Abstract
Purpose
Few studies have examined responsiveness of bioimpedance (BIA) to detect changes over time in body composition using a longitudinal design. Accuracy of BIA and skinfold thickness in estimating body composition among 39–64 year-old women was investigated using dual-energy X-ray absorptiometry (DXA) as a criterion method both cross-sectionally and during a training intervention.
Methods
97 women had percentage of fat assessed using DXA, skinfolds and eight-polar BIA using multi-frequency current. Fat mass and lean mass were estimated by DXA and BIA. Measurements were performed before and after the 21-week training intervention.
Results
At baseline relative to DXA, BIA under predicted percentage of fat (−6.50 %) and fat mass (−3.42 kg) and overestimated lean mass (3.18 kg) considerably. Also skinfold measurement under predicted percentage of fat compared to DXA, but the difference was smaller (−1.69 % units). Skinfold measurement overestimated percentage of fat at low values and underestimated at high values (r 2 = 0.535). A significant bias was detected between DXA and BIA’s estimate of change in percentage of fat, fat mass and lean mass. Compared to DXA, BIA and skinfolds underestimated the training-induced positive changes in body composition.
Conclusions
BIA and skinfold methods compared to DXA are not interchangeable to quantify the percentage of fat, fat mass and lean mass at the cross-sectional design in middle-aged women. Moreover, exercise training-induced small changes in body composition cannot be detected with BIA or skinfold method, even though DXA was able to measure statistically significant within-group changes in body composition after training.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aging is generally associated with increased general adiposity and redistribution of body fat into visceral depot (Kuk et al. 2009; Rissanen et al. 1988). In addition, with advancing age, muscle mass declines (Frontera et al. 1991, 2000). These changes in body composition result in a decrease in functional capacity and increase risk for metabolic diseases. Physical training has been shown to improve not only physical performance but also body composition even in older individuals (Treuth et al. 1994, 1995). In terms of increasing health benefits, the primary goal of exercise interventions among middle-aged and older individuals is to maximize the loss of fat mass (FM) while preserving or increasing fat free mass (FFM). Several body composition methods have been used for estimating total and regional body composition and fat distribution, but less is known of their suitability for assessing the differential changes in body composition following endurance and strength training interventions.
Dual-energy X-ray absorptiometry (DXA) is considered to be a valid technique for total and regional fat and muscle tissue assessment and also a sensitive method for assessing small changes in body composition (Houtkooper et al. 2000; Pritchard et al. 1993). However, it must be noted that different DXA devices and software have been shown to give different estimates of body composition (Aasen et al. 2006, 2010; Genton et al. 2002; Huffman et al. 2005) and compared to MRI and 4-component method DXA has been reported to show only reasonable accuracy at the individual level (Kim et al. 2002; van der Ploeg et al. 2003). Direct measurements of lean tissue, fat tissue and bone mineral by DXA have shown high precision (2–3 % for soft tissue measurements) (Jebb et al. 1993). Other advantages are relatively fast scanning time of 10–15 min and low radiation dose. The equipment is rather expensive and due to radiation dose the measurement requires health care professional. Therefore, DXA is not widely available outside of the clinical and research settings. There is an urgent need for low cost equipment that can estimate body composition with good reliability in both cross-sectional and intervention studies.
Bioelectrical impedance method (BIA) is widely available, rapid, non-invasive, relatively inexpensive and without a requirement for high-level operator training (Malavolti et al. 2003). BIA measures resistance to an electronic current, so that the lowest resistance is observed by FFM due to the high-water content. After measuring resistance or impedance, raw values will be converted into percentage of body fat using special algorithms. Various BIA machines are supplied with proprietary prediction equations for the estimations of different body composition parameters. The details of these equations as well as the raw measurement values generated by the BIA machine are often unavailable for the users. These population-specific equations may contribute to an error in body composition measurements in different populations. BIA also is quite sensitive to hydration status, temperature, the time of the measurement, body symmetry and position (Andreoli et al. 2009). Previous validation studies of the accuracy of the BIA technique have shown contradictory results. The discordance between results may in part be due to the methodological differences such as the various devices used, and also due to the heterogeneity of the populations and rather a low number of subjects studied.
Various BIA machines have been developed over the years, and the direct segmental multi-frequency BIA analysis has been shown to have better accuracy compared to the other BIA devices (Demura et al. 2004). Even this BIA method has, however, been shown to produce mixed results in body composition estimates, especially when these machines have been validated against DXA (Beeson et al. 2010; Demura et al. 2004; Leahy et al. 2011; Ling et al. 2011; Malavolti et al. 2003). Previous studies have shown that the BIA methods provide systematically lower values for FM than, for example, DXA (Bolanowski and Nilsson. 2001; Leahy et al. 2011; Volgyi et al. 2008). Also according to some studies, the accuracy of BIA in estimating body fat is negatively affected by obesity (Leahy et al. 2011; Neovius et al. 2006; Shafer et al. 2009).
Although several studies (Beeson et al. 2010; Demura et al. 2004; Leahy et al. 2011; Ling et al. 2011; Malavolti et al. 2003; Neovius et al. 2006; Volgyi et al. 2008) have tried to cross validate different body composition devices, only a couple of studies have compared the utility of different methods to assess changes in body composition in intervention studies (Evans et al. 1999; Houtkooper et al. 2000; Mahon et al. 2007; Nelson et al. 1996). These studies have used different designs as well as different analyzing and statistical methods and subjects. The results have been rather inconsistent. For example, Nelson et al. (1996) concluded that hydrostatic weighting is superior to anthropometry, BIA and DXA to estimate changes in body FM in strength trained, older, weight-stable women. In contrast, Houtkooper et al. (2000) reported that DXA was more sensitive than hydrostatic weighing and a multicomponent model for assessing small changes in body composition in post-menopausal, weight-stable women after physical training.
Only a few studies have compared the usability of BIA, skinfolds and DXA in detecting training-induced changes in body composition. According to our knowledge, there are no studies that have investigated responsiveness of multifrequency BIA to detect changes over time using longitudinal data. Therefore, the purpose of this study was to compare Lunar Prodigy DXA and direct segmental BIA and skinfold methods to evaluate their capability to estimate training-induced changes in %FAT, FM and LM over the 21-week intervention period in 39 to 65-year-old women, who participated in the three different exercise training programs or served as controls. Based on the literature, we hypothesized that DXA is superior to bioimpedance and skinfolds to estimate changes in body composition during training.
Materials and methods
Subjects
Women (mean 51.6 ± 7.5 years, range 39–64 years) living in the Jyväskylä city region were selected as subjects. A newspaper advertisement in the local free newspaper was published. 97 volunteers who fulfilled the inclusion criteria and passed the baseline physical examination were randomly assigned, with stratification for age, BMI and menopausal status (pre- or post-menopausal), to three training groups and one control group. The project was approved by the Ethics Committee of the Central Finland Health Care District. Subjects signed a consent form before participation. This work was a part of a larger project, and detailed data on changes in aerobic and neuromuscular performance as well as changes in body composition measured by DXA have been published in detail with a smaller number of subjects (Karavirta et al. 2011; Sillanpaa et al. 2009).
Exclusion criteria
All physical or psychological diseases, which may have precluded the ability to perform the requested strength and endurance training and testing, including pronounced overweight or obesity (body mass index > 28 kg/m2), impaired glucose tolerance and diabetes, and medications known to influence physical performance or interpretation of the findings were used as exclusion criteria. Subjects with a background in moderate to high-intensity endurance or strength training more than once a week during the last year before the study were also excluded.
Study design
The female subjects were randomized into the endurance training (E, n = 24), strength training (S, n = 29), combined strength and endurance training (SE, n = 25) or control group (C, n = 19). Body composition of the subject groups presented in Table 1. The measurements for all subjects took place twice before training at weeks −1 and 0 (a control period with no experimental training) and after 21 weeks of training, but the measurements for the body composition by dual X-ray absorptiometry (DXA) and maximal cycling tests were performed only once before and after the study period. During the 21-week training period, both strength and endurance groups trained two times a week and the combined strength and endurance group trained two times a week for strength and two times a week for endurance. All training sessions were supervised. Missed training sessions were made up during subsequent training weeks so that the total amount of training sessions was reached. All subjects were instructed to continue their habitual physical activities as before. A short nutrition counseling session was provided for the training groups before the study. This session included both verbal and written instructions, which were based on the Finnish nutrition recommendations. The main purpose was to provide guidance on a healthy diet sufficient for exercise requirements. The women did not use pre- or post-workout protein or other supplements during the study.
Endurance training
The intensity of cycle training was based on the aerobic performance tests (aerobic and anaerobic threshold) and controlled by heart rate monitoring (Aunola and Rusko 1986; Hakkinen et al. 2006). Training was periodized into three training cycles and training intensity and duration was progressively increased throughout the training period. Training program has been described in detail earlier (Karavirta et al. 2011).
Strength training
The present 21-week strength training program was a total body program for the lower and upper extremities and trunk. The training program has been described in detail earlier (Sillanpaa et al. 2008). Briefly, the training period consisted of three specific training cycles of 7 weeks in duration: (1) to improve muscle strength endurance and to reduce total fat (loads of 40–60 % of 1RM), (2) to produce muscle hypertrophy to increase the total muscle mass/fat ratio (60–80 % of 1RM), and (3) to optimize gains in maximal strength of the trained muscles (70–90 % of 1RM). The individual loads of strength training were determined based of the strength tests. The supervised training sessions averaged from 60 to 90 min in length two times a week.
Measurements
Body composition
All body composition measurements were performed and analyzed by the same investigator throughout the study period. Subjects were instructed to rest at least 8 h during the previous night and to avoid strenuous exercise, alcohol consumption and sauna for 24-h. All metal items were removed from the participants to ensure the accuracy of the measurement. BIA measurements were performed in the post-absorptive state after a 12-h overnight fast and measurements were performed between 7:00 a.m. and 9:00 a.m. During the measurement subjects were in light clothing.
Dual-energy X-ray absorptiometry (DXA)
Body composition was estimated by DXA (Lunar Prodigy, GE Healthcare). The subjects were positioned supine in the center of the table. They were scanned using the default scan mode for total body scanning automatically selected by the Prodigy software. The system software (enCORE 2005, version 9.30) provides the mass of lean soft tissue, fat, and bone mineral. Body composition was analyzed using estimated FM and lean mass of soft tissue without bone (LM). Precision of the repeated measurements expressed as the percent coefficient of variation was 2.2 % for fat.
Bioelectrical impedance analysis (BIA)
Body composition was estimated by an eight-polar bioimpedance method using multifrequency current (InBody 720, Biospace Co., Seoul, Korea). The device was pre-set by the manufacturer. This device takes readings from the body using an eight-point tactile electrode method, measuring resistance at five specific frequencies (1, 50, 250, 500, and 1 MHz) and reactance at three specific frequencies (5, 50, and 250 kHz). The Inbody bioimpedance device estimates total body water using the sum of five segmental resistances, which are calculated for all frequencies (the prediction equation and its reference have not been published) (Demura et al. 2004). FFM is estimated based on the assumption that hydration of FFM is 73.2 %. FM is calculated by subtraction of FFM from total weight. Soft lean mass without bone was selected into the analysis, instead of FFM, because it is more comparable to DXA LM, which does not include bone. By BIA, LM is calculated by subtracting bone mass from FFM (Malavolti et al. 2003; Pietrobelli et al. 1996). Bone mass is predicted using predicted FFM and a special prediction equation that uses DXA bone values as a reference (detailed equations have not been published). Before the test, subjects were instructed to excrete. Body height, age and gender were entered to the device by the research personnel. During measurements, they wiped their palms and foot soles with an electrolyte cloth provided by the manufacturer. Subjects stood with the ball and heel of each foot on two metal electrodes on the floor scale and held handrails with metal grip electrodes. Arms were fully extended and abducted approximately 20° laterally. After the measurement, data were electronically imported to Excel using Lookin’Body software.
Skin folds (SF)
The fat percentage was estimated by measuring skin-fold thickness at four different sites according to Durnin and Womersley (1974). The average of three measurements was used in calculations. The same investigator made all the measurements.
Body height, weight and body mass index (BMI)
Height was measured by an inelastic plastic tape measure with the subjects standing barefoot. Body weight was measured with the calibrated electrical scale (Model 708 [d = 0.1 kg], Seca, Germany) with the subjects in their underwear. BMI was calculated by dividing weight in kilograms by the square of height in meters (kg/m2).
Physical fitness
Aerobic performance
The graded exercise test was carried out using the Monark E839 (Monark Oy, Sweden) cycle ergometer to determine maximal oxygen uptake as well as aerobic and anaerobic thresholds. Oxygen uptake was measured breath-by-breath continuously (SensorMedics® Vmax229). Maximal oxygen uptake (VO2max) was determined at the highest 1-min average of VO2 during the test (Karavirta et al. 2011).
Leg extension strength
A David 210 dynamometer (David Fitness and Medical, Outokumpu, Finland) was used to measure maximal bilateral concentric force production of the leg extensors (hip, knee, and ankle extensors) in a horizontal leg press exercise.
Statistical analyses
The changes in study variables during intervention between the groups were compared with the analysis of covariance (ANCOVA) using the baseline values (week 0) as the covariate. If necessary, the data were transformed logarithmically before ANCOVA to fulfill the criterion of normal distribution. Within-group analyses were performed with paired samples T-tests. The relationships between different variables at baseline were assessed with the Pearson’s correlation test and the relations between the changes in variables during the intervention were studied using partial correlation analysis with adjustment for group. Statistical significance was assessed at the level of p ≤0.05. Reproducibility of percentage of fat analysis by BIA and skinfolds was tested by comparing the two control period measurements (at week −1 and week 0). The reliability was assessed by one-way random model of intraclass correlation coefficient (ICC) (Weir 2005).
The Bland–Altman statistical test was used to examine bias (mean difference) and limits of agreement (±2 SD) between the two methods, and DXA was used as a criterion method. Pearson correlation coefficient was used to test if the amount of FM or LM was related to the magnitude of the change between the methods. Differences between groups in mean values of DXA and BIA and DXA and skinfolds as well as differences in the changes were tested by T-tests.
Results
At baseline, the mean leg extension strength was 98.1 ± 14.4 kg and maximal oxygen uptake 26.2 ± 5.3 ml/kg/min in the total group of subjects. The 21-week intervention period resulted in significant increases in leg extension strength in S (9.5 ± 8.6 %, p < 0.001) and SE (11.7 ± 7.2 %, p < 0.001), but not in E (between groups p < 0.001). In addition, maximal oxygen consumption (ml/kg/min) increased more both in E (20.7 ± 15.6 %, p < 0.001) and in SE (15.8 ± 10.6 %, p < 0.001) than in S (7.14 ± 16.5 %, p = 0.048) (between groups p < 0.001). There were no changes in physical performance in the control group during the 21-week intervention period. Food intake was similar in all four groups at baseline. Average energy intake (mean from weeks 0 and 21) varied between 7.0 and 7.3 MJ in all groups and did not change during intervention. There were no changes between groups in food intake during the intervention period and within-group changes were minor (data not shown).
At baseline
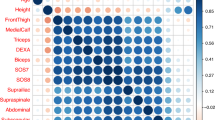
At baseline in the total group of subjects, there was a significant correlation between DXA and BIA for estimating %FAT (r = 0.917, p < 0.001), FM (r = 0.965, p < 0.001) and LM (r = 0.910, p < 0.001). Also %FAT measured by skinfolds correlated significantly with %FAT measured by DXA (r = 0.773, p < 0.001) and BIA (r = 0.802, p < 0.001). Intraclass correlation coefficient for %FAT measured by BIA and skinfolds was 0.986 and 0.993.
BIA under predicted %FAT (−6.50 %), FM (−3.42 kg) and overestimated LM (3.18 kg) relative to DXA (all p < 0.001) (Figs. 1, 2; Table 2). Also skinfold measurement under predicted %FAT compared to DXA, but the bias was smaller (−1.69 %, p < 0.001) than with BIA. The use of skinfolds resulted in systematic errors for the prediction of %FAT compared with DXA (r 2 = 0.535), with skinfold measurement overestimating %FAT at low values and underestimating at high values (Fig. 1).
The longitudinal assessment
The longitudinal assessment showed in the total group of trained subjects that changes in %FAT correlated significantly with DXA and BIA (r = 0.684, p < 0.001) and DXA and skinfolds (r = 0.526, p < 0.001). Changes in FM correlated well with DXA and BIA (r = 0.814, p < 0.001), but a weaker correlation occurred in the changes of LM (r = 0.371, p < 0.001). Significant changes in %FAT were measured by DXA and skinfolds and in FM and LM measured by DXA and in the total group of trained subjects, while BIA detected statistically significant change only in FM (Table 2). In separate groups, the mean weight loss during the intervention was significant in E and C (Table 1). %FAT measured by skinfolds decreased significantly only in the strength training group (−0.5 ± 1.3 %, p = 0.041), but with DXA in all training groups (E −1.6 ± 2.0, p = 0.001, S −1.1 ± 2.1, p = 0.010 and SE −1.9 ± 1.8, p < 0.001). BIA did not detect change in %FAT. FM decreased significantly in the endurance trained groups (E −1.3 ± 1.8 kg, p = 0.001 and SE −1.1 ± 1.4 kg, p = 0.001) as measured by DXA, but BIA did not detect any statistically significant changes. Statistically significant increases were observed in LM in the combined training group (0.8 ± 1.1 kg, p = 0.003) as measured by DXA, but not by BIA.
In the total group of trained subjects, a significant bias was detected between DXA and BIA’s estimate of change in %FAT (Fig. 3). According to the results, both BIA (bias −1.110, limits of agreement [2.122 to −4.343], p < 0.001) and skinfold method (bias −1.140, limits of agreement [2.134 to −4.415], p < 0.001) underestimated the change in %FAT and individual variations were high.
The difference between the DXA and skinfold methods in estimating changes in body composition seems to be affected slightly (r 2 = 0.251) by the amount of ∆%FAT so that skinfolds overestimated ∆%FAT at low values and underestimated ∆%FAT at high values. Compared to DXA, BIA underestimated the loss of FM (bias 0.638 kg, p < 0.001) and gains in LM (bias −0.544 kg, p < 0.001) after the intervention (Fig. 4). The limits of agreement varied between 1.597 and −2.873 in ΔFM and between 3.110 and −2.021 in ΔLM between DXA and BIA.
Discussion
The data from this study indicate that on the group basis or on the individual basis the direct segmental multi-frequency BIA and skinfold methods compared against DXA are not interchangeable to quantify the %FAT, FM and LM at the cross-sectional design in middle-aged women. Although the direct segmental BIA and skinfold correlated very well with DXA in %FAT, FM and LM analysis, BIA underestimated both %FAT and FM and overestimated LM. With skinfolds, the underestimation of %FAT was smaller, but this four point method seems to include a systematic error in the %FAT analysis. DXA was able to measure statistically significant within-group increases in LM in the combined training group, decreases in FM in the endurance trained groups and decreases in %FAT in all training groups. These training-induced small changes in body composition could not be detected with the BIA or skinfold methods.
The 21-week exercise intervention resulted in small, but statistically significant training specific adaptations in body composition. The magnitude of the increase, for example, in muscle mass depends largely on the body composition method used in the study. Previous studies have reported that high-intensity strength training interventions have resulted in 9–11 % increases muscle thickness (Alegre et al. 2006; Reeves et al. 2004; Sillanpaa et al. 2008) measured by ultrasound, 7–9 % increases in muscle cross-sectional area measured by magnetic resonance imaging or computed tomography (Ferri et al. 2003; Hakkinen et al. 2003), while increases in total body LM have been 2–3 % (Nindl et al. 2000; Sillanpaa et al. 2008) as reported also in this study. It is difficult to estimate training-induced changes in exercise interventions, thus, the method variability limits the possibility of drawing conclusions. For example, with DXA, precision of the repeated measurement expressed as the percent coefficient of variation has been 2.2 % for %FAT in our lab (Volgyi et al. 2008). Thus, the changes observed in the training groups in this study were −1.1 to −1.9 % units, corresponding 5.6 % decrease %FAT.
Bland–Altman method used in this study estimates both bias and limits of agreement between the selected standard method and other methods. However, currently there are no standard acceptable limits of agreement within body composition literature. Therefore, clinical judgment is always needed. In the present study, the small changes observed among the training groups limited the possibility to compare the methods. To detect true changes in %FAT, FM and LM, it is necessary to achieve changes in body composition that are beyond the variation of the body composition method used. The method variability of the body composition techniques must be considered when choosing a method to estimate changes in body composition in intervention studies. In the present study, reliability (ICC) of BIA and skinfold methods in %FAT estimations was high.
Several studies have compared body composition assessed by segmental multi-frequency BIA (Inbody) and different DXA machines in a cross-sectional design (Demura et al. 2004; Ling et al. 2011; Malavolti et al. 2003; Volgyi et al. 2008) and reported conflicting results. Both Völgyi et al. (2008) and Shafer et al. (2009) observed gender and obesity degree-related differences between these methods in a large sample of middle-aged adults. According to Shafer et al. (2009), BIA seems to underestimate %FAT in normal weight subjects and overestimate %FAT in overweight and obese subjects. Volgyi et al. (2008) reported, similarly as we did, that BIA systematically underestimated %FAT compared to DXA and the underestimation is at its largest in normal weight subjects. Völgyi et al. used the same DXA (Lunar Prodigy) device as we did in this study.
Recently, Ling et al. (2011) reported good agreement with Hologic QDR 4500 DXA and Inbody 720 BIA in a large sample of middle-aged participants. They found that BIA is a valid tool especially in LM assessments. Our results, which showed underestimation of FM and overestimation of LM, are different. In the study of Ling et al. (2011), BIA measurements were not performed in fasting conditions, which may affect the results. It is also clear that even though DXA is widely used in body composition analysis, differences between the Inbody and DXA validation studies may also be related to differences between the DXA devices and softwares, which has been reported several times (Aasen et al. 2006; Genton et al. 2002; Huffman et al. 2005). The validity of DXA in body composition analysis has also been challenged by some studies reporting low agreement of DXA at the individual level compared to four component model measurements (van der Ploeg et al. 2003) and air-displacement plethysmography (Fields et al. 2002).
Our results from the cross-sectional analysis agrees with previous studies showing also strong relative correlations between BIA and DXA for the assessment of %FAT, FM and LM, but a significant underestimation of FM and overestimation of LM by BIA (Frisard et al. 2005; Sillanpaa et al. 2008), and suggests that application of BIA for the absolute parameters for body composition may be limited due to the systematic error. The original Inbody validation studies were also performed with Korean population, and it is possible that scale difference at the group level results from differences between Korean and Caucasian population in body composition. In addition, at the individual level, quite large limits of agreement were observed by BIA in the %FAT analysis compared to DXA. With skinfolds, the bias compared to DXA was smaller than with BIA, but limits of agreement were wider. The skinfold method seems also to include a systematic error in %FAT analysis.
The primary purpose of this study was to investigate the utility of BIA and skinfolds for assessing changes in body composition during exercise interventions. Small training-induced reductions in %FAT in all training groups were tracked only by DXA and in the strength training group only by skinfolds. BIA did not detect any changes in %FAT at the group level. Moreover, statistically significant decreases in FM in the endurance trained groups and increases in LM in the combined training group were tracked only by the DXA method. With the skinfold method, the similar systematic error seems also to be present among changes during training than with the cross-sectional estimation of %FAT.
Other studies that have compared the ability of different methods to detect weight loss induced reductions in body fat and %FAT have concluded that different BIA machines are sensitive enough to detect changes in body composition (Frisard et al. 2005; Thomson et al. 2007). The magnitude of weight loss may influence the accuracy of BIA to assess changes in body composition (Frisard et al. 2005). Based on the results of the present study, it seems that BIA is not suitable for detecting the small changes in %FAT. This method seems to be rather weak, when the intervention includes concurrent small increases in LM and decreases in FM.
Men and women follow a different pattern of body composition, and significant gender-related differences in %FAT, FM and LM have been shown. Moreover, body fat is distributed in a different manner between men and women, and genders may also differ in training-responses. According to some studies, men are more prone to lose abdominal fat during training interventions. We have earlier measured middle-aged men during a similar intervention by DXA and BIA (Sillanpaa et al. 2008). The results from the present study are comparable with these earlier findings. Also in men baseline percent body fat values measured by BIA were systematically lower than those measured by DXA, on average 6.4 %, although a high correlation existed between these methods (r = 0.90). Also Bolanowski and Nilsson (2001) have reported a similar systematic difference in percentage of fat analysis between DXA and BIA. The correlations between %FAT changes were also much weaker in men compared to correlations observed in women in the current study.
Standardized practices were followed in this study to avoid confounding effects of hydration status, acute exercise and medications. Moreover, we tried to minimize the measurement error in the skinfold measurement by marking the anatomical measurement places with tattoo points. The same instructions, time of day, investigator, measurement technique and calibrated measurement equipment were always used to study changes in all the outcome variables of body composition. Also the data analysis of different variables was performed by the same investigator, equipment and technique pre- and post-training. The subjects were selected using the convenience sampling (i.e. sampling of volunteers) and strict inclusion and exclusion criteria used in this study compound the selection bias even more (Sousa et al. 2004). The criteria were, however, essential to confirm that healthy, non-obese and well-motivated subjects were selected as subjects due to the nature of the intervention. Therefore, our results can be generalized only to healthy, non-obese middle-aged women. In this study %FAT, FM and LM were estimated using the manufacturer’s instructions and equations with multi-frequency current when using the BIA device. We were not able to estimate how the equation effects on the estimation of body composition.
Both BIA and skinfold correlate well with DXA in the %FAT analysis. Multi-frequency BIA, however, underestimates %FAT and FM and overestimates LM in middle-aged women at the cross-sectional analysis and these methods cannot be used interchangeably. In contrast, the skinfold method seems to have a systematic error in estimation of body fat compared to DXA. Only DXA was able to detect small training-induced changes in LM and FM during the 21-week intervention even in middle-aged weight-stable women. We conclude that BIA and skinfolds technique need more development before they can be used in research purposes in longitudinal designs.
References
Aasen G, Fagertun H, Halse J (2006) Body composition analysis by dual X-ray absorptiometry: in vivo and in vitro comparison of three different fan-beam instruments. Scand J Clin Lab Invest 66:659–666
Aasen G, Fagertun H, Halse J (2010) Effect of loss of regional fat assessed by DXA on insulin resistance and dyslipidemia in obese men. Scand J Clin Lab Invest 70:547–553
Alegre LM, Jimenez F, Gonzalo-Orden JM, Martin-Acero R, Aguado X (2006) Effects of dynamic resistance training on fascicle length and isometric strength. J Sports Sci 24:501–508
Andreoli A, Scalzo G, Masala S, Tarantino U, Guglielmi G (2009) Body composition assessment by dual-energy X-ray absorptiometry (DXA). Radiol Med 114:286–300
Aunola S, Rusko H (1986) Aerobic and anaerobic thresholds determined from venous lactate or from ventilation and gas exchange in relation to muscle fiber composition. Int J Sports Med 7:161–166
Beeson WL, Batech M, Schultz E et al (2010) Comparison of body composition by bioelectrical impedance analysis and dual-energy X-ray absorptiometry in Hispanic diabetics. Int J Body Compos Res 8:45–50
Bolanowski M, Nilsson BE (2001) Assessment of human body composition using dual-energy X-ray absorptiometry and bioelectrical impedance analysis. Med Sci Monit 7:1029–1033
Demura S, Sato S, Kitabayashi T (2004) Percentage of total body fat as estimated by three automatic bioelectrical impedance analyzers. J Physiol Anthropol Appl Human Sci 23:93–99
Durnin JV, Womersley J (1974) Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr 32:77–97
Evans EM, Saunders MJ, Spano MA, Arngrimsson SA, Lewis RD, Cureton KJ (1999) Body-composition changes with diet and exercise in obese women: a comparison of estimates from clinical methods and a 4-component model. Am J Clin Nutr 70:5–12
Ferri A, Scaglioni G, Pousson M, Capodaglio P, Van Hoecke J, Narici MV (2003) Strength and power changes of the human plantar flexors and knee extensors in response to resistance training in old age. Acta Physiol Scand 177:69–78
Fields DA, Goran MI, McCrory MA (2002) Body-composition assessment via air-displacement plethysmography in adults and children: a review. Am J Clin Nutr 75:453–467
Frisard MI, Greenway FL, Delany JP (2005) Comparison of methods to assess body composition changes during a period of weight loss. Obes Res 13:845–854
Frontera WR, Hughes VA, Lutz KJ, Evans WJ (1991) A cross-sectional study of muscle strength and mass in 45- to 78-year-old men and women. J Appl Physiol 71:644–650
Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ, Roubenoff R (2000) Aging of skeletal muscle: a 12-year longitudinal study. J Appl Physiol 88:1321–1326
Genton L, Hans D, Kyle UG, Pichard C (2002) Dual-energy X-ray absorptiometry and body composition: differences between devices and comparison with reference methods. Nutrition 18:66–70
Hakkinen K, Alen M, Kraemer WJ et al (2003) Neuromuscular adaptations during concurrent strength and endurance training versus strength training. Eur J Appl Physiol 89:42–52
Hakkinen A, Holopainen E, Kautiainen H, Sillanpaa E, Hakkinen K (2006) Neuromuscular function and balance of prepubertal and pubertal blind and sighted boys. Acta Paediatr 95:1277–1283
Houtkooper LB, Going SB, Sproul J, Blew RM, Lohman TG (2000) Comparison of methods for assessing body-composition changes over 1 y in postmenopausal women. Am J Clin Nutr 72:401–406
Huffman DM, Landy NM, Potter E, Nagy TR, Gower BA (2005) Comparison of the Lunar DPX-L and Prodigy dual-energy X-ray absorptiometers for assessing total and regional body composition. Int J Body Compos Res 3:25–30
Jebb SA, Goldberg GR, Elia M (1993) DXA measurements of fat and bone mineral density in relation to depth and adiposity. Basic Life Sci 60:115–119
Karavirta L, Hakkinen A, Sillanpaa E et al (2011) Effects of combined endurance and strength training on muscle strength, power and hypertrophy in 40–67-year-old men. Scand J Med Sci Sports 21:402–411
Kim J, Wang Z, Heymsfield SB, Baumgartner RN, Gallagher D (2002) Total-body skeletal muscle mass: estimation by a new dual-energy X-ray absorptiometry method. Am J Clin Nutr 76:378–383
Kuk JL, Saunders TJ, Davidson LE, Ross R (2009) Age-related changes in total and regional fat distribution. Ageing Res Rev 8:339–348
Leahy S, O’Neill C, Sohun R, Jakeman P (2011) A comparison of dual energy X-ray absorptiometry and bioelectrical impedance analysis to measure total and segmental body composition in healthy young adults. Eur J Appl Physiol 112:589–595
Ling CH, de Craen AJ, Slagboom PE et al (2011) Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr 30:610–615
Mahon AK, Flynn MG, Iglay HB et al (2007) Measurement of body composition changes with weight loss in postmenopausal women: comparison of methods. J Nutr Health Aging 11:203–213
Malavolti M, Mussi C, Poli M et al (2003) Cross-calibration of eight-polar bioelectrical impedance analysis versus dual-energy X-ray absorptiometry for the assessment of total and appendicular body composition in healthy subjects aged 21–82 years. Ann Hum Biol 30:380–391
Nelson ME, Fiatarone MA, Layne JE et al (1996) Analysis of body-composition techniques and models for detecting change in soft tissue with strength training. Am J Clin Nutr 63:678–686
Neovius M, Hemmingsson E, Freyschuss B, Udden J (2006) Bioelectrical impedance underestimates total and truncal fatness in abdominally obese women. Obesity (Silver Spring) 14:1731–1738
Nindl BC, Harman EA, Marx JO et al (2000) Regional body composition changes in women after 6 months of periodized physical training. J Appl Physiol 88:2251–2259
Pietrobelli A, Formica C, Wang Z, Heymsfield SB (1996) Dual-energy X-ray absorptiometry body composition model: review of physical concepts. Am J Physiol 271:E941–E951
Pritchard JE, Nowson CA, Strauss BJ, Carlson JS, Kaymakci B, Wark JD (1993) Evaluation of dual energy X-ray absorptiometry as a method of measurement of body fat. Eur J Clin Nutr 47:216–228
Reeves ND, Narici MV, Maganaris CN (2004) In vivo human muscle structure and function: adaptations to resistance training in old age. Exp Physiol 89:675–689
Rissanen A, Heliovaara M, Aromaa A (1988) Overweight and anthropometric changes in adulthood: a prospective study of 17,000 Finns. Int J Obes 12:391–401
Shafer KJ, Siders WA, Johnson LK, Lukaski HC (2009) Validity of segmental multiple-frequency bioelectrical impedance analysis to estimate body composition of adults across a range of body mass indexes. Nutrition 25:25–32
Sillanpaa E, Hakkinen A, Nyman K et al (2008) Body composition and fitness during strength and/or endurance training in older men. Med Sci Sports Exerc 40:950–958
Sillanpaa E, Laaksonen DE, Hakkinen A et al (2009) Body composition, fitness, and metabolic health during strength and endurance training and their combination in middle-aged and older women. Eur J Appl Physiol 106:285–296
Sousa VD, Zauszniewski JA, Musil CM (2004) How to determine whether a convenience sample represents the population. Appl Nurs Res 17:130–133
Thomson R, Brinkworth GD, Buckley JD, Noakes M, Clifton PM (2007) Good agreement between bioelectrical impedance and dual-energy X-ray absorptiometry for estimating changes in body composition during weight loss in overweight young women. Clin Nutr 26:771–777
Treuth MS, Ryan AS, Pratley RE et al (1994) Effects of strength training on total and regional body composition in older men. J Appl Physiol 77:614–620
Treuth MS, Hunter GR, Kekes-Szabo T, Weinsier RL, Goran MI, Berland L (1995) Reduction in intra-abdominal adipose tissue after strength training in older women. J Appl Physiol 78:1425–1431
van der Ploeg GE, Withers RT, Laforgia J (2003) Percent body fat via DEXA: comparison with a four-compartment model. J Appl Physiol 94:499–506
Volgyi E, Tylavsky FA, Lyytikainen A, Suominen H, Alen M, Cheng S (2008) Assessing body composition with DXA and bioimpedance: effects of obesity, physical activity, and age. Obesity (Silver Spring) 16:700–705
Weir JP (2005) Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res 19:231–240
Acknowledgments
This study was partly supported by a grant from the Ministry of Education, Finland, the Central Finland Health Care District, Jyväskylä Finland, Juho Vainio Foundation, Finland, Sport Institute Foundation, Finland and Yrjö Jahnsson Foundation, Finland.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Klaas R Westerterp.
Rights and permissions
About this article
Cite this article
Sillanpää, E., Häkkinen, A. & Häkkinen, K. Body composition changes by DXA, BIA and skinfolds during exercise training in women. Eur J Appl Physiol 113, 2331–2341 (2013). https://doi.org/10.1007/s00421-013-2669-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-013-2669-9