Abstract
Background
Internal rectal prolapse and rectocele are frequent clinical findings in patients with obstructed defecation syndrome (ODS). However, there is still no evidence whether stapled transanal rectal resection (STARR) provides a safe and effective surgical option. Therefore, the German STARR registry was initiated to assess safety, effectiveness, and quality of life.
Methods
The German STARR registry was designed as an interventional, prospective, multicenter audit. Primary outcomes include safety (morbidity and adverse events), effectiveness (ODS, symptom severity, and incontinence scores), and quality of life (PAC-QoL and EQ-5D) documented at baseline and at 6 and 12 months. Statistical evaluation was performed by an independent research organization of clinical epidemiology.
Results
Complete data of 379 patients (78% females, mean age 57.8 years) were entered into the registry database. Mean operative time was 40 min, mean hospitalization was 5.5 days. A total of 103 complications and adverse events were reported in 80 patients (21.1%) including staple line complications (minor bleeding, infection, or partial dehiscence; 7.1%), major bleeding (2.9%), and postsurgical stenosis (2.1%). Comparisons of ODS and symptom severity scores (SSS) demonstrated a significant reduction in ODS score between baseline (mean 11.14) and 6 months (mean 6.43), which was maintained at 12 months (mean 6.45), and SSS at preoperative and at 6- and 12-month follow-up (13.02 vs. 7.34 vs. 6.59; paired t test, p < 0.001). Significant reduction in ODS symptoms was matched by an improvement in quality of life as judged by symptom-specific PAC-QoL and generic ED-5Q (utility and visual analog scale) scores and was not associated with an impairment of incontinence score following STARR (p > 0.05). However, 11 patients (2.9%) showed de novo incontinence, and new-onset symptoms of fecal urgency were observed in 25.3% of patients.
Conclusion
These data indicate that STARR is a safe and effective procedure. However, conclusions are limited due to the selection and reporting bias of a registry. The problem of fecal urgency needs cautious reassessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Internal rectal prolapse (intussusception) and rectocele are frequent morphological findings in patients suffering from obstructed defecation syndrome (ODS). Derived from stapled hemorrhoidopexy introduced by Antonio Longo, the stapled transanal rectal resection (STARR) procedure using two PPH01® circular stapler devices (Ethicon Endo-Surgery, Norderstedt, Germany) has been advocated as a surgical option for ODS. In the meantime, safety and promising functional results of the STARR procedure related to symptom resolution for ODS caused by internal rectal prolapse have been reported [1–3]. In contrast, some case series on major complications and unsatisfactory functional results following STARR have caused a general controversy whether the STARR procedure is an appropriate surgical option to resolve constipation symptoms related to internal rectal prolapse [4, 5]. Referring to these conflicting results, there is still no evidence whether the STARR procedure provides a safe and effective surgical method in ODS patients. Therefore, the German STARR registry was initiated in 2006 to assess safety, effectiveness, and quality of life.
Methods
Structure of the German STARR registry
The German STARR registry was an interventional (open label, nonrandomized), prospective, multicenter audit. Study design and structure have been published previously [6]. Simultaneously, databases were set up in Germany, the UK, and Italy, each under the auspices of their respective national coloproctological societies. The respective registries were designed with a web-based interface (“electronic case report form” [eCRF]) to facilitate data entry by online access and to allow pooling of data into the European STARR registry [7]. The German STARR registry was run under the auspices of the “Deutsche Gesellschaft für Koloproktologie.” Data were collected preoperatively and at 6 weeks and at 6 and 12 months postoperatively (Table 1). The online registry was managed by an independent clinical trial and statistical support agency, Medalliance, with offices in Paris and Brussels. The Medalliance eCRF system had been specifically developed for European clinical studies (including phase I–IV studies), and the “STARR-DE” database was on a server in Brussels. The Medalliance server was monitored by a data manager, and completeness of data were monitored by the study coordinators on a country level. All data which were entered into the eCRF were considered for evaluation, and no exclusion of data was possible.
Study design and data collection
Although the registry was formally not a clinical trial, primary and secondary end-points were defined. The primary end-point focused on symptom improvement provided as the change in ODS score at 12 months following surgery. Additional outcomes include safety (morbidity, adverse events, and mortality), effectiveness, and quality of life: in addition to the ODS score (Table 2), data collection included evaluation of symptom severity score (SSS; Table 3), Wexner's incontinence score [8], and quality of life as assessed by the validated symptom-specific PAC-QoL and generic ED-5Q instruments [9, 10]. All preoperative, operative, and postoperative data collection were the responsibility of the individual investigating surgeon. Standardized prospective data evaluation within the German registry was processed either by PC internet documentation (“online eCRF”) or by standardized printout protocols. Completely anonymized data were entered voluntary by the individual investigator. From the formal aspect, the registry functioned as a multicenter data collection audit rather than a structured clinical trial. Therefore, formal ethical approval was not necessary. However, informed consent was obtained from all patients who participated in the registry. Moreover, informed consent for the surgical technique was a prerequisite prior to any surgery. Patient accrual for the German STARR registry started on May 15, 2006. Recruitment phase was 1 year (until May 15, 2007). Follow-up study ended on May 15, 2008. In the meantime, an interim analysis of the German STARR registry solely focusing on preliminary safety data was performed on January 2, 2007 [6]. The official closing of the German online access was December 31, 2008.
Patient selection and surgical technique
Focusing on patient selection, recommendations were made for inclusion and exclusion criteria, based on a previous consensus conference [11]. Inclusion recommendations were that patients should be selected on the basis of recognized symptoms of ODS with evidence of anatomical defects (internal rectal prolapse and/or rectocele) assessed clinically and confirmed by dynamic imaging (defecography or dynamic magnetic resonance imaging) and adequate anal sphincter function as assessed by at least digital rectal examination. Exclusion criteria included patients with a contraindication to general anesthesia, immunocompromised status, physical or psychological problems precluding data collection, inflammatory bowel disease, or septic conditions of the anorectum [12]. Recommendations for patient selection were based on previously published position statements derived from a consensus conference and from a proposed algorithm [11, 12], but the ultimate decision-making was left to individual investigators in accordance with the local policy.
Focusing on surgical technique, only STARR procedures using two PPH01® staplers were included. As described previously [1–3, 6, 7], the patient was positioned in lithotomy position under spinal or general anesthesia, and the perineum prepared and draped. The anal canal was gently dilated and the circular anal dilator (CAD33) was inserted. The extent of the internal prolapse was identified. Two to three semicircumferential purse-string sutures were placed in the anterior rectum at approximately 1.5, 2, and 3 cm above the anorectal junction. The posterior rectal mucosa was protected with a spatula and the first PPH01® stapling device inserted into the anorectum. The three anterior sutures were delivered through the side channels in the stapler and tension was applied to prolapse the redundant anterior rectal wall into the stapler housing. The stapler was closed, taking care to ensure that the posterior vaginal wall had not been incorporated, and was fired. A similar procedure was repeated for the posterior rectal wall with two or three posterior semicircumferential purse-string sutures and a second PPH01® stapler to produce a complete full-thickness circumferential distal rectal resection.
Actual analysis and statistical evaluation
On January 9, 2009, the current data set from the German STARR registry was downloaded by Medalliance for analysis of 12-month follow-up outcomes. Out of 405 patients who were primarily entered into the registry, data sets with complete 12-month follow-up observation in terms of safety were available for 379 patients (94%). To provide objective surgical and functional outcome, analysis was restricted to these 379 patients. Assessment of functional outcomes (ODS, SSS, and incontinence score; PAC-QoL and EQ-5D) was performed comparing baseline (preoperative) with 6- and 12-month follow-up data. In these evaluations, completion rates were indicated separately. The overall ODS score and SSS were calculated by summation of their individual components to give a maximum score of 40 and 36, with a higher score indicating an increased severity of symptoms. Comparison of fecal urgency was derived from the corresponding component which was included in the SSS (item “difficulty to withstand urge to open bowels”; Table 3). For comparative analysis of urgency at baseline and at 6 and 12 months, a cut-off was established at a score of 3 (score 0–2 vs. score 3 or higher). The overall PAC-QoL and EQ-5D scores were derived according to their original derivations with an improvement in quality of life indicated by a decrease in numerical value of the PAC-QoL score but an increase in numerical value of the ED-5Q utility and visual analog scale (VAS) scores. Overall incontinence scores were derived by summation with an overall score of 20, with a higher score indicating worse function. Only complete data were analyzed for assessment of ODS, SSS, incontinence, and quality of life. Analysis of safety data included all patients entered into the registry regardless of the completeness of other data collection. No data were excluded from analysis. Mean values were computed for all outcome measures and are presented with 95% confidence intervals (95% CI). Statistical analysis was performed using paired t tests for continuous variables, Pearson's chi-squared and Fisher's exact test where appropriate (p < 0.05 statistically significant).
Results
Surgical and safety data
Complete data of 379 patients (78% females) were entered into the registry database within May 2006 and May 2007 by 27 centers (STARR procedures per center: minimum 1, maximum 73). Mean age of patients was 57.8 years, mean operative time was 40 min, and mean length of hospitalization was 5.5 days. A total of 103 complications and adverse events were reported in 80 patients, giving an overall morbidity rate of 21.1%. Most common complications were staple line complications including minor bleeding, infection, or partial dehiscence (7.1%), major bleeding requiring surgical revision (2.9%), and postsurgical stenosis requiring interventional dilatation (2.1%). Morbidity and adverse events are outlined in Table 4. Focusing on severe complications, two patients had stoma formation after STARR procedure due to rectal necrosis and major leakage (0.5%). No mortality occurred.
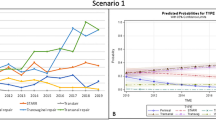
Effectiveness
In terms of ODS, symptom severity, and incontinence scores, the completion rate of follow-up data at 12 months varied according to the investigative score being assessed. Details on completion rate and comparisons of the three scores are summarized in Table 5. As outlined in Fig. 1a, b, comparison of ODS score demonstrated a significant reduction in ODS score between baseline (mean 11.14) and 6 months (mean 6.43), which was maintained at the 12-month (mean 6.45) follow-up (paired t test, p < 0.001). As summarized in Fig. 2, comparison of SSS at preoperative and at 6- and 12-month follow-up also showed a significant reduction between baseline (mean 13.02), at 6 months (mean 7.34), and at 12 months (mean 6.59; paired t test, p < 0.001). Significant improvement in ODS symptoms (overall score and components) was not associated with an impairment of continence with no significant changes in incontinence score (Fig. 3). However, 11 patients (2.9%) had a significant deterioration of their continence status 12 months after STARR. Two patients (0.5%) underwent resection–rectopexy due to symptom persistence of ODS.
Quality of life
Improvement in ODS score and SSS was matched by an overall improvement in quality of life as judged by the symptom-specific PAC-QoL questionnaire (overall score and four component scores assessing physical discomfort, psychosocial discomfort, worries and concerns, and satisfaction) and the generic ED-5Q scores at 6- and 12-month follow-up (Figs. 4a, b and 5a, b). Details on completion rate and comparisons of the scores are summarized in Table 6.
Fecal urgency
Specific assessment of fecal urgency was based on complete data sets in 312 patients (82%). Analyzing these 312 patients (adverse events and SSS), a 25.3% rate of new-onset symptoms of fecal urgency (score 1 or higher) after 12 months (n = 79) was documented. However, detailed analysis of this collective showed that fecal urgency was experienced “most of the time” or “all the time” (score 3 or higher) in a minority of these patients with a new onset of urgency symptoms (n = 17, 21.5%). A symptom resolution of preoperative urgency symptoms was observed in 8.0% of patients (n = 25).
Discussion
Internal rectal prolapse (intussusception) associated with anterior rectocele are common findings in females, and the question whether symptoms of ODS or continence disorders are related to these morphological findings has been debated for decades [13, 14]. Furthermore, the issue whether surgery can resolve symptoms is controversial. If surgery is indicated, a variety of approaches including transabdominal (rectopexy with/without resection, with/without mesh) and transrectal procedures such as Delorme's operation have been proposed [15–20]. Summarizing important studies of experienced centers, it can be highlighted that functional success of both resection–rectopexy [15–18] and Delorme's operation [19, 20] for symptomatic internal rectal prolapse are disappointing and can lead to new-onset symptoms such as urgency or tenesmus. Similarly, the introduction of the STARR procedure has been a focus of controversial discussion. Consequently, the German STARR registry was established in May 2006 to assess safety, effectiveness, and quality of life.
Obviously, there is the question whether the methodology of this registry has an impact on best clinical practice [21, 22]. Of course, there is a dilemma as to the best methodology to use, and this often involves a trade-off between maximizing data collection and ensuring completeness and accuracy of follow-up. In the case of STARR, this choice was determined primarily by the lack of a convincing comparative surgical tool, and a randomized controlled study comparing STARR vs. biofeedback was already initiated [23]. The advantages of the registry approach are that it allows rapid accumulation of large volumes of data at relatively inexpensive costs and a pragmatic design facilitates the capture of “real life” practice compared to the more rigorous and limiting constraints of a randomized study. Conversely, there are some important disadvantages including the dependency on voluntary data submission which led to a selection and reporting bias. It is for this reason that the completeness of follow-up data related to effectiveness and quality of life data varies between 56% (ODS score) and 80% (incontinence score). However, the authors would defend the approach on the basis that the high numbers recruited is likely to dilute any inconsistencies that have crept into the data through incomplete or incorrect reporting.
In addition, one has to admit that both ODS and SSS used in the registry are unvalidated tools for assessing symptoms of ODS. However, they were chosen because of their use in previous studies reporting on the STARR procedure and due to the lack of a validated alternative at the time of set up of the registry in 2006. In the meantime, validated scores specifically assessing ODS are available [24]. At the time of initiation of the registry, the St. Marks incontinence score was available which addresses urgency and which has been shown to correlate well with the severity of incontinence symptoms [25]. However, the Wexner incontinence score had been selected by the steering committee.
One of the reasons to assess the safety of the STARR procedure were case reports or small series of unsatisfactory functional outcome and serious complications which accelerated the controversial discussion on the procedure [4, 5]. In the meantime, recently published studies carefully describing poor functional results, fecal incontinence, and complications such as rectal perforation, pelvic sepsis, or rectovaginal fistula with the need for fecal diversion have a major impact on both indication and distribution of the STARR procedure [26, 27]. In detail, Pesactori and Zbar reported on 20 patients following STARR surgery [27]: They published a high rate of reinterventions either directly related to STARR (e.g., staple removal, fistulectomy) or associated with other significant morphological disorders (e.g., enterocele repair, rectosigmoid resection). Moreover, they demonstrated that many patients with poor functional outcome had coexisting psychological symptoms (depression or anxiety) [27]. However, reflecting the current results on morbidity after 379 STARR procedures, it becomes obvious that the STARR procedure is a safe procedure in the majority of cases. A 21.1% rate of morbidity and/or adverse events seems to be very high on the first view, but most of complications could be managed conservatively. However, two serious complications of rectal necrosis and major leakage requiring fecal diversion (0.5%) were documented within the registry. Speculating on the cause of these serious complications, the first was potentially related to a compromised blood supply of the rectum following laparoscopic resection–rectopexy. This course, in particular, clearly shows that patient selection—not only based on symptoms and clinical findings—has also to focus on proposed contraindications from the surgical or technical view [11, 12]. No mortality occurred.
In general, one has to admit that ODS symptoms are frequently associated with a variety of clinical findings of the pelvic floor and the anorectum [28–34]. Therefore, the question whether an internal rectal prolapse (with or without a rectocele)—clinically and radiologically confirmed—mainly causes symptoms of ODS cannot be answered definitely. In particular, the majority of female patients also show symptoms based on associated pelvic floor pathology (including prolapsing hemorrhoids, paradoxical puborectalis syndrome, anism, among others), and the differential diagnosis of ODS symptoms from irritable bowel syndrome is frequently difficult. Moreover, psychological symptoms can be observed in a high proportion of patients which has a tremendous impact on patient selection. Based on this background and focusing on effectiveness, comparison of both ODS and SSS demonstrated a significant reduction in both scores at 12-month follow-up. Significant improvement in ODS symptoms was not associated with an impairment of continence following STARR with no significant changes in Wexner's incontinence score. Improvement in ODS score and SSS was matched by an overall improvement in quality of life as judged by the symptom-specific PAC-QoL questionnaire and the generic ED-5Q scores at 6- and 12-month follow-up.
Fecal incontinence is always a major concern with any transanal surgical approach, and this is particularly so following STARR. A change in continence after STARR is, however, difficult to assess objectively, as it is frequently a component of the ODS symptom complex prior to any surgical intervention. Thus, 11.2% of patients had a Wexner incontinence score of ≥3 preoperatively. This compared to 8% and 5.1% with a score of ≥3 at 6 and 12 months, respectively. This was mirrored by a significant improvement in patient-reported symptoms of incontinence/soiling which formed one component of the SSS (data not shown). It would, therefore, appear that there is an overall improvement in incontinence symptoms, which is most marked at 12-months follow-up. However, a minority of patients will experience a worsening of incontinence, and this is reflected in the 2.7% incontinence rate reported as a complication of the procedure.
A similar argument holds true for the symptom “inability to withhold defecation” or “fecal urgency.” Again, this is a frequently reported complication of the STARR procedure, but is also a feature of preoperative ODS symptoms. Unfortunately, we did not use the St. Marks incontinence score which includes “urgency” [25]. The only tool available in the registry to analyze fecal urgency was the SSS. One component of this score recorded “difficulty to withstand urge to open bowels” on a four-point scale (0 = none of the time, 1 = a little of the time, 2 = some of the time, 3 = most of the time, 4 = all of the time). On the first view, a 25.3% de novo fecal urgency rate 12 months after STARR is extraordinarily high, but this figure summarizes all patients with score 1 or higher. However, exclusive analysis of this data complex showed that fecal urgency was experienced “most of the time” or “all of the time” (score ≥3) in only 21.1% of these patients. To be honest, urgency rate is a problem, and the issue of post-STARR urgency remains contentious, as we have still to accept that the mechanisms underlying ODS are complex and poorly understood [33]. In addition to the “mechanical” aspects addressed by the STARR procedure, one has also to consider the physiological components; moreover, the majority of females with ODS are multiparous and likely to have coexisting pudendal neuropathy which will affect pelvic floor and anal sphincter function and may manifest as fecal urgency following STARR. Further research on this field is required and, hopefully, subgroup analysis of the European registry may help to elucidate this. Particularly, patients with fecal urgency have to be reassessed carefully.
Conclusion
These data of the German STARR registry indicate that STARR is a safe and effective procedure in the treatment of ODS. However, related to a relatively high percentage of missing data, a general uncertainty of the representative character of the samples, and the use of a nonvalidated ODS score, these conclusions are limited and the results may reflect a selection and reporting bias of a registry.
References
Boccasanta P, Venturi M, Salamina G, Cesana BM, Bernasconi F, Rovario G (2004) New trends in the surgical management of outlet-obstruction: clinical and functional results of two novel transanal stapled techniques from a randomised controlled trial. Int J Colorectal Dis 19:359–369
Schwandner O, Farke S, Bruch HP (2005) Stapled transanal rectal resection (STARR) for obstructed defecation caused by rectocele and rectoanal intussusception. Viszeralchirurgie 40:331–341
Ommer A, Albrecht K, Wenger F, Walz MK (2006) Stapled transanal rectal resection (STARR): a new option in the treatment of obstructive defecation syndrome. Langenbecks Arch Surg 391:32–37
Pescatori M, Dodi G, Salafia C, Zbar AP (2005) Rectovaginal fistula after double-stapled transanal rectotomy (STARR) for obstructed defecation. Int J Colorectal Dis 20:83–85
Dodi G, Pietroletti R, Milito G, Binda G, Pecatori M (2003) Bleeding, incontinence, pain and constipation after STARR transanal double stapling rectotomy for obstructed defecation. Tech Coloproctol 7:148–153
Schwandner O, Fuerst A (2007) German STARR registry. Preliminary results of a prospective, multicenter observational study. Coloproctology 29:13–21
Jayne D, Schwandner O, Stuto A (2009) Stapled transanal rectal resection (STARR) for obstructive defecation syndrome: one-year results of the European STARR registry. Dis Colon Rectum 52:1205–1214
Oliveira J, Pfeiifer J, Wexner SD (1996) Physiological and clinical outcome of anterior sphincteroplasty. Br J Surg 83:502–505
Marquis P, De la Loge C, Dubois D, McDermott A, Chassany O (2005) Develpoment and validation of the patient assessment of constipation quality of life questionnaire. Scand J Gastroenterol 40:540–551
National Institute for Health and Clinical Excellence. Interventional procedure guidance 169: stapled transanal rectal resection for obstructed defaecation. Available at http://www.nice.org.uk
Corman ML, Carriero A, Hager T, Herold A, Jayne DG, Lehur PA, Lomanto D, Longo A, Mellgren A, Nicholls J, Nystrom PO, Senagore AJ, Stuto A, Wexner SD (2006) Consensus conference on the stapled rectal resection resection (STARR) for disordered defaecation. Colorectal Dis 8:98–101
Schwandner O, Stuto A, Jayne D, Lenisa L, Pigot F, Tuech JJ, Scherer R, Nugent K, Corbisier F, Basany EE, Hetzer F (2008) Decision-making algorithm for the STARR procedure in obstructed defecation syndrome: position statement of the group of STARR Pioneers. Surg Innov 15:105–109
Dvorkin LS, Knowles CH, Scott SM, Williams NS, Lunniss PJ (2005) Rectal intussusception: characaterization of symptomatology. Dis Colon Rectum 48:824–831
Zbar AP, Lienemann A, Fritsch H, Beer-Gabel M, Pescatori M (2003) Rectocele: pathogenesis and surgical management. Int J Colorectal Dis 18:369–384
Christiansen J, Zhu BW, Rasmussen OO, Sorensen M (1992) Internal rectal intussusception: results of surgical repair. Dis Colon Rectum 35:1026–1029
Van Tets WF, Kuijpers JHC (1995) Internal rectal intussusception: fact or fancy? Dis Colon Rectum 38:1080–1083
Tsiaoussis J, Chrysos E, Athanasakis E, Pechlivanides G, Tzortzinis A, Zoras O, Xynos E (2005) Rectoanal intussusception: presentation of the disorder and late results of resection rectopexy. Dis Colon Rectum 48:838–844
Von Papen M, Ashari LHS, Lumley JW, Stevenson ARL, Stitz RW (2006) Functional results of laparoscopic resection rectopexy for symptomatic rectal intussusception. Dis Colon Rectum 50:50–55
Sielezneff I, Malouf A, Cesari J, Brunet C, Sarles JC, Sastre B (1999) Selection criteria for internal rectal prolapse repair by Delorme's transrectal excision. Dis Colon Rectum 42:367–373
Abbas SM, Bissett IP, Neill ME, Macmillan AK, Milne D, Parry BR (2005) Long-term results of the anterior Delorme's operation in the management of symptomatic rectocele. Dis Colon Rectum 48:317–322
Benson K, Hartz AJ (2000) A comparison of observational studies and randomized, controlled trials. N Engl J Med 342:1878–1886
Jayne DG, Finan PJ (2005) Stapled transanal rectal resection for obstructed defaecation and evidence-based practice. Br J Surg 92:793–794
Lehur PA, Stuto A, Fantoli M, Villani RD, Queralto M, Lazorthes F, Hershman M, Carriero A, Pigot F, Meurette G, Narisetty P, Villet R, ODS II Study Group (2008) Outcomes of stapled transanal rectal resection vs. biofeedback for the treatment of outlet obstruction associated with rectal intussusception and rectocele: a multicenter, randomized, controlled trial. Dis Colon Rectum 51:1611–1618
Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V (2008) Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis 10:84–88
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Pescatori M, Gagliardi G (2008) Postoperative complications after procedure for prolapsed hemorrhoids (PPH) and stapled transanal rectal resection (STARR) procedures. Tech Coloproctol 12:7–19
Pesactori M, Zbar AP (2009) Reinterventions after complicated or failed STARR procedure. Int J Colorectal Dis 24:87–95
Bruch HP, Fischer F, Schiedeck THK, Schwandner O (2004) Obstructed defecation. Chirurg 75:861–870
Schwandner O, Fürst A (2008) Actual role of stapled transanal rectal resection (STARR) for obstructed defecation syndrome. Zentbl Chir 133:116–122
Schwandner O, Bruch HP (2006) Significance of obstructed defecation in hemorrhoidal disease: results of a prospective study. Coloproctology 28:13–20
Boccasanta P, Venturi M, Rovario G (2007) Stapled transanal rectal resection versus stapled anopexy in the cure of hemorrhoids associated with rectal prolapse. A randomized controlled trial. Int J Colorectal Dis 22:245–251
Sperber AD, Shvartzman P, Friger M, Fich A (2007) A comparative reappraisal of the Rome II and Rome III diagnostic criteria: are we getting closer to the “true” prevalence of irritable bowel syndrome? Eur J Gastroenterol Hepatol 19:441–447
Pescatori M, Spyrou M, Pulvirenti d'Ùrso A (2007) A prospective evaluation of occult disorders in obstructed defecation using the “iceberg diagram”. Colorectal Dis 9:452–456
Renzi C, Pescatori M (2000) Psychologic aspects in proctalgia. Dis Colon Rectum 43:535–539
Acknowledgement
The authors thank all participating surgeons who enrolled patients' data to the registry; Mrs. M. Bauer, coordinating study nurse, Regensburg; Dr. F. Daoud, Medalliance, for statistical evaluation and data management; and Dr. G. Ribaric, Ethicon Endo-Surgery Europe, for organization and support.
Conflict of interest (financial disclosure)
The prospective registry was run under the auspices of the “Deutsche Gesellschaft für Koloproktologie.” The German STARR registry was supported by a grant of Ethicon Endo-Surgery Europe. Ethicon Endo-Surgery Europe provided financial support to finance a study nurse (administrative work). There was no pressure or influence of Ethicon Endo-Surgery Europe on the scientific outcome of the registry.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix German STARR registry study group
Appendix German STARR registry study group
Participating centers and collaborating surgeons are (in row of the number of patients included):
Waldkrankenhaus “Rudolf Elle,” Eisenberg (Dr. M. Fiedler, Dr. M. Hopp, Dr. G. Konrad);
Krankenhaus Dresden-Friedrichstadt, Dresden (Dr. S. Stelzner, Fr. Dr. K. Köhler, Dr. G. Hellmich);
Krankenhaus St. Hedwig, Berlin (Dr. J. Schmalfeldt, Dr. E. Lorenz);
Klinikum Mittleres Erzgebirge, Zschopau (Dr. H.-U. Dorn);
Oder-Spree-Krankenhaus, Beeskow (Dr. M. El-Din);
St. Barbara-Klinik, Hamm-Heesen (Dr. L. Sangueza, PD Dr. M. Krämer);
Westpfalz-Klinikum, Kirchheimbolanden (Dr. J. Heist);
Städtisches Klinikum Fulda (Dr. C. Bismarck, PD Dr. J. Hellinger);
Krankenhaus Waldfriede, Berlin (Dr. Th. Unglaube, Dr. R. Scherer);
Klinikum Ludwigsburg, Ludwigsburg (Dr. D. Weimann, Prof. Dr. Th. Schiedeck);
Caritas-Krankenhaus St. Josef, Regensburg (Prof. Dr. O. Schwandner, PD Dr. A. Fürst);
Mathias-Spital, Rheine (Dr. G. Reitemeyer, Prof. Dr. M. Lausen);
St. Martinus-Krankenhaus, Düsseldorf (Dr. U. Vogel, Dr. O. Bachmann, Dr. H. Grosch);
Klinikum Pirna, Pirna (Dr. J. Stiebitz);
Praxis für Koloproktologie, Kiel (Dr. J. Jongen, Dr. H. Peleikis);
Krankenhaus St. Elisabeth und St. Barbara, Halle (Dr. T. Plettner, Dr. W. Asperger);
Marien-Hospital, Erwitte (Dr. A. Peters);
Bethesda-Allgemeines Krankenhaus, Hamburg (PD Dr. S. Petersen, Prof. Dr. M. Sailer);
Schön-Kliniken, Neustadt i. Holstein (Dr. M. Konrad, Prof. Dr. H. Schimmelpenning);
Diakonissenkrankenhaus, Dresden (Dr. T. Jacobi);
Evangelisches Krankenhaus, Herne (Dr. R. Schmidt, Dr. M. Kemen);
Klinikum Essen-Mitte, Essen (Dr. A. Ommer);
DKD, Wiesbaden (Dr. A. Hofmeister);
Chirurgische Klinik Aschersleben-Staßfurt, Aschersleben-Staßfurt (Dr. Th. Landes);
Enddarmzentrum Mannheim, Mannheim (Prof. Dr. A. Herold);
Universitätsklinikum Lübeck, Lübeck (Dr. J. Nolde, Prof. Dr. H.-P. Bruch);
St. Anna-Virngrund-Klinik, Ellwangen (Dr. O. Mayer, Prof. Dr. B. Ultsch).
Rights and permissions
About this article
Cite this article
Schwandner, O., Fürst, A. & on behalf of the German STARR Registry Study Group. Assessing the safety, effectiveness, and quality of life after the STARR procedure for obstructed defecation: results of the German STARR registry. Langenbecks Arch Surg 395, 505–513 (2010). https://doi.org/10.1007/s00423-009-0591-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-009-0591-8