Abstract
Purpose
Several studies have shown that the augmentation index (AIx) is negatively correlated with heart rate (HR). This led some authors to claim that the use of HR-lowering drugs may be detrimental in hypertension. The aim of this study was to assess the longitudinal and cross-sectional relationships of HR with AIx and central blood pressure (BP) in 346 subjects from the HARVEST (mean age 30.7 ± 8.5 years).
Methods
At baseline, HR was measured with 24-h ambulatory recording. Central hemodynamics were evaluated with Specaway DAT system after a median of 8.0 years from baseline. In multivariate linear regression analyses, AIx and central systolic BP were used as dependent variables and night-time HR or office HR as predictors adjusting for several risk factors and confounders.
Results
In fully adjusted models, baseline night-time HR was a significant positive predictor of AIx (p < 0.001) and central BP (p = 0.014) measured 8 years later. Adjusted office HR measured at the time of arterial distensibility assessment was inversely correlated with AIx (p = 0.001) a relationship which was attenuated after physical activity (p = 0.004) and left ventricular ejection time (p = 0.015) were taken into account. In addition, office HR was inversely correlated with central BP (p = 0.039) a relationship which was no longer significant after physical activity and ejection time were accounted for.
Conclusions
These data show that HR measured during sleep is longitudinally associated with AIx and central BP. Thus, low HR in the long term may have beneficial effects on central hemodynamics and the wall properties of the large arteries in hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arterial stiffness is traditionally assessed by means of pulse wave velocity (PWV) (Laurent et al. 2016). However, other measures of arterial stiffness can provide relevant clinical information such as the augmentation index (AIx), which gives an estimate of aortic wave reflection (McEniery et al. 2005; Wilkinson et al. 2002). This index has been found to be a predictor of mortality and cardiovascular events independently of peripheral pressures and is thus likely to be clinically useful (Vlachopoulos et al. 2010; Janner et al. 2013). However, AIx has been shown to be influenced by several clinical variables including age, sex, height, blood pressure (BP), and small artery compliance (McEniery et al. 2005; Wilkinson et al. 2002). In addition, several studies have shown that AIx is negatively correlated with heart rate (HR), and thus, modulation of HR with drugs may have an important impact on this index and on patients’ prognosis (McEniery et al. 2005; Wilkinson et al. 2000). This led some authors to affirm that the use of beta-blockers in hypertension can increase arterial stiffness through the reduction in HR and that these drugs should no longer be included among first-line antihypertensive agents (Williams et al. 2006; Messerli et al. 2016). However, the present information on the relationship between HR and central hemodynamics is based on cross-sectional (McEniery et al. 2005; Wilkinson et al. 2002) or short-term (Manisty and Hughes 2013) studies, whereas the long-term relationship between these clinical variables is largely unknown. High HR has been positively correlated with future arterial stiffness (Benetos et al. 2002; Tomiyama et al. 2010) and adverse cardiovascular outcomes (Palatini et al. 2002; Jouven et al. 2005; Kolloch et al. 2008) in a large number of longitudinal studies. It is, thus, possible that the apparent adverse effect of low HR on central hemodynamics observed in cross-sectional studies is outweighed by its long-term benefits on the arterial wall. Thus, the aim of this study was to assess the longitudinal and cross-sectional relationships of HR with AIx and other central hemodynamic variables in a sample of stage 1 hypertensive adults younger than 45 years. In particular, we tested the long-term prognostic value of HR recorded during sleep with ambulatory monitoring which proved to have better prognostic capacity than HR recorded during waking hours or measured in the office (Hozawa et al. 2008; Hansen et al. 2008; Palatini et al. 2013). Another aim of this investigation was to assess the relationship of baseline ambulatory HR with the development of hypertension needing pharmacological treatment.
Materials and methods
The study participants, took part in the HARVEST (Hypertension and Ambulatory Recording VEnetia STudy), a long-term prospective observational study, initiated in April 1990 in Italy (Palatini et al. 1994b; Sartori et al. 2003; Saladini et al. 2017). Four HARVEST centers agreed to participate in the arterial elasticity study. Arterial elasticity assessment was performed in 346 subjects, a median of 8.0 years after enrolment (interquartile range 2.2–11.1 years). Their mean age at baseline was 30.7 ± 8.5 years and 74.6% were males. Patients’ recruitment was obtained with the collaboration of the local general practitioners who were instructed during local meetings. Patients enrolled were 18–45-year-old subjects, screened for stage 1 hypertension (office systolic BP, 140–159 mmHg, and/or clinic diastolic BP, 90–99 mmHg), who had never been treated for hypertension before. The presence of diabetes, renal impairment, cardiac diseases, and secondary forms of hypertension was excluded at the baseline on the basis of a complete history, physical examination, and by standard diagnostic procedures (Palatini et al. 1994b; Sartori et al. 2003; Saladini et al. 2017). These included serum potassium, urinalysis, plasma renin activity, plasma and urinary aldosterone, and urinary catecholamines. To further exclude the presence of renovascular disease, all patients underwent a doppler examination of the renal arteries or renal scintigraphy. A written informed consent was given by the participants. The study was approved by the HARVEST Ethics Committee and by the Ethics Committee of the University of Padova.
Procedures
Baseline data included medical and family history and a self-compiled questionnaire about current use of alcoholic beverages, smoking status, and physical activity habits (Palatini et al. 1994b; Sartori et al. 2003; Saladini et al. 2017). At the enrollment, all subjects underwent physical examination, anthropometry, office, and ambulatory BP and heart rate measurements. Subjects were categorized as nonexercisers if they did not regularly perform any sports activity and as exercisers if they had performed sports at least once a week during the previous 2 months. Subsequently, among the nonexercisers, the fully sedentary subjects were distinguished from those who performed light physical activities, such as walking, gardening, etc. Among the exercisers, the subjects performing competitive sports were separated from those not involved in competitions (Palatini et al. 1994b). Brachial office BP at entry was the mean of six measurements obtained with a mercury sphygmomanometer, during two visits, performed 2 weeks apart. 24-h BP and heart rate monitoring was performed using the A&D TM2420 model 7 (A&D, Tokyo, Japan) or ICR Spacelabs 90207 monitor (Spacelabs, Redmond, WA, USA) devices. Both these devices were previously validated (Palatini et al. 1991; O’Brien et al. 1991) and were shown to provide comparable results (Palatini et al. 1994a). All assessments including 24-h ambulatory monitoring were performed on a non-exercise day. In each patient, 24-h recording was started between 8:00 a.m. and 10:00 a.m., soon after office BP measurement.
Follow-up visits were scheduled after 1, 2, 3, and 6 months and thereafter at 6-month intervals. At the beginning, all subjects were given general information about non-pharmacological measures by the HARVEST investigators, following the suggestions of the current guidelines on the management of hypertensive patients. If after at least 6 months of implementation of non-pharmacological measures, the participant’s BP was above the “operational threshold level”, the patient was rescheduled for a visit within 2–4 weeks, and the average BP was calculated. If BP was still above the limit, the patient was given antihypertensive drug treatment, otherwise, he or she was checked at monthly intervals. The BP “operational threshold level” was established on the basis of the criteria adopted by international guidelines at the time of patients’ evaluation. Hypertension needing pharmacological treatment was considered as one of the endpoints of the study. Details on follow-up procedures in the HARVEST study are reported in the supplementary material. The arterial distensibility assessment was always performed before giving antihypertensive treatment.
Arterial distensibility assessment
Central BP was assessed from brachial pressure waveform, recorded at the radial artery with applanation tonometry. We used the DAT System (SN1002-960604-12, Specaway, Sydney, Australia), connected to a Millar tonometer (SPC-301; Millar Instruments, Huston, TX, USA). After acquiring 30 sequential waveforms at the radial artery, a software system, which incorporated a validated transfer function, was used to generate an average peripheral and corresponding ascending aortic pressure waveform (Chen et al. 1997). From the radial pulse wave analysis, using a generalized transfer function, derived from the invasive measurements, we obtained central BP values (Chen et al. 1997; Gallagher et al. 2004). The device also returned the radial AIx as the ratio of the difference between the pressure at the second systolic shoulder and diastolic BP to that between diastolic BP and pressure at the first inflection point: AIx = 100 × (P2 − DBP)/(P1 − DBP) (Cameron et al. 1998). PWV (D/ΔT) was determined by simultaneous applanation tonometry and electrocardiography recording, where D was the distance between two sampling sites (carotid and radial artery) and ΔT was the time of travel of pulse wave over this distance. Left ventricular (LV) ejection time was derived from the radial waveform by measuring the time interval from the foot of the pressure waveform to the beginning of the incisura caused by aortic valve closure (Weber et al. 2006; Sugawara et al. 2007).
Patients also underwent measurement of small artery compliance by means of arterial pulse waveform analysis using the HDI/Pulse WaveTM CR2000 (Hypertension Diagnostics, Inc., Eagan, NY, USA) (Cohn et al. 1995). This technique involves a 30-s non-invasive recording of radial artery waveforms by applanation tonometry. The tonometry unit contained an array of pressure transducers capable of measuring the relative intra-arterial pulse amplitude with high accuracy. The tonometer was centered over the radial artery obtaining the optimal waveform by pneumatical stabilization. Brachial BP was oscillometrically measured on the opposite arm. A beat-marking algorithm determined the beginning of the systole, peak systole, onset of diastole, and end-diastole for each beat during the measurement period. To obtain arterial compliance, a model was used that divides the total systemic arterial compliance into large artery and small artery (or oscillatory) compliance (Cohn et al. 1995). The reproducibility of the arterial distensibility measures during the same session and after 4 months was assessed in 72 subjects, as previously described (Longo et al. 2006). Arterial distensibility assessment was always performed in the early afternoon.
Data analysis
Systolic BP amplification was calculated as the difference between peripheral brachial BP and central BP. In keeping with most studies on the prognostic significance of HR, participants were divided into quintiles of either night-time or office HR. To simplify the data presentation, subjects in quintiles 2–4 were grouped together. Thus, we finally obtained three groups with low HR, intermediate HR, and high HR (Tables 1, 2). The top HR quintile has been frequently used in the literature to define people with tachycardia (Palatini et al. 2016).
Statistical analysis
Data are presented as mean ± standard deviation (SD) unless specified. The distributions of clinical variables at baseline were compared across groups by ANCOVA adjusting for age and sex. The significance of differences in categorical variables was assessed with the χ2 test. One-way ANCOVA was used to compare central hemodynamic variables between the HR groups, adjusting for variables potentially influencing central hemodynamics (Table 2). A multivariable linear regression model was used to define the relationship between night-time HR or office HR (predictors) and hemodynamic variables (dependent variables) adjusting for other risk factors and confounders (see Tables 3, 4). A logistic regression model was used to test the predictive capacity of ambulatory and office HRs for development of hypertension needing treatment adjusting for the same variables included in the linear regression analyses. A two-tailed probability value < 0.05 was considered significant. All analyses were performed using Systat versions 12 (SPAA Inc., Evanston, IL, USA).
Results
The baseline characteristics of the study participants, grouped according to night-time HR, are presented in Table 1. Participants with high night-time HR were heavier, were more frequently females, and had higher 24-h diastolic BP compared to the other two groups. In addition, they were less active in sports, though the difference did not attain the level of statistical significance.
Follow-up data
Baseline ambulatory HR as predictor of follow-up central hemodynamics and incident hypertension
Follow-up central BP and AIx progressively increased on going from the participants with low to those with high baseline night-time HR (Table 2). In a multivariable regression analysis, baseline night-time HR was an independent positive predictor of central systolic BP (p = 0.014), pressure amplification (p = 0.004), and AIx (p < 0.001, Table 3) measured 8.0 years later. The relationships with AIx were weaker for 24-h HR (p = 0.014) and daytime HR (p = 0.070). Baseline office HR was unrelated to follow-up central hemodynamics (p = n.s.).
During the 8-year follow-up, 153 participants (44.2%) developed hypertension needing pharmacological treatment. In a fully adjusted logistic regression model (using the same variables, as shown in Table 3), baseline night-time HR was an independent positive predictor of incident hypertension with an odds ratio of 1.39 (95% CI 1.04–1.75) for each 10-bpm increment in HR (p = 0.027). The association with future hypertension was weaker and non-significant for 24-h HR (p = 0.070) and daytime HR (p = 0.065). Baseline office HR was not associated with this outcome (p = n.s.).
Follow-up office HR as predictor of central hemodynamics
Office HR measured at the time of the arterial distensibility assessment was negatively associated with AIx (p = 0.001, Table 4) and central systolic BP (p = 0.039). After inclusion of physical activity habits (p = 0.004) and LV ejection time (p = 0.015) in the regression, the strength of the negative office HR relationship with AIx was attenuated, and the relationship with central BP was abolished (p = 0.14 and p = 0.58, respectively). Office HR was an independent positive predictor of PWV (p = 0.003) measured in the same session. In all regression models, the variance inflation factor was < 2.5 for all variables indicating the absence of multicollinearity.
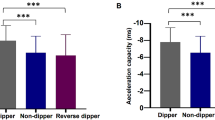
In Figs. 1 and 2, the divergent relationships of baseline night-time HR and follow-up office HR with AIx are shown in the participants divided into HR groups. A positive independent relationship was found for baseline night-time HR (Fig. 1) and a negative relationship for follow-up office HR (Fig. 2). Adjusted mean ± SEM AIx was 19.9 ± 2.5% in the top night-time HR quintile, 14.8 ± 1.4% in the intermediate quintiles, and 5.0 ± 2.7% in the bottom quintile. The corresponding values for adjusted central systolic BP were 126.0 ± 1.8, 121.8 ± 1.0, and 119.0 ± 1.7 mmHg, respectively.
Augmentation index measured 8 years after baseline examination in 346 HARVEST participants divided into quintiles of baseline night-time heart rate. Data are mean ± SEM. p for ANCOVA after adjusting for age, sex, body height, body mass index, mean office blood pressure, pulse wave velocity, small artery compliance, and left ventricular ejection time
Augmentation index in 346 HARVEST participants divided into quintiles of office resting heart rate measured in the same session. Data are mean ± SEM. p for ANCOVA after adjusting for age, sex, body height, body mass index, mean office blood pressure, pulse wave velocity, and small artery compliance. After inclusion of left ventricular ejection time in the model the association was attenuated to a non-significant level (p = 0.093)
Discussion
The present data show that HR recorded with ambulatory monitoring is a positive longitudinal predictor of AIx, central BP, and pressure amplification indicating that low HR in the long term has a favorable impact on central hemodynamics in hypertension. The association of night-time HR with central hemodynamics remained significant also when variables such as physical activity, PWV, or small artery compliance, which have been implicated as possible modulators of AIx (Edwards and Lang 2005; Laurent et al. 2011; Courand and Lantelme 2014; Segers et al. 2001; Saladini et al. 2014) were taken into account. Another interesting finding was that baseline night-time HR was associated with future hypertension needing pharmacological treatment, whereas 24-h HR, daytime HR, and office HR were not significantly associated with this outcome. These results were obtained in a cohort of young-to-middle-age subjects screened for stage 1 hypertension and never treated for the disease.
The relationship between HR and arterial stiffness depends on the complex interplay of many different factors. Several cross-sectional studies have shown that a lower resting HR is associated with higher aortic systolic BP and greater AIx (Wilkinson et al. 2000, 2002; Courand and Lantelme 2014; Laurent et al. 2003). This observation has been attributed to a shift of the backward wave reflected from the periphery into late systole secondary to the prolongation of LV ejection time and to the increase in stroke volume at low HRs (McEniery et al. 2005; Wilkinson et al. 2000, 2002; Messerli et al. 2016). This finding led some authors to claim that HR reduction in hypertension is detrimental, because it may favor the risk of cardiovascular events (Williams et al. 2006; Messerli et al. 2016). However, other factors such as high PWV and low small artery compliance can cause earlier backward wave reflection, thereby increasing AIx and central BP (Courand and Lantelme 2014; Saladini et al. 2014). Studies in human beings have shown that there is a progressive increase in PWV by increasing HR with pacing which is independent from pressure changes (Lantelme et al. 2002; Tan et al. 2016), and in the present study, office HR was cross-sectionally associated with PWV. Thus, pharmacological HR lowering by reducing PWV might have a favorable effect on central hemodynamics. However, the present results showed that when PWV was accounted for in the multivariable regressions, AIx and central systolic BP still had a negative relationship with simultaneously measured office HR (Table 4).
A totally different picture was observed for long-term associations. Tomiyama et al. (2010) and Benetos et al. (2002) have shown that high HR was a long-term predictor of accelerated arterial stiffness measured with PWV in either normotensive or hypertensive subjects. Our results show that a positive longitudinal relationship with HR is present also for central hemodynamics. Indeed, in the present study, night-time HR was an independent predictor of AIx and central BP measured 8 years after baseline HR assessment. This finding indicates that HR reduction in the long run can have a favorable effect and not a detrimental one on all parameters of arterial distensibility and contributes to explain why people with lower HR have a reduced risk of cardiovascular events and mortality in hypertension (Palatini et al. 2002; Jouven et al. 2005; Kolloch et al. 2008). The association of night-time HR with incident hypertension confirms the previous results from other investigators (Inoue et al. 2007; Wang et al. 2014). Elevated heart rate exposes the arteries to increased magnitude and frequency of mechanical load which may eventually increase the stiffness of the vascular wall (Giannoglou et al. 2008) as shown by the above-mentioned reports. It is thus possible that the increase in vascular stiffness favors the development of hypertension in people with tachycardia.
In the present study, among the ambulatory HRs, night-time HR emerged as the strongest predictor of future central hemodynamics and systemic hypertension. This finding is in keeping with the previous data which showed that high HR during the night-time but not during waking hours was associated with increased cardiovascular events (Palatini et al. 2013) or non-cardiovascular mortality (Hozawa et al. 2008; Hansen et al. 2008) indicating that night-time HR is more representative of the overall hemodynamic load on the arteries. HR during sleep is more stable and reproducible than HR measured during waking hours or in the office which may be influenced by random fluctuations related to emotional triggers or occasional physical activities (Palatini et al. 2013).
Study limitations
A possible limitation of the present study is that central systolic BP was estimated from non-invasive pressure waveforms and was not measured directly. With this technique, the values for central pressures depend on the validity and applicability of the generalized transfer function used to generate the central aortic waveforms. However, the transfer function used by the DAT system to derive central BP has been validated in several studies which showed a good correspondence between calculated and directly recorded central BP (Chen et al. 1997; Adji et al. 2007). In addition, it should be noted that the calibration of central aortic pressures heavily depends on the accuracy of the brachial BP measurements. Another potential weakness of this study is that we did not control for dietary factors. Dietary components such as antioxidants might be important in determining differences in arterial distensibility parameters. However, our data were obtained from a homogeneous cohort of people with similar dietary habits. Finally, the present results were obtained in subjects younger than 45 years, and thus, they may not be extrapolated to older individuals. However, the previous data suggest that central AIx is a more sensitive marker of large artery stiffness in younger (< 50 years) than older individuals (McEniery et al. 2005).
Conclusion
In contrast with data from cross-sectional studies, we found that HR recorded during sleep with ambulatory monitoring was directly and positively associated with central hemodynamics measured 8 years later. Thus, HR lowering in hypertension may have long-term favorable effects on the wall properties of the large arteries and improve patients’ prognosis. However, whether lowering high ambulatory HR can actually improve cardiovascular outcomes in hypertensive patients remains to be seen.
Abbreviations
- AIx:
-
Augmentation index
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- HR:
-
Heart rate
- LV:
-
Left ventricular
- PWV:
-
Pulse wave velocity
- SD:
-
Standard deviation
- SEM:
-
Standard error mean
References
Adji A, Hirata K, Hoegler S, O’Rourke MF (2007) Noninvasive pulse waveform analysis in clinical trials: similarity of two methods for calculating aortic systolic pressure. Am J Hypertens 20:917–922
Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K (2002) Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation 105:1202–1207
Cameron JD, McGrath BP, Dart AM (1998) Use of radial artery applanation tonometry and a generalized transfer function to determine aortic pressure augmentation in subjects with treated hypertension. J Am Coll Cardiol 32:1214–1220
Chen CH, Nevo E, Fetics B, Pak PH, Yin FC, Maughan WL et al (1997) Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure. Validation of generalized transfer function. Circulation 95:1827–1836
Cohn JN, Finkelstein S, McVeigh G, Morgan D, LeMay L, Robinson J et al (1995) Noninvasive pulse wave analysis for the early detection of vascular disease. Hypertension 26:503–508
Courand PY, Lantelme P (2014) Significance, prognostic value and management of heart rate in hypertension. Arch Cardiovasc Dis 107:48–57
Edwards DG, Lang JT (2005) Augmentation index and systolic load are lower in competitive endurance athletes. Am J Hypertens 18:679–683
Gallagher D, Adji A, O’Rourke MF (2004) Validation of the transfer function technique for generating central from peripheral upper limb pressure waveform. Am J Hypertens 17:1059–1067
Giannoglou GD, Chatzizisis YS, Zamboulis C, Parcharidis GE, Mikhailidis DP, Louridas GE et al (2008) Elevated heart rate and atherosclerosis: an overview of the pathogenetic mechanisms. Int J Cardiol 126:302–312
Hansen TW, Thijs L, Boggia J, Li Y, Kikuya M, Björklund-Bodegård K et al (2008) Prognostic value of ambulatory heart rate revisited in 6928 subjects from 6 populations. Hypertension 52:229–235
Hozawa A, Inoue R, Ohkubo T, Kikuya M, Metoki H, Asayama K et al (2008) Predictive value of ambulatory heart rate in the Japanese general population: the Ohasama study. J Hypertens 26:1571–1576
Inoue T, Iseki K, Iseki C, Kinjo K, Ohya Y, Takishita S (2007) Higher heart rate predicts the risk of developing hypertension in a normotensive screened cohort. Circ J 71:1755–1760
Janner JH, Godtfredsen NS, Ladelund S, Vestbo J, Prescott E (2013) High aortic augmentation index predicts mortality and cardiovascular events in men from a general population, but not in women. Eur J Prev Cardiol 20:1005–1012
Jouven X, Empana JP, Schwartz PJ, Desnos M, Courbon D, Ducimetiere P (2005) Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med 352:1951–1958
Kolloch R, Legler UF, Champion A, Cooper-Dehoff RM, Handberg E, Zhou Q et al (2008) Impact of resting heart rate on outcomes in hypertensive patients with coronary artery disease: findings from the INternational VErapamil-SR/trandolapril STudy (INVEST). Eur Heart J 29:1327–1334
Lantelme P, Mestre C, Lievre M, Gressard A, Milon H (2002) Heart rate: an important confounder of pulse wave velocity assessment. Hypertension 39:1083–1087
Laurent P, Albaladejo P, Blacher J, Rudnichi A, Smulyan H, Safar ME (2003) Heart rate and pulse pressure amplification in hypertensive subjects. Am J Hypertens 16:363–370
Laurent P, Marenco P, Castagna O, Smulyan H, Blacher J, Safar ME (2011) Differences in central systolic blood pressure and aortic stiffness between aerobically trained and sedentary individuals. J Am Soc Hypertens 5:85–93
Laurent S, Marais L, Boutouyrie P (2016) The noninvasive assessment of vascular aging. Can J Cardiol 32:669–679
Longo D, Zaetta V, Perkovic D, Frezza P, Ragazzo F, Mos L et al (2006) Impaired arterial elasticity in young patients with white-coat hypertension. Blood Press Monit 11:243–249
Manisty CH, Hughes AD (2013) Meta-analysis of the comparative effects of different classes of antihypertensive agents on brachial and central systolic blood pressure, and augmentation index. Br J Clin Pharmacol 75:79–92
McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR, ACCT Investigators (2005) Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 46, 1753–1760
Messerli FH, Rimoldi SF, Bangalore S, Bavishi C, Laurent S (2016) When an increase in central systolic pressure overrides the benefits of heart rate lowering. J Am Coll Cardiol 68:754–762
O’Brien E, Mee F, Atkins N, O’Malley K (1991) Accuracy of the SpaceLabs 90207 determined by the British Hypertension Society protocol. J Hypertens 9:573–575
Palatini P, Penzo M, Canali C, Pessina AC (1991) Validation of the accuracy of the A & D TM-2420 model 7 for ambulatory blood pressure monitoring and effect of microphone replacement on its performance. J Amb Monit 4:281–288
Palatini P, Mormino P, Canali C, Santonastaso M, De Venuto G, Zanata G et al (1994a) Factors affecting ambulatory blood pressure reproducibility. Results of the harvest trial. Hypertension 23:211–216
Palatini P, Graniero G, Mormino P, Nicolosi L, Mos L, Visentin P et al (1994b) Relation between physical training and ambulatory blood pressure stage I hypertensive subjects. Results of the HARVEST Trial. Hypertension and Ambulatory Recording Venetia Study. Circulation 90:2870–2876
Palatini P, Thijs L, Staessen JA, Fagard RH, Bulpitt CJ, Clement DL et al (2002) Predictive value of clinic and ambulatory heart rate for mortality in elderly subjects with systolic hypertension. Arch Intern Med 162:2313–2321
Palatini P, Reboldi G, Beilin LJ, Eguchi K, Imai Y, Kario K et al (2013) Predictive value of night-time heart rate for cardiovascular events in hypertension. The ABP-International study. Int J Cardiol 168:1490–1495
Palatini P, Rosei EA, Casiglia E, Chalmers J, Ferrari R, Grassi G et al (2016) Management of the hypertensive patient with elevated heart rate: statement of the second consensus conference endorsed by the European Society of Hypertension. J Hypertens 34:813–821
Saladini F, Benetti E, Mos L, Mazzer A, Casiglia E, Palatini P (2014) Regular physical activity is associated with improved small artery distensibility in young to middle-age stage 1 hypertensives. Vasc Med 19:458–464
Saladini F, Fania C, Mos L, Mazzer A, Casiglia E, Palatini P (2017). Office pulse pressure is a predictor of favourable outcome in young-to-middle-aged subjects with stage 1 hypertension. Hypertension 70 (in press)
Sartori M, Semplicini A, Siffert W, Mormino P, Mazzer A, Pegoraro F et al (2003) G-protein beta3-subunit gene 82ST allele and hypertension: a longitudinal study in young grade I hypertensive. Hypertension 42:909–914
Segers P, Qasem A, De Backer T, Carlier S, Verdonck P, Avolio A (2001) Peripheral “oscillatory” compliance is associated with aortic augmentation index. Hypertension 37:1434–1439
Sugawara J, Komine H, Hayashi K, Maeda S, Matsuda M (2007) Relationship between augmentation index obtained from carotid and radial artery pressure waveforms. J Hypertens 25:375–381
Tan I, Spronck B, Kiat H, Barin E, Reesink KD, Delhaas T et al (2016) Heart rate dependency of large artery stiffness. Hypertension 68:236–242
Tomiyama H, Hashimoto H, Tanaka H, Matsumoto C, Odaira M, Yamada J et al (2010) Synergistic relationship between changes in the pulse wave velocity and changes in the heart rate in middle-aged Japanese adults: a prospective study. J Hypertens 28:687–694
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C (2010) Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 31:1865–1871
Wang A, Liu X, Guo X, Dong Y, Wu Y, Huang Z et al (2014) Resting heart rate and risk of hypertension: results of the Kailuan cohort study. J Hypertens 32:1600–1605
Weber T, Auer J, O’Rourke MF, Punzengruber C, Kvas E, Eber B (2006) Prolonged mechanical systole and increased arterial wave reflections in diastolic dysfunction. Heart 92:1616–1622
Wilkinson IB, MacCallum H, Flint L, Cockcroft JR, Newby DE, Webb DJ (2000) The influence of heart rate on augmentation index and central arterial pressure in humans. J Physiol 525 Pt 1:263–270
Wilkinson IB, Mohammad NH, Tyrrell S, Hall IR, Webb DJ, Paul VE et al (2002) Heart rate dependency of pulse pressure amplification and arterial stiffness. Am J Hypertens 15:24–30
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D et al (2006) Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation 113:1213–1225
Funding
The study was funded by the University of Padova, Padua, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interest.
Additional information
Communicated by Massimo Pagani.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Palatini, P., Saladini, F., Mos, L. et al. Low night-time heart rate is longitudinally associated with lower augmentation index and central systolic blood pressure in hypertension. Eur J Appl Physiol 118, 543–550 (2018). https://doi.org/10.1007/s00421-017-3789-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-017-3789-4