Abstract
Purpose
The current study was designed to identify prognostic factors for long-term survival in patients with advanced colorectal cancer in a consecutive cohort.
Methods
A total of 123 patients were operated because of T4 colorectal cancer between 1 January 2002 and 31 December 2008 in the Clinic of Surgery, UK-SH Campus Luebeck.
Results
A total of 78 patients underwent a multivisceral resection. The postoperative morbidity was elevated in the patient group with multivisceral resections (34.6% vs. 26.7%). Nevertheless, we detected no significant differences concerning 30 days mortality (7.7% vs. 8.9%; p = 0.815). The main prognostic factor that reached significance in the multivariate analysis was the possibility to obtain a R0 resection (p < 0.0001) resulting in a 5-year survival rate of 55% for patients with curative resection. There were no statistically significant differences in 5-year survival between multivisceral and non-multivisceral resections (p = 0.608). Also we were not able to detect any significant differences for cancer of colonic or rectal origin (p = 0.839), for laparoscopic vs. open procedures (p = 0.610), and for emergency vs. planned operations (p = 0.674). Moreover, the existence of lymph node metastases was not a predictive factor concerning survival as there was no difference between patients with and without lymph node metastases (p = 0.658).
Conclusions
Multivisceral resections are associated with the same 5-year survival as standard resections. Therefore, the aim to perform a R0 resection should always be the main goal in surgery for colorectal cancer. In planned operations, a laparoscopic approach is justified in selected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because of its high prevalence and incidence, colorectal cancer is the second most cancer associated cause of death in Europe [1]. About 10% of all colorectal cancers are adhesive to neighboring organs or are even invading them [2]. The indication to perform a multivisceral resection (MVR) is often made during the operation due to the lack of preoperative exact data. Moreover, multivisceral resections are associated with a high perioperative mortality and morbidity [2–6]. Therefore, these resections are challenging even for an experienced colorectal surgeon.
The en bloc resection of the tumor is of pivotal importance and was shown to be associated with a highly significant improvement in 5-year survival [7]. The impact of the existence of lymph node metastases [5, 8, 9] and emergency surgery [5, 10] was discussed controversially in earlier publications and was described to be associated with an adverse outcome.
Preceding publications focusing on the comparison of multivisceral and non-multivisceral resections in colorectal cancer often had a high proportion of T3 and even T2 carcinomas in the patient cohort analyzed. Furthermore, most publications had a high percentage of cancers of colonic origin together with only few rectal cancers. The 5-year survival rates for T2 and T3 patients were significantly better than those of patients with a T4 carcinoma [4, 5], and rectal cancer was described to be associated with a significantly worse prognosis compared to cancer of colonic origin in some of these publications. In addition, the 5-year survival rates for T4 patients were between 42% and 89.5% [2, 5]. This wide range in patient survival might be attributable to the fact that the patient collectives analyzed were very heterogeneous. Potential differences detected were in part related to a selection bias of the patients by only analyzing short-term outcome of multivisceral resected patients omitting a comparison with the standard non-multivisceral resections.
We therefore did a retrospective analysis of all patients with T4 colorectal cancer operated between 2002 and 2008. The type of operation, multivisceral vs. non-multivisceral and laparoscopic vs. open resection, was analyzed for potential differences concerning the most important factor for the individual patient: long-term survival.
Patients and methods
Methods
Pathologic results and follow-up data of all patients treated because of a colorectal carcinoma at the Surgical Clinic of the University Clinic of Luebeck were entered in a prospective database after obtaining informed consent. Most patients had a preoperative chest X-ray and an ultrasound of the abdomen. In elective patients, a colonoscopy was done. Almost all patients except some emergency cases had a preoperative CT scan of the abdomen. The tumors were operated following a standardized approach with no touch technique of the tumor and high ligation of the corresponding lymph vascular bundle. Moreover, if infiltration into adjacent organs was possible, mobilization or sharp dissection was objectionable, and a primary multivisceral resection was performed. No carcinoma with a suspected infiltration pre- or intraoperative was treated by a standard resection. Standard resections were limited to carcinomas without adhesions or infiltrations into neighboring organs.
The 6th edition of the Union for International Cancer Control (UICC) classification from 2002 was used to categorize colorectal carcinomas. Colorectal cancer stage T4, N0 is classified as stage IIb in this classification; therefore, this apparently quite “low” staging also includes T4 carcinomas. Rectal cancer was defined as carcinomas with a distal margin of 15 cm from the anal verge measured with a rigid endoscope. In rectal cancer, a neoadjuvant radiochemotherapy was recommended in stage II carcinomas. Not all patients received a neoadjuvant therapy due to palliative or emergency operations. Some patients also refused from the neoadjuvant radiochemotherapy due to personal concerns. Chemotherapy was recommended to patients with colon cancer beginning with stage III. Starting initially in 1981, a standardized follow-up was implemented, and all patients were included in the prospective database in our clinic. When patients needed additional treatment in the Surgical Clinic, these data were also included in the database.
The data were evaluated using descriptive statistical techniques. Patients with MVR were analyzed compared to patients without multivisceral resections (nMVR). Differences and correlations between the groups were compared using the U test and the chi-square test. Comparisons of time to recurrence and survival time were made using the Kaplan–Meier method and the log-rank test. Only data of R0-resected patients were used to calculate the survival curves and potential differences between subgroups. A p value < 0.05 was considered significant. Factors associated independently with survival were identified using the Cox model.
Patients
Between 1 January 2002 and 31 December 2008, a total of 128 patients were operated with a histological proven T4 colorectal carcinoma at the Surgical Clinic of the University Clinic of Schleswig-Holstein Campus Luebeck. One hundred twenty-three patients suffered from a single tumor burden in the colorectum. In the remaining five patients, additional carcinomas of different origins were detected; these five patients were excluded from data review. The 123 patients that were allocated to a T4 stage were analyzed after division into two patient groups:
One patient group underwent MVR and one patient group nMVR. Multivisceral resections were defined as the resection of at least one adjacent organ or structure together with the primary carcinoma. In the nMVR group, the pathologic examination showed a penetration of the serosa without invasion into neighboring organs. According to current guidelines, these patients were treated without multivisceral resection.
Results
The patients were assigned to two treatment groups: patients that had MVR performed and patients without nMVR. The exact allocation to the different stages is presented in Table 1. One patient had synchronous cancer of the colon and the rectum. Two patients had synchronous tumors in different parts of the colon; two patients had rectal cancer in different localizations of the rectum. Table 2 shows the localizations of the cancer in the patient groups evaluated. There were no statistically significant differences between the groups.
In our patient cohort, 78 (63.4%) patients were operated via a median laparotomy, and 45 (36.6%) patients were operated via a laparoscopic approach. The nMVR cohort comprised 45 patients. The median age was 70.4 years (40–94 years). The male/female ratio was 30:15. A total of 78 patients were allocated to the MVR cohort. The median age of this cohort was 69.0 years (41–92 years) accounting for a non-statistically significant difference between the two cohorts. The male/female ratio was 38:40 in the MVR cohort.
A total of 137 organs were resected together with the primary carcinomas. In most patients, we resected only one organ that was potentially infiltrated by the carcinoma (41 patients, 52.6%). Tumor adherence leading to resection of two adjacent organs was detected in 21 patients (26.9%). In 12 patients, we found an infiltration of three organs (15.4%), and one patient was resected on six different organs and compartments of the body (1.3%). Tumor growth in the lower abdomen led most often to an infiltration of the abdominal or pelvic wall as well as to infiltration of parts of the small bowel. In carcinomas of the sigmoid colon and the cecum, an infiltration of the bladder was also common. In women, the inner genital organs were most often infiltrated by carcinomas; moreover, infiltration of parts of the small intestine was detected often during the pathological examination. Figure 1 shows the organs that were resected in relation to the patients’ sex.
Of the 78 multivisceral resections performed, 52 were done because of cancer of colonic origin (66.7%); the remaining 26 carcinomas (33.3%) were localized in the rectum. Table 3 shows the distribution of the cancers in relationship to the distance from the anal verge.
The 123 operative interventions were analyzed for the method of resection. The majority of resections were accomplished as resections with primary anastomosis. No significant differences could be detected between the two patient cohorts.
The majority of the operative interventions when performing a multivisceral resection under curative intention were done via a median laparotomy. A total of 17.9% of the curative resections were done via a laparoscopic approach (details see Table 4). Neither in the overall patient group (p = 0.435) nor in the patients with treatment under curative intentions (p = 0.610) we detected a statistically significant difference between the two groups concerning open vs. laparoscopic access.
In 96 of 123 patients (78%), planned operative interventions were done. The remaining 27 patients (22%) presented as emergency cases. There were no statistically significant differences between the groups concerning planned vs. emergency operations (p = 0.674). Emergency operations were all done via a median laparotomy.
Neoadjuvant therapy MVR vs. nMVR
Neoadjuvant therapy was limited to patients with rectal cancer treated with curative intention. Of the total 123 patients, only 13 received a neoadjuvant therapy. Four patients were in the nMVR cohort, and nine patients were allocated to the MVR cohort. The therapies administered were very heterogeneous so a statistical analysis has not been done.
Morbidity and mortality
Postoperative complications were observed in 39 patients; these were 31.7% of the total patient population. The overall complication rate for the MVR cohort was 34.6% (27 of 67 patients) while it was 26.7% (12 of 45 patients) for the nMVR cohort. The most common complications were impairments in the local healing of the wounds of the operative access or drainage sites (11 patients, 8.9%). There were no statistically significant differences between the two groups. An anastomotic leakage was detected in 8 of 85 patients (9.4%). Four patients were associated to each of the two groups which accounts for no statistical significance (p = 0.599). Major hemorrhage was detected in a total of five patients (4.1%). Three patients (3.8%) were from the MVR group while two patients were from the nMVR group (p = 0.468); 21 patients (7.1%) underwent a redo operation. Of these 21 patients, 15 (71.4%) were from the MVR and six (28.6%) from the nMVR cohort. Figure 2 shows the complications in the two groups.
Due to the small number of the individual complications, a statistical evaluation is not justified. Nevertheless, the tables show a strong tendency toward less complications in the nMVR group.
Corresponding to the higher rate of complications, the median length of hospital stay was much longer in the MVR group with 21.7 days (12–124 days). The median length of stay was 15.2 days (11–59) in the nMVR group.
Mortality
The 30-day mortality of the overall patient cohort was 8.1%. Four of 45 patients from the nMVR group (8.9%) and six of 78 patients from the MVR group (7.7%) died. There was no statistically significant difference between the two treatment groups (p = 0.815). In patients operated under curative intentions (55 of 123), the overall mortality was lower with a total of 5.5%. Again there was no statistically significant difference between the two patient groups. Two patients died from the nMVR, and one patient was from the MVR cohort.
Follow-up
After discharge from the hospital, 71 patients were treated in multimodal therapy concepts. A total of 45 patients were from the MVR group; the remaining 26 patients were from the nMVR group. Among the therapies administered were adjuvant chemotherapy protocols in 65 of 71 patients, 16 patients underwent a radiation therapy, and two patients received an immunotherapy. There were no significant differences between the groups. The therapies administered were very heterogeneous; we therefore did no statistical evaluation of this variable.
Disease relapse MVR vs. nMVR patients
The possible infiltration into neighboring organs does not per se exclude an operation with curative intention. Among the 123 T4 carcinomas, a total of 55 were operated under curative intentions. Thirty-three of the patients were allocated to the MVR group. A palliative indication for the conduction of the operation was apparent in more than half of the patients. There was no statistically significant difference between the MVR and nMVR patients.
We were able to achieve a local R0 situation in 101 of 123 patients with T4 colorectal cancer. Of the R0 resected MVR patients, we detected a true tumorous invasion into adjacent organs or structures in 63% of the patients. In the remaining patients, only inflammatory adhesions were detected. Sixteen patients had a R1 resection while 1.6% had a R2 situation after resection. No statistically significant differences were detected. In the patients resected under curative intentions, the proportion of R0 resections was much higher with 93.9% in the MVR and 95.5% in the nMVR group.
The patients were followed up on a regular basis by a specialized unit of our clinic (E.O., C.K.). The progression rates discussed hereafter only refer to the patients operated under curative intentions after excluding the patients deceased in the early postoperative course (52 patients to be analyzed). There was no statistically significant difference between the two groups as 5 of 20 patients in the nMVR and 8 of 24 patients in the MVR group suffered from disease progression. If possible, a local recurrence or distant metastases were resected.
Table 5 shows the relapse rates in relation to the UICC staging of the disease. No statistically significant differences between the tumor stages were detected. Progressive disease was divided into distant metastasation and local recurrences. The results presented in Table 6 clearly show the very low local recurrence rate of 1.9% in the patients operated under curative intentions although a tumor stage T4 was the cause of the initial operation.
Overall survival
The patients operated under curative intentions had a much better prognosis concerning long-term survival. The Kaplan–Meier curves were only calculated for these patients. The 5-year survival rate for the curatively operated patients with colorectal cancer was 55%. A total of 33 patients were operated because of cancer of colonic origin; 18 patients suffered from rectal cancer. There were no differences in overall survival in the curatively operated patients (p = 0.495). Moreover, we also detected no statistically significant differences analyzing our results for the MVR and nMVR patients with colon and rectal cancer (log-rank: p = 0.839). Therefore, the patients are analyzed as the whole cohort of curatively operated patients concerning multivisceral vs. non-multivisceral resections.
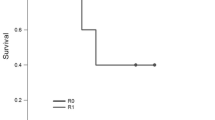
The 5-year survival for the 52 patients treated curatively was 55%. In contrast, the cumulative 5-year survival of the 61 patients treated with palliative intentions was 6%. This accounts for a highly significant statistical difference (p < 0.0001) (see Fig. 3 and Table 7).
Taking the difference in postoperative complications between the two groups into consideration described above, we detected no statistical significant differences between the MVR and nMVR groups concerning 5-year survival (54% vs. 57%, p = 0.608). Comparing the 3- and 5-year survival rates of the two groups interestingly, the 3-year survival rate is much better with 70% in the MVR group compared to 57% in the nMVR group (see Fig. 4 and Table 7).
The quality and the adequate radicalness of the operation are influenced in a profound manner by the extent and the completeness of a regional adenectomy. We detected no significant differences concerning the incidence of lymph node metastases in the nMVR vs. the MVR group. The median number of lymph nodes resected during colonic operative procedures was 17.76 ± 6.04. A median of 5.76 ± 6.37 lymph nodes was infiltrated by carcinoma cells. In rectal cancers, we resected a mean of 17.2 ± 6.02 lymph nodes. Of these resected specimens, a mean of 5.6 ± 5.93 was infiltrated by metastases. The likelihood of lymph node metastases and the mean number of lymph node metastases were independent from the treatment group (p = 0.613); besides, we were not able to detect any statistically significant differences between the open and the laparoscopic approach (p = 0.547).
In the overall collective, 44 of 123 patients (45.8%) were classified as N0 according to the tumor–node–metastasis staging. This accounts for 63.4% of all patients with lymph node metastases at the time of operation.
A potential influence on the long-term survival could be attributed to the existence of lymph node metastases. Our patient cohort comprised 34 patients with lymph node but without any distant metastases. Twenty-eight patients had neither lymph node nor distant metastasation. Figure 5 and Table 7 show the survival rates of these patients resected under curative intentions (n = 49). We were not able to detect any statistically significant differences between these subgroups (p = 0.658). After 5 years, the patients with N0 status have a strong tendency toward improved long-time survival.
As mentioned above, we also calculated for potential differences between elective and emergency operations. We were not able to show any significant differences (p = 0.674) between the two subgroups as shown in Fig. 6 and Table 7.
Discussion
The focus of our analysis of the data of the Luebeck registry for patients treated because of a colorectal carcinoma was on possible differences between patients stage T4 that underwent multivisceral or non-multivisceral resections. The complete resection of the carcinoma is of pivotal importance for the long-term outcome of the patient. During the resection procedure, it is mandatory to resect the carcinoma without dissecting it or leaving carcinoma remnants behind. The results of different meta-analysis and single-center studies published all together demonstrated a significantly reduced overall survival for patients in whom a transection of the tumor from adhesive structures was attempted [2, 3, 11, 12].
A strong argument against the performance of multivisceral resections is the severely elevated morbidity compared to standard surgical resections. Preceding studies demonstrated morbidity rates between 11% and 49% [2, 3, 5, 6, 13]. This elevated proportion of complications in the MVR group was confirmed by the results of the current study with a morbidity rate of 34.6% compared to 26.4% in the nMVR group. Nevertheless, we were able to show that the patients treated with multivisceral resections have the same 5-year survival compared with the patients with non-multivisceral resections. From our point of view, this important detection might be explainable by specific circumstances in our clinic.
First we perform a mandatory en bloc resection of the tumor without dissecting them from surrounding tissue. This is also true for the abandonment of intraoperative instantaneous sections for the detection of possible organ invasions. This approach led to a very high proportion of R0 resections of 93.9% and 95.5% in the two groups. Afore this background, our operative approach seems to be justified although a real tumorigenic invasion was shown in the histopathology examination in only 63% of all patients.
Secondly, our patients were all treated on a specialized surgical intensive care ward in the early postoperative course. Earlier publications described differences in long-term survival to be associated with a high early postoperative mortality [3]. In our cohort, the patients had no significant differences concerning 30-day mortality. Hence, an experienced intensive care unit should not be underestimated concerning perioperative patient management and is mandatory for such operations together with highly experienced surgeons. The perioperative mortality in the multivisceral resected patients under curative intention (5.5%) is absolutely comparable to preceding publications [2–6]. A direct comparison to the other studies is difficult because of the inclusion of emergency patients into our analysis and the high proportion of rectal cancer. This might also be an explanation for the relatively high mortality in the overall cohort because of the inclusion of palliative and emergency resections in the analysis. The value of a specialized surgical intensive care unit is also supported by the lack of a survival difference in patients undergoing emergency operations that were associated with reduced 5-year survival in earlier publications.
All emergency procedures were performed as open surgery. We detected no significant differences for multivisceral and standard resections. These results are somewhat contrary to the results of preceding trials as they described emergency procedures to be associated with a higher perioperative morbidity and mortality [14–17]. Some studies even excluded emergency patients from the statistical analysis [4]. An indirect sign concerning emergency procedures might also be attributed to the demonstrated highly significant correlation between intraoperative blood loss and survival [3]. The group described this influencing variable to be unrecognized before but did not provide data concerning the proportion of emergency surgery [3]. A multivisceral resection is therefore from our point of view always justified in the setting of optimal intra- and postoperative patient care.
A remarkable result of our study is the absolutely comparable long-term mortality in the two treatment groups. Long-term survival thus seems to be independent from the extent of surgical interventions in patients with colorectal cancer in experienced centers. The results are even more interesting as our patient cohort comprised a high percentage of patients with rectal cancer.
Other study groups described rectal cancer to be associated with an adverse outcome for the patients [18]. These observations are not supported by our data as there were no survival differences between patients with cancers of colonic or rectal origin. When carefully reviewing the respective results of the published studies, it seemed apparent that the negative prognostic implications of rectal cancer seemed to be associated with a significantly higher likelihood of the development of local recurrence postoperatively and a higher perioperative mortality [3, 18]. Our results of only 1.9% local recurrences in the curatively operated patients were independent from the primary localization of the cancer.
Croner et al. described patients with N2 metastases to be associated with a higher probability of the development of local recurrences [5]. Our data do not support these results. After radical surgical resection and the implementation of a close patient monitoring in short intervals together with adjuvant (radio-) chemotherapy protocols, the 5-year survival of the patients after curative resection is independent from the prevalence of lymph node metastases.
We detected late lymph node metastases as a cause of disease recurrence in 5.8% of all patients. As a result, adjuvant (radio-) chemotherapy in N+ patients seems to be without alternative if the patient is able to endure the additional stress from the adjuvant therapy.
Our 5-year survival rate of 55% is comparable to the published data [2–6]. Limitations in the comparison with other studies are constituted by the relatively high proportion of patients with rectal cancer in our study cohort. These patients are often underrepresented in other studies. Besides, we only analyzed the data of T4 patients which per se have a worse prognosis compared to T3 patients that constitute a large part of the patients of other studies.
Laparoscopic procedures are established therapeutic approaches for the treatment of cancer of colorectal origin. The oncological results of the procedures are comparable to the open operations as demonstrated in several meta-analyses [19]. In our surgical clinic, the laparoscopic resection of cancer of colorectal origin is the operative standard. We therefore did also planned laparoscopic resections in patients with a T4 carcinoma of the colorectum.
Preceding publications and discussions on national and international summits often questioned the adequate oncologic radicalism of such an approach and state, for example, a putative inadequate lymph node yield by the laparoscopic procedures although several publications clearly illustrated the point of a non-inferiority and absolute comparability of this operative approach even in patients with T4 colorectal cancer [19–21].
The results presented afore clearly argue against these concerns as there were no differences in long-term survival, numbers of lymph nodes harvested, and the risk of a local recurrence of the tumor. We even detected a tendency toward higher long-term survival in laparoscopic procedures. This apparent effect is induced by a survival of 100% after 4 years in the six multivisceral resected patients. A bias because of the small number of patients or even a selection bias choosing “better” patients for the laparoscopic approach might be subject to discussion.
Thus, we consider the planned laparoscopic resection of T4 colorectal carcinomas as feasible (Fig. 7; Table 7). Our results are supported by studies recently published [19–21]. The working groups also detected no differences concerning long-term survival, local recurrence, and the proportion of R0 resections. What is different in our patient cohort from the published data is the relatively high rate of conversion of about 18% in the preceding studies. All patients that were operated via a primary laparoscopic approach had their operation completed without converting to a laparotomy.
Conclusion
Multivisceral resections offer the possibility to obtain a R0 situation in patients with advanced colorectal cancer. A postoperative R0 status is the only prognostic factor that reached significance in our study. These resections should be performed by experienced colorectal surgeons afore the background of a specialized intensive care unit. Our preliminary data provided evidence for the possibility and comparability of laparoscopic multivisceral colorectal resections.
References
Brenner H, Bouvier AM, Foschi R, Hackl M, Larsen IK, Lemmens V, Mangone L, Francisci S (2011) Progress in colorectal cancer survival in Europe, from the late 1980s to the early 21st century: The EUROCARE study. Int J Cancer. doi:10.1002/ijc.26192
Gebhardt C, Meyer W, Ruckriegel S, Meier U (1999) Multivisceral resection of advanced colorectal carcinoma. Langenbeck’s Arch Surg 384:194–199
Lehnert T, Methner M, Pollok A, Schaible A, Hinz U, Herfarth C (2002) Multivisceral resection for locally advanced primary colon and rectal cancer. An analysis of prognostic factors in 201 patients. Ann Surg 235:217–225
Nakafusa Y, Tanaka T, Tanaka M, Kitajima Y, Sato S, Miyazaki K (2004) Comparison of multivisceral resection and standard operation for locally advanced colorectal cancer: analysis of prognostic factors for short-term and long-term outcome. Dis Colon Rectum 47:2055–2063
Croner RS, Merkel S, Papadopoulos T, Schellerer V, Hohenberger W, Goehl J (2009) Multivisceral resection for colon carcinoma. Dis Colon Rectum 52(8):1381–1386
Eisenberg SB, Kraybill WG, Lopez MJ (1990) Long-term results of surgical resection of locally advanced colorectal cancer. Surgery 108:779–786
Hermanek P (1999) Prognostic factor research in oncology. J Clin Epidemiol 52:371–374
Radespiel-Troeger M, Hohenberger W, Reingruber B (2004) Improved prediction of recurrence after curative resection of colon carcinoma using tree-based risk stratification. Cancer 100:958–967
Tsai HL, Lu CY, Hsieh JS, Wu DC, Jan CM, Chai CY, Chu KS, Chan HM, Wang JY (2007) The prognostic significance of total lymph node harvest in patients with T2-4N0M0 colorectal cancer. J Gastrointest Surg 11(5):660–665
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis 11(7):733–739
Hunter JA, Ryan JA, Schultz P (1987) En bloc resection of colon cancer adherent to other organs. Am J Surg 145:67–71
Gall FP, Tonak J, Altendorf A (1987) Multivisceral resections in colorectal cancer. Dis Colon Rectum 30:337–341
Kruschewski M, Pohlen U, Hotz HG, Ritz JP, Kroesen AJ, Buhr HJ (2006) Results of multivisceral resection of primary colorectal cancer. Zentralbl Chir 131:217–222
Bokey EL, Chapuis PH, Fung C (1995) Postoperative morbidity and mortality following resection of the colon and rectum for cancer. Dis Colon Rectum 38:480–487
Anderson JH, Hole D, McArdle CS (1992) Elective versus emergency surgery for patients with colorectal cancer. Br J Surg 89:1557–1562
Merkel S, Meyer C, Papadopoulos T, Meyer T, Hohenberger W (2007) Urgent surgery in colon carcinoma. Zentralbl Chir 132:16–25
Andreoni B, Chiappa A, Bertani E, Bellomi M, Orecchia R, Zampino M, Fazio N, Venturino M, Orsi F, Sonzogni A, Pace U, Monfardini L (2007) Surgical outcomes for colon and rectal cancer over a decade: results from a consecutive monocentric experience in 902 unselected patients. World J Surg Oncol 5:73
Darakhshan A, Lin BPFC, Chan C, Chapuis PH, Dent OF, Bokey L (2008) Correlates and outcomes of tumor adherence in resected colonic and rectal cancers. Ann Surg 247:650–658
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev 2:CD003432
Bretagnol F, Dedieu A, Zappa M, Guedj N, Ferron M, Panis Y (2011) T4 colorectal cancer: is laparoscopic resection contraindicated? Colorectal Dis 13(2):138–143
Hemandas AK, Abdelrahman T, Flashman KG, Skull AJ, Senapati A, O’Leary DP, Parvaiz A (2010) Laparoscopic colorectal surgery produces better outcomes for high risk cancer patients compared to open surgery. Ann Surg Jul 252(1):84–89
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoffmann, M., Phillips, C., Oevermann, E. et al. Multivisceral and standard resections in colorectal cancer. Langenbecks Arch Surg 397, 75–84 (2012). https://doi.org/10.1007/s00423-011-0854-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0854-z