig. 4a, e) and ROCK (Fig. 4c, g), but not by PKC inhibitor (Fig. 4b, f) or JAK2 inhibitor (Fig. 4d, h).
a–d Paracellular calcium transport and e–h calcium permeability (P Ca) in the cecum directly exposed to 800 ng/mL PRL in the presence and absence of PI3K inhibitor (75 µmol/L LY294002), PKC inhibitor (1 µmol/L GF109203X), ROCK inhibitor (1 µmol/L Y27632), or JAK2 inhibitor (50 µmol/L AG490). The mucosal side was bathed with solution containing various calcium concentrations, i.e., 1.25, 2.5, 5, 10, or 20 mmol/L (n = 4 per each concentration; total 120 setups used), whereas the serosal solution had calcium concentration of 1.25 mmol/L. The same values of the control and PRL-treated groups are presented in a–d and e–h with those of the inhibitor-treated groups for clear comparisons. All experiments were performed under open-circuit condition. *p < 0.001 PRL vs. control. † p < 0.001 PRL+inhibitor vs. control
As seen in Fig. 5, TER values of normal cecal epithelia were linearly increased with mucosal calcium concentration (r 2 = 0.99) as a result of the calcium-induced conductance block of the paracellular pores, similar to that reported previously [47]. Hence, Isc but not PD was gradually decreased when mucosal calcium concentration was increased (data not shown). In 800 ng/mL PRL-treated cecal epithelia, although the relationship between mucosal calcium and TER still showed linearity (r 2 = 0.99), PRL markedly reduced TER, and the slopes were reduced from the control value of 119.59 ± 3.03 to 71.01 ± 1.77 kΩ cm2 L mmol−1 (p < 0.001). Such PRL effects on TER were abolished by PI3K inhibitor (Fig. 5a) and ROCK inhibitor (Fig. 5c), but not by PKC inhibitor (Fig. 5b) or JAK2 inhibitor (Fig. 5d). Inhibitors alone and vehicle (DMSO) had no effect on TER (data not shown).
Effect of 800 ng/mL PRL on the relationship between mucosal calcium concentration and transepithelial resistance (TER) of cecal epithelium (n = 4 per each concentration) incubated with a PI3K inhibitor (75 µmol/L LY294002), b PKC inhibitor (1 µmol/L GF109203X), c ROCK inhibitor (1 µmol/L Y27632), or (d) JAK2 inhibitor (50 µmol/L AG490). The same control and PRL data are presented in a–d with those of the inhibitor-treated groups for clear comparisons. *p < 0.001 PRL vs. control. † p < 0.001 PRL+inhibitor vs. control
PRL altered Na+/Cl−-selective property of the cecal epithelium
Since the paracellular calcium transport and epithelial calcium permeability could be increased by altering the charge-selective property of cecal epithelium, we determined the absolute permeability to sodium (P Na) and chloride (P Cl) as well as the P Na/P Cl ratio, all of which are indicative of the paracellular charge selectivity [21, 47]. Under normal conditions (Fig. 6), the cecal epithelium exhibited a cation selectivity with P Na being greater than P Cl (p < 0.001), and P Na/P Cl was ∼2.0. After exposure to 800 ng/mL PRL, P Na was markedly increased by ∼2.6-fold (Fig. 6a) without any change in P Cl (Fig. 6b), thereby raising P Na/P Cl (Fig. 6c). The increases in P Na and P Na/P Cl, similar to the increase in paracellular calcium transport, were diminished by PI3K and ROCK inhibitors, but not by PKC inhibitor (Fig. 6a, c). Inhibitors alone were without effects. The results, therefore, suggested that PRL enhanced the paracellular cecal calcium transport by increasing the epithelial cation selectivity through PI3K and ROCK pathways.
a P Na, b P Cl, and c P Na/P Cl of the cecal epithelia exposed to PI3K inhibitor (75 µmol/L LY294002), PKC inhibitor (1 µmol/L GF109203X), or ROCK inhibitor (1 µmol/L Y27632) with (+PRL) and without (−PRL) 800 ng/mL PRL. DMSO was used as vehicle for inhibitor preparation. Numbers in parentheses represent the number of animals. **p < 0.01, ***p < 0.001 compared with the control group
Discussion
In the present study, we demonstrated, for the first time, that PRL stimulated the transcellular and paracellular calcium transport in rat cecum. The presence of PRLRs in cecal epithelial cells and the ability of PRLR antibody to block PRL-stimulated calcium transport confirmed direct action of PRL on this intestinal segment. It was evident that the PRL-enhanced transcellular cecal calcium transport was dependent on PI3K, PKC, and ROCK, while the enhanced paracellular calcium transport required PI3K and ROCK, but not PKC. Such PRL signalings were nongenomic, since they were observed within 60 min after PRL exposure, and were not abolished by inhibitors of gene transcription (DRB) or protein biosynthesis (cycloheximide).
Although most recent investigations have focused on calcium transport in the small intestine, the proximal large intestine, particularly the cecum, is a highly efficient site for calcium absorption [39]. Karbach and Feldmeier reported that the rat cecum, as compared to other intestinal segments, had the highest rate of calcium absorption [28]. The present calcium flux study confirmed that the cecal calcium transport was greater than that in the duodenum by ∼1.5-fold. Besides, the cecum which strongly expresses transcellular calcium transporters (Fig. 1f) is another site with sizable transcellular calcium absorption [28]. In some mammals, e.g., mole rats, the transcellular active calcium transport exclusively occurs in the proximal large intestine [41].
Physiological significance of the cecum in an overall calcium absorption was questionable because calcium may be present in the cecal lumen as a water-insoluble complex with indigestible luminal content [12]. Cecectomy also did not affect the fractional calcium absorption in 1,25(OH)2D3-repleted rats [4]. However, other studies showed that microbial fermentation in the cecum could liberate calcium from the indigestible fibers [10, 51]. Moreover, short-chain fatty acid as well as small organic acids, e.g., propionic acid, succinic acid, and lactic acid, produced during fermentation decreased the luminal pH, which in turn released calcium from the complexes [10, 36, 38]. Cecal calcium absorption becomes salient when hindgut fermentors, such as humans and rats, ingest naturally occurring resistant starch (e.g., oatmeal and pearl barley), a fermentable carbohydrate that benefits healthy individuals as well as diabetic patients [44, 51].
The aforementioned evidence also collectively suggests that the cecum has a high capacity to supply additional calcium to the body when needed, for examples, in pregnancy and lactation [42]. Coincidentally, PRL is a hormone with markedly elevated levels during these periods, and we have previously shown that it was an important hormone to enhance calcium absorption, especially in the duodenum and proximal jejunum [5]. However, PRL was without effect on calcium transport in the distal large intestine although it could regulate water absorption and inhibit the calcium-dependent Cl− and K+ secretion in the colon [34, 43]. In the present study, the cecum, which expressed essential genes for the transcellular and paracellular calcium transport, responded to PRL by increasing calcium fluxes via both transcellular and paracellular pathways, similar to that seen in the duodenum [25]. Calcium fluxes observed in the 800 ng/mL PRL-treated cecum was greater than that in the duodenum exposed to the same PRL concentration by 2-fold, i.e., ∼120 nmol h−1 cm−2 in the cecum compared to ∼60 nmol h−1 cm−2 reported in the duodenum [25]. In the presence of ∼5–20 mmol/L transepithelial calcium gradient, this PRL concentration markedly increased the amount of calcium transported by cecal epithelium from a nanomole range to micromole range. These information collectively strengthened the physiological significance of the cecal calcium absorption during hyperprolactinemic states, such as in lactating animals.
Nevertheless, nothing was known pertaining the detailed mechanisms by which PRL enhanced cecal calcium transport. The PRL-stimulated transcellular calcium absorption in the duodenum was explained by increases in the brush-border calcium uptake and PMCA activity [7]. In the cecum, the PRL effect was also abolished by inhibitors of apical calcium uptake (ruthenium red) or basolateral calcium extrusion (trifluoperazine). Regarding the cecal paracellular calcium transport, the PRL-induced increase in calcium movement through the paracellular space was explained by a decrease in TER (Fig. 5) as well as an increase in the epithelial cation selectivity, as indicated by the increased P Na and P Na/P Cl (Fig. 6), similar to that observed in Caco-2 monolayer [48]. The P Na/P Cl value of the control groups, which increased from the mobility ratio of Na+ and Cl− of ∼0.6 in free solution to ∼2.0 [17], also suggested that, under normal conditions, the cecal epithelium naturally prefers paracellular movement of cations more than anions. Generally, tight junction proteins of the claudin family undergo polymerization to form charge-selective paracellular pores [15]. Thus, the epithelial charge selectivity is determined by the fixed negative or positive charges on the extracellular loops of claudins which impede the movement of ions with the opposite charge [50]. Claudin-2, claudin-3, and claudin-12, which are also expressed in cecal epithelial cells, have been suggested to regulate the paracellular calcium transport [14, 35]. Our recent preliminary study in Caco-2 monolayer showed that an increase in cation selectivity observed after the PRL-induced claudin phosphorylation could increase the paracellular calcium movement (Nakkrasae et al. 2009, unpublished observation). However, further experiment is required to demonstrate that the PRL-induced increases in paracellular cecal calcium transport and cation selectivity are directly mediated by claudin phosphorylation.
PRL signaling pathways in the intestinal epithelial cells have been studied in the duodenum and Caco-2 intestinal-like cells [25, 48], while that in the cecum was unknown. Since cecal epithelial cells predominantly expressed PRLR-L, it was likely that PRL exerted its functions through PRLR-L, similar to that reported in Caco-2 cells [48]. In contrast, as PRLR-S lacks the cytoplasmic tails required to activate the intracellular downstream pathways, PRLR-S may act as the dominant-negative molecules to silence or reduce PRL actions [2]. Interestingly, the typical biphasic response to PRL was also demonstrated in the cecum, i.e., in contrast to the lower effective doses (600 and 800 ng/mL), 1,000 ng/mL PRL only slightly increased calcium transport. This phenomenon has been explained by inability of PRLRs to form functional dimers. At extremely high PRL concentrations, most available PRLRs were occupied as nonfunctional 1:1 complexes instead of 1:2 functional complexes needed to induce signal transduction [13, 22].
The principal PRL signaling pathways found in the cecum, i.e., PI3K, PKC, and ROCK, were consistent with those reported in duodenal epithelial cells and Caco-2 monolayer [25, 48]. Although JAK2 usually mediates PRL signals in several tissues, e.g., mammary epithelium [24], and several factors, e.g., 1,25(OH)2D3, could increase calcium uptake through PKA [30], the PRL effects herein appeared to be independent of both JAK2 and PKA. Generally, PI3K is the most upstream enzyme of several kinase targets, including PKC and ROCK known to modulate the transepithelial calcium transport and paracellular permeability [19, 27, 37, 46]. In the cecum, PKC was likely to be more important in the transcellular calcium transport than the paracellular transport, presumably by its ability to augment the basolateral calcium efflux [30]. In contrast, ROCK was essential for both transport mechanisms. It was noteworthy that activation of ROCK is commonly required to increase paracellular permeability or decrease TER in several epithelia, e.g., brain endothelium, renal proximal tubule, and human colonic epithelial monolayer [27, 45, 46]. Hence, PRL might use this common pathway to decrease TER, and increase cation selectivity and paracellular calcium permeability, thereby enhancing the paracellular calcium transport.
Finally, it could be concluded that the rat cecum was a target tissue of PRL, in which it directly stimulated the transcellular and paracellular calcium transport via the nongenomic signaling pathways. The downstream pathways for PRL signaling involved PI3K, ROCK, and PKC, the last of which mainly mediated the signal for the PRL-enhanced transcellular calcium transport. The present investigation, therefore, elaborated possible physiological roles of PRL in the cecum and provided more complete understanding of the effects of PRL on calcium homeostasis. Since the rate of cecal calcium absorption is subjected to effects of certain dietary components, e.g., resistant carbohydrates, we speculate that such nutraceuticals could be useful for enhancement of calcium absorption during lactation, when the plasma PRL surge is in the range of ∼650–800 ng/mL [1].
References
Arbogast LA, Voogt JL (1998) Endogenous opioid peptides contribute to suckling-induced prolactin release by suppressing tyrosine hydroxylase activity and messenger ribonucleic acid levels in tuberoinfundibular dopaminergic neurons. Endocrinology 139:2857–2862
Berlanga JJ, Garcia-Ruiz JP, Perrot-Applanat M, Kelly PA, Edery M (1997) The short form of the prolactin (PRL) receptor silences PRL induction of the β-casein gene promoter. Mol Endocrinol 11:1449–1457
Boass A, Lovdal JA, Toverud SU (1992) Pregnancy- and lactation-induced changes in active intestinal calcium transport in rats. Am J Physiol Gastrointest Liver Physiol 263:G127–G134
Brommage R, Binacua C, Carrie AL (1995) The cecum does not participate in the stimulation of intestinal calcium absorption by calcitriol. J Steroid Biochem Mol Biol 54:71–73
Charoenphandhu N, Krishnamra N (2007) Prolactin is an important regulator of intestinal calcium transport. Can J Physiol Pharmacol 85:569–581
Charoenphandhu N, Limlomwongse L, Krishnamra N (2001) Prolactin directly stimulates transcellular active calcium transport in the duodenum of female rats. Can J Physiol Pharmacol 79:430–438
Charoenphandhu N, Limlomwongse L, Krishnamra N (2006) Prolactin directly enhanced Na+/K+- and Ca2+-ATPase activities in the duodenum of female rats. Can J Physiol Pharmacol 84:555–563
Charoenphandhu N, Wongdee K, Teerapornpuntakit J, Thongchote K, Krishnamra N (2008) Transcriptome responses of duodenal epithelial cells to prolactin in pituitary-grafted rats. Mol Cell Endocrinol 296:41–52
de Boland AR, Norman A (1990) Evidence for involvement of protein kinase C and cyclic adenosine 3′, 5′ monophosphate-dependent protein kinase in the 1, 25-dihydroxyvitamin D3-mediated rapid stimulation of intestinal calcium transport, (transcaltachia). Endocrinology 127:39–45
Duflos C, Bellaton C, Pansu D, Bronner F (1995) Calcium solubility, intestinal sojourn time and paracellular permeability codetermine passive calcium absorption in rats. J Nutr 125:2348–2355
Favus MJ (1985) Factors that influence absorption and secretion of calcium in the small intestine and colon. Am J Physiol 248:G147–G157
Favus MJ, Pak C (2001) Evidence for absorption of ionic calcium and soluble calcium complexes by the duodenum and cecum in the rat. Am J Ther 8:425–431
Fuh G, Colosi P, Wood WI, Wells JA (1993) Mechanism-based design of prolactin receptor antagonists. J Biol Chem 268:5376–5381
Fujita H, Sugimoto K, Inatomi S, Maeda T, Osanai M, Uchiyama Y, Yamamoto Y, Wada T, Kojima T, Yokozaki H, Yamashita T, Kato S, Sawada N, Chiba H (2008) Tight junction proteins claudin-2 and -12 are critical for vitamin D-dependent Ca2+ absorption between enterocytes. Mol Biol Cell 19:1912–1921
Furuse M, Tsukita S (2006) Claudins in occluding junctions of humans and flies. Trends Cell Biol 16:181–188
Garcia J, Carabano R, Perez-Alba L, de Blas JC (2000) Effect of fiber source on cecal fermentation and nitrogen recycled through cecotrophy in rabbits. J Anim Sci 78:638–646
Greger R (1996) Epithelial transport. In: Greger R, Windhorst U (eds) Comprehensive human physiology: from cellular mechanisms to integration. Springer, Berlin, pp 1217–1232
Hawkins PT, Anderson KE, Davidson K, Stephens LR (2006) Signalling through class I PI3Ks in mammalian cells. Biochem Soc Trans 34:647–662
Hirsch E, Costa C, Ciraolo E (2007) Phosphoinositide 3-kinases as a common platform for multi-hormone signaling. J Endocrinol 194:243–256
Hoenderop JG, Nilius B, Bindels RJ (2005) Calcium absorption across epithelia. Physiol Rev 85:373–422
Hou J, Paul DL, Goodenough DA (2005) Paracellin-1 and the modulation of ion selectivity of tight junctions. J Cell Sci 118:5109–5118
Ilondo MM, Damholt AB, Cunningham BA, Wells JA, de Meyts P, Shymko RM (1994) Receptor dimerization determines the effects of growth hormone in primary rat adipocytes and cultured human IM-9 lymphocytes. Endocrinology 134:2397–2403
Imaizumi MO, Sakurai T, Nakamura S, Nakanishi S, Matsuda Y, Muramatsu S, Nonomura Y, Kumakura K (1992) Inhibition of Ca2+-dependent catecholamine release by myosin light chain kinase inhibitor, wortmannin, in adrenal chromaffin cells. Biochem Biophys Res Commun 185:1016–1021
Jahn GA, Daniel N, Jolivet G, Belair L, Bole-Feysot C, Kelly PA, Djiane J (1997) In vivo study of prolactin (PRL) intracellular signalling during lactogenesis in the rat: JAK/STAT pathway is activated by PRL in the mammary gland but not in the liver. Biol Reprod 57:894–900
Jantarajit W, Thongon N, Pandaranandaka J, Teerapornpuntakit J, Krishnamra N, Charoenphandhu N (2007) Prolactin-stimulated transepithelial calcium transport in duodenum and Caco-2 monolayer are mediated by the phosphoinositide 3-kinase pathway. Am J Physiol Endocrinol Metab 293:E372–E384
Kahle KT, Macgregor GG, Wilson FH, Van Hoek AN, Brown D, Ardito T, Kashgarian M, Giebisch G, Hebert SC, Boulpaep EL, Lifton RP (2004) Paracellular Cl− permeability is regulated by WNK4 kinase: insight into normal physiology and hypertension. Proc Natl Acad Sci USA 101:14877–14882
Kapus A, Szászi K (2006) Coupling between apical and paracellular transport processes. Biochem Cell Biol 84:870–880
Karbach U, Feldmeier H (1993) The cecum is the site with the highest calcium absorption in rat intestine. Dig Dis Sci 38:1815–1824
Khanal RC, Nemere I (2008) Regulation of intestinal calcium transport. Annu Rev Nutr 28:179–196
Khanal RC, Nemere I (2008) Endocrine regulation of calcium transport in epithelia. Clin Exp Pharmacol Physiol 35:1277–1287
Kimizuka H, Koketsu K (1964) Ion transport through cell membrane. J Theor Biol 6:290–305
Kornberg A, Daft FS, Sebrell WH (1944) Mechanism of production of vitamin K deficiency in rats by sulfonamides. J Biol Chem 155:193–200
Krause LJ, Forsberg CW, O’Connor DL (1996) Feeding human milk to rats increases Bifidobacterium in the cecum and colon which correlates with enhanced folate status. J Nutr 126:1505–1511
Krishnamra N, Ousingsawat J, Limlomwongse L (2001) Study of acute pharmacologic effects of prolactin on calcium and water transport in the rat colon by an in vivo perfusion technique. Can J Physiol Pharmacol 79:415–421
Kutuzova GD, DeLuca HF (2004) Gene expression profiles in rat intestine identify pathways for 1, 25-dihydroxyvitamin D3 stimulated calcium absorption and clarify its immunomodulatory properties. Arch Biochem Biophys 432:152–166
Levrat MA, Remesy C, Demigne C (1991) High propionic acid fermentations and mineral accumulation in the cecum of rats adapted to different levels of inulin. J Nutr 121:1730–1737
Little D, Dean RA, Young KM, McKane SA, Martin LD, Jones SL, Blikslager AT (2003) PI3K signaling is required for prostaglandin-induced mucosal recovery in ischemia-injured porcine ileum. Am J Physiol Gastrointest Liver Physiol 284:G46–G56
Mineo H, Amano M, Minaminida K, Chiji H, Shigematsu N, Tomita F, Hara H (2006) Two-week feeding of difructose anhydride III enhances calcium absorptive activity with epithelial cell proliferation in isolated rat cecal mucosa. Nutrition 22:312–320
Nellans HN, Goldsmith RS (1981) Transepithelial calcium transport by rat cecum: high-efficiency absorptive site. Am J Physiol 240:G424–G431
Nellans HN, Goldsmith RS (1983) Mucosal calcium uptake by rat cecum: identity with transcellular calcium absorption. Am J Physiol 244:G618–G622
Pitcher T, Buffenstein R (1995) Intestinal calcium transport in mole-rats (Cryptomys damarensis and Heterocephalus glaber) is independent of both genomic and non-genomic vitamin D mediation. Exp Physiol 80:597–608
Prentice A (2000) Calcium in pregnancy and lactation. Annu Rev Nutr 20:249–272
Puntheeranurak S, Schreiber R, Spitzner M, Ousingsawat J, Krishnamra N, Kunzelmann K (2007) Control of ion transport in mouse proximal and distal colon by prolactin. Cell Physiol Biochem 19:77–88
Robertson MD, Bickerton AS, Dennis AL, Vidal H, Frayn KN (2005) Insulin-sensitizing effects of dietary resistant starch and effects on skeletal muscle and adipose tissue metabolism. Am J Clin Nutr 82:559–567
Samarin SN, Ivanov AI, Flatau G, Parkos CA, Nusrat A (2007) Rho/Rho-associated kinase-II signaling mediates disassembly of epithelial apical junctions. Mol Biol Cell 18:3429–3439
Stamatovic SM, Dimitrijevic OB, Keep RF, Andjelkovic AV (2006) Protein kinase Cα-RhoA cross-talk in CCL2-induced alterations in brain endothelial permeability. J Biol Chem 281:8379–8388
Tang VW, Goodenough DA (2003) Paracellular ion channel at the tight junction. Biophys J 84:1660–1673
Thongon N, Nakkrasae LI, Thongbunchoo J, Krishnamra N, Charoenphandhu N (2008) Prolactin stimulates transepithelial calcium transport and modulates paracellular permselectivity in Caco-2 monolayer: mediation by PKC and ROCK pathways. Am J Physiol Cell Physiol 294:C1158–C1168
Thongon N, Nakkrasae LI, Thongbunchoo J, Krishnamra N, Charoenphandhu N (2009) Enhancement of calcium transport in Caco-2 monolayer through PKCζ-dependent Cav1.3-mediated transcellular and rectifying paracellular pathways by prolactin. Am J Physiol Cell Physiol (in press). doi: 10.1152/ajpcell.00053.2009
Van Itallie CM, Anderson JM (2006) Claudins and epithelial paracellular transport. Annu Rev Physiol 68:403–429
Younes H, Demigne C, Remesy C (1996) Acidic fermentation in the caecum increases absorption of calcium and magnesium in the large intestine of the rat. Br J Nutr 75:301–314
Acknowledgments
This work was supported by the Thailand Research Fund (RSA5180001 to N. Charoenphandhu) and the Mahidol University Postdoctoral Fellowship Program (to L.-i. Nakkrasae).
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Figure S1
Transepithelial calcium flux in 800 ng/mL PRL-exposed cecal tissues under open- and short-circuit conditions. The tissue was bathed on both sides with 1.25 mmol/L Ca2+-containing solution. Numbers in parentheses represent the number of animals. **p < 0.01 compared with its respective control group (GIF 15 kb)
Supplemental Figure S2
Mucosa (M)-to-serosa (S) and S-to-M calcium fluxes in 800 ng/mL PRL-exposed cecal tissues under short-circuit condition. The removed cecal tissue from a rat was divided into two pieces for M-to-S and S-to-M studies. Net calcium flux was calculated by subtracting S-to-M calcium flux from M-to-S calcium flux. Each tissue was bathed on both sides with 1.25 mmol/L Ca2+-containing solution. Numbers in parentheses represent the number of animals. **p < 0.01 compared with its respective control group (GIF 17 kb)
Rights and permissions
About this article
Cite this article
Kraidith, K., Jantarajit, W., Teerapornpuntakit, J. et al. Direct stimulation of the transcellular and paracellular calcium transport in the rat cecum by prolactin. Pflugers Arch - Eur J Physiol 458, 993–1005 (2009). https://doi.org/10.1007/s00424-009-0679-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-009-0679-6