Abstract
Purpose
Cephalic hemodynamic assessment is important in initial orthostatic hypotension. We sought to investigate cephalic blood flow (CBF) in the earlobe using a mini laser Doppler flowmeter (LDF) during orthostatic challenge. In addition, we clarified hemodynamic differences during a new active standing protocol using a footstool standing test (FST) with bending of the legs on the footstool in the sitting position to reduce the load of the squatting posture in the conventional squat standing test (SST).
Methods
Ten healthy men (21 ± 0.5 years) performed the SST after a 1 min squat and the FST after a 1 min load consisting of bending the legs on a footstool in the sitting position. Earlobe CBF, beat-to-beat arterial blood pressure (ABP), mean arterial blood pressure (MAP), and heart rate (HR) were recorded during each test.
Results
Earlobe CBF showed a transient fall synchronized with the ABP during each test. No significant differences in the recovery times (RTs) of CBF and MAP were observed during the SST (CBF 12.9 ± 0.6 s vs. MAP 12.1 ± 0.5 s, P = 0.313) and FST (CBF 10.6 ± 0.4 s vs. MAP 10.1 ± 0.8 s, P = 0.552). Although the CBF and ABP decreases were not different in each test, the HR increase was significantly lower with the FST (24 ± 2 bpm) than with the SST (31 ± 3 bpm, P < 0.005).
Conclusions
Earlobe CBF reflects the compensatory ABP regulatory response during standing and is potentially useful for estimating the orthostatic ABP response indirectly. Furthermore, the FST is a low-load protocol that can be an effective protocol for a standing test of cardiac function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Initial orthostatic hypotension (IOH) is an exaggerated transient decrease in arterial blood pressure (ABP) that occurs within 15 s after active standing (Wieling et al. 2007; Vaddadi et al. 2007). Despite the acute decrease in ABP, ABP is well maintained during standing by compensatory physiological regulation, such as baroreflex stimulation (Rossberg and Penaz 1988), which is associated with tachycardia and secondary peripheral vasoconstriction (Philips and Scheen 2011; Scheen and Philips 2012). However, when these responses are insufficient, they occasionally lead to syncope or short-lasting symptoms of pre-syncope (light-headedness, visual disturbances, and nausea), precipitated by insufficient cerebral perfusion (Lipsitz 1989; Thomas et al. 2009). Hence, evaluation of the cerebral blood flow during orthostatic stress is also important clinically, in addition to beat-to-beat ABP measurement (Imholz et al. 1990; van der Velde et al. 2007).
Recently, we developed a mini laser Doppler flowmeter (LDF) that can be worn on the earlobe to measure cephalic blood flow (CBF) during orthostatic stress. The orthostatic response of CBF in the earlobe has not been clarified. The auricle of the ear lacks sympathetic innervation (Peuker and Filler 2002). Hence, we predicted that CBF in the earlobe is likely to show a sensitive response corresponding to systemic hemodynamic changes on standing by removing the influence of sympathetic nerve activity, and it might be a useful index of cephalic perfusion during orthostatic challenge.
In regard to standing methods, active standing such as standing from the supine position (Tanaka et al. 1996; Hilz 2002) or passive standing, such as the head-up tilt (HUT) (Tanaka et al. 1996; Rickards and Newman 2003), has been performed clinically. In recent years, standing from a squat position (squat standing test: SST) has been investigated as an active standing test (Rossberg and Penaz 1988; Rickards and Newman 2003; Philips and Scheen 2011). The SST has an advantage for IOH assessment, since it tends to elicit a greater hypotensive response than HUT (Rossberg and Penaz 1988; Rickards and Newman 2003; Wieling et al. 2007), and only requires a 1–2 min load of squatting before standing (compared with at least 5 min of supine rest) (Wieling et al. 2007). Other advantages are that it is a quick and simple method without large scale equipment, such as a bed, and provides a highly reproducible cardiovascular stimulus (Convertino et al. 1998). However, it is difficult for subjects, especially elderly people, to maintain the squatting posture for at least 1 min without leg pain. These are the constraints in clinical practice. Thus, to reduce the load of pre-standing, a new active standing method using a footstool (footstool standing test: FST) to achieve a pseudo-squatting posture with bending of the legs on the footstool in the sitting position was developed and evaluated in this study.
The purpose of this study was to investigate the earlobe CBF response during orthostatic stress and to clarify the physiological differences in the hemodynamic responses during the FST and the SST to verify whether the FST can be used as an active standing test.
Materials and methods
Subjects
Ten healthy men (mean ± SD age: 21 ± 0.5 years, height 172 ± 5 cm, weight 61 ± 11 kg) volunteered to participate in the study. All volunteers were free of known cardiovascular or neurological disease, and no volunteers were taking prescription drugs or other medications. The study conformed to the guidelines established by the Declaration of Helsinki and was approved by the Institutional Review Board of the Faculty of Medicine, University of Yamanashi (approval No. 924). Each subject gave his informed consent after an explanation of the experimental procedures and potential risks. The experiments were performed >2 h after the volunteers had a midday meal.
Mini laser Doppler blood flowmeter
The LDF (de Mul et al. 1984; Obeid et al. 1990; Serov et al. 2006) is intended to estimate tissue blood flow (BF). A mini LDF (105 mm × 62 mm × 25 mm; 144 g) was newly developed by Pioneer Corp (Kawasaki, Japan) (Fig. 1a). This is a miniaturized model of a conventional stationary LDF and prototype for research. The principle of LDF measurement is laser Doppler flowmetry (Bonner and Nossal 1981). When a laser is irradiated on the tissue, the BF is estimated from the spread of the Doppler-shifted frequency generated by the interference between the non-Doppler-shifted light backscattered from static tissue and the Doppler-shifted light backscattered from red blood cells flowing in blood capillaries. The values of BF are represented by the product of the amount and the speed of red blood cells. The sensor probe of the new device (21 mm × 12 mm × 3 mm; 21 g) is composed of the laser emitting unit and the backscattered light receiving unit and is provided with a window on the surface contacting the body. This new device was designed to generate little artifact noise in a dynamic environment such as postural change. The main unit of the new device includes a battery and a wireless transfer function, and it is also wearable by subjects because of its small size and light weight. A laser wavelength of 850 nm was used and the BF was expressed in arbitrary units. In this study, the mini LDF was used to measure CBF in the earlobe continuously during orthostatic postural changes of the body. The sensor probe was worn on the subjects’ earlobe attached by a clip (Fig. 1b). The BF values transferred via a Bluetooth system were recorded on a personal computer equipped with specially developed data acquisition software. The sampling frequency of the BF waveform was 50 Hz.
Prior to the present study, the new device’s performance for BF measurement was confirmed to be equivalent to the conventional stationary LDF device by measuring a physiological blood flow response, the sympathetic skin blood flow response (SFR) (Low et al. 1983), as follows. One healthy subject wore the conventional LDF sensor probe (CDF-2000 SNCR; CyberFirm, Tokyo, Japan) and the mini LDF sensor probe on the second fingertip of the left hand simultaneously, and then the fingertip BF was measured. After the measurement at rest for about 20 s, the subject performed deep breathing, known to induce a SFR, and a transient decrease of fingertip BF was recorded.
Physiological Measurements
Continuous beat-to-beat ABP was measured using noninvasive tonometry monitoring (model BP-608, Omron Colin, Kyoto, Japan) on the wrist of the left hand (the radial artery), which was supported at the level of the right atrium on an adjustable pad with a band support. Mean arterial blood pressure (MAP) was calculated with off-line analysis from tonometry ABP monitoring. Stroke volume (SV) and heart rate (HR) were recorded beat-to-beat by non-invasive cardiac output measurement using analysis of thoracic electrical bioimpedance signals (Physioflow Lab-1; Manatec Biomedical, Macheren, France). Cardiac output (CO) was calculated from HR and SV using the following equation: \({\text{CO = HR }} \times {\text{ SV}}\). Total peripheral resistance (TPR) was calculated from MAP and CO using the following equation: \({\text{TPR = MAP/CO}}\). All measurements were connected to an acquisition system (PowerLab 8/30, ADInstruments, Bella Vista, Australia) interfaced with a personal computer equipped with data acquisition software (LabChart 6, ADInstruments) for beat-to-beat recording of variables. Waveforms were sampled at 1 kHz.
Experimental procedure
The subjects were seated on a prepared chair, and then instrumented for hemodynamic measurements (ABP, SV, HR, CO, and TPR). Furthermore, a mini LDF probe was attached to the left earlobe for CBF measurement. Then, two standing-up tests, the SST and the FST, were carried out using the following steps.
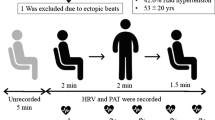
SST protocol: the protocol is shown in Fig. 2a. After subjects rested in the sitting position for 2 min, they took a squatting position on the floor and maintained the position for 1 min. Subsequently, they stood up within 1 or 2 s, and then maintained the standing position for 1 min. Since it was expected that respiration-induced periodic fluctuation of blood pressure could interfere with the CBF waveform on standing, the subjects were instructed to stand up after breathing out slightly and stopping respiration just before standing. Subjects resumed respiration after ABP started to recover. These steps were performed as one measurement, and then repeated three times for each subject.
FST protocol: the protocol is shown in Fig. 2b. After subjects rested in the sitting position for 2 min, they took a pseudo-squatting posture formed by bending and holding their legs with their hands on the prepared footstool in the seated position and maintained the position for 1 min. The footstool used in this study had a height of 30 cm, and it was adjusted to be the interval of 10 cm between the top of the footstool and the seat of the chair. Subsequently, the subjects stood up on the floor within 1 or 2 s after the footstool was removed, and they then maintained the standing position for 1 min. The subjects stood after breathing out slightly and stopping respiration just before standing, and they resumed respiration after ABP started to recover, as for the SST. These steps were performed as one measurement, and then repeated three times for each subject. In the SST and FST protocols, the standing distances in the vertical direction are different. The standing distance of the FST (df) is shorter than that of the SST (ds) (ds > df), as shown in Fig. 2.
Data analysis
In order to compare hemodynamic responses between the SST and FST, each hemodynamic index was resampled at 10 Hz, and then averaged time series waveforms were generated as the amount of change from the pre-standing baseline, defined as the average of the 30 s period just before standing. In calculating the amount of the peak or nadir change from the pre-standing baseline for each hemodynamic index, measurements of each standing test were taken three times for each subject and averaged as one subject data (n = 10 in triplicate). Thus, the mean values obtained for the 10 subjects’ data with each standing test were compared. The recovery times (RTs) of MAP and CBF were defined as the intervals between just after standing and the point when recovery to the pre-standing baseline had occurred (Fig. 3). Mean RT values were compared between MAP and CBF and between SST and FST. The decrease time (DT), defined as the time from just after standing to the nadir, and the increase time (IT), defined as the time from the nadir to pre-standing baseline (Fig. 3), were calculated. The mean values of DT and IT were compared in order to elucidate the difference in RT between the SST and FST. The mean RT, DT, and IT values were basically calculated from the 10 subjects’ data obtained by averaging the three measurement values on each standing test as one subject data (n = 10 in triplicate). However, for calculating RT and IT, the data that had not recovered completely to baseline were excluded, because these parameters could not be calculated.
Statistics
All group data are expressed as mean ± SE. The differences in mean values were evaluated by a paired t-test, after the assumption of normality of paired differences was confirmed with a Shapiro-Wilk test. P < 0.05 was considered significant. All data were analyzed using SPSS 22.0 for Windows (SPSS Japan Inc, Tokyo, Japan).
Results
First of all, the new device’s performance for BF measurement was confirmed. When measuring the SFR by deep breathing using the conventional LDF and the new mini LDF, a transient decrease of fingertip BF was observed, and the BF response of the new device showed good agreement with that of the conventional device (Fig. 4). Although these results comparing the two measurements in one person, at one time, are only an indication that they are measuring the same physiological phenomenon, the performance of the new device was confirmed to be comparable to that of the conventional stationary LDF device.
Orthostatic response of CBF in the earlobe
Typical acute responses of CBF and ABP to the SST and FST in one subject are presented in Fig. 5. Just after the subjects stood up from the squatting position, CBF decreased immediately, and then recovered to the pre-standing level within 15 s (Fig. 5a). It was seen that this transient fall reaction of CBF was synchronized with the change in ABP. CBF and ABP were also measured with the FST protocol, in which the subjects stood up from the sitting position after removal of the footstool. The transient falls in CBF and ABP after standing were also observed with the FST protocol (Fig. 5b). The changes in CBF and ABP in the FST protocol (Fig. 5b) were almost the same as those in the SST protocol (Fig. 5a).
Orthostatic responses of each hemodynamic parameter
In addition to CBF, beat-to-beat hemodynamic signals, MAP, SV, HR, CO, and TPR were also measured during the SST and FST protocols. Figure 6 shows the averaged time series waveforms as the amount of change from the pre-standing baseline (n = 10 in triplicate). In the SST protocol, MAP decreased transiently and recovered within 15 s after rising in parallel with the change in CBF. A transient fall of MAP was similarly detected in the FST protocol. With either protocol, SV decreased gradually after standing and then recovered, and HR and CO increased rapidly after standing, and then began to decrease. TPR also showed a transient decrease with both protocols. Although HR with the FST showed a slight increase from 3 s just before standing, this increase was not observed with the SST.
Averaged time series waveforms of hemodynamic parameters as the amount of change from the pre-standing baseline during the SST (a) and the FST (b). Solid lines and error bars represent means and ±SE values, respectively. The vertical broken line in each panel indicates the onset of standing. HR heart rate, SV stroke volume, CO cardiac output, TPR total peripheral resistance
The amounts of the changes from the pre-standing baseline to the peak or nadir during the SST and FST protocols were then calculated for the hemodynamic parameters (Table 1). For calculating the nadir variation of SV, the data of one subject during the SST were excluded because no decrease in SV was observed after standing. The amount of HR change from the pre-standing baseline was significantly lower during the FST than during the SST (P < 0.05). In contrast, there were no significant differences in the changes of other variables (CBF, MAP, SV, CO, and TPR) during the SST and FST.
Time-dependent changes of CBF and MAP
Since CBF showed transient falls and recovery to the pre-standing baseline after standing, the time from start to the baseline (RT) was investigated and compared with that of MAP. For calculating RT, the SST data for subjects whose CBF did not recover completely to baseline were excluded (n = 1). During the SST, there was no significant difference (P = 0.313) in the RT between CBF and MAP, which were 12.9 ± 0.6 s and 12.1 ± 0.5 s, respectively (Fig. 7a). During the FST, there was also no significant difference (P = 0.552) in the RT between CBF and MAP, 10.6 ± 0.4 s and 10.1 ± 0.8 s, respectively (Fig. 7a). In the comparison between the two standing protocols, the RT of CBF was significantly shorter during the FST (10.7 ± 0.4 s) than during the SST (12.9 ± 0.6 s, P < 0.01, Fig. 7b). Moreover, MAP showed a significantly shorter RT during the FST (10.1 ± 0.8 s) than during the SST (12.0 ± 0.4 s, P < 0.05, Fig. 7b).
a Comparisons of the RT of CBF during the SST and the RT of MAP during the SST, and of the RT of CBF during the FST and the RT of MAP during the FST. b Comparisons of the RT of CBF during the SST and the RT of CBF during the FST, and of the RT of MAP during the SST and the RT of MAP during the FST. Data are mean ± SE values. Asterisk significant different between the SST and FST (P < 0.05, paired t test). NS not significant. Note that significant differences are not seen in the RTs for CBF and MAP during the SST and FST. a SST (CBF: n = 9, MAP: n = 9), FST (CBF: n = 10, MAP: n = 10), b CBF (SST: n = 9, FST: n = 9), MAP (SST: n = 10, FST: n = 10)
In order to elucidate the difference in RT between SST and FST, RT was divided into two phases, DT and IT. For calculating IT, the SST data of one subject whose CBF did not recover completely to baseline were excluded (n = 1). Although the DT of MAP was significantly shorter during the FST than during the SST (P < 0.05; Table 2), IT did not show a significant difference between the protocols (P = 0.057; Table 2). There was also a significantly shorter DT of CBF during the FST than during the SST (P < 0.001; Table 2). However, there was no significant difference in the IT of CBF between the two protocols (P = 0.230; Table 2).
Discussion
The goals of this study were to clarify the orthostatic response of CBF in the earlobe and the physiological differences of the hemodynamic responses during the FST and the SST. The key novel findings in this regard were as follows. First, a transient CBF response associated with the ABP on standing was observed. Second, the pattern of hemodynamic responses was similar between the SST and FST. Third, the amounts of the falls of the CBF and MAP did not differ between the tests. Fourth, the increase in HR from the pre-standing baseline was significantly lower during the FST than during the SST. Fifth, the RT during each standing test was not different for the CBF and MAP, although the RTs of the CBF and MAP were significantly shorter during the FST than during the SST.
The CBF response during orthostatic stress would be considered to be under the influence of the ABP response. The transient response in ABP that occurred within 15 s after standing, the rapid ABP recovery, was due to arterial baroreflex stimulation (Rossberg and Penaz 1988; Thrasher 2005), which is associated with tachycardia and vasoconstriction (Philips and Scheen 2011; Scheen and Philips 2012). Consequently, it appears that CBF also recovered depending on ABP recovery. These results suggest that a rapid and transient fall of CBF occurs physically and directly along with the dynamic and systemic ABP changes that occur with standing. This appeared to be a reasonable response, because ABP works to send blood to the head during orthostatic postural change. Furthermore, the good synchronization between CBF in the earlobe and ABP on standing may be related to the region of the earlobe. For example, the SFR occurs at the fingertips by sympathetic stimulation (Low et al. 1983). However, the SFR does not occur at the earlobe and differs from other regions such as the fingertip, because the earlobe is devoid of sympathetic nerve supply (Peuker and Filler 2002). Hence, CBF in the earlobe might be more sensitive to dynamic ABP changes by removing sympathetic nerve effects. Fingertip blood flow measurement of the orthostatic response has been previously reported (Oimomi et al. 1985). However, the earlobe is a more suitable region to evaluate orthostatic hemodynamics for that reason. CBF in the earlobe can reflect the response seen with the compensatory ABP regulation mechanism that leads to recovery of the ABP fall through the baroreflex, even though the CBF is not equivalent to central ABP.
The basic trends of the hemodynamic responses after standing were almost equivalent between the SST and FST. In particular, the MAP decrease during the FST would be due to the decreased TPR as in the SST, because the falls of MAP and TPR occur at the same time that CO increases during standing. A number of investigators has previously reported that IOH is due to a cardiopulmonary baroreflex induced by a sudden increase in right atrial pressure on standing (Borst et al. 1984; Sprangers et al. 1991; Tanaka et al. 1996; Yamaguchi et al. 1996). The effects of the muscle pump on standing are responsible for a sudden rise in right atrial pressure via translocation of blood from venous beds toward the heart. This immediate increase in right atrial pressure activates cardiopulmonary baroreflex-mediated sympathetic inhibition and a subsequent fall of TPR. On the other hand, we do not know how much the cardiopulmonary baroreflex contributes to the ABP fall, because ABP and TPR decreased concurrently. In particular, sympathetic nervous control of peripheral resistance is relatively slow, showing a delay of about 4 s (Rowell 1993; Toska et al. 1994). Furthermore, Wieling et al. proposed that the almost immediate onset and rapid fall in the systemic vascular resistance during leg exercise is too fast to be explained by sympathetically mediated reflex effects due to stimulation of cardiopulmonary afferents (Wieling et al. 1996). For these reasons, one cannot suggest that the cardiopulmonary baroreflex contributes to ABP falling profoundly during active standing, such as during the SST and the FST.
Tschakovsky et al. reported that the decrease in MAP on standing from squatting could be attributed to the increase in virtual vascular conductance in the lower limbs, and, therefore, any involvement of the cardiopulmonary baroreflex in IOH was so small as to be physiologically insignificant (Tschakovsky et al. 2011). In our other experiment, large decreases in TPR and ABP were observed simultaneously after releasing cuff pressure of 200 mmHg at the thigh. These facts suggest that vascular conductance increases greatly, both physically and mechanically, when released from a state in which the lower limb joints are bent or compressed. Moreover, a downward shift of blood due to standing also contributes to increased vascular conductance. Therefore, it seems that the reduction in ABP is due to expansion of lower limb vascular conductance also during the FST, and the involvement of the cardiopulmonary baroreflex in IOH may be so small as to be physiologically insignificant also during the FST.
The SST and FST in this study induced sufficient decreases of CBF and MAP within the 1 min load of pre-standing. Rossberg and Penaz (Rossberg and Penaz 1988) reported a MAP fall of approximately 45 mmHg when standing up after 6 min of squatting, and Rickards and Newman (Rickards and Newman 2003) observed a MAP fall of 24 ± 2 mmHg 10 s after standing up from 4 min of squatting. In the present study, the fall in MAP was 27 ± 3 mmHg during the SST and 22 ± 3 mmHg during the FST 4 s after standing up from a 1 min pre-load. Furthermore, the MAP fall during the SST was similar to that reported by Rickards and Newman (Rickards and Newman 2003). Although the amount of the MAP fall during the FST tended to be somewhat smaller than that during the SST, there was no significant difference between them. Therefore, the present FST with the 1 min pre-load of standing induced a sufficient reduction in MAP that was as much as that during the SST. In contrast, the difference in the amount of reduction of MAP may be related to pre-load time, and a long pre-load time may be suitable for evaluation of orthostatic challenge because of the larger decrease in MAP. However, a large ABP fall due to a long pre-load time may result in some subjects developing a number of pre-syncopal symptoms, including dizziness, nausea, pallor, sweating of the skin, and blurred vision (Rickards and Newman 2003), and the specificity of the standing-up test is probably lower because of pre-syncopal symptoms in healthy subjects (Wieling et al. 2007). Hence, a standing-up test with a long pre-load period or pain is not appropriate for a clinical test.
In contrast, the characteristic physiological difference in the FST/SST protocols was the HR response during standing. The increase in the HR during standing was significantly lower during the FST than during the SST. This finding leads us to conclude that the FST has an important advantage in that subjects can be tested with less cardiac load. The amount of exercise due to standing during the FST is smaller than that during the SST because the distance moved in the vertical direction is shorter during the FST than during the SST. In addition, cardiac sympathetic tone due to the arterial baroreflex (Borst et al. 1982; Rossberg and Penaz 1988) might be less during the FST than during the SST. On the other hand, the mild rise in HR just before standing during the FST may be related to a slight transition movement of a few seconds caused by moving the legs from the footstool to the floor. This leg motion could have acted as mild exercise when the subjects received the signal to stand up from the examiner.
In the time-dependent change, the RTs of CBF and MAP were comparable during the two standing-up methods. This could be attributed to the synchronization between CBF and ABP and indicates that the RT of CBF offers promise as an evaluation index of ABP recovery during orthostatic challenge. In contrast, the RTs of CBF and MAP were significantly smaller during the FST than during the SST. These results may be due to small DTs of CBF and MAP during the FST (Table 2). The expansion of lower limb vascular volume on standing may be greater during the SST because lower limb vascular volume is much smaller due to the greater load during the squatting position. Therefore, more time for ABP to fall may be expected. In contrast, the time for the ABP to fall during the FST might be shorter because the load of pre-standing is small, and the expansion of lower limb vascular volume on standing is also smaller than during the SST. The state of increase would indicate ABP recovery by the arterial baroreflex (Rossberg and Penaz 1988; Thrasher 2005). The IT may also be an efficient index to evaluate circulatory regulation.
Generally, non-invasive continuous monitoring of beat-to-beat ABP (i.e., Finapres) is useful for IOH evaluation, because intermittent ABP measurements cannot detect rapid and transient ABP falls (van der Velde et al. 2007). However, the device is not necessarily convenient, and the procedure is normally unavailable for routine clinical practice. Although estimating the orthostatic ABP response from CBF in the earlobe is an indirect method, the present results with the mini LDF device would contribute to simple assessment of the ABP response seen with the compensatory ABP regulation mechanism during postural change, from clinical practice to healthcare field. In addition, the FST would be a useful and safe method, for example, especially for elderly subjects, because of the low load of pre-standing and the lesser effect on cardiac function on standing. In the FST, however, the degree of bending of the legs is alleviated to some extent as compared to the SST, during which the legs are bent sufficiently by their own weight during squatting. Therefore, sufficient leg bending on the footstool is important during the FST to induce a sufficient ABP decrease on standing.
Limitations
The present study was restricted to healthy young men. There are differences in postural cardiac autonomic modulation by sex, and the degree of the autonomic response to orthostatic challenge varies with normal aging (Barantke et al. 2008). Aging is associated with diminished arterial baroreflex sensitivity and with ABP instability during orthostatic challenge (Shi et al. 2003). Therefore, the RT of CBF in the earlobe may be extended in elderly healthy subjects. These effects could be evaluated in further mechanism studies. On the other hand, the FST protocol will be useful and safe for elderly subjects because of the low load of pre-standing and the lesser effect on cardiac function on standing. Hence, the FST protocol needs to be investigated in elderly subjects. As to the relation between CBF in the earlobe and cerebral blood flow, it was not investigated in the present study. CBF in the earlobe is supplied by external carotid artery and not internal carotid artery that mainly supplies the brain. Hence, it is unknown whether CBF in the earlobe is directly related to cerebral blood flow. Measurements of continuous middle cerebral artery BF velocity by transcranial Doppler ultrasound (Aaslid et al. 1982) may be able to clarify the relation between CBF in the earlobe and cerebral blood flow. In addition, subjects with abnormal hemodynamics, such as those with autonomic failure, syncope, or orthostatic intolerance, were not evaluated. Future research should also be conducted to investigate whether CBF in the earlobe obtained from orthostatic challenge is associated with the abnormal ABP response in subjects with orthostatic intolerance.
Conclusions
In summary, our findings suggest that the CBF in the earlobe reflects the ABP response during standing. Consequently, the CBF in the earlobe using mini LDF is potentially useful for estimating the orthostatic ABP response indirectly; the RT of the CBF can be an effective index to assess ABP recovery. We also demonstrate that the fundamental mechanism of orthostatic ABP response during each test appears to be the same and the FST not only elicits a sufficient ABP fall but also reduces the load on cardiac function on standing. The FST can be an effective protocol as a standing test imposing a low load on cardiac function during standing.
Abbreviations
- ABP:
-
Arterial blood pressure
- BF:
-
Blood flow
- CBF:
-
Cephalic blood flow
- CO:
-
Cardiac output
- DT:
-
Decrease time
- FST:
-
Footstool standing test
- HR:
-
Heart rate
- HUT:
-
Head-up tilt
- IOH:
-
Initial orthostatic hypotension
- IT:
-
Increase time
- LDF:
-
Laser Doppler flowmeter
- MAP:
-
Mean arterial blood pressure
- RT:
-
Recovery time
- SST:
-
Squat standing test
- SFR:
-
Sympathetic flow response
- SV:
-
Stroke volume
- TPR:
-
Total peripheral resistance
References
Aaslid R, Markwalder TM, Nornes H (1982) Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg 57:769–774
Barantke M, Krauss T, Ortak J, Lieb W, Reppel M, Burgdorf C, Pramstaller P, Schunkert H, Bonnemeier H (2008) Effects of gender and aging on differential autonomic responses to orthostatic maneuvers. J Cardiovasc Electrophysiol 19:1296–1303
Bonner R, Nossal R (1981) Model for laser Doppler measurements of blood flow in tissue. Appl Opt 20:2097–2107
Borst C, van Brederode J, Wieling W, van Montfrans G, Dunning AJ (1984) Mechanisms of initial blood pressure response to postural change. Clin Sci (Lond) 67:321–327
Borst C, Wieling W, van Brederode J, Hond A, de Rijk L, Dunning A (1982) Mechanisms of initial heart rate response to postural change. Am J Physiol 243:H676–H681
Convertino V, Tripp LD, Ludwig DA, Duff J, Chelette TL (1998) Female exposure to high G: chronic adaptations of cardiovascular functions. Aviat Space Environ Med 69:875–882
de Mul FFM, van Spijker J, van der Plas D, Greve J, Aarnoudse J, Smits T (1984) Mini laser-Doppler (blood) flow monitor with diode. Appl Opt 23:2970–2973
Hilz M (2002) Assessment and evaluation of hereditary sensory and autonomic neuropathies with autonomic and neurophysiological examinations. Clin Auton Res 12:133–143
Imholz BP, Settels JJ, van der Meiracker AH, Wesseling KH, Wieling W (1990) Non-invasive continuous finger blood pressure measurement during orthostatic stress compared to intra-arterial pressure. Cardiovasc Res 24:214–221
Lipsitz L (1989) Orthostatic hypotension in the elderly. N Engl J Med 321:952–957
Low P, Neumann C, Dyck P, Fealey R, Tuck R (1983) Evaluation of skin vasomotor reflexes by using laser Doppler velocimetry. Mayo Clin Proc 58:583–592
Obeid AN, Barnett NJ, Dougherty G, Ward G (1990) A critical review of laser Doppler flowmetry. J Med Eng Technol 14:178–181
Oimomi M, Nishimoto S, Matsumoto S, Hatanaka H, Ishikawa K, Baba S (1985) Evaluation of periflux blood flow measurement in diabetic patients with autonomic neuropathy. Diabetes Res Clin Pract 1:81–85
Peuker ET, Filler TJ (2002) The nerve supply of the human auricle. Clin Anat 15:35–37
Philips JC, Scheen AJ (2011) Squatting test: a posture to study and counteract cardiovascular abnormalities associated with autonomic dysfunction. Auton Neurosci 162:3–9
Rickards CA, Newman DG (2003) A comparative assessment of two techniques for investigating initial cardiovascular reflexes under acute orthostatic stress. Eur J Appl Physiol 90:449–457
Rossberg F, Penaz J (1988) Initial cardiovascular response on change of posture from squatting to standing. Eur J Appl Physiol Occup Physiol 57:93–97
Rowell L (1993) Human cardiovascular control. Oxford University Press, New York, pp 443–444
Scheen AJ, Philips JC (2012) Squatting test a dynamic postural manoeuvre to study baroreflex sensitivity. Clin Aut Res 22:35–41
Serov AN, Nieland J, Oosterbaan S, de Mul FFM, van Kranenburg H, Bekman HHPT, Steenbergen W (2006) Integrated optoelectronic probe including a vertical cavity surface emitting laser for laser Doppler perfusion monitoring. IEEE Trans Biomed Eng 53:2067–2074
Shi X, Huang G, Smith S, Zhang R, Formes K (2003) Aging and arterial blood pressure variability during orthostatic challenge. Gerontology 49:279–286
Sprangers R, Wesseling K, Imholz A, Imholz B, Wieling W (1991) Initial blood pressure fall on stand up and exercise explained by changes in total peripheral resistance. J Appl Physiol 70:523–530
Tanaka H, Sjöberg BJ, Thulesius O (1996) Cardiac output and blood pressure during active and passive standing. Clin Physiol 16:157–170
Thomas KN, Cotter JD, Galvin SD, Williams MJA, Willie CK, Ainslie PN (2009) Initial orthostatic hypotension is unrelated to orthostatic tolerance in healthy young subjects. J Appl Physiol 107:506–517
Thrasher TN (2005) Baroreflex control of sodium excretion and arterial pressure baroreceptors, baroreceptor unloading, and the long-term control of blood pressure. Am J Physiol Regul Integr Comp Physiol 288:R819–R827
Toska K, Eriksen M, Walløe L (1994) Short-term cardiovascular responses to a step decrease in peripheral conductance in humans. Am J Physiol 266:H199–H211
Tschakovsky ME, Matusiak K, Vipond C, McVicar L (2011) Lower limb-localized vascular phenomena explain initial orthostatic hypotension upon standing from squat. Am J Physiol Heart Circ Physiol 301:H2102–H2112
Vaddadi G, Lambert E, Corcoran SJ, Esler MD (2007) Postural syncope: mechanisms and management. Med J Aust 187:299–304
Van der Velde N, van den Meiracker AH, Stricker BHC, van der Cammen TJM (2007) Measuring orthostatic hypotension with the Finometer device: is a blood pressure drop of one heartbeat clinically relevant? Blood Press Monit 12:167–171
Wieling W, Harms M, ten Harkel A, van Lieshout J, Sprangers R (1996) Circulatory response evoked by a 3 s bout of dynamic leg exercise in humans. J Physiol 494:601–611
Wieling W, Krediet CTP, van Dijk N, Linzer M, Tschakovsky ME (2007) Initial orthostatic hypotension: review of a forgotten condition. Clin Sci (Lond) 112:157–165
Yamaguchi H, Tanaka H, Adachi K, Mino M (1996) Beat-to-beat blood pressure and heart rate responses to active standing in Japanese children. Acta Paediatr 85:577–583
Acknowledgments
The authors wish to sincerely thank the subjects for their interest and cooperation.
Conflict of interest
Financial support of collaboration for this study was provided by the Pioneer Corporation. M. Goma and Y. Kimura are employed by Pioneer Corporation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Massimo Pagani.
Rights and permissions
About this article
Cite this article
Goma, M., Kimura, Y., Shimura, H. et al. Orthostatic response of cephalic blood flow using a mini laser Doppler blood flowmeter and hemodynamics of a new active standing test. Eur J Appl Physiol 115, 2167–2176 (2015). https://doi.org/10.1007/s00421-015-3197-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-015-3197-6