Abstract
Purpose
This study aims to evaluate the efficacy of admission contrast-enhanced CT scans in formulating strategies for performing early laparoscopic cholecystectomy in cases of acute gallstone pancreatitis.
Methods
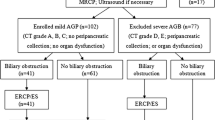
Patients diagnosed with acute gallstone pancreatitis underwent a CT scan upon admission (after at least 24 h from symptom onset) to confirm diagnosis and assess peripancreatic fluid, collections, gallstones, and common bile duct stones. Patients with mild acute gallstone pancreatitis, following the Atlanta classification and Baltazar score A or B, were identified as candidates for early cholecystectomy (within 72 h of admission).
Results
Within the analyzed period, 272 patients were diagnosed with mild acute gallstone pancreatitis according to the Atlanta Guidelines. A total of 33 patients (12.1%) were excluded: 17 (6.25%) due to SIRS, 10 (3.6%) due to local complications identified in CT (Balthazar D/E), and 6 (2.2%) due to severe comorbidities. Enhanced CT scans accurately detected gallstones, common bile duct stones, pancreatic enlargement, inflammation, pancreatic collections, and peripancreatic fluid. Among the cohort, 239 patients were selected for early laparoscopic cholecystectomy. Routine intraoperative cholangiogram was conducted in all cases, and where choledocholithiasis was present, successful treatment occurred through common bile duct exploration. Only one case required conversion from laparoscopic to open surgery. There were no observed severe complications or mortality.
Conclusion
Admission CT scans are instrumental in identifying clinically stable patients with local tomographic complications that contraindicate early surgery. Patients meeting the criteria for mild acute gallstone pancreatitis, as per Atlanta guidelines, without SIRS or local complications (Baltazar D/E), can safely undergo early cholecystectomy within the initial 72 h of admission.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute pancreatitis is one of the most common causes of emergency admission. Alcoholism, hyperlipidemia and gallstones are three of the most frequent causes of pancreatitis. Acute pancreatitis predominantly arises from gallstones and its surgical treatment is fundamental. Its genesis typically involves the transient passage of a gallstone through the Vater's ampulla [1, 2].
Consensus currently holds that in cases of severe acute gallstone pancreatitis (AGP), cholecystectomy should be delayed until the local and systemic inflammatory condition fully resolves—typically around six weeks post-AGP because the inflammation and oedema could distort the biliary anatomy [3]. However, the optimal approach for mild AGP remains a topic of contention, whether to perform surgery within 48 to 72 h of admission or delay cholecystectomy for at least six weeks [4, 5].
Various studies have highlighted the safety and efficacy of early cholecystectomy within 48–72 h of hospital arrival for preventing recurrent pancreatitis in mild to moderate AGP cases without local complications of Balthazar type D/E [3, 6]. This study aims to evaluate the utility of routine admission computed tomography as an adjunctive tool in identifying eligible candidates for early surgical intervention.
Material and methods
This study is an observational, retrospective study. A retrospective cohort comprising patients over 18 years diagnosed with AGP between January 2009 and July 2019 at the General Surgery Service of the Hospital Italiano in Buenos Aires was selected. All chosen patients underwent an abdominal computed tomography (CT) scan with intravenous contrast at admission, at least 24 h after symptom onset. This study received approval from the Institutional Ethics Committee (Protocol number 2907) and adhered to the Helsinki Declaration. The outcomes have been reported such as incidence of complications and confidence interval.
The 2019 Atlanta Guidelines [7] were used to diagnose pancreatitis, considering: (A) Acute onset of severe and persistent epigastric pain, often radiating to the back, (B) serum amylase and/or lipase activity at least three times the upper limit of normal and (C) characteristic findings of acute pancreatitis on dynamic CT with intravenous contrast, occasionally supplemented by magnetic resonance imaging (MRI) or abdominal ultrasound.
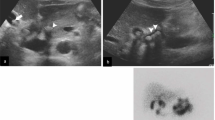
All patients underwent CT within 24 h of hospital admission to gauge pancreatitis severity and guide subsequent action, regardless of confirmation by other diagnostic criteria.
Severity assessment followed the Atlanta Guidelines and Balthazar CT criteria. Mild AGP, per the Atlanta guidelines, denotes no organ failure, typically with a short course and spontaneous resolution. Moderately severe AGP involves transient organ failure (lasting < 48 h) and/or local complications. Severe AGP entails persistent organ failure (> 48 h), often with local and systemic complications.
Balthazar criteria include (A) normal pancreas, (B) pancreatic enlargement, (C) inflammation of the pancreatic and/or peripancreatic fat, (D) single collection of peripancreatic fluid and (E) two or more collections of fluids and/or retroperitoneal air.
Our assessment focused on the safety of early laparoscopic cholecystectomy (within 72 h of abdominal pain onset) in patients without SIRS or local complications from CT. Additionally, we evaluated the laparoscopic approach's efficacy in addressing underlying biliary pathology, along with hospitalization duration and discharge day in correlation with Balthazar grades in AGP patients.
Postoperative complications at 90 days were categorized using the Clavien–Dindo (CD) classification: mild (CD I/II), severe (CD III–IV), and fatal (CD V) [8, 9]. Patients with associated acute cholangitis (bilirubin > 4 mg/dL, fever, and/or leukocytosis) and/or cholecystitis or with local imaging (Balthazar D/E) were excluded.
Results
During the analyzed period, 272 patients were diagnosed with mild acute gallstone pancreatitis according to the Atlanta Guidelines. However, 33 patients (12.1%) were excluded: 17 due to SIRS (6.25%), 10 with local complications found in CT scans (Balthazar D/E) (3.6%), and 6 due to severe comorbidities (2.2%). The average age of the 239 remaining patients was 53 years, with a median amylase value of 1900 UI/L at admission. The median range for days until discharge was 4 days. The severity distribution according to the Balthazar grade was equal, with 33% in each group A, B, and C. The enhanced CT scan accurately detected gallstones, common bile duct stones, pancreatic enlargement, inflammation, pancreatic collections, and peripancreatic fluid. Out of the entire cohort, 239 patients were selected as candidates for early laparoscopic cholecystectomy. In all cases, routine intraoperative cholangiograms were performed. If choledocholithiasis was present, it was successfully treated with common bile duct exploration. Only one case required conversion from laparoscopic to open surgery.
Acute gallstone pancreatitis is more often caused when common bile duct stone is present, in our study 28 patients (11,7%) out of the 239 patients had common bile duct stone in addition to gallbladder stones that were treated with transcystic choledocholithotomy. Only three of them needed ERCP for a second look.
Notably, no severe complications or mortality were observed. The incidence of complications was 2.25% (0.73–5.17) CI (95%—confidence interval), and none exceeded D-C level III (Tables 1 and 2) (Fig. 1.).
Discussion
Existing literature strongly advocates early laparoscopic cholecystectomy for patients experiencing mild pancreatitis, a safety aspect our study also corroborates [6]. This approach notably slashes hospital stays, reduces expenses, and averts potential complications like cholangitis or cholecystitis [3, 10, 11]. When appropriately indicated, this procedure exhibits remarkably low morbidity rates according to numerous reports [12]. However, cautious consideration is imperative for patients with moderately severe or severe acute biliary pancreatitis, given its association with heightened postoperative mortality and morbidity [13].
The specific timing for early cholecystectomy lacks a uniform definition. While UK guidelines recommend avoiding a delay beyond two weeks post-hospital discharge and preferably conducting the procedure during admission, the International Association of Pancreatology suggests surgery after resolving the underlying inflammatory condition. Conversely, the American Gastroenterological Association suggests an optimal window of 2 to 4 weeks for surgery [14,15,16,17,18]. In mild pancreatitis cases, early surgery does not significantly affect morbidity but might elevate the risk of recurrence, accompanied by negative economic implications [7]. There is a widespread lack of adherence to evidence-based guidelines in managing acute biliary pancreatitis, evident in the variability in optimal timing for CT scans, use of prophylactic antibiotics, early enteral feeding, and the implementation of early cholecystectomy strategies [19].
All patients in our study underwent clinical evaluation as per the mentioned parameters to gauge the condition's severity. Every case involved an abdominopelvic CT scan with intravenous contrast, crucial for classifying pancreatitis based on Balthazar criteria [20]. This approach ensured exclusion of patients with seemingly mild symptoms but underlying extensive necrosis or fluid collections unsuitable for early surgery. Research demonstrates that after 12 h, observed necrosis on CT ceases to evolve further. Inadequate evaluation within the initial 48 h often overlooks late necrosis. Among the 249 patients who underwent tomography, 77 (30.9%) had Balthazar A, 65 (26.1%) B, 97 (38.9%) C, and 10 (4.1%) D/E classifications.
Patients scoring between A and C underwent early cholecystectomy within 48–72 h. We performed laparoscopic cholecystectomy with systematic intraoperative cholangiography, omitting additional preoperative choledocholithiasis studies. In instances of choledocholithiasis, simultaneous transcystic bile duct exploration was our initial approach, proven safe and viable for this population. Choledochotomy was reserved for complex cases.
The morbidity rates, as demonstrated in the results, were remarkably low, with no complications exceeding Dindo Clavien [8, 9] level III. The incidence of complications was 2.25% (0.73–5.17) CI.
Most patients in our study were discharged within 48 h post-surgery. Consistent with other studies, our findings reinforce the efficacy of early laparoscopic cholecystectomy, indicating reduced surgery time and hospitalization duration for all early-operated patients during admission. Regarding patients classified as D/E, 10 (4.1%) did not meet clinical criteria for moderate/severe pancreatitis. This underscores the importance of tomography, which effectively ruled out candidates for cholecystectomy within the initial 72 h based solely on clinical criteria.
The primary limitation of our study is its retrospective nature, where none of the patients diagnosed with clinical mild AGP and a Balthazar Score D/E in CT underwent early cholecystectomy.
Conclusion
In light of current scientific understanding, performing a cholecystectomy within the initial 72 h in patients without SIRS or local complications is deemed safe. This determination is made through adherence to the criteria outlined in the Atlanta guidelines and the Balthazar tomographic classification. Conducting an admission tomography (within the first 24 h) in acute pancreatitis cases serves as a valuable tool to identify clinically stable patients (mild-moderate) exhibiting Balthazar D/E tomographic irregularities. These individuals warrant consideration for a delayed cholecystectomy, aiding in the prevention of potential complications.
Data Availability
Data is provided within the manuscript.
References
Moody N, Adiamah A, Yanni F, Gomez D (2019) Meta-analysis of randomized clinical trials of early versus delayed cholecystectomy for mild gallstone pancreatitis. Br J Surg 106:1442–51. https://doi.org/10.1002/bjs.11221
Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB, Maisonneuve P (2009) Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol 104:2797–805. https://doi.org/10.1038/ajg.2009.405
Group DPS, Dutch Pancreatitis Study Group, Bakker OJ, van Santvoort HC, Hagenaars JC, Besselink MG et al (2011) Timing of cholecystectomy after mild biliary pancreatitis. Br J Surg 98:1446–54. https://doi.org/10.1002/bjs.7587
Aboulian A, Chan T, Yaghoubian A, Kaji AH, Putnam B, Neville A et al (2010) Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis. Ann Surg 251:615–9. https://doi.org/10.1097/sla.0b013e3181c38f1f
El-Dhuwaib Y, Deakin M, David GG, Durkin D, Corless DJ, Slavin JP (2012) Definitive management of gallstone pancreatitis in England. Ann R Coll Surg Eng. 94:402–6. https://doi.org/10.1308/003588412x13171221591934
Giuffrida P, Biagiola D, Cristiano A, Ardiles V, de Santibañes M, Sanchez Clariá R et al (2020) Laparoscopic cholecystectomy in acute mild gallstone pancreatitis: how early is safe? Updates Surg 72(1):129–135
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG et al (2013) Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 62(1):102–111
Dindo D. The Clavien–Dindo Classification of Surgical Complications. Treatment of Postoperative Complications After Digestive Surgery. 2014. p. 13–7. https://doi.org/10.1007/978-1-4471-4354-3_3
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al (2009) The Clavien-Dindo Classification of Surgical Complications. Ann Surg 250:187–96. https://doi.org/10.1097/sla.0b013e3181b13ca2
Pellegrini CA (1993) Surgery for gallstone pancreatitis. Am J Surg 165:515–8. https://doi.org/10.1016/s0002-9610(05)80952-3
Kelly TR, Elliott DW (1990) Proper timing of surgery for gallstone pancreatitis. Am J Surg 159:361–2. https://doi.org/10.1016/s0002-9610(05)81270-x
Dubina ED, de Virgilio C, Simms ER, Kim DY, Moazzez A (2018) Association of early vs delayed cholecystectomy for mild gallstone pancreatitis with perioperative outcomes. JAMA Surg 153:1057. https://doi.org/10.1001/jamasurg.2018.2614
Di Martino M, Ielpo B, Pata F et al (2023) Timing of cholecystectomy after moderate and severe acute biliary pancreatitis. JAMA Surg 158(10):e233660. https://doi.org/10.1001/jamasurg.2023.3660
Pancreatitis UKWP on A, UK Working Party on Acute Pancreatitis (2005) UK guidelines for the management of acute pancreatitis. Gut 549:iii1-9. https://doi.org/10.1136/gut.2004.057026
Uhl W, Warshaw A, Imrie C, Bassi C, McKay CJ, Lankisch PG et al (2002) IAP Guidelines for the surgical management of acute pancreatitis. Pancreatology 2:565–73. https://doi.org/10.1159/000067684
International association of pancreatology. https://internationalpancreatology.org/. Accessed 18 June 2024
American Gastroenterological Association. https://gastro.org/. Accessed 18 June 2024
UK guidelines for the management of acute pancreatitis Gut (2005) 54:iii1-iii9. https://gut.bmj.com/content/54/suppl_3/iii1. Accessed 18 June 2024
Podda M, Pellino G, Coccolini F et al (2021) Compliance with evidence-based clinical guidelines in the management of acute biliary pancreatitis: the MANCTRA-1 study protocol. Updates Surg 73:1757–1765. https://doi.org/10.1007/s13304-021-01118-z
Raghuwanshi S, Gupta R, Vyas MM, Sharma R (2016) CT Evaluation of Acute Pancreatitis and its Prognostic Correlation with CT Severity Index. J Clin Diagn Res 10(6):TC06-11
Author information
Authors and Affiliations
Contributions
S.K, M.G and F.H wrote the main manuscript. M.D.S was the main reviewer of the manuscript. V.A helped with the statistics and the interpretation of data R.S.C, O.M and J.P helped with conception and design of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Küstner, S., Gallardo, M., Higuera, F. et al. Early laparoscopic cholecystectomy in acute mild gallstone pancreatitis. Is there a role for routine admission contrast-enhanced CT Scan?. Langenbecks Arch Surg 409, 219 (2024). https://doi.org/10.1007/s00423-024-03394-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03394-w