Abstract
Aims
Colon cancer is the most common intra-abdominal cancer in older people. In the elderly with cancer, clinical decision making is often complicated by the effects of aging. However, as life expectancy continues to rise, more people aged 80 and older will present with colorectal cancer and may need major surgery.
Methods
Between 2000 and 2020 we operated on 352 patients aged 80 and older for colorectal cancer. We reviewed the case-notes of these patients and made a survival analysis for those patients who had a surgical resection of the tumor.
Results
In 20 patients a palliative procedure was performed. Three hundred and thirty-two (332) patients had a colorectal cancer resected. Of these, 57 patients died within 90 days postoperatively. Survival analysis was done for 275 patients who were alive longer than 90 days postoperatively. The overall 5-year survival in this group is 41.5%. There was no significant difference in postoperative survival between patients over the age of 85 and patients aged 80–84 at the time of operation. The survival of patients with stage IV colorectal adenocarcinoma is significantly worse than survival in stage I–III patients (Cox-Mantel log-rank test p < 0.001).
Conclusions
After exclusion of the patients in the 90-day mortality group the overall 5-year survival in octogenarians who had a resection of a colorectal cancer was 41.5%. The most difficult problem is to choose the right treatment for the right patient. Optimal surgical and adjuvant treatment should not be denied to these older patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Life expectancy for both men and women continues to rise. In 2018 in Belgium life expectancy at birth was 81.5 years for the whole population, or 83.7 years for women and 79.2 years for men. In Flanders (northern part of Belgium) life expectancy at birth is higher (82.3 years) (www.statbel.fgov.be accessed June 13th, 2020). Historically gains in life expectancy have been attributed to a reduction in early-life mortality. More recently however data show evidence for a decline in late-life mortality [1]. In the USA, people aged above 85 years are projected to be the fastest growing group of the senior population during this century, rising from 5 to 18 million by 2050. Once an individual reaches the age of 80, life expectancy is 8.3 years and at 85 it is 6.0 years.
Not only life expectancy increases but also health and quality of life of senior adults are improving.
In older persons with cancer, clinical decision making is often complicated by the effects of aging. Age alone is no longer the only parameter to be considered when dealing with medical problems in the older patient, and co-morbidity, geriatric syndromes, and social factors play a more important role when deciding to start anti-cancer treatment.
Chronological aging, which is the passage of chronological time, should be differentiated from biological aging or senescence, which is affected by different factors such as diet, race, sex, hormonal balance, physical activity, and smoking.
The age of patients treated with invasive and complex procedures is rising, and more senior adult patients undergo complex surgical treatment.
Colorectal cancer is the most common intra-abdominal cancer in the older population. The risks related to abdominal surgery are significant but colon and rectal cancer surgery also improves the quality of life of the older patient, even if the surgery would not prevent the progression of metastases outside the intestine [2].
In this article, our experience with older patients (aged 80 and older) who were operated for colorectal cancer between 2000 and 2020 is described and discussed.
Patients and methods
Data collection
We reviewed the case-notes of all patients aged 80 and older who had surgical treatment for colorectal cancer in our department from October 2000 till February 2020. In this period laparoscopic surgery for colorectal cancer was introduced (from 2005), and we started to use ERAS (enhanced recovery after surgery) protocols (from 2009) in the peri-operative period. Formal comprehensive geriatric assessments were introduced in our department since February 2020.
We found 352 patients aged 80 and older who had surgical treatment for colorectal cancer in our surgical oncology database. In 20 patients we performed a palliative procedure (bypass-procedure, derivative stoma). In 332 patients we were able to remove the malignant process.
The postoperative pathologic diagnosis and staging were recorded. The date of death was recorded, and for all patients still alive we recorded the date of the last medical contact (December 2021). The minimal follow-up for all patients still alive postoperatively was 20 months. Peri-operative mortality was defined as mortality within 90 days after the surgical procedure. Survival (months) and follow-up were counted from the day of surgery.
Statistical analysis
Mean and median were calculated by standard methods. Groups were compared by Chi-square tests and means by Student’s t test.
We performed Kaplan–Meier survival analysis for all patients who survived more than 90 days postoperatively.
SPSS 26 and Graphpad prism (version 10) were used for the statistics.
Results
In this period (Oct 2000–Feb 2020) 1543 patients were operated on for colorectal cancer in our department. Three hundred and fifty-two patients in this group (22.8%) were 80 years or older at the time of the operation.
Of these three hundred and fifty-two (352) patients, 20 patients did not have the colorectal tumor resected (Table 1). In this group there were 4 patients who had pre-operative radiotherapy for a rectum carcinoma and a diverting colostomy. One of these patients was still alive more than 10 years after the surgery.
We identified 332 patients, aged 80 and older who had a surgical resection for colorectal cancer. There were 167 men and 165 women. In this group 202 patient were between 80 and 84 years at the time of surgery. One hundred and thirty patients were 85 or older at the time of surgery. A colorectal resection with primary anastomosis was performed in 293 patients. A resection without anastomosis (Hartmann’s procedure, abdominoperineal rectum resection) was performed in 34 patients. Local resection (trans anal rectal cancer resection) was done in 5 patients.
In Table 2 the surgical procedures performed are shown.
Thirty-seven (37) patients died within 30 days postoperatively (11.4%). Twenty patients were in the age group 80–84 (20/202 (9.9%)), 17 patients in the aged over 85 group (17/130 (13.1%)). In this group (30-day mortality) end-of-life decisions were made in 12/37 (32.4%) of patients.
Fifty-seven (57) died within 90 days postoperatively (17.2%). Forty-seven patients (47/57) in the 90-day mortality group had a colorectal resection with primary anastomosis. An anastomotic leak was recorded in 16 of these 47 patients (34.0%).
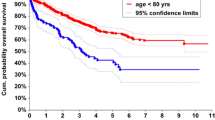
Two hundred and seventy-five (275) patients survived more than 90 days postoperatively. In this group there were 131 men and 144 women. Kaplan–Meier survival analysis was done for this group of 275 patients who survived more than 90 days postoperatively. The overall 5-year survival of this group is 41.5% (Fig. 1).
The 5-year survival rate was significantly better in women (47.4%) compared to men (35.3%) (Cox-Mantel log-rank test p=0.015, this result is significant at p<0.05); the overall 10-year survival is 15.4% (women 19.9% men 10.13%) (Fig. 2).
There was no significant difference in postoperative survival between the group of patients operated on over the age of 85 and the group of patients aged 80–84 at the date of operation (Fig. 3).
The survival of patients with stage IV colorectal adenocarcinoma is significantly worse than survival in stage I–III patients (Cox-Mantel log-rank test p<0.001) (Fig. 4).
Discussion
Older patients are an important surgical challenge due to the complexity of comorbid conditions coupled with the physiologic changes that occur with aging.
Almost 75 years ago, Welch [3] reported in his large series of abdominal operations in patients over 70 years a peri-operative mortality of 20.7%. His conclusion at that time was that surgery is safe but that the aged patient requires intensified peri-operative management.
Chronological age as such does not affect the postoperative morbidity and mortality or the long-term survival of cancer surgery in patients with solid tumors. In the 1983 Congress of the Royal Belgian Society for Surgery, a session devoted to surgery in patients over 80 years showed that surgery in this group of patients with colonic obstruction resulted in a morbidity of 65% and a mortality of 41% [4].
In a study on gastrointestinal surgery not limited to cancer in patients over the age of 80 years, the overall postoperative mortality was 23% [5]. The following factors were associated with a higher mortality rate: age over 85 years, American Society of Anaesthesiologists (ASA) score 3 or higher, surgery for cancer, peritonitis, palliative, and emergency surgery.
In 2005 Damhuis et al. [6] reported a 30-day postoperative mortality of 8% in the group patients aged 80–84 and 13% in the group aged over 85 for colorectal cancer surgery.
Pirrera et al. [7] reported in 2016 similar a 30-day postoperative mortality (8.2%) in the ≥ 80 group. In this study, age ≥ 80 was significantly influencing 30-day mortality in surgery for carcinoma of colon and rectum compared to 30-day mortality in patients aged 70–80.
These outcomes show the importance of patient selection, and traditionally this has been based on good clinical practice, consisting of clinical judgement with performance status and organ function parameters. In 2003 Lichtman wrote that there seems to be a need for a more comprehensive tool of pre-treatment assessment so that the potential complications in the treatment of older patients can be predicted and avoided [8].
Another important factor complicating patient selection is the heterogeneity of the older patient group. There are competent and active individuals as well as frail and cognitively impaired patients. Several scoring systems are used to assess the patients’ surgical risk. In a study, published in the Journal of the American College of Surgery in 2004, it was shown that in elderly people, over 80 years, the surgical risk (peri-operative mortality) was equal or less than 1% if the patient had an ASA score of 2; in patient classified ASA 4 the peri-operative mortality did rise to 25% [9]. Later similar results were seen in a study on major emergency abdominal surgery in patients over 85 years [10]. The authors concluded that with an overall mortality rate of over 30% and with the clear correlation between increased mortality and higher ASA score, the place of palliative (less invasive) treatment must remain a major consideration for patients in the age group over 85 classified ASA III or higher [9, 10].
Many tools and scores have been developed to help the decision-making process. The general health condition of onco-geriatric surgical candidates can be defined by the Preoperative Assessment of Cancer in the Elderly (PACE) [11]. In addition to comprehensive geriatric assessment (CGA), PACE also incorporates several tools used in surgical risk assessment. Prevention of postoperative complications can contribute to better 1-year and long-term survival. For prevention of postoperative complications in older patients, the involvement of a multi-disciplinary team in perioperative decision- making and care, in addition to tailor-made surgical and medical strategies, can be helpful. This team, possibly with use of a CGA, can help to select those patients who might benefit from additional measures in the preoperative period to prevent complications. The CGA, which focuses not only on physical domains but also on cognition and functioning, has proven to be useful in the detection of frail patients who are at an increased risk for developing postoperative complications. [12]. In their study on survival outcome on operated and non-operated elderly patients with rectal cancer Bhangu et al. [13] found that overall survival and cancer specific survival diverge. It appears that older patients go forward to die of other causes than cancer, hence justifying curative surgery. These benefits are contrary to common expectation, and they support the consideration of maximal therapy regardless of age in selected patients deemed to be fit.
The crucial role of frailty assessment in predicting the outcome after colorectal cancer surgery was recently addressed in the International GOSAFE study [14]. Good quality of life and staying independent are essential outcome factors in colorectal cancer surgery in older patients. Predictors for failing to achieve these essential outcomes were defined in this study and can be used in preoperative counseling of these patients and their families [15].
The estimation of the patient’s life expectancy is another important factor in the counseling of octogenarians and their family: if this is short the patient may not live long enough to benefit from his treatment or to experience any problems caused by cancer.
In Belgium the average life expectancy of a healthy patient at the age of 80 was 8.66 years in 2020; for an 85-year-old patient this was 5.97 years. In 2000 the average life expectancy for these patients was 7.89 and 5.59 years (www.statbel.fgov.be accessed on 23/01/2022).
Gastro-intestinal malignancy is common in older patients, and this condition has a far worse prognosis if treated under emergency conditions. It is therefore important that symptomatic older patients are diagnosed at an earlier stage.
Colonoscopy can be performed safely and successfully in the elderly. Malignancy is found in 4–60% of symptomatic patients or in patients with suggestive radiographic findings [16].
Colon resections are performed at an acceptably low morbidity and mortality rate in the elderly, while these rates are higher in rectal cancer, especially if a low anastomosis is made.
End-of-life decisions play an important role in the peri-operative period. Patients and their family should clearly state their health care–related priorities, such as the importance of prolonging life, preserving independence, or maintaining quality of life before deciding to have an operation. A surgical risk calculator, such as the one proposed by the American College of Surgeons, might be helpful in this process.
Conclusions
As life expectancy is increasing, the group of older patients (≥80 years) with cancer will grow. This patient group represents an important part of the patients (22.8%) we treated surgically in the time frame we observed. In this study we present the survival in octogenarians who had a colorectal cancer surgery. The overall 5-year survival after exclusion of those patients that died within 90 days postoperatively was 41.5%. The most difficult problem is to choose the right treatment for the right patient. A CGA and the more surgery-specific PACE are valuable tools in this decision-making process. Good quality of life and staying independent are essential outcome factors in colorectal cancer surgery in older patients. Using the predictors for failing to achieve these essential outcomes as defined in the GOSAFE study [15] will refine the indications for major cancer surgery and further improve perioperative outcome.
Optimal surgical and adjuvant treatment should not be denied to older patients [13, 16, 17].
Data Availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Dong X, Milholland B, Vijg J (2016) Evidence for a limit to human lifespan. Nature 538(7624):257–259. https://doi.org/10.1038/nature19793
Ng O, Watts E, Bull CA, Morris R, Acheson A, Banerjea A (2016) Colorectal cancer outcomes in patients aged over 85 years. Ann R Coll Surg Engl 98:216–221
Welch CS (1948) Surgery in the aged. NEJM 238:821–832
Mendes Da Costa P, Allegaert W (1983) Chirurgie de l’ octogenaire, résultats d’une enquête nationale. Acta Chir Belg 83(suppl):1–100
Gainant A, Sautereau D, Minani M, Cubertafond P (1992) Digestive surgery in patients over 80 years of age. Apropos 690 Oper Ann Chir 46(10):923–7
Damhuis R, Meurs C (2005) Meijer W Postoperative mortality after cancer surgery in octogenarians and nonagenarians: results from a series of 5390 patients. World J Surg Oncol 3:71. https://doi.org/10.1186/1477-7819-3-71
Pirrera B, Vaccari S, Cuicchi D, Lecce F, De Raffele E, Dalla Via B, Di Laudo M, Tonini V, Cervellera M (2016) Cola B Impact of octogenarians on surgical outcome in colorectal cancer. Int J Surg 35:28–33
Lichtman SM (2003) Guidelines for the treatment of elderly cancer patients. Cancer Control 10(6):445–453
Richardson JD, Cocanour C, Kern J et al (2004) Perioperative risk assessment in elderly and high-risk patients. J Am Coll Surg 199(1):133–146
Zerbib Ph, Kulick J, Lebuffe G et al (2005) Emergency major abdominal surgery in patients over 85. World J Surg 29:820–825
Audisio R, Ramesh H, Longo W, Zbar A, Pope D (2005) Preoperative assessment of surgical risk in oncogeriatric patients. Oncologist 10:262–268
Weerink L, Gant C, van Leeuwen B, de Bock G, Kouwenhoven E (2018) Faneyte I Long-term survival in octogenarians after surgical treatment for colorectal cancer: prevention of postoperative complications is key. Ann Surg Oncol 25(13):3874–3882
Bhangu A, Kiran RP, Audisio R, Tekkis P (2014) Survival outcome of operated and non-operated elderly patients with rectal cancer: a surveillance, epidemiology, and end results analysis. Eur J Surg Oncol 40(11):1510–1516. https://doi.org/10.1016/j.ejso.2014.02.239
Montroni I, Rostoft S, Spinelli A, Van Leeuwen BL et al (2020) GOSAFE—Geriatric Oncology Surgical Assessment and Functional recovery after Surgery early analysis on 977 patients. J Geriatric Oncol 11:244–255
Montroni I, Ugolini G, Saur N, Rosoft S et al (2023) Predicting functional recovery and Quality of Life in older patients undergoing colorectal cancer surgery: real-world data from the international GOSAFE study. J Clin Oncol. https://doi.org/10.1200/JCO.22.02195
Zerey M, Paton B, Kahn P et al (2007) Colonoscopy in the very elderly: a review of 157 cases. Surg Endosc 21:1806–1809
Dworsky JQ (2019) Russell MM Surgical decision making for older adults. JAMA 321(7):716. https://doi.org/10.1001/jama.2019.0283
Blansfield J, Clark S, Hofmann M, Morris J (2004) Alimentary tract surgery in the nonagenarian: elective vs. emergent operations. J Gastrointest Surg 8:539–542
Author information
Authors and Affiliations
Contributions
P.W wrote the main manuscript text and prepared the figures
P.W. and S.P. did the statistical analysis
P.W., S.D and S.H. did perform/ were involved in the surgical procedures
P.W., FvF and S.P. were involved in the follow-up of the patients
All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was presented as a poster at ESSO 41, Bordeaux, France 19–22 0ctober 2022.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Willemsen, P., Devriendt, S., Heyman, S. et al. Colorectal cancer surgery in octogenarians: real-world long-term results. Langenbecks Arch Surg 409, 13 (2024). https://doi.org/10.1007/s00423-023-03201-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03201-y