Abstract
Purpose
The presumption in a cold sensitivity test (CST) used for cold injuries is that the skin temperature (T sk) observed reflects the return of blood flow to the extremity following a local cold challenge. We questioned this assumption.
Methods
Six non-cold injured participants undertook two CSTs in 30 °C air. The control (CON) CST involved 12 min gentle exercise prior to immersing the foot into 15 °C water for 2 min followed by 15 min of spontaneous rewarming. The occlusion (OCC) CST was the same except that blood flow to the foot was occluded during the rewarming period. These results were compared to CSTs from six individuals with non-freezing cold injury and moderate–severe cold sensitivity (CS) and a non-perfused human digit model (NPDM).
Results
Before immersion, great toe skin blood flow (SkBF) was similar in CON and OCC conditions [255 (107) laser Doppler units (LDU)] and was higher than CS [59 (52) LDU]. During rewarming, SkBF in CON returned to 104 % of the pre-immersion value and was higher than both OCC and CS. Great toe T sk before immersion was lower in CS [28.5 (2.1) °C] compared to CON [34.7 (0.4) °C], OCC [34.6 (0.9) °C] and NPDM [35.0 (0.4) °C]. During rewarming skin/surface temperature in OCC, CS and NPDM were similar and all lower than CON.
Conclusions
SkBF does contribute to the skin rewarming profile during a CST as a faster rate of rewarming was observed in CON compared to either OCC or NPDM. The lower T sk in CS may be due to a reduced basal SkBF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-freezing cold injury (NFCI) occurs as a result of prolonged exposure to low ambient temperatures and often wet conditions, leading to a protracted period of cold-induced vasoconstriction and reduced skin blood flow (SkBF). In the long term this can result in lasting cold sensitivity (CS) (defined as pronounced and prolonged vasoconstriction to a mild cold stimulus) and persistent pain (Ungley and Blackwood 1942).
NFCI of the feet was the largest cause of non-combative casualties during the Falkland Isles Conflict (Francis 1984) and remains a significant cause of morbidity, lost training time, and long-term disability for the military (Francis and Oakley 1996; Oakley 1996). NFCI is also a high risk for the homeless (King et al. 1958; Mills and Mills 1993) and elderly (Ramstead et al. 1980; Williams et al. 2005) who may be exposed to cool temperatures for prolonged periods. Similarly, victims of earthquakes and other such accidents that render individuals immobile in cool and temperate climates may also be at risk. Furthermore, with the increasing popularity of outdoor pursuits such as mountaineering (Imray et al. 2009; Imray and Oakley 2005; Marcus 1979), skiing and water sports (Eglin 2011; Laden et al. 2007) where individuals are exposed to cold and wet environments for extended periods, the risk of NFCI in civilians may also be significant.
The cold sensitivity test (CST) used currently in cold injury clinics (in conjunction with a medical examination to diagnose NFCI), uses infrared thermography to measure skin surface temperature as an estimation of SkBF in response to a cold challenge. Patients rest for an hour in 30 °C air, then immerse their foot (protected by a plastic bag to prevent skin wetting and subsequent evaporative cooling) in water at 15 °C for 2 min following which their foot is allowed to spontaneously rewarm in air for 5 min. The degree of cold sensitivity (CS) is then classified according to the toe skin temperature (T sk) before immersion and at 5 min post immersion (Thomas and Oakley 2001).
The technique of measuring T sk with infrared thermography as an estimation of SkBF during and after a CST is described in the literature (Francis and Oakley 1996; Oakley 1998). However, it is not possible to determine whether the changes in T sk observed are due to vasodilatation, passive rewarming of unperfused tissues or a combination of the two. In addition, if the pre-immersion equilibrium period is not of sufficient duration or temperature to promote adequate vasodilatation, then following the cold challenge, vasoconstriction may continue in uninjured individuals as well as those with a NFCI.
To examine the role of a haemodynamic mechanism in the observed T sk changes to cold challenge, Golden et al. (2003) investigated the response of non-perfused tissue to a CST. A non-perfused human digit model (NPDM) was incubated in 34.5 °C water for 1 h before following the standard CST protocol. Following the CST, the surface temperature rewarming of the NPDM was very similar to the response of uninjured individuals. This indicated that for some participants, the thermograms were in fact measuring passive changes in T sk and not changes in SkBF, suggesting that the CST protocol lacked specificity.
It has been shown that increasing deep body temperature by 0.3 °C prior to immersion through gentle exercise promoted vasodilatation and increased the reproducibility of the CST (Eglin et al. 2005). However a relationship between T sk and SkBF measured using infrared photoplethysmography was not observed during the CST (Eglin et al. 2005). A poor correlation between infrared thermography and SkBF measured using laser Doppler has been reported previously and attributed to the poor sensitivity of infrared thermography to changes in blood flow compared to that of laser Doppler (Clark et al. 2003). However, in the study by Eglin et al. (2005), the possibility remains that the poor correlation was due to observed changes in T sk being due to passive rewarming (from either the environment or deeper tissues) and not vasodilatation.
The aim of this study was to identify the contribution of SkBF to the T sk responses to a CST of non-cold injured individuals by comparing the responses of a perfused foot with a non-perfused foot in which the arterial blood flow to the limb was occluded during the rewarming phase. These responses were compared to those of a group of individuals who had been diagnosed with NFCI and had moderate/severe or severe CS.
It was hypothesised that arterial occlusion at the ankle would result in slower rewarming following a CST in non-cold injured participants (hypothesis 1). It was also hypothesised that the CS would have a reduced SkBF, lower resting T sk and rewarm slower when compared to the non-cold injured controls (hypothesis 2).
Methods
This study was approved by the University of Portsmouth BioSciences Research Ethics Committee and all participants gave their informed written consent prior to participating in the study.
Participants
Six volunteer participants, three Caucasian males, two Caucasian females and one Chinese female, with no history of cold injury (frostnip, frostbite or NFCI) or peripheral vascular disease (Raynaud’s phenomenon, vibration white finger or diabetes) took part in the study [mean (SD); age = 21 (1) years; body mass = 75.1 (14.0) kg; height = 178.5 (9.7) cm; resting, supine systolic blood pressure = 126 (9) mmHg]. The phase of the menstrual cycle was not controlled in this study as previous studies have found no difference in the vasoconstrictor response to local cooling with changes in reproductive hormone status (Charkoudian and Johnson 1999). Individuals who smoked regularly (more than 10 cigarettes a week) were excluded from the study due to the effect of nicotine on peripheral blood flow (Rodrigues et al. 2001). The testing was carried out over 1 week during February when the average outside air temperature was 9 °C.
Five African–Caribbean males and one African–Caribbean female [mean (SD); age = 28 (6) years] previously diagnosed with NFCI at a cold injuries clinic and with moderate/severe or severe CS of the feet (classified from toe skin temperatures during a CST conducted in air at 30 °C: below 32 °C before immersion and below 28 °C after 5 min of rewarming) were also tested. None were smokers. They were tested at different times of the year (January, April, May and October with an average outside temperature of approximately 10 °C), 3.4 (1.2) years following their injury (range of 1.3–4.9 years).
Procedures
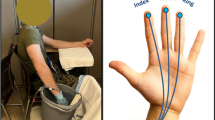
Each non-cold injured participant attended two laboratory sessions (CON and OCC), in a balanced order and the cold sensitive participants attended one session. Both groups carried out the protocol as described by Eglin et al. (2005). The participants entered a climatic chamber at an air temperature of 30.7 (0.5) °C, removed their shoes and socks, and sat resting for 15 min. At the end of this period, their foot T sk was recorded. The non-cold injured participants then cycled on a cycle ergometer (874E, Monark, Sweden) for 12 min at an external work rate of 50 W. The CS participants carried out either the cycle ergometer exercise (50 W, n = 4), stepping (at 22 steps min−1 on a 20 cm step, n = 1) or arm cranking (10 W, n = 1); the mode of exercise being determined by peripheral pain resulting from their cold injury. Following this, the participants rested in a recumbent position for 5 min, whilst auditory stimuli were kept to a minimum (Edwards et al. 1998) and they refrained from speaking, as rate and phase of respiration have been found to affect microcirculation (Mayrovitz and Groseclose 2002; Wilder-Smith et al. 2005). Throughout this time baseline T sk and SkBF were recorded.
The participant’s right foot was then placed in a plastic bag to keep it dry and then immersed in a water bath to the point of their mid-malleoli for 2 min. The water bath was stirred and maintained at 14.9 (0.2) °C. After the immersion period, the plastic bag was removed and in the CON condition and for the CS group, rewarming was monitored for 15 min whilst the participant remained resting in a supine position. One participant in the CS group was only monitored for 10 min during the rewarming period and therefore from 11 to 15 min n = 5 for this group. In the OCC condition, a blood pressure cuff was placed at the ankle prior to the immersion and on removal from the water was inflated to 40 mmHg above the resting systolic pressure measured at the ankle. This pressure (approximately 160–170 mmHg) was maintained for the duration of the 15 min rewarm phase.
A comparison of the surface temperature profiles of a NPDM was also made. Two non-perfused models, with similar anthropometric and thermal properties to a human digit, made from pig tissue, were placed in a thin latex glove and incubated in a water bath at 37.3 °C for 60 min. This temperature was chosen as it gave the same surface temperature as the mean pre-immersion T sk of the non-cold injured participants. They were then dried and a thermal image was taken in 30 °C air. The NPDM was placed in a plastic bag and immersed in water at 15 °C for 2 min. After the immersion period, the plastic bag was removed and rewarming was monitored for 15 min with the NPDM suspended from a clamp in 30 °C air. Thermal images were recorded every 2 s throughout the rewarming period.
Measurements
Resting blood pressure at the arm and ankle was measured manually using a mercury sphygmomanometer (Dekamet MK3, Accoson, UK) while the participant rested in a recumbent position. This was used to determine the occlusion pressure. Participants’ anthropometric data were recorded including their height using a stadiometer (Leicester, Bodycare, UK) and their mass using digital weighing scales (770, Seca, Germany).
Deep body temperature of the six non-cold injured participants was measured using a rectal thermistor self-inserted 15 cm beyond the anal sphincter (REC-U-VL-2, Grant Instruments Ltd, Cambridge, UK, with a resolution of 0.05 °C that was checked against a Digitron T600 thermometer, RS Components Ltd, UK calibrated in compliance with ISO 17025:2005) and recorded using a data logger (1000 series, Grants Instruments Ltd, Cambridge, UK).
T sk was measured using a thermal imaging camera (A320G, FLIR systems, UK). T sk was taken from the great toe pad and recorded on entering the chamber, prior to exercise, prior to immersion and every 2 s of the 15 min rewarm period.
SkBF was estimated using multichannel laser Doppler probe (VPIT/7 probe, Moorlab, Moor Instruments, UK) attached to both great toe pads and recorded continuously. Probes were attached with double adhesive tape, having been calibrated before each test against Brownian motion with a standardised colloidal suspension of polystyrene microspheres. In addition, a biological zero calibration was performed by occluding the blood flow to the foot using a manual sphygmomanometer with the cuff placed around the ankle. Minute averages for laser Doppler units (LDU) were calculated for the rewarming period starting from the end of immersion/start of rewarm (time 0). Pre-immersion SkBF was calculated as an average over 2 min during the resting period prior to immersion. SkBF during the immersion was the average value from 30 to 90 s of immersion and thus avoided any movement artefact.
Data analyses
Data were checked for normality using the Shapiro–Wilk and Kolmogorov–Smirnov normality tests. Change in rectal temperature was found to be normally distributed and differences between CON and OCC were analysed post exercise, during immersion after 5, 10 and 15 min of rewarming using a repeated measures ANOVA.
Absolute T sk, change in T sk and SkBF were analysed between conditions at the following time points: pre-immersion, immediately following immersion (0 min), the first 5 min of the rewarm and at 10 and 15 min post immersion. Change in T sk was found to be normally distributed and was analysed using a-two-way ANOVA followed by Bonferroni post hoc tests using GraphPad Prism 5.0.
SkBF and T sk were not normally distributed and were analysed with nonparametric tests using SPSS v18, PASW Statistics. Differences between the CON and OCC conditions were analysed using Friedman’s test followed by post hoc Wilcoxon tests. Differences between groups (CS and NPDM and CON/OCC) were analysed using Kruskal–Wallis test followed by Mann–Whitney U post hoc tests. Differences between SkBF and T sk within conditions at 5, 10 and 15 min of rewarming were explored using Wilcoxon tests. Data are reported as the arithmetic mean (standard deviation), the limit for statistical significance was set to P < 0.05.
Results
Rectal temperature
Following 12 min of exercise at 50 W, there was a significant increase in rectal temperature of 0.26 (0.12) °C in the CON condition and 0.22 (0.06) °C in the OCC condition (P = 0.0001). There was no significant difference in rectal temperature between the CON and OCC conditions at any time point during the testing.
Skin blood flow
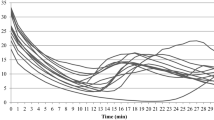
There was no significant difference in great toe SkBF between the CON and the OCC condition before or during immersion (Fig. 1). The CS group had a significantly lower pre-immersion SkBF compared to the non-cold injured controls (CON and OCC) with mean (SD) values of 59 (52) and 255 (107) LDU respectively (Fig. 1; P = 0.002). During immersion, SkBF in the CS group was lower compared to CON (P = 0.047) but not OCC. Following immersion, SkBF in the CON group rapidly returned to 104 % of resting values within the first minute of the rewarm period and was significantly higher than that seen in the CS or OCC condition [317 (135) LDU vs 93 (79) LDU; P = 0.002 and 45 (5) LDU; P = 0.016, respectively]. SkBF in CON remained significantly higher when compared to OCC (P = 0.016) and CS (P = 0.002) from 2 to 5 min, 10 to 15 min however there was no significant difference between the OCC and CS groups throughout the duration of the rewarm (Fig. 1). Within CON and OCC there was no significant change in SkBF between 5, 10 and 15 min, however in the CS group, SkBF at 15 min was increased compared to the value at 5 min [74 (50) LDU vs 121 (95) LDU P = 0.031].
Mean (SD) great toe skin blood flow during a cold sensitivity test in non-cold injured participants with (OCC) and without (CON) arterial occlusion (n = 6) and a cold sensitive group (CS; n = 6 up to 10 min, n = 5 from 11 to 15 min). Each bar represents the mean value over a 1 minute period. *Significant difference between CS and CON (P < 0.05); †significant difference between CS and OCC (P < 0.05); #significant difference between CON and OCC (P < 0.05)
Skin temperature
Pre-immersion, mean (SD) T sk of the great toe was similar in the CON and OCC condition and to the surface temperature of the NPDM at 34.7 (0.4), 34.6 (0.9) and 35.0 (0.4) °C respectively (Fig. 2). The CS group had a significantly lower T sk of 28.5 (2.1) °C (P = 0.001).
Mean (SD) great toe skin temperature during a cold sensitivity test in non-cold injured participants with (OCC) and without (CON) arterial occlusion (n = 6) and a cold sensitive group (CS; n = 6 up to 10 min, n = 5 from 11 to 15 min) and the surface temperature of NPDM (n = 2). *Significant difference between CS and CON, OCC and NPDM (P < 0.05); †significant difference between CS and CON and OCC (P < 0.05); ‡significant difference between NPDM and CON and OCC (P < 0.05); #significant difference between CON and OCC, CS and NPDM (P < 0.05)
Immediately following immersion (0 min), T sk was similar in the CON [24.8 (2.5) °C] and OCC [24.0 (1.6) °C] conditions. Compared to CON at this time point, the surface temperature of the NPDM and the T sk of the CS were significantly lower [22.1 (0.4) °C; P = 0.036 and 21.8 (0.9) °C; P = 0.002, respectively; Fig. 2].
Following 2 min of rewarming and for the remainder of the rewarming period, T sk was significantly higher in CON compared to OCC, CS and NPDM at each time point (P = 0.016, 0.001 and 0.036, respectively). The latter three groups did not differ during the rewarm period (Fig. 2).
In the CON condition, great toe T sk increased from 35.0 (0.4) °C at 5 min to 35.8 (0.3) °C at 10 min (P = 0.031), but no further increase was seen at 15 min. In the OCC condition and the CS group a gradual increase in great toe T sk was observed [OCC: 5 min = 28.0 (0.7) °C; 10 min = 28.7 (0.6) °C, P = 0.047; 15 min = 29.0 (0.6) °C, P = 0.016. CS: 5 min = 26.2 (1.1) °C; 10 min = 27.6 (1.3) °C, P = 0.016; 15 min = 29.7 (1.9) °C, P = 0.031].
To highlight any difference in the rewarming profile following the immersion, the T sk was normalised to the temperature measured immediately following immersion for each group (Fig. 3). The CS, OCC and the NPDM groups showed the same rewarming profile for the whole of the rewarm period with no significant difference between these groups at any time point. The change in T sk of CON was significantly higher than OCC from 2 to 15 min (P < 0.0001) and higher than NPDM from 3 to 15 min (P < 0.05). Compared to CS, change in T sk in CON was greater from 2 to 13 min (P < 0.05), after which it was similar (Fig. 3).
Mean (SD) change in great toe skin temperature during the rewarming phase of a cold sensitivity test in the CON and OCC conditions (n = 6) and CS group (n = 6 up to 10 min, n = 5 from 11 to 15 min) and the change in surface temperature of NPDM (n = 2). *Significant difference between CON and OCC, CS and NPDM (P < 0.05); #significant difference between CON and OCC (P < 0.05); †significant difference between CON and CS (P < 0.05)
Discussion
Since there was minimal blood flow to the limb during occlusion (Fig. 1), it can be concluded that any difference in T sk between CON and OCC was solely due to the effect of blood flow. In CON, T sk stabilised 7 °C higher than in the OCC condition (Fig. 2) demonstrating that SkBF contributes to the rewarming of the skin following a cold challenge in non-cold injured individuals.
In the CS group, starting T sk of the great toe was significantly lower than that of the non-cold injured controls (Fig. 2). T sk in the cold sensitive individuals tended to be below ambient air temperature (30 °C). Although the presence of perspiration on the skin of the feet was not noted at the time of testing, hyperhydrosis is a common, lasting symptom of NFCI (Ungley and Blackwood 1942). Therefore evaporative heat loss may have contributed to the low skin surface temperatures observed in the CS group.
The fact that individuals diagnosed with severe and moderate/severe CS show the same rewarming profile as a non-perfused model of human tissue and an occluded limb (Fig. 3) suggests that the blood flow to their injured limb was not contributing to the changes in T sk seen during rewarming. This would therefore indicate that rewarming occurred passively from the environment (30 °C) or from deeper tissues. In a more representative ambient temperature of the UK, one would anticipate that the rate of rewarming following a cold challenge would be even slower in the cold sensitive individuals, thus making them more susceptible to further cold injury.
Following a period of exercise in 30 °C air to elevate deep body temperature by approximately 0.3 °C it would be expected that an individual would be vasodilated with a relatively high SkBF. However, the CS group had a significantly lower pre-immersion SkBF in the great toe compared to that seen in CON or OCC (95, 313 and 196 LDU respectively; Fig. 1). Furthermore, SkBF in the CS group did not decrease on application of the local cold stimulus (Fig. 1). This finding could possibly indicate that the CS individuals may already be vasoconstricted prior to the cold water immersion. The response seen in the CS group was similar to that observed by Hodges et al. (2006) in participants exposed to local cooling who had been pretreated with L-NAME (a nitric oxide synthase inhibitor). Therefore the low SkBF observed in the CS group could be due to disruption of the nitric oxide pathway. In uninjured individuals treated with L-NAME, SkBF is fully restored by the infusion of a potent vasodilator and nitric oxide donor, sodium nitroprusside (Hodges et al. 2006). In addition, studies in our laboratory suggest that sublingual administration of glyceryl trinitrate (GTN) to cold-sensitive individuals improves the blood flow response and therefore rewarming following a CST (Hope 2012).
One limitation of this study was that the CS group comprised individuals from an African–Caribbean origin whereas the non-cold injured participants were mainly Caucasian. It has been previously reported that African–Caribbean individuals are at greater risk of receiving a cold injury on exposure to cold (Burgess and McFarlane 2009). The reason for this remains unclear. However, there do appear to be ethnic differences in the uninjured response to a cold challenge; with African–Americans showing lower finger T sk and fewer cold-induced vasodilatations (CIVDs) compared to their Caucasian counterparts (Iampietro et al. 1959; Jackson et al. 1989; Rennie and Adams 1957).
It is concluded that the changes in T sk observed following a CST in uninjured individuals are partially due to changes in SkBF and are not solely a result of passive rewarming of the tissues, therefore both hypotheses are accepted. The lower resting T sk and slow rewarming seen in individuals with CS may be a result of the low SkBF observed. The mechanisms behind the low resting blood flow in cold sensitive individuals are still unclear. It is possible that inhibition of basal nitric oxide production may be involved although further investigations are required.
Abbreviations
- CON:
-
Control condition
- CS:
-
Cold sensitive group
- CST:
-
Cold sensitivity test
- LDU:
-
Laser Doppler units
- NFCI:
-
Non-freezing cold injury
- NPDM:
-
Non-perfused digit model
- OCC:
-
Occluded condition
- SkBF:
-
Skin blood flow
- T sk :
-
Skin temperature
References
Burgess JE, McFarlane F (2009) Retrospective analysis of the ethnic origins of male British army soldiers with peripheral cold weather injury. J R Army Med Corps 155:11–15
Charkoudian N, Johnson JM (1999) Reflex control of cutaneous vasoconstrictor system is reset by exogenous female reproductive hormones. J Appl Physiol 87:381–385
Clark S, Dunn G, Moore T, Jayson Mt, King TA, Herrick AL (2003) Comparison of thermography and laser Doppler imaging in the assessment of Raynaud’s phenomenon. Microvasc Res 66:73–76
Edwards CM, Marshall JM, Pugh M (1998) Lack of habituation of the pattern of cardiovascular response evoked by sound in subjects with primary Raynaud’s disease. Clin Sci 95:249–260
Eglin C (2011) Cold sensitivity in windsurfers. In: Kounalakis S, Koskolou M (eds) Proceedings of the 14th international conference on environmental ergonomics. National and Kapodestrian University of Athens, Greece, pp 47–48
Eglin C, Golden F, Tipton M (2005) Increasing the reproducibility of a cold sensitivity test for non-freezing cold injury. In: Holmer I, Kuklane K, Gao C (eds) Environmental ergonomics 2005. Lund University, Ystad, pp 274–277
Francis TJ (1984) Non-freezing cold injury: a historical review. J Roy Nav Med Serv 70:134–139
Francis TJ, Oakley EH (1996) Cold Injury. In: Tooke JE, Lowe GDO (eds) A textbook of vascular medicine. Arnold, London, pp 353–370
Golden F, Eglin C, Inns R, Laight D, Martin L, Tipton M (2003) Non-freezing cold injury: its nature and assessment. Report to the MoD. University of Portsmouth, Portsmouth
Hodges GJ, Zhao K, Kosiba WA, Johnson JM (2006) The involvement of nitric oxide in the cutaneous vasoconstrictor response to local cooling in humans. J Physiol 574:849–857
Hope K (2012) The effect of glyceryl trinitrate (GTN) on response to a cold challenge in cold-exposed individuals. MSc thesis, Kings College London, London
Iampietro PF, Goldman RF, Buskirk ER, Bass DE (1959) Response of Negro and white males to cold. J Appl Physiol 14:798–800
Imray CH, Oakley EH (2005) Cold still kills: cold-related illnesses in military practice freezing and non-freezing cold injury. J R Army Med Corps 151:218–222
Imray C, Grieve A, Dhillon S (2009) Cold damage to the extremities: frostbite and non-freezing cold injuries. Postgrad Med J 85:481–488
Jackson RL, Roberts DE, Cote RA, McNeal P, Fay JT, Sharp MW, Kraus E, Rahman SA, Hamlet MP (1989) Psychological and physiological responses of Blacks and Caucasians to hand cooling. Report No. T20-89, US Army Research Institute of Environmental Medicine, Natick
King RC, Parrish JA, Allibone A (1958) Trench-foot in peacetime England. Br Med J 1:1099–1102
Laden GD, Purdy G, O’Rielly G (2007) Cold injury to a diver’s hand after a 90-min dive in 6 degrees C water. Aviat Space Environ Med 78:523–525
Marcus P (1979) “Trench foot” caused by the cold. Br Med J 1:622
Mayrovitz HN, Groseclose EE (2002) Neurovascular responses to sequential deep inspirations assessed via laser-Doppler perfusion changes in dorsal finger skin. Clin Physiol Funct Imaging 22:49–54
Mills WJ Jr, Mills WJ 3rd (1993) Peripheral non-freezing cold injury: immersion injury. Alaska Med 35:117–128
Oakley EH (1996) The long term sequelae of cold injury among the “chosen few”. Report No. 96043, Institute of Naval Medicine, Alverstoke
Oakley EH (1998) Non-freezing cold injury. In: Cold injury: diagnosis and management of the long term sequelae. Department of Veterens Affairs, Washington
Ramstead KD, Hughes RG, Webb AJ (1980) Recent cases of trench foot. Postgrad Med J 56:879–883
Rennie DW, Adams T (1957) Comparative thermoregulation responses of Negroes and white persons to acute cold stress. J Appl Physiol 11:201–204
Rodrigues LM, Pinto PC, Leal A (2001) Transcutaneous flow related variables measured in vivo: the effects of gender. BMC Dermatol 1:4
Thomas JR, Oakley EH (2001) Nonfreezing cold injury. In: Pandolf KB, Burr RE (eds) Medical aspects of harsh environments. Office of the Surgeon General, US Army, Virginia, pp 467–490
Ungley CC, Blackwood W (1942) Peripheral vasoneuropathy after chilling “immersion foot and immersion hand”. Lancet 2:447–451
Wilder-Smith E, Liu L, Thein MaMa K, Ong BK (2005) Relationship of inspiratory flow rate and volume on digit tip skin and ulnar artery vasoconstrictor responses in healthy adults. Microvasc Res 69:95–100
Williams GL, Morgan AE, Harvey JS (2005) Trench foot following a collapse: assessment of the feet is essential in the elderly. Age Ageing 34:651–652
Acknowledgments
We would like to thank all the participants who volunteered for this study and Dr Frank Golden for his advice.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Narihiko Kondo.
Rights and permissions
About this article
Cite this article
Davey, M., Eglin, C., House, J. et al. The contribution of blood flow to the skin temperature responses during a cold sensitivity test. Eur J Appl Physiol 113, 2411–2417 (2013). https://doi.org/10.1007/s00421-013-2678-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-013-2678-8