Abstract
The purpose of this investigation was to determine the influence of heat stress on the dynamics of muscle metabolic perturbation during high-intensity exercise. Seven healthy males completed single-legged knee-extensor exercise until the limit of tolerance on two separate occasions. In a randomized order the subjects underwent 40 min of lower-body immersion in warm water at 42°C prior to exercise (HOT) or received no prior thermal manipulation (CON). Following the intervention, muscle metabolism was measured at rest and throughout exercise using 31P-MRS. The tolerable duration of high-intensity exercise was reduced by 36% after passive heating (CON: 474 ± 146 vs. HOT: 303 ± 76 s; P = 0.005). Intramuscular pH was lower over the first 60 s of exercise (CON: 7.05 ± 0.02 vs. HOT: 7.00 ± 0.03; P = 0.019) in HOT compared to CON. The rate of muscle [PCr] degradation during exercise was greater in the HOT condition (CON: −0.17 ± 0.08 vs. HOT: −0.25 ± 0.10% s−1; P = 0.006) and pH also tended to change more rapidly in HOT (P = 0.09). Muscle [PCr] (CON: 26 ± 14 vs. HOT: 29 ± 10%), [Pi] (CON: 504 ± 236 vs. HOT: 486 ± 186%) and pH (CON: 6.84 ± 0.13 vs. HOT: 6.80 ± 0.14; P > 0.05) were not statistically different at the limit of tolerance (P > 0.05 for all comparisons). These results suggest that the reduced time-to-exhaustion during high-intensity knee-extensor exercise following lower-body heating might be related, in part, to accelerated rates of change of intramuscular [PCr] and pH towards ‘critical’ values that limit muscle function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human thermoregulatory system maintains core temperature within a narrow range under basal conditions. During sub-maximal exercise, defined as a work rate that does not elicit the maximum oxygen uptake (\( {\dot{V}}{{{\text{O}}_{{2{ \max }}} }} \)), muscle and core temperatures are elevated but stabilize at sub-maximal values (González-Alonso et al. 1999; Nybo and Nielsen 2001a, b; Nybo et al. 2002a, b). In contrast, during maximal exercise, body temperature continues to increase until the limit of tolerance (Febbraio et al. 1996; Ferguson et al. 2006; Nybo et al. 2001). Superimposition of thermal stress results in a more rapid increase in muscle (Febbraio et al. 1996; Ferguson et al. 2006) and core (Nybo and Nielsen 2001a, b; Nybo et al. 2001, 2002a, b) temperature and is accompanied by more rapid muscle fatigue development (Nybo and Nielsen 2001b) and reduced exercise tolerance (Parkin et al. 1999). Raising the muscle and/or core temperature prior to exercise has also been shown to accelerate the development of muscle fatigue (Edwards et al. 1972; González-Alonso and Calbet 2003; González-Alonso et al. 1999; Morrison et al. 2004; Nybo et al. 2001), whereas pre-cooling improves exercise tolerance (e.g., González-Alonso et al. 1999). Therefore, the rate of body heat accumulation has important implications for the development of muscle fatigue and exercise performance.
Muscle fatigue is a complex multi-faceted phenomenon that comprises central (Gandevia 2001) and peripheral (Allen et al. 2008; Jones et al. 2008) components. It is well documented that skeletal muscle blood flow may be reduced during exercise in the heat (e.g., González-Alonso and Calbet 2003; see González-Alonso et al. 2008 for review). However, during sub-maximal exercise, the reduction in muscle blood flow can be compensated by dehydration-induced haemoconcentration and increased muscle O2 extraction such that \( {\dot{V}}{{\text{O}}_{2} } \) is similar in hyperthermia compared to normothermia (González-Alonso et al. 1998). Consequently, intramuscular concentrations of adenosine triphosphate ([ATP]), phosphocreatine ([PCr]) and lactate may not be significantly altered by a period of sub-maximal exercise with an elevated muscle temperature (Starkie et al. 1999). A higher skeletal muscle [glycogen] has been reported at exhaustion during sustained sub-maximal exercise in the heat (Febbraio 2000). Therefore, peripheral fatigue components may not be responsible for the greater fatigue observed during prolonged sub-maximal exercise with hyperthermia. Instead, the existing literature indicates that fatigue in these conditions may be predominantly of central origin since hyperthermia has been shown to reduce cerebral blood flow (Nybo et al. 2002a), brain heat removal (Nybo et al. 2002b), and voluntary muscle activation and handgrip MVC force following 50 min bicycling exercise at 40°C (Nybo and Nielsen 2001b).
While it is clear that central fatigue contributes to exercise intolerance during prolonged sub-maximal exercise in hyperthermia, peripheral fatigue may be more important at higher exercise intensities (González-Alonso and Calbet 2003; Nybo et al. 2001). During maximal exercise in the heat, the reduction in muscle blood flow cannot be compensated by increased muscle O2 extraction (González-Alonso and Calbet 2003) and, as a result, \( {\dot{V}}{\text{O}_{2}} \) kinetics is slower (Nybo et al. 2001) and \( {\dot{V}}{\text{O}_{2 \max}} \) is reduced (González-Alonso and Calbet 2003). These reductions in oxidative energy yield mandate an increased rate of ATP resynthesis from substrate level phosphorylation and an increased muscle metabolic perturbation, as evidenced by elevated rates of PCr degradation and intramuscular lactate accumulation (Febbraio et al. 1996; González-Alonso and Calbet 2003), as well as a reduction in intramuscular [ATP] (González-Alonso and Calbet 2003) and [glycogen] (Febbraio et al. 1996). Collectively, these data suggest that peripheral mechanisms may make a greater contribution to fatigue development during high-intensity exercise in the heat.
Only a limited number of studies have investigated muscle metabolism during maximal exercise in hyperthermic humans (Febbraio et al. 1996; Ferguson et al. 2006; González-Alonso and Calbet 2003), and we are not aware of any investigations that have characterized the dynamics of the changes in muscle metabolism during exercise performed with and without prior heating. In this regard, 31phosphorus magnetic resonance spectroscopy (31P-MRS) affords several advantages not least that it permits non-invasive measurements of a number of muscle substrates and metabolites that have been associated with the fatigue process (i.e., [ATP], [PCr], [Pi], pH) with a high temporal resolution. The available literature is equivocal over the effects of hyperthermia on muscle metabolism with some studies reporting that muscle metabolic perturbation was greater with elevated thermal stress (Febbraio et al. 1996; González-Alonso and Calbet 2003) and another suggesting no significant difference compared to normothermia (Ferguson et al. 2006). Only in the study of González-Alonso and Calbet (2003) was exercise continued until exhaustion to elucidate how the metabolic changes observed in hyperthermia might impact on exercise tolerance.
We investigated whether the reduced exercise tolerance commonly reported with elevated heat stress during high-intensity exercise is related to muscle metabolic factors. Knee-extensor muscle metabolism was measured using 31P-MRS with and without passive pre-exercise lower-body heating. We hypothesized that pre-exercise heating would reduce the tolerable duration of high-intensity exercise. We also hypothesized that the rate of muscle metabolic perturbation would be accelerated (i.e., there would be faster reductions in muscle [PCr] and pH and a more rapid increase in muscle [Pi]) such that the same ‘limiting’ metabolic milieu (Hogan et al. 1999; Vanhatalo et al. 2010) would be more rapidly attained after passive heating.
Methods
Subjects
Seven healthy, recreationally active males (mean ± SD, age 33 ± 5 year, height 1.80 ± 0.02 m, body mass 81 ± 7 kg) volunteered to participate in this study. None of the subjects were tobacco smokers or users of dietary supplements. The procedures employed in this study were approved by the Institutional Research Ethics Committee. All subjects gave their written informed consent prior to the commencement of the study, after the experimental procedures, associated risks, and potential benefits of participation had been explained. Subjects were instructed to arrive at the laboratory in a rested and fully hydrated state, at least 3 h postprandial, and to avoid strenuous exercise in the 24 h preceding each testing session. Each subject was also asked to refrain from caffeine and alcohol consumption 6 and 24 h before each test, respectively. All tests were performed at the same time of day (±2 h).
Experimental protocol
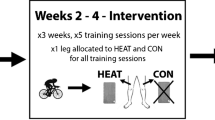
Following familiarization, subjects were required to report to the laboratory on two occasions, separated by at least 48 h, to complete the experimental testing. During these laboratory visits, participants completed single-legged knee-extensor exercise in the prone body position. The exercise tests were continued until the limit of tolerance. All participants were familiar with these exercise testing procedures having previously participated in similar studies in our laboratory. Using prior knowledge of the work rate/time-to-exhaustion relationship from these previous investigations (Jones et al. 2008; Vanhatalo et al. 2010), a high-intensity work rate was selected to bring the subjects to exhaustion in approximately 480 s. These exhaustive exercise tests were performed at an ambient temperature of ~27°C with (HOT) and without (CON) passive lower-body heating prior to exercise. Subjects exercised at the same absolute work rate in the HOT and CON conditions. The HOT and CON protocols were administered in a randomized order as part of a cross-over experimental design. Passive heating was induced by immersing the subject in a bath of warm water such that the water level intersected the iliac crest. The temperature of the water was held constant at 42°C and the subjects sat in the bath for a 40-min period to increase muscle temperature. In a previous study conducted in our laboratory, this passive heating protocol increased muscle temperature (measured with a needle thermistor) by 2.6°C and core temperature (measured with a rectal thermometer) by 0.6°C (Burnley et al. 2002). In the CON condition, the subjects sat quietly for 40 min in a thermoneutral environment (21°C).
Immediately following the HOT and CON pre-exercise interventions, subjects were positioned inside a whole-body magnetic resonance imaging system in the prone body position. A 6 cm 31P transmit/receive surface coil was placed within the bed and the subject was asked to lie upon it such that the coil was centred over the quadriceps muscle of the right leg. Subjects were then secured to the ergometer bed with Velcro straps at the thigh, buttocks and lower back to minimize extraneous movement during the protocol. The ergometer consisted of a nylon frame that fitted onto the bed in alignment with the subject’s feet and a base unit that was positioned behind the bed. The right foot was connected to a pulley system which permitted a nonmagnetic weight to be lifted and lowered. Knee-extensor exercise was performed at a rate of 40 repetitions per minute with the subjects lifting and lowering the mass over a distance of ~0.22 m in accordance with a visual cue projected onto the front wall of the scanner room. Exercise commenced 5 min after subjects entered the scanner room. The contraction phase of the knee extensors and the interrogation of the quadriceps by 31P-MRS were synchronized. When subjects were unable to sustain the required contraction frequency, the tolerable duration of exercise was recorded.
Magnetic resonance spectroscopy measurements
31P-MRS was performed in the Peninsula Magnetic Resonance Research Centre, Exeter, using a 1.5-T superconducting magnetic resonance scanner (Intera, Philips, Eindhoven, The Netherlands) for the determination of in vivo skeletal muscle metabolism. A number of pre-acquisition steps were carried out to optimize the signal from the muscle under investigation. Matching and tuning of the coil was performed and an automatic shimming protocol was then undertaken within a volume that defined the quadriceps muscle. To ensure that the examined muscle was consistently at the same point relative to the coil during exercise, the subject was visually queued via a display consisting of two vertical bars, one which moved at a constant rate with a frequency of 0.67 Hz and one which monitored foot movement via a sensor present within the pulley to which they were connected. The subject endeavored to match the movements of these two bars. The work done by the subject was recorded via a nonmagnetic strain gauge present within the pulley mechanism, enabling work rate to be calculated.
Prior to and during the exercise, data were acquired every 1.5 s, with a spectral width of 1,500 Hz, and 1,000 data points. Phase cycling with four phase cycles was employed, leading to a spectrum being acquired every 6 s. The subsequent spectra were quantified via peak fitting, assuming prior knowledge, using the jMRUI (version 2) software package employing the AMARES fitting algorithm (Vanhamme et al. 1997). Spectra were fitted assuming the presence of the following peaks: Pi, phosphodiester, PCr, α-ATP (two peaks, amplitude ratio 1:1), γ-ATP (two peaks, amplitude ratio 1:1) and β-ATP (three peaks, amplitude ratio 1:2:1). In all cases, relative amplitudes recorded during exercise were corrected for partial saturation by obtaining a baseline spectrum before exercise with long repetition time (TR = 20 s) in which the relative unsaturated peak amplitudes could be determined. Intracellular pH was calculated using the chemical shift of the Pi spectral peak relative to the PCr peak (Taylor et al. 1983).
Resting and end-exercise (at the limit of tolerance) values of [PCr], [Pi] and pH were calculated over the last 60 and 30 s of the rest or exercise period, respectively. [PCr] and [Pi] were expressed as a percentage of the resting baseline values. The mean [PCr], [Pi] and pH values were also calculated for 30 s windows surrounding 60, 120 and 180 s of exercise. The rate of change of muscle [PCr] was calculated as the difference between the [PCr] reported at the limit of tolerance and at baseline divided by the time to the limit of tolerance (Tlim); [Pi] and pH dynamics were calculated in a similar fashion.
Statistics
Differences in the muscle metabolic variables and exercise tolerance between HOT and CON were analyzed with two-tailed, paired-samples t tests. Relationships between variables were assessed using Pearson’s product moment correlation coefficient. Data are presented as mean ± SD, unless otherwise stated. Statistical significance was accepted when P < 0.05.
Results
All subjects were able to tolerate the 40-min period of warm water immersion. The work rate administered in both the CON and HOT conditions was 21 ± 3 W.
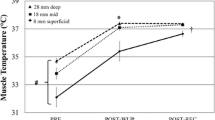
Muscle metabolic responses to CON and HOT are presented in Table 1 and illustrated in Fig. 1. The tolerable duration of high-intensity exercise was reduced by 36% in the HOT condition (CON: 474 ± 146 vs. HOT: 303 ± 76 s; P = 0.005; paired-samples 95% confidence interval 73, 268) and this is illustrated in Fig. 2.
Muscle metabolic responses to high-intensity exercise in the CON and HOT conditions in a representative individual. The change in muscle [PCr] (a), [Pi] (b), and pH (c) are illustrated. Note that muscle [PCr], [Pi] and pH are similar at the limit of tolerance but attain these critical values earlier in the HOT condition
Group mean ± SEM time-to-exhaustion during high-intensity exercise in the CON and HOT conditions. The mean ± SEM response in CON is presented as the open bar and the HOT response as the filled bar. Individual changes in the tolerance of severe exercise between the two experimental conditions are shown as dashed lines. Note that exercise tolerance was reduced in all seven participants in the HOT condition
Intramuscular [PCr] was not significantly different between the HOT and CON conditions at 60, 120, or 180 s of exercise and was also not different at the limit of tolerance (Table 1; Fig. 1). While there was a trend for an increased [Pi] at 60 s in the HOT condition (P = 0.06), the [Pi] was not significantly different at 120, 180 s or at the limit of tolerance (Table 1; Fig. 1). Intramuscular pH, on the other hand, was significantly lower at baseline and at 60 s of exercise and also tended to be lower at 120 s in HOT. There was no significant difference in muscle pH at 180 s or at the limit of tolerance between the experimental conditions (Table 1; Fig. 1). The intramuscular [Pi]/[PCr] ratio was not significantly different between the HOT and CON conditions at any time during exercise (P > 0.05; data not shown).
Although there were only limited differences between conditions in absolute [PCr], [Pi] and pH when discrete time points within the first 180 s of exercise were compared, it was apparent that, when the entire exercise bout was considered, these variables changed more rapidly over time in HOT (Fig. 1). The rate of muscle [PCr] degradation was 45% greater in HOT compared to CON (CON: −0.17 ± 0.08 vs. HOT: −0.25 ± 0.10% s−1; P = 0.006; paired-samples 95% confidence interval 0.033, 0.127). Moreover, muscle [Pi] accumulated 38% more rapidly (CON: 0.99 ± 0.68 vs. HOT: 1.37 ± 0.88% s−1) and pH declined 45% more rapidly (CON: −0.03 ± 0.02 vs. HOT: −0.05 ± 0.04 pH units·min−1) in the HOT condition; however, these differences in the rates of change of [Pi] and pH did not attain statistical significance (P = 0.23 for [Pi] and P = 0.09 for pH).
Discussion
This study used 31P-MRS to investigate, for the first time, the influence of heat stress on the dynamics of muscle metabolic perturbation in humans performing high-intensity knee-extensor exercise. At the limit of tolerance, intramuscular [PCr], [Pi] and pH were not significantly different between the experimental conditions, suggesting that the tolerable duration of exercise coincided with the attainment of a critical intramuscular metabolic environment. However, consistent with our experimental hypotheses, these critical metabolite levels were more rapidly attained in the HOT condition and high-intensity exercise tolerance was reduced accordingly. Therefore, these data suggest that the reduced high-intensity exercise tolerance reported in conditions of heat stress can be explained, at least in part, by the more rapid attainment of an intramuscular metabolic environment that predisposes to impaired muscle function (i.e., low [PCr] and pH and high [Pi]).
We employed a pre-exercise heating protocol that has been shown to increase both core and muscle temperature (Burnley et al. 2002). Similar passive heating protocols have also resulted in increased core (González-Alonso et al. 1999; Gray et al. 2006, 2008) and/or muscle (Edwards et al. 1972; Febbraio et al. 1996; Ferguson et al. 2006; Gray et al. 2006, 2008; Starkie et al. 1999) temperature. The influence of increased heat stress on muscle oxidative metabolism during high-intensity exercise is unclear. Pre-exercise heating, using a water-perfused jacket that contacted the skin of the trunk and lower arms, has been shown to reduce muscle blood flow and \( {\dot{V}}{{{\text{O}}_{{2{ \max }}} }} \) during upright bicycling exercise (González-Alonso and Calbet 2003). In contrast, thigh blood flow, muscle \( {\dot{V}}{{\text{O}}_{2}} \) and aerobic ATP production were not significantly altered following passive heating during one-legged knee-extensor exercise (Ferguson et al. 2006). The extent to which pre-exercise heating impacts on oxidative metabolism therefore appears to be dependent on the volume of muscle mass engaged and, thus, the competition for the available blood flow.
The reaction kinetics of key metabolic enzymes including creatine kinase (Wyss et al. 1990) and phosphofructokinase (Pettigrew and Frieden 1979) may be optimized at elevated temperatures, facilitating a greater anaerobic ATP yield. Indeed, PCr hydrolysis (Edwards et al. 1972; Febbraio et al. 1994b; González-Alonso and Calbet 2003; Gray et al. 2006, 2008) and anaerobic glycolysis (Drust et al. 2005; Edwards et al. 1972; Febbraio et al. 1994b; González-Alonso and Calbet 2003; Gray et al. 2006, 2008) are augmented during intense exercise under conditions of increased thermal stress. Consistent with these observations, pre-exercise heating accelerated muscle PCr degradation and H+ accumulation during high-intensity exercise in the present investigation. This shift towards greater anaerobic metabolism was not observed in a study by Ferguson and colleagues (2006). The reason for this discrepancy is unclear but may be related to methodological differences between the experiments, including a different pre-exercise heating protocol and a different muscle contraction frequency.
Several investigations have reported a greater reduction in muscle [glycogen] (Febbraio et al. 1994a, b, 1996; Starkie et al. 1999) and a greater increase in muscle [lactate] (Febbraio et al. 1994a, b, 1996; González-Alonso and Calbet 2003; Parkin et al. 1999) and other glycolytic intermediates (Edwards et al. 1972) when muscle temperature is elevated. However, the only available information on temperature effects on muscle pH is related to all-out sprint exercise (King et al. 1985; Mohr et al. 2006). Therefore, the underlying mechanisms responsible for the small reduction in muscle pH in the HOT condition in the present study are obscure. Thermal stress may have augmented signaling for glycolytic flux via: an increased accumulation of products of adenine nucleotide metabolism, catecholaminergic stimulation, or a Q10 effect (Febbraio 2000). However, Febbraio et al. (1996) reported that the derivatives of adenine nucleotide metabolism were not significantly altered in the m. vastus lateralis at rest following passive heating. Moreover, glycolytic energy production can be enhanced in the absence of changes in adrenaline and noradrenaline after passive heating (Febbraio et al. 1996; Starkie et al. 1999) which suggests that the temperature-induced elevation in glycolytic flux is not necessarily sympathetically mediated. Therefore, a temperature-induced speeding of key glycolytic enzyme activity via a Q10 effect (e.g., phosphofructokinase; Pettigrew and Frieden 1979) might have contributed to the lower muscle pH at baseline and during exercise in the current study. Another possibility is that raising muscle temperature impeded H+ efflux from the muscle. H+ clearance through the Na+–H+ exchanger has been shown to decline in mammalian ventricular myocytes at higher temperatures (Ch’en et al. 2003), but to what extent heat stress influences the activity of the Na+–H+ exchanger and the lactate–H+ co-transporter in human skeletal muscle is unclear. It should be emphasized that the reductions in resting and contracting muscle pH following heating in the present study, although statistically significant, were quite small and may not be physiologically meaningful.
The 36% reduction in high-intensity exercise tolerance in the HOT condition is in line with several previous investigations which have imposed heat stress during exercise (e.g., González-Alonso and Calbet 2003; Nybo et al. 2001). We have previously shown, using the same exercise modality and measurement techniques adopted herein, that a similar intramuscular metabolic milieu was attained at the limit of tolerance in four different high-intensity constant-work-rate exercise bouts performed in a normoxic and normothermic environment (Vanhatalo et al. 2010). Specifically, similar low intramuscular [PCr] and pH and similar high intramuscular [Pi] and [ADP] values were observed at the limit of tolerance across the four trials (Vanhatalo et al. 2010). It is well documented that PCr degradation and anaerobic glycolysis are accelerated in conditions of heat stress, as determined from the analysis of skeletal muscle biopsy samples (e.g., Febbraio et al. 1996; González-Alonso and Calbet 2003). This greater muscle metabolic perturbation with heat stress would therefore be predicted to expedite the attainment of a ‘critical’ muscle metabolic milieu and to reduce the tolerable duration of high-intensity exercise. Indeed, relative to CON, the decline in muscle [PCr] and pH and, to a lesser extent, the increase in [Pi] were accelerated in HOT such that these variables attained ‘critical’ levels more rapidly (Fig. 1). That the same muscle metabolite levels were reached at the limit of tolerance in both conditions, but that the tolerable duration of exercise occurred earlier in the HOT condition, indicates that the attainment of this critical intramuscular metabolic environment may be a determinant of high-intensity exercise tolerance. This is supported by the findings that dietary nitrate supplementation (Bailey et al. 2010) and variations in the fraction of inspired O2 (Hogan et al. 1999; Vanhatalo et al. 2010) impact on the tolerable duration of high-intensity exercise by changing the rate at which muscle metabolic perturbation develops but without altering the absolute values of these substrates and metabolites at the limit of tolerance. It is unclear, however, whether these critical muscle metabolite levels reduced exercise tolerance directly, for example, by impacting on processes that operate distal to the neuro-muscular junction, including muscle excitability, sarcoplasmic reticulum Ca2+ handling and/or cross-bridge cycling (i.e., peripheral fatigue; Allen et al. 2008), or indirectly, through afferent feedback to the brain and a subsequent reduction in central motor output (i.e., central fatigue; Gandevia 2001).
A limitation to the present study was that we did not measure the muscle temperature. This was because the majority of subjects did not consent to this invasive procedure. Measurements of rectal temperature in some subjects (n = 3), however, confirmed that the effects were similar to those measured in our previous study where we used an identical passive heating protocol (Burnley et al. 2002). We have therefore assumed that this protocol resulted in a similar elevation of quadriceps muscle temperature to that reported previously (Burnley et al. 2002). Although we have presented data suggesting that the degree of muscle metabolic perturbation may be an important determinant of high-intensity exercise tolerance, we cannot exclude a possible role for central factors. Indeed, the increased core temperature might reduce voluntary muscle activation (Morrison et al. 2004). Furthermore, elevated heat stress has been shown to increase circulating [ammonia] ([NH3]; Mohr et al. 2006). NH3 can cross the blood–brain barrier and has been implicated in central fatigue (Banister and Cameron, 1990). It is also possible that the earlier attainment of a critical metabolic environment in the HOT condition was communicated to the brain via metabolically sensitive type III and IV afferents within the muscle, leading to a reduction in central motor drive (Amann 2011). Therefore, the periphery and brain may have interacted to reduce the tolerable duration of exercise in the HOT condition ensuring that peripheral fatigue did not exceed critical levels. Further research is required to elucidate the central and peripheral determinants of skeletal muscle fatigue during high-intensity exercise in the heat.
In conclusion, this study used 31P-MRS to characterize the dynamics of intramuscular metabolic perturbation during high-intensity exercise with and without prior lower-body heating. A passive heating protocol known to increase both muscle and core temperature was shown to accelerate the decline in muscle [PCr] and pH and, to a lesser extent, the increase in muscle [Pi]. The intramuscular pH, [PCr] and [Pi] were not significantly different at the limit of tolerance in the HOT and CON conditions; however, the same absolute values were more rapidly attained in the HOT condition in which the tolerable duration of exercise was reduced. These results suggest that the more rapid development of intramuscular metabolic perturbation may be an important contributory factor to the reduced fatigue resistance observed during high-intensity exercise following prior heating.
References
Allen DG, Lamb GD, Westerblad H (2008) Skeletal muscle fatigue: cellular mechanisms. Physiol Rev 88:287–332
Amann M (2011) Central and peripheral fatigue: interaction during cycling exercise in humans. Med Sci Sports Exerc 43:2039–2045
Bailey SJ, Fulford J, Vanhatalo A, Winyard PG, Blackwell JR, DiMenna FJ, Wilkerson DP, Benjamin N, Jones AM (2010) Dietary nitrate supplementation enhances muscle contractile efficiency during knee-extensor exercise in humans. J Appl Physiol 109:135–148
Banister EW, Cameron BJ (1990) Exercise-induced hyperammonemia: peripheral and central effects. Int J Sports Med 11(Suppl 2):S129–S142
Burnley M, Doust JH, Jones AM (2002) Effects of prior heavy exercise, prior sprint exercise and passive warming on oxygen uptake kinetics during heavy exercise in humans. Eur J Appl Physiol 87:424–432
Ch’en FF, Dilworth E, Swietach P, Goddard RS, Vaughan-Jones RD (2003) Temperature dependence of Na+–H+ exchange, Na+–HCO3 − co-transport, intracellular buffering and intracellular pH in guinea-pig ventricular myocytes. J Physiol 552:715–726
Drust B, Rasmussen P, Mohr M, Nielsen B, Nybo L (2005) Elevations in core and muscle temperature impairs repeated sprint performance. Acta Physiol Scand 183:181–190
Edwards RH, Harris RC, Hultman E, Kaijser L, Koh D, Nordesjö LO (1972) Effect of temperature on muscle energy metabolism and endurance during successive isometric contractions, sustained to fatigue, of the quadriceps muscle in man. J Physiol 220:335–352
Febbraio MA (2000) Does muscle function and metabolism affect exercise performance in the heat? Exerc Sport Sci Rev 28:171–176
Febbraio MA, Snow RJ, Hargreaves M, Stathis CG, Martin IK, Carey MF (1994a) Muscle metabolism during exercise and heat stress in trained men: effect of acclimation. J Appl Physiol 76:589–597
Febbraio MA, Snow RJ, Stathis CG, Hargreaves M, Carey MF (1994b) Effect of heat stress on muscle energy metabolism during exercise. J Appl Physiol 77:2827–2831
Febbraio MA, Carey MF, Snow RJ, Stathis CG, Hargreaves M (1996) Influence of elevated muscle temperature on metabolism during intense, dynamic exercise. Am J Physiol 271:1251–1255
Ferguson RA, Krustrup P, Kjaer M, Mohr M, Ball D, Bangsbo J (2006) Effect of temperature on skeletal muscle energy turnover during dynamic knee-extensor exercise in humans. J Appl Physiol 101:47–52
Gandevia SC (2001) Spinal and supraspinal factors in human muscle fatigue. Physiol Rev 81:1725–1789
González-Alonso J, Calbet JA (2003) Reductions in systemic and skeletal muscle blood flow and oxygen delivery limit maximal aerobic capacity in humans. Circulation 107:824–830
González-Alonso J, Calbet JA, Nielsen B (1998) Muscle blood flow is reduced with dehydration during prolonged exercise in humans. J Physiol 513:895–905
González-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B (1999) Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol 86:1032–1039
González-Alonso J, Crandall CG, Johnson JM (2008) The cardiovascular challenge of exercising in the heat. J Physiol 586:45–53
Gray SR, De Vito G, Nimmo MA, Farina D, Ferguson RA (2006) Skeletal muscle ATP turnover and muscle fiber conduction velocity are elevated at higher muscle temperatures during maximal power output development in humans. Am J Physiol Regul Integr Comp Physiol 290:376–382
Gray SR, Söderlund K, Ferguson RA (2008) ATP and phosphocreatine utilization in single human muscle fibres during the development of maximal power output at elevated muscle temperatures. J Sports Sci 26:701–707
Hogan MC, Richardson RS, Haseler LJ (1999) Human muscle performance and PCr hydrolysis with varied inspired oxygen fractions: a 31P-MRS study. J Appl Physiol 86:1367–1373
Jones AM, Wilkerson DP, DiMenna F, Fulford J, Poole DC (2008) Muscle metabolic responses to exercise above and below the “critical power” assessed using 31P-MRS. Am J Physiol Regul Integr Comp Physiol 294:585–593
King DS, Costill DL, Fink WJ, Hargreaves M, Fielding RA (1985) Muscle metabolism during exercise in the heat in unacclimatized and acclimatized humans. J Appl Physiol 59:1350–1354
Mohr M, Rasmussen P, Drust B, Nielsen B, Nybo L (2006) Environmental heat stress, hyperammonemia and nucleotide metabolism during intermittent exercise. Eur J Appl Physiol 97:89–95
Morrison S, Sleivert GG, Cheung SS (2004) Passive hyperthermia reduces voluntary activation and isometric force production. Eur J Appl Physiol 91:729–736
Nybo L, Nielsen B (2001a) Middle cerebral artery blood velocity is reduced with hyperthermia during prolonged exercise in humans. J Physiol 534:279–286
Nybo L, Nielsen B (2001b) Hyperthermia and central fatigue during prolonged exercise in humans. J Appl Physiol 91:1055–1060
Nybo L, Jensen T, Nielsen B, González-Alonso J (2001) Effects of marked hyperthermia with and without dehydration on \( {\dot{V}}{{\text{O}_{2} }} \) kinetics during intense exercise. J Appl Physiol 90:1057–1064
Nybo L, Møller K, Volianitis S, Nielsen B, Secher NH (2002a) Effects of hyperthermia on cerebral blood flow and metabolism during prolonged exercise in humans. J Appl Physiol 93:58–64
Nybo L, Secher NH, Nielsen B (2002b) Inadequate heat release from the human brain during prolonged exercise with hyperthermia. J Physiol 545:697–704
Parkin JM, Carey MF, Zhao S, Febbraio MA (1999) Effect of ambient temperature on human skeletal muscle metabolism during fatiguing submaximal exercise. J Appl Physiol 86:902–908
Pettigrew DW, Frieden C (1979) Rabbit muscle phosphofructokinase. A model for regulatory kinetic behavior. J Biol Chem 254:1896–1901
Starkie RL, Hargreaves M, Lambert DL, Proietto J, Febbraio MA (1999) Effect of temperature on muscle metabolism during submaximal exercise in humans. Exp Physiol 84:775–784
Taylor DJ, Bore PJ, Styles P, Gadian DG, Radda GK (1983) Bioenergetics of intact human muscle. A 31P nuclear magnetic resonance study. Mol Biol Med 1:77–94
Vanhamme L, van den Boogaart A, Van Huffel S (1997) Improved method for accurate and efficient quantification of MRS data with use of prior knowledge. J Magn Reson 129:35–43
Vanhatalo A, Fulford J, DiMenna FJ, Jones AM (2010) Influence of hyperoxia on muscle metabolic responses and the power-duration relationship during severe-intensity exercise in humans: a 31P magnetic resonance spectroscopy study. Exp Physiol 95:528–540
Wyss M, Schlegel J, James P, Eppenberger HM, Wallimann T (1990) Mitochondrial creatine kinase from chicken brain. Purification, biophysical characterization, and generation of heterodimeric and heterooctameric molecules with subunits of other creatine kinase isoenzymes. J Biol Chem 265:15900–15908
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by David C. Poole.
Rights and permissions
About this article
Cite this article
Bailey, S.J., Wilkerson, D.P., Fulford, J. et al. Influence of passive lower-body heating on muscle metabolic perturbation and high-intensity exercise tolerance in humans. Eur J Appl Physiol 112, 3569–3576 (2012). https://doi.org/10.1007/s00421-012-2336-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-012-2336-6