Abstract
Background and aims
Innate immunity cells play a crucial role in host anticancer defense: cancer patients with high levels of natural killer (NK) cells and eosinophils have a better prognosis. Recombinant interleukin-2 (rIL-2) immunotherapy stimulates innate immunity cells. This study aims to evaluate the toxicity of pre- and postoperative rIL-2 treatment and the effects on innate immunity both in peripheral blood and in cancer tissue of patients with resectable pancreatic adenocarcinoma.
Materials and methods
Seventeen patients received high dose rIL-2 preoperative subcutaneous administration and two low dose postoperative cycles. We evaluated NK cell and eosinophil count in blood and in pancreatic surgical specimens.
Results
Toxicity was moderate. In the early postoperative period, blood NK cells and eosinophils significantly increased compared to basal values (p < 0.02). Histopathological analysis did not find significant intratumoral infiltration of NK cells nor of eosinophils.
Conclusions
Preoperative high dose rIL-2 administration is able to counteract surgery-induced deficiency of NK cells and eosinophils in peripheral blood in the early postoperative period, although it cannot overcome local mechanisms of immune tumor escape in cancer tissue. The amplification of innate immunity, induced by immunotherapy, may improve the control of metastatic cells spreading in the perioperative period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In industrialized nations, pancreatic ductal adenocarcinoma is the fifth leading cause of cancer death with an incidence of nine to ten per 100,000 [1, 2]. Surgical resection nowadays is the only hope for cure [3], but despite advancements in treatment, pancreatic adenocarcinoma still has a dismal prognosis [4]. A new strategy to improve the prognosis of pancreatic cancer patients is immunotherapy which can be based on administration of exogenous cytokines as recombinant interleukin-2 (rIL-2).
The aim of immunotherapy is to enhance the activity of the immune system, both innate (phagocytic cells and lymphocytes with natural cytotoxicity) and adaptive, against tumor cells [5]. In pancreatic cancer patients, a depression of both adaptive and innate immune system has been observed [6–9], with decreased natural killer cell (NK) blood count. NK cells and other immune cells undergo a further count and activity reduction [10] in the postoperative period due to surgical stress [11–18].
Recombinant IL-2 typically acts as T-lymphocyte growth factor [19], but it can also amplify the NK cell and eosinophil pool [20].
Subcutaneous rIL-2 administration shows lower toxicity than intravenous supply [21–25]; preoperative rIL-2 administration in patients with resectable cancers is able to avoid cancer- and surgery-related depression of the immune system. These findings correlate with a better survival, probably because of rIL-2 action on reducing the dissemination of tumor cells in the perioperative period [26–28]. In the postoperative period, repeated cycles of low doses of rIL-2 can increase the amount of NK cells and eosinophils, contributing to control the minimal residual disease [22–25, 29].
The purpose of this study is to evaluate the toxicity of preoperative high dose rIL-2 and postoperative low dose rIL-2 treatment as well as the effects on innate immunity in patients with pancreatic ductal adenocarcinoma. In particular, we compared in one group of pancreatic cancer patients treated with rIL-2 the preoperative NK cell and eosinophil count in peripheral blood with postoperative count; moreover, we compared the NK cell and eosinophil infiltration of the surgical specimens of our rIL-2-treated group with a historical control group of patients.
Materials and methods
Selection of patients
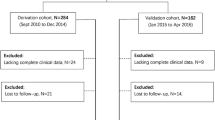
Between September 2003 and January 2006, 45 patients underwent pancreatic resection for pancreatic neoplastic disease at the Department of Surgery of the San Gerardo Hospital in Monza. Before entry, all patients were evaluated by physical examination, chest radiography, abdominal ultrasonography, and computerized tomography of the abdomen.
Inclusion criteria for this study were: diagnosis of pancreatic neoplastic disease amenable to cancer-directed resectional therapy confirmed by imaging procedures, absence of hepatic and/or peritoneal metastases, absence of other primary tumors, Karnofsky performance status superior or equal to 80%, absence of previous radio- or chemotherapy, unaltered renal function, age over 18 years, ability to write informed consent, and histopathological diagnosis of pancreatic ductal adenocarcinoma on surgical specimen. Exclusion criteria were: evidence of central nervous system metastases, active infections, pregnancy, organ failures (cardiac failure grade III–VI of NYHA, uncontrolled angina pectoris, uncontrolled cardiac arrhythmia, uncontrolled asthma or bronchopulmonary disease, lung failure), surgery in the previous 4 weeks, requirement of cortisone therapy, recent cerebral transient ischemic attack or stroke, and histopathological diagnosis on surgical specimen different from pancreatic ductal adenocarcinoma. Considering our criteria, 17 consecutives patients were enrolled in this study. All patients provided written informed consent before entry into the study. The protocol was approved by the local ethics committee.
Surgical procedures
Procedures performed were: 14 pylorus-preserving pancreatico-duodenectomies (Longmire–Traverso procedure), two distal pancreatectomies plus splenectomy, and one total pancreatectomy. All the procedures were macroscopically surgically radical. The removed pathologic specimens were sampled and processed in the Department of Clinical Pathology.
Drug preparation and study design
Human recombinant IL-2 (Proleukin) was supplied by Chiron B.V. (Amsterdam, Netherlands) in vials containing 18 × 106 IU as a lyophilized white sterile powder. Each vial was reconstituted with 3.0 mL of sterile water and kept refrigerated at 4°C to 8°C.
In the preoperative period, 5-mL syringes with an attached 25-gauge needle suitable for subcutaneous injection were each filled with a total volume of 1 mL, containing 6 million IU rIL-2. Such rIL-2 dose was given to patients at 8.00 a.m. and 8.00 p.m. each day, for three consecutive days (from day −4 to day −2, with respect to day of surgery), by subcutaneous injections. In total, patients received 12 million IU daily for 3 days. The day before surgery (day −1), the patients did not receive any immunotherapy and on day 0 they underwent surgical resection.
In the postoperative period, 1 month after surgery (day +30), 5-mL syringes with an attached 25-gauge needle were each filled with 0.5 mL, containing 3 million IU rIL-2. Such rIL-2 dose was given subcutaneously to patients once a day for six consecutive days (day +30/+35). This cycle was repeated monthly for a total of two postoperative cycles (Table 1).
Toxicity
All patients were monitored during each pre- and postoperative cycle for any sign of local and systemic toxicity. Toxicity was graded according to the World Health Organization (WHO) criteria [30]. Complementary treatments consisted of paracetamol and fluid infusion in case of therapy-related pyretic reactions and therapy-related hypotensive reactions, respectively.
Immunological effects in peripheral blood and analytic methods
Once enrolled into the study, patients were evaluated for eosinophils and NK cell count in peripheral blood. Peripheral blood samples were drawn before starting the preoperative rIL-2 treatment (on day −4) and then on the first, seventh, and 14th postoperative days and monthly before each postoperative cycle (on day +30, +60, +90; Table 1).
Peripheral venous blood was collected in 3 mL tubes each filled with 0.072 mL EDTA. Eosinophil count was analyzed using a Sysmex SE 9 500 apparatus (Sysmex Corporation, KOBE, Japan). To measure eosinophil amount, 2.4 μL of blood was extracted from each tube and treated with 0.5976 mL of a red blood cell and white blood cell lysis solution (STROMATOLYSER-EO II) that keeps eosinophilic morphology unaltered, at 40°C. Eosinophil amount was then measured by an impedance system, as provided by the manufacturer.
NK lymphocyte count was measured through a phenotypic analysis of the lymphocytic subpopulations by flow cytometry (FACStar Becton Dickinson Mountain View, CA, USA) using monoclonal antibodies combined with phycoerythrin or fluorescein isothiocyanate. CD16-positive–CD56-positive cells were regarded as NK lymphocytes. The parameters were expressed as cells/mmc. All monoclonal antibodies were provided by Becton Dickinson. The reference values provided from our laboratory were the following: eosinophil count 40–500/μL; NK cell (CD16+/CD56+) count >200/mm3.
Histopathological and immunohistochemical analysis of surgical specimens
The pancreatic specimens were fixed in 10% formaldehyde solution, embedded in paraffin and processed conventionally. Five-micrometer sections were stained with hematoxylin and eosin. Eosinophilic infiltrate was evaluated quantitatively by counting the number of eosinophils per high power field (HPF, ×400). We analyzed a number of ten microscopic fields for each case.
Immunohistochemistry was performed by the avidin–biotin–peroxidase technique. We used anti-CD56 antibody to detect NK cells.
The histopathological findings were compared to those obtained in a historical control group (from January 2002 to August 2003) composed of 16 pancreatic ductal adenocarcinoma patients with comparable characteristics (mean age, location of the tumor, type of surgical resection, TNM staging, histopathological grading, residual disease).
Statistical analysis
Data from blood sample analysis were expressed as mean ± SD. We analyzed differences in eosinophils and NK cell count pre- and postoperatively in peripheral blood. To assess the statistical significance of observed differences, we used Student’s t test for paired samples for continuous variables. p values < 0.05 were considered significant.
Data from histopathological analysis were expressed as mean ± SD. The difference between the treated group and the historical control group for the number of eosinophils and NK cells, infiltrating surgical specimens, was analyzed with Student’s t test for unpaired samples. p values < 0.05 were considered significant.
Results
Patients’ characteristics
Histological diagnosis was pancreatic ductal adenocarcinoma for all patients enrolled in this study. All patients received the preoperative rIL-2 immunotherapy according to the fixed schedule. All patients completed the two postoperative cycles. Characteristics of the patients are shown in Table 2.
Treatment toxicity
Toxicity related to the preoperative rIL-2 treatment was mild, consisting of fever (grade 1 WHO in ten patients and grade 2 in five patients), skin reaction at the site of injection in all patients, and hypotension (grade 1 WHO) in one patient. These symptoms had complete resolution within 24 h from the last rIL-2 administration. Toxicity due to postoperative treatment consisted of fever of grade 1 in 14/17 patients and injection site erythema in all of them. Major toxicity never occurred in both preoperative and postoperative cycles. The treatment could be considered feasible and well tolerated.
Peripheral blood cell response
The mean basal eosinophil value was within reference range (178.7 ± 122.5/μL). In the first 14 postoperative days, we observed a rise in the eosinophil count, reaching a peak of 800.0 ± 568.1/μL on the seventh day (p = 0.0003 with respect to basal value). In the following 3 months, eosinophil amount is close to that one reached on the 14th day (381.3 ± 293.9/μL), although it is significantly superior to basal values only on the 60th day (397.7 ± 282.2/μL, p = 0.008; Table 3, Fig. 1).
NK cell blood count showed a similar response. The baseline mean NK cell appeared close to the inferior limit of the reference range (205.2 ± 106.6/mm3, ranging from 73 to 450/mm3) and with half of the patients with lower values. In the first postoperative day, the typical sudden and important decrease of NK cell count did not occur, and actually, a peak increase of 105.9% was seen (422.6 ± 257.6/mm3) with a p value of 0.005. The elevation versus basal values are significant on the seventh, 14th, and 30th postoperative days. Mean values were significantly higher than basal values (p = 0.001, p = 0.004, and p = 0.005, respectively).
After the 30th postoperative day, we could not observe statistically significant variations of NK cell count (Table 4, Fig. 1).
Histopathological and immunohistochemical analysis
The microscopic analysis revealed that the overall mean value of eosinophils was 1.1 per HPF; in the group of treated patients, the value was 0.68 ± 0.92, while in the control group this was 1.08 ± 0.98. The difference between the two groups was not statistically significant.
The tumor infiltrate did not show the presence of NK cells in the control group nor in the treated group.
Discussion
In pancreatic cancer, several soluble factors produced by a tumoral environment are distributed and have been detected within the host circulatory system, where they create a generalized immunodepression [9]. Immune response cytolytic effectors that interact with tumoral cells are innate (NK cells and eosinophils) and adaptive (as CD8+ cytotoxic T lymphocytes).
NK cells are large granular lymphocytes that cooperate with adaptive immunity and rapidly detect atypical cells, eliminating them. Animal studies reveal a NK cell role critical in suppressing the growth and metastatic spread of tumoral cells [31]. In neoplastic patients, the degree of NK cell activity impairment is directly related to the invasiveness of malignancy and to the risk of recurrence after surgery [32]. Eosinophilia has been seen to have a positive correlation with disease stabilization in cancer patients, confirming that eosinophils play an important role against cancers [33]. Although the antitumoral activity of NK cells and eosinophils, this kind of immunity cannot overcome pancreatic cancer growth because these immune cells may get turned off as they approach the tumor [34, 35].
Since the 1980s, rIL-2 has been utilized in cancer therapy, reaching significant results in improving survival in renal cancer and melanoma patients and in preventing postoperative immunodepression in gastric and colorectal patients [36–38]. Although the focus of rIL-2 immunotherapy effect has been on adaptive immunity, recently it has expanded to rIL-2 effect on promoting NK cell and eosinophil expansion, too. The differentiation and function of these immune cells lead to efficient elimination of tumor cells, thanks to the high affinity IL-2 receptors on their cell surface [33, 39, 40]. Several studies have shown the power of rIL-2 subcutaneous administration to expand eosinophil and NK cell pools in the peripheral blood of cancer patients [41, 42]. Preoperative rIL-2 therapy enhances NK count and activity in patients with colorectal cancer [27], while intermittent and sequential injections of low dose rIL-2 induce a progressive increase in blood NK cells and eosinophils in cancer patients [43].
Pancreatic cancer patients reveal a massive reduction of their innate compartment of immune defense [44] that suffers further important insult by resective operation [11–18]. This is the rationale of our study: to enhance innate immunity in patients with weighty immunosuppression induced by cancer and surgery, as pancreatic cancer patients are.
This study proves the feasibility and tolerability of rIL-2 immunotherapy in operable pancreatic cancer patients. High dose rIL-2 therapy in the preoperative period raised no relevant toxicity, and it was actually well tolerated by almost the entire population studied, as did the two postoperative cycles of treatment with low dose rIL-2.
At baseline, most of our patients presented with reduced levels of innate immunity cells; in particular, the depletion was greater for NK cells than for eosinophils.
The first part of our protocol consisted of a preoperative rIL-2 treatment aimed to abrogate the suppression of blood NK cells and eosinophils, in the very early postoperative period (day +1 to day +30). The daily rIL-2 dose was divided into two half doses in order to guarantee a better distribution throughout the entire day [45]. After preoperative immunotherapy and radical surgery, instead of the expected dramatic decrease of both NK cell and eosinophil count, data actually showed a significant peak of their values since the first postoperative day, doubling the baseline levels. The amount of innate immune cells remained elevated until the 14th postoperative day for eosinophils and until the 30th day for NK cells.
Another aim of our protocol was to power the innate immunosurveillance against the minimal residual disease [46] in the late postoperative period (day +30 to day +90), by two cycles of low dose rIL-2. This treatment failed to improve the high levels of blood NK cells and eosinophils reached in the previous period. It is possible that timing of blood sampling was not appropriate to detect blood cell changes. In fact, we evaluated NK cell and eosinophil count 24 days after the end of each postoperative cycle, just before the new monthly treatment, when the rIL-2 effect is supposed to have already worn off; in this way, probably, we lost the rise of the immune cells. As recent works show [47], we would expect more relevant results for the low dose postoperative cycles if measurements were taken just after 36–38 h from the last rIL-2 administration, when the rIl-2 effect is supposed to be greater.
The histopathological aim of our study was to evaluate the efficacy of preoperative rIL-2 administration to induce a migration and/or increase of eosinophils and NK cells in the pancreatic cancer tissue. It has been shown that in colorectal cancer tissue, rIL-2 treatment promotes eosinophilic infiltration [48]. This releases powerful cytotoxins, like peroxidase and major basic protein, which seem to have an antitumor function [49, 50]. Despite differences of opinions, several studies have reported favorable prognosis in tumors demonstrating tissue eosinophilia [34, 51]. NK cells infiltrating tumors may protect against tumor spread [52], but these cells have never been studied in pancreatic cancer tissues after rIL-2 treatment.
All the cases in our study revealed a very low count of eosinophils in the surgical specimens that could not be defined as “eosinophilic infiltrate”. Neither was there evidence of NK cell infiltration (without significant differences between treated and untreated patients). This result was in contrast to our expectations: the evident effect of rIL-2 in expanding NK cell and eosinophil count in the peripheral blood did not occur in the pancreatic cancer tissue. It is known that pancreatic adenocarcinoma is not typically associated with brisk inflammatory infiltrate, probably due to immunological escape mechanisms performed by tumoral cells [8]. It must also be considered that the method used in our study for the evaluation of eosinophilic infiltrate is not standardized, and that in the literature, other methods are described [34, 53].
Conclusion
Our study demonstrates that peripheral blood NK cells and eosinophils are strongly positively influenced by preoperative immunotherapy with recombinant interleukin-2 at high doses. This effect lasts until 30 days after surgery, and it may play an important role in limiting the spread of tumor cells during surgery and during the immediate following period. We suppose that the host immune stimulation obtained with rIL-2 treatment (although no evident local effect on tumoral tissue) could have a positive impact on overall survival of pancreatic cancer patients.
Our results compel us to further study the effect of rIL-2 therapy on overall survival in randomized groups of pancreatic cancer patients and to check that the induced increase of innate immunity cells is accompanied by an improvement of their activation state. Moreover, we are aimed to research the efficacy of other immunotherapies (as active immunization protocol, use of antibodies against immunosuppressive molecules, adoptively transferred activated immune cells) in pancreatic cancer in order to verify if they are able to overcome the tumoral escape mechanisms.
References
Cruickshank AH, Benbow EW (1995) Pathology of the pancreas, 2nd edn. Springer, London
Rosewicz S, Wiedenmann B (1997) Pancreatic carcinoma. Lancet 15:786–792
Yeo CJ, Cameron JL (1998) Prognostic factors in ductal pancreatic cancer. Langenbecks Arch Surg 383:129–133
Smeenk HG, Tran TC, Erdmann J, van Eijck CH, Jeekel J (2005) Survival after surgical management of pancreatic adenocarcinoma: does curative and radical surgery truly exist? Langenbecks Arch Surg 390:94–103 doi:10.1007/s00423-004-0476-9
Fearon DT, Locksley RM (1996) The instructive role of innate immunity in the acquired immune response. Science 272:50–54 doi:10.1126/science.272.5258.50
Lissoni P, Viviani S, Santoro A (1989) Serum levels of Interleukin-2 in cancer patients: preliminary considerations. Int J Biol Markers 4:203–206
Maltoni M, Pirovano M, Nanni O, Marinari M, Indelli M, Gramazio A et al (1997) Biological indices predictive of survival in 519 Italian terminally ill cancer patients. Italian Multicenter and Study Group on Palliative Care. J Pain Symptom Manage 13:1–9 doi:10.1016/S0885-3924(96)00265-5
von Bernstorff W, Voss M, Freichel S, Schmid A, Vogel I, Johnk C et al (2001) Systemic and local immunosuppression in pancreatic cancer patients. Clin Cancer Res 7(3):925s–932s
Plate JM, Harris JE (2000) Immune cell functions in pancreatic cancer. Crit Rev Immunol 20:375–392
Pollock RE, Lotzova E, Stanford SD (1991) Mechanism of surgical stress impairment of human perioperative natural killer cell cytotoxicity. Arch Surg 126:338–342
Constantian MB, Menzoian JO, Nimberg RB, Schmid K, Mannick JA (1977) Association of a circulating immunosuppressive polypeptide with operative and accidental trauma. Ann Surg 185:73–77 doi:10.1097/00000658-197701000-00012
Lennard TWJ, Shenton BK, Borzotta A, Donnelly PK, White M, Gerrie LM et al (1985) The influence of surgical operations on components of the human immune system. Br J Surg 72:771–776 doi:10.1002/bjs.1800721002
Griffith CD, Rees RC, Platts A, Jermy A, Peel J, Rogers K (1984) The nature of enhanced natural killer lymphocyte cytotoxicity during anaesthesia and surgery in patients with benign disease and cancer. Ann Surg 200:753–758 doi:10.1097/00000658-198412000-00014
Akiyoshi T, Koba F, Arinaga S, Miyazaki S, Wada T, Tsuji H (1985) Impaired production of interleukin-2 after surgery. Clin Exp Immunol 59:45–49
Prochazka M, Vyhnanek F, Jira M, Streicek J (1987) Effect of interleukin-2 on peripheral blood mononuclear cells in severity injured patients. Acta Chir Scand 153:401–404
Brivio F, Lissoni P, Mancini D, Tisi E, Tancini G, Barni S et al (1991) Effect of antitumor surgery on soluble interleukin-2 receptor serum levels. Am J Surg 161:466–469 doi:10.1016/0002-9610(91)91113-W
Hamid J, Bancewicz J, Brown R, Ward C, Irving MH, Ford WL (1984) The significance of changes in blood lymphocyte populations following surgical operations. Clin Exp Immunol 56:49–57
Brivio F, Lissoni P, Alderi G, Barni S, Lavorato F, Fumagalli L (1996) Preoperative interleukin-2 subcutaneous immunotherapy may prolong the survival time in advanced colorectal cancer patients. Oncology 53:263–268
Smith KA (1988) Interleukin-2: inception, impact, and implications. Science 240:1169–1176 doi:10.1126/science.3131876
Brivio F, Lissoni P, Perego MS, Dissoni A, Fumagalli L (2001) Abrogation of surgery-induced IL-6 hypersecretion by presurgical immunotherapy with IL-2 and its importance in the prevention of postoperative complications. J Biol Regul Homeost Agents 15:370–374
Jeal W, Goa K (1997) Aldesleukin (recombinant interleukin-2): a review of its pharmacological properties, clinical efficacy and tolerability in patients with renal cell carcinoma. BioDrugs 7:285–317
Angevin E, Valteau-Couanet D, Farace F, Dietrich PY, Lecesne A, Triebel F et al (1995) Phase I study prolonged low-dose subcutaneous recombinant interleukin-2 (IL-2) in patients with advanced cancer. J Immunother Emphasis Tumor Immunol 18:188–195
Lindemann A, Brossart P, Hoffken K, Flasshove M, Voliotis D, Diehl V et al (1993) Immunomodulatory effects of ultra-low-dose interleukin-2 in cancer patients: a phase-IB study. Cancer Immunol Immunother 37:307–315 doi:10.1007/BF01518453
Nicolini A, Mancini PA, Ferrari P, Anselmi L, Sagripanti A, Carpi A (1996) Immunological and side effects of low sc recombinant interleukin-2 dose in addition to conventional treatment in relapsed breast and colorectal cancer patients. Biomed Pharmacother 50:344–349 doi:10.1016/S0753-3322(96)89666-1
Meropol NJ, Porter M, Blumenson LE, Lindemann MJ, Perez RP, Vaickus L et al (1996) Daily subcutaneous injection of low-dose interleukin-2 expands natural killer cells in vivo without significant toxicity. Clin Cancer Res 2:669–677
Brivio F, Lissoni P, Tisi E, Erba L, Barni S, Tancini G et al (1992) Effects of a preoperative therapy with IL-2 on surgery induced lymphocytopenia in cancer patients. Oncology 49:215–218
Deehan DJ, Heys SD, Ashby J, Eremin O (1995) Interleukin-2 (IL-2) augments host cellular immune reactivity in the perioperative period in patients with malignant disease. Eur J Surg Oncol 21:16–22 doi:10.1016/S0748-7983(05)80061-7
Nieken J, Sleijfer DT, Buter J, de Leij L, Mulder NH (1996) Outpatient based subcutaneous interleukin-2 momotherapy in advanced renal cell carcinoma: an update. Cancer Biother Radiopharm 11:289–295
Guida M, Abbate I, Casamassima A, Musci MD, Latorre A, Lorusso V et al (1995) Long-term subcutaneous recombinant interleukin-2 as maintenance therapy: biological effects and clinical implications. Cancer Biother 10:195–203
Miller AB, Hoogstraten B, Staquet M, Winkler A (1981) Reporting results of cancer treatment. Cancer 47:207–214 doi:10.1002/1097-0142(19810101)47:1<207::AID-CNCR2820470134>3.0.CO;2-6
Kim S, Iizuka K, Aguila HL, Weissman IL, Yokoyama WM (2000) In vivo natural killer cell activities revealed by natural killer cell-deficient mice. Proc Natl Acad Sci U S A 97:2731–2736 doi:10.1073/pnas.050588297
Pross HF, Lotzova E (1993) Role of natural killer cells in cancer. Nat Immunol 12:279–292
Lechin F, Van Der Djis B (2004) Natural killer cells activity and neuroimmunological treatment of cancer. Clin Cancer Res 10:8120–8121 doi:10.1158/1078-0432.CCR-04-1508
Wong DTW, Bowen SM, Elovic A, Gallagher GT, Weller PF (1999) Eosinophil ablation and tumor development. Oral Oncol 35:496–501 doi:10.1016/S1368-8375(99)00023-8
Wallace ME, Smyth MJ (2005) The role of natural killer cells in tumor control—effectors and regulators of adaptive immunity. Springer Semin Immunopathol 27:49–64 doi:10.1007/s00281-004-0195-x
Rosenberg SA (2001) Progress in the development of immunotherapy for the treatment of patients with cancer. J Intern Med 250:462–475 doi:10.1046/j.1365-2796.2001.00911.x
Cerea K, Romano F, Ferrari Bravo A, Motta V, Uggeri F, Brivio F et al (2001) Phase IB study on prevention of surgery-induced immunodeficiency with preoperative administration of low-dose subcutaneous interleukin-2 in gastric cancer patients. J Surg Oncol 78:32–37 doi:10.1002/jso.1120
Nichols P, Ramsden CW, Ward U, Sedman PC, Primrose JN (1992) Perioperative immunotherapy with recombinant interleukin 2 in patients undergoing surgery for colorectal cancer. Cancer Res 52:5765–5769
Miller JS (2001) The biology of natural killer cells in cancer, infection and pregnancy. Exp Hematol 29:1157–1168 doi:10.1016/S0301-472X(01)00696-8
Rivoltini L, Viggiano V, Spinazze S, Santoro A, Colombo MP, Takatsu K et al (1993) In vitro anti-tumor activity of eosinophils from cancer patients treated with subcutaneous administration of interleukin-2. Role of interleukin 5. Int J Cancer 54(5):887 doi:10.1002/ijc.2910540528
Meropol NJ, Barresi GM, Fehniger TA, Hitt J, Franklin M, Caligiuri MA (1998) Evaluation of natural killer cell expansion and activation in vivo with daily subcutaneous low-dose interleukin-2 plus periodic intermediate-dose pulsing. Cancer Immunol Immunother 46:318–326 doi:10.1007/s002620050493
Fehniger TA, Bluman EM, Porter MM, Mrozer E, Cooper MA, Van Deusen JB et al (2000) Potential mechanisms of human natural killer cell expansion in vivo during low-dose IL-2 therapy. J Clin Invest 106:117–124 doi:10.1172/JCI6218
Lissoni P (1997) Effects of low-dose recombinant interleukin-2 in human malignancies. Cancer J Sci Am 3(suppl 1):S115–S120
Brittenden J, Heys SD, Ross J, Eremin O (1996) Natural killer cells and cancer. Cancer 77:1226–1243 doi:10.1002/(SICI)1097-0142(19960401)77:7<1226::AID-CNCR2>3.0.CO;2-G
Davey RT, Chaitt DG, Piscitelli SC, Wells M, Kovacs JA, Walker RE et al (1997) Subcutaneous administration of interleukin-2 in human immunodeficiency virus type 1-infected persons. J Infect Dis 175:781–789
Uhr JW, Scheuermann RH, Street NE, Vitetta ES (1997) Cancer dormancy: opportunities for new therapeutic approaches. Nat Med 3:505–509 doi:10.1038/nm0597-505
Buzio C, Andrulli S, Santi R, Pavone L, Passalacqua R, Potenzoni D et al (2001) Long-term immunotherapy with low-dose interleukin-2 and interferon-alpha in the treatment of patients with advanced renal cell carcinoma. Cancer 92:2286–2296 doi:10.1002/1097-0142(20011101)92:9<2286::AID-CNCR1575>3.0.CO;2-I
Bovo G, Brivio F, Brenna A, Fumagalli L, Perego P, Brivio O et al (1995) Pre-operative Interleukin-2 immunotherapy induces eosinophilic infiltration in colorectal neoplastic stroma. Pathologica 87(2):135–138
Iwasaki K, Torisu M, Fujimura T (1986) Malignant tumor and eosinophils. I. Prognostic significance in gastric cancer. Cancer 58:1321–1327 doi:10.1002/1097-0142(19860915)58:6<1321::AID-CNCR2820580623>3.0.CO;2-O
Fernandez-Acenero MJ, Galindo-Gallego M, Sanz J, Aljama A (2000) Prognostic influence of tumor-associated eosinophilic infiltrate in colorectal carcinoma. Cancer 88:1544–1548 doi:10.1002/(SICI)1097-0142(20000401)88:7<1544::AID-CNCR7>3.0.CO;2-S
Nagtegaal ID, Marijnen CA, Kranenbarg EK, Mulder-Stapel A, Hermans J, van de Velde CJ et al (2001) Local and distant recurrences in rectal cancer patients are predicted by the nonspecific immune response; specific immune response has only a systemic effect—a histopathological and immunohistochemical study. BMC Cancer 1(1):7 doi:10.1186/1471-2407-1-7
Ishigami S, Natsugoe S, Tokuda K, Nakajo A, Che X, Iwashige H et al (2000) Prognostic value of intratumoral natural killer cells in gastric carcinoma. Cancer 88:577–583 doi:10.1002/(SICI)1097-0142(20000201)88:3<577::AID-CNCR13>3.0.CO;2-V
Nielsen HJ, Hansen U, Christensen IJ, Reimert CM, Brunner N, Moesgaard F (1999) Independent prognostic value of eosinophil and mast cell infiltration in colorectal cancer tissue. J Pathol 189:487–495 doi:10.1002/(SICI)1096-9896(199912)189:4<487::AID-PATH484>3.0.CO;2-I
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Degrate, L., Nobili, C., Franciosi, C. et al. Interleukin-2 immunotherapy action on innate immunity cells in peripheral blood and tumoral tissue of pancreatic adenocarcinoma patients. Langenbecks Arch Surg 394, 115–121 (2009). https://doi.org/10.1007/s00423-008-0393-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0393-4