Abstract
Background and aims
Polypropylene mesh repair of large incisional ventral hernias has become increasingly popular. Long-term effects of the mesh on pain and abdominal muscles are not known.
Patients/methods
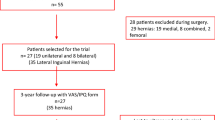
Retromuscular pre-peritoneal polypropylene mesh was placed by open technique in 84 consecutive patients with large ventral hernias (mean defect size 130 cm2). We re-examined the patients after a mean follow-up time of 3 years to find out the frequency of recurrence and chronic pain. We measured the thickness of abdominal muscles of eight patients preoperatively, and postoperatively after 1 year, using magnetic resonance imaging (MRI).
Results
Recurrent hernias had appeared in four patients (5%) at follow-up. Nine patients (13%) needed occasional pain-relieving drugs, but only three (4%) suffered persistent, severe, pain from the mesh. Some limitation during leisure-time physical activities was found in 10% of patients. Only ten patients (12%) were re-operated on because of wound complications or recurrence. MRI study indicated that abdominal muscles were postoperatively well preserved. Although wound infections (6%) and seroma (9%) were frequent complications, there was no need for meshes to be removed in the follow-up.
Conclusion
Open ventral herniorrhaphy with mesh is safe, effective and inexpensive. Small, recurrent hernias were infrequent and easy to re-operated on. Severe pain from the mesh was not common. Postoperative MRI study indicated no obvious damage of abdominal muscles after mesh placement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Incisional hernia develops in 10–20% of patients after abdominal surgery and is an important source of morbidity. It can be repaired by open suture, by use of autogenous tissue flaps or synthetic mesh [1, 2, 3, 4, 5]. Allogenic mesh material has usually been prepared from either polypropylene or polytetrafluoroethylene (ePTFE) [6, 7, 8]. Closure of the complex abdominal hernia is a challenging problem. Recurrence rates after primary suture repair range from 25 to 50% [1, 8, 9]. For open or laparoscopic mesh techniques, the recurrence has varied between 0 and 10%, and wound complications between 2 and 16% [1].
It was recently reported that almost 30% of the patients with inguinal hernias repaired with mesh suffered long-term pain [10]. The aetiological factors may include irritation or damage of inguinal nerves, mesh inguinodynia, inflammatory reaction against the mesh or simply scar tissue [10, 11]. Although a large synthetic mesh between ventral abdominal muscles seems to decrease the recurrence rate, few studies have focused on long-term recurrence, pain or quality of life [12]; therefore, we analysed pain and hernia recurrence after 3 years of follow-up in 84 patients who had been operated on. In addition, we performed magnetic resonance imaging (MRI) of eight patients prior to the operation and 1 year postoperatively to find out if mesh placement would cause atrophy and fatty degeneration of rectus abdominal muscles.
Materials and methods
This was a prospective case series during the years 1997–2002 at a community-based teaching hospital. Eighty-four consecutive patients were operated on between 1997 and 2000 and re-examined by a physician in 2002. The mean follow-up time was 36±22 months (range 20 to 71 months). MRI of eight patients was performed prior to and 12 months after the operation. Patient selection for open mesh repair was based on clinical criteria: fascial defect >4 cm, recurrent hernia, multiple hernias or hernia in a morbidly obese patient [6, 7, 13]. Two senior consultant surgeons operated on 71% of patients, and the rest were operated on by surgical residents with one of the senior consultant.
The operation was based on the open technique popularized by Rives et al. [6], Stoppa [7] and Wantz [13]. Thin, poorly vascularized skin around the hernia sac was excised. The medial borders of both rectus sheaths were incised and the posterior sheath of the rectus dissected up to the edge of the neurovascular pedicle. Inferior epigastric vessels were not damaged if possible. The mesh was placed under the rectus muscle, but external to the posterior fascia or peritoneum, to overlap the defect by at least 4 cm in all directions. The edges of the prosthesis were loosely fixed with six to eight 3–0 absorbable sutures (Vicryl) through the muscle layers and tied over the skin through a small skin incision. The knots were placed into subcutaneous fat under the skin. Usually, three sutures were placed laterally on each side (10-cm gaps), and 1–2 sutures cranially, to fix the mesh. Preservation of the hernia sac unopened provided a layer of viable autogenous tissue to serve as a barrier between the mesh and bowel. If the sac was large it was excised, and the peritoneum and posterior rectus sheath were carefully closed with continuous, absorbable sutures. If possible, the fascia of the anterior rectus sheath was closed by a continuous absorbable suture. We performed no relaxing incisions to help this closure because we tried to avoid damage to skin circulation. Two drains were placed on the mesh and removed after 2 to 3 days postoperatively.
The patients’ characteristics and perioperative data are presented in Table 1. The patients’ data, size of mesh and hernia defect, operation time and wound complications were recorded. The major risk factor for the formation of incisional hernia was obesity. Sixteen patients (19%) had undergone one to three previous ventral hernia operations. There were 26 incisional upper midline hernias, 35 incisional lower midline hernias, 16 other incisional, five umbilical hernias and only two primary hernias. The 35×35 cm multifilament polypropylene mesh (Premilene, B. Braun AG, Germany, or Prolene, Ethicon, USA) was trimmed and placed between the rectus muscles and underlying fascia. To reduce wound infections we administered a single dose of 2 g ceftriaxone intravenously, 30 min before the operation. Thrombo-embolic prophylaxis of low-molecular-weight heparin was given preoperatively and postoperatively for up to 5 days. The routine clinical follow-up examinations by the operating physicians were carried out at 1 and 6 months postoperatively. We obtained long-term results at 36 months by performing a clinical examination and asking the following questions:
1. | Have you felt pain in your trunk muscles within the last month? | Yes/no |
2. | If yes, have you taken any pain-relieving pills? | Yes/no |
3. | Have there been any limitations to your work or leisure-time activities? | Yes/no |
4. | Were there any problems with wound healing? | Yes/no |
5. | Are you satisfied with the operation? | Yes/no |
MRI was performed with a Siemens Harmony 1.0-T magnetic unit (Siemens, Erlangen, Germany). Routine T1-FS and T2-weighted transaxial imaging sequences were used. Slice thickness was 10 mm, to cover the whole abdominal area [14]. The thickness of the rectus abdominis muscle was measured on both sides by use of region-of-interest facilities (Fig. 1). Measure points for each patient were selected on the mid-abdominal area, approximately at the level of the kidneys or at the level of hernia sac. Each patient served as his or her own control. The possible atrophy and fatty degeneration of muscles were also visually assessed on the preoperative and postoperative magnetic resonance images.
The data analysis was carried out with Statistical Package for the Social Sciences (SPPS) for Windows, version 10.0 (SPSS, Chicago, Ill., USA). The statistical evaluation was performed by Student’s t-test for paired values. P<0.05 was regarded as significant.
Results
Wound seromas (9%) and superficial infections (6%) were the most frequent immediate postoperative complications (Table 2). Seroma diagnosis was usually clinical (pain, swelling, fluctuation). If the patient was obese and seroma was suspected, we performed ultrasound scans. Only large, symptomatic seromas were punctioned. None of the meshes had to be removed due to infection. One patient had a late S. aureus infection 6 months postoperatively, and a small part of her mesh was removed during the abscess drainage. Thirty-three patients (40%) were older than 70 years. Small, recurrent hernias at the lateral edges of the mesh were found in four patients (5%) at follow-up. We performed re-operation by placing small piece of the same mesh, to reinforce the defect. Severe pain from the mesh was found in three patients. This was relieved by multiple corticosteroid and local anaesthetic injections. Altogether, ten patients (12%) were re-operated on because of wound complications or suspicion of recurrence (Table 2). No differences in the results were observed between two meshes (Premilene/Prolene).
Long-term quality of life investigation indicated that 80% of the patients were free of pain and 13% had occasionally used pain-relieving drugs (Table 3). Ten per cent felt some limitation during leisure-time or sports activities, and 87% of the patients were satisfied with the operation.
MRI indicated that the abdominal muscles above the mesh were well preserved at 1-year follow-up (Fig. 1). Prior to operation the thickness of rectus muscle on the right and left sides of the hernia were 8.9±2.9 mm and 8.7±2.6 mm, respectively, and postoperatively, 9.3±2.1 mm and 8.3±2.8 mm (not significant, n=8). No progressive atrophic or fatty degeneration changes of the muscles adjacent to the mesh were noticed on postoperative follow-up.
Discussion and conclusions
Incisional hernia is a common complication of abdominal surgery, reported in up to 11% of patients generally, and in up to 23% when associated with wound infection [1]. Our study indicated that the open mesh technique had an outcome that was comparable to previous studies [6, 7, 12]. The immediate complications, long-term hernia recurrence and mesh pain were rare and comparable to laparoscopic results [9]. Our follow-up time was over 2 years, because approximately 66 to 90% of ventral hernia recurrences develop within 2 years of the operation [8]. The technique was relatively simple to learn, even by residents, when compared with laparoscopic or autologous sliding myofascial flap techniques [3, 5]. Almost 90% of the patients were satisfied with the operative result. When mesh was placed into the retromuscular space and properly fixed, the recurrence rate was much lower than in previously reported open series [1, 4, 15, 16, 17]. A few small, recurrent hernias were always at the lateral edges of the mesh. The reason for recurrences was always that too small a mesh had been placed in obese patients. Because polypropylene meshes shrink by up to 30% in the body, the mesh should overlap the hernia defect by at least 4 to 6 cm.
Five comparative studies recently reported advantages of laparoscopic over open mesh repair [1, 9]. Laparoscopic operation resulted in reductions in hospital stay, postoperative pain, blood loss, wound complications and time required for convalescence [8, 9]. Serious complications, such as seromas, infections requiring mesh removal, prolonged suture pain, intestinal injures and trocar site problems have been reported in 13% of laparoscopic techniques as well [8]. The main problem with mesh is that it provides no dynamic support to the abdominal wall. Some surgeons believe that innervated, autogenous tissue, as opposed to prosthetic mesh, is the method of choice in abdominal wall reconstruction [2, 3]. With transection of the external oblique muscle, a compound flap is created that can be advanced 10 cm at the waistline on both sides [3, 18]. The technique may have hernia recurrence of up to 31%, and wound complications in 11% to 40% of patients [18].
Postoperative wound complications can be a source of significant morbidity after open, ventral, hernia repair. The skin and soft tissue over the hernia are usually thin and poorly vascularized and not optimal for healing. Furthermore, the peri-umbilical and epigastric perforators, which partially supply blood and nerves to the abdominal wall, are not all preserved when the open mesh technique is used. Fistula formation and infection are potential complications, but in most series they are below 6% [1, 15, 16, 17]. We think that a wide excision of skin around the hernia sac is necessary to minimize problems in wound healing. Although some perforating vessels and nerves have to be cut when the mesh is being placed, no obvious damage to muscles was noticed on the postoperative magnetic resonance images. Muscle thickness and viability had not changed at follow-up. Modern cross-sectional imaging techniques are being employed with increasing frequency for the assessment of anatomical details of abdominal wall hernias [14]. With most of our patients, the shape and thickness of the rectus abdominal muscles were already reduced preoperatively because of patient’s obesity and inability to use the muscles. In a few patients with massive hernias, it was not easy for us to delineate the muscles in MRI.
Long-term pain after mesh placement in the repair of ventral hernias has not been much studied. Recently, Martin-Duce and co-workers reported that 42 patients of 152 operated on by the open mesh technique suffered from postoperative pain [12]. They reported that all patients had pain for up to 3 months postoperatively, but none of them endured it for more than 12 months [12]. In inguinal herniorrhaphy, long-term pain from the mesh is a well-known complication. We found nerve entrapment in the mesh-fixing sutures in two patients. Only three patients in our study suffered prolonged pain after mesh placement. This was neurogenic in nature and relieved by anti-inflammatory analgesics, corticosteroids and bubivacain injections. Most surgeons use non-absorbable sutures to anchor the mesh. We believe that this causes high tension and may be the cause of prolonged abdominal pain [1, 19]. In conclusion, we feel that the use of open retromuscular mesh is an easy, inexpensive and relatively safe method to repair large incisional hernias. In the long-term follow-up, it may cause low rates of recurrence and pain. Open ventral herniorrhaphy with mesh is safe, effective and inexpensive. Small, recurrent hernias were infrequent and easy to re-operate on. MRI indicated that the rectus muscles are well preserved after mesh placement.
References
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Sukkar SM, Dumanian GA, Szczerba SM, Tellez MG (2001) Challenging abdominal wall defects. Am J Surg 181:115–121
Ramirez OM, Ruas E, Dellon L (1990) “Components separation” method for closure of abdominal wall defects: an anatomic and clinical study. Plast Reconstr Surg 86:519–526
Luijendijk RW, Hop WCJ, van den Tol MP (2000) A comparison of suture repair with mesh repair for incisional hernia. N Eng J Med 343:392–398
Mathes SJ, Steinwald PM, Foster RD, Hoffman WY, Anthony JP (2000) Complex abdominal wall reconstruction: a comparison of flap and mesh closure. Ann Surg 232:586–596
Rives J, Pire JC, Flament JB (1985) Treatment of large eventrations. New therapeutic indications apropos of 322 cases. Chirurgie 111:215–225
Stoppa RE (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Heniford BT, Park A, Ramshaw BJ, Voeller G (2000) Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg 190:645–650
Ramshaw BJ, Esartia P, Schwab J (1999) Comparison of laparoscopic and open ventral herniorrhaphy. Am Surg 65:827–832
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19:48–54
Martin-Duce A, Noquerales F, Villeta R, Hernandez P (2001) Modifications to Rives technique for midline incisional hernia repair. Hernia 5:70–72
Wantz GE (1991) Incisional hernioplasty with Mersilene. Surg Gynecol Obstet 172:129–137
Toms AP, Dixon AK, Murphy JM, Jamieson NV (1999) Illustrated review of new imaging techniques in the diagnosis of abdominal wall hernias. Br J Surg 86:1243–1249
Petersen S, Henke G, Freitag M, Faulhaber A, Ludwig K (2001) Deep prosthesis infection in incisional hernia repair: predictive factors and clinical outcome. Eur J Surg 167:453–457
Temudom T, Siadati M, Sarr MG (1996) Repair of complex giant or recurrent ventral hernias by using tension-free intraparietal prosthetic mesh (Stoppa technique): lessons learned from our initial experience (fifty patients). Surgery 120:738–743
McLanahan D, King LT, Weems C, Novotney M, Gibson K (1997) Retrorectus prosthesis mesh repair of midline abdominal hernia. Am J Surg 173:445–449
Maas SM, Reilingh TSV, Goor H, de Jong D, Bleichrodt RP (2002) Endoscopically assisted “components separation technique” for the repair of complicated ventral hernias. Am Coll Surg 194:388–340
Paajanen H (2002) Do absorbable mesh sutures cause less chronic pain than nonabsorbable sutures after Lichtenstein inguinal herniorrhaphy? Hernia 6:26–28
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Paajanen, H., Hermunen, H. Long-term pain and recurrence after repair of ventral incisional hernias by open mesh: clinical and MRI study. Langenbecks Arch Surg 389, 366–370 (2004). https://doi.org/10.1007/s00423-003-0440-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-003-0440-0