Abstract
The purpose of this study is to test the role that parasympathetic postganglionic neurons could play on the adaptive electrophysiological changes produced by physical training on intrinsic myocardial automatism, conduction and refractoriness. Trained rabbits were submitted to a physical training protocol on treadmill during 6 weeks. The electrophysiological study was performed in an isolated heart preparation. The investigated myocardial properties were: (a) sinus automatism, (b) atrioventricular and ventriculoatrial conduction, (c) atrial, conduction system and ventricular refractoriness. The parameters to study the refractoriness were obtained by means of extrastimulus test at four different pacing cycle lengths (10% shorter than spontaneous sinus cycle length, 250, 200 and 150 ms) and (d) mean dominant frequency (DF) of the induced ventricular fibrillation (VF), using a spectral method. The electrophysiological protocol was performed before and during continuous atropine administration (1 μM), in order to block cholinergic receptors. Cholinergic receptor blockade did not modify either the increase in sinus cycle length, atrioventricular conduction and refractoriness (left ventricular and atrioventricular conduction system functional refractory periods) or the decrease of DF of VF. These findings reveal that the myocardial electrophysiological modifications produced by physical training are not mediated by intrinsic cardiac parasympathetic activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The effects of aerobic endurance training on sinus chronotropism and atrioventricular conduction are well known. Indeed, a decrease in the resting heart rate and a depressed atrioventricular conduction has been reported in human and experimental studies (Katona et al. 1982; Bedford and Tipton 1987; Stein et al. 2000). It has been proposed that these modifications are the result of an increased resting vagal tone (Bedford and Tipton 1987; Seals and Chase 1989; Shi et al. 1995). However, data presented by several investigations have shown the involvement of intrinsic mechanisms in the heart rate decrease (Lewis et al. 1980; Katona et al. 1982; Bonaduce et al. 1998; Stein et al. 2002) and the atrioventricular conduction depression characteristics of the trained athlete (Stein et al. 2002), albeit other possible influences like humoral factors could not be excluded on these in vivo studies. Similar results have been obtained in experimental models using isolated heart preparations and thus not submitted to humoral or extrinsic nervous influences, not only on sinus chronotropism (Nylander et al. 1982; Such et al. 2002, 2008) and atrioventricular node conduction (Such et al. 2008), but also on ventricular refractoriness, which increased by training (Such et al. 2002, 2008).
On the other hand, the heart contains postganglionic cholinergic neurons distributed throughout each major atrial and ventricular ganglionated plexus (Papka 1976; Pardini et al. 1987; Armour 2004; Johnson et al. 2004). It has been reported that these neurons can display ongoing activity (Gagliardi et al. 1988) even after acute decentralization (Armour and Hopkins 1990a, b) and can modify cardiac activity (Gray et al. 2004; Johnson et al. 2004), although their precise function and physiological relevance is not completely known (Armour 2004). Furthermore, despite the interruption of parasympathetic discharges from the vagus nerve by isolating the heart, synthesis and release of acetylcholine (ACh) from parasympathetic postganglionic neurons do not cease even under resting conditions (Löffelholz 1981).
Since the involvement of parasympathetic postganglionic neurons on automatism, conduction and ventricular refractoriness modifications produced by chronic exercise is not well-known, our purpose is to investigate the role of intrinsic cholinergic neurons on these electrophysiological modifications in a model of isolated heart preparation from trained rabbits. We hypothesize that the electrophysiological changes produced by physical training are mediated by parasympathetic postganglionic neurons activity.
Materials and methods
Animals and study design
Thirty-two male New Zealand white rabbits (Oryctolagus cuniculus) were used in the present study. Animals were divided into three experimental groups: a trained group (n = 11), a control group (n = 11) and a sham-operated group (n = 10). Animals in control and sham-operated group were housed in the animal quarters for 46 days and rabbits in the trained group were submitted to a physical exercise program. After familiarization with treadmill running for 4 days, animals in trained group ran 5 days/week for 6 weeks at 0.33 m s−1. Each training session was divided into six periods of 4 min of running and 1 min of rest (Such et al. 2008). The correct execution of treadmill exercise was constantly supervised and those animals that did not adequately run on the treadmill, because they either stopped frequently or ran irregularly, were excluded from the study. Housing conditions and experimental procedures were in accordance with the European Union regulation on the use of animals for scientific purposes (2003/65/CE) and as promulgated by Spanish legislation (RD 1201/2005). The University of Valencia Animal Care and Use Committee approved all the procedures used in this study.
Preparation and perfusion
Following heparinization and anesthesia (ketamine 25 mg kg−1, i.v.), animals were euthanized. After thoracotomy, the heart was quickly removed and immersed in cold (4°C) Tyrode solution for further preparation. The aorta was cannulated and connected to a Langendorff system to provide the heart with warmed, oxygenated Tyrode solution containing (in mM) 130 NaCl, 5.6 KCl, 2.2 CaCl2, 0.6 MgCl2, 1.4 NaH2PO4, 25 NaHCO3, and 12.2 glucose. Oxygenation was carried out with a mixture of 95% O2 and 5% CO2. Tyrode temperature was constant throughout the experiment (37 ± 0.5°C), and perfusion pressure was maintained at 60 mmHg.
Two bipolar surface electrodes (silver wire, Teflon-coated) with an inter-electrode distance of 1 mm were positioned on the right atrium for recording and pacing, and an identical electrode was placed on the left ventricle for pacing. Ventricular recordings were made by means of a plaque with 240 unipolar stainless steel electrodes (electrode diameter = 0.125 mm, interelectrode distance = 1 mm) positioned at the epicardial surface of the lateral wall of the left ventricle. The indifferent electrode was a 4 × 6 mm stainless steel plaque located over the cannulated aorta. Recordings were obtained with a cardiac electrical activity mapping system (MAPTECH, Waalre, The Netherlands). The electrograms were amplified with a gain of 100–300, broad-band (1–400 Hz) filtered and multiplexed. The sampling rate in each channel was 1 kHz. Electrical stimuli were delivered by a Grass S-88 stimulator (Grass Instruments, Quincy, MA, USA) connected to a stimulus isolation unit.
Measurements and calculations
In the experiments, we used the same procedure with trained and non-trained rabbits. The parameters studied and their definitions were the following (for a detailed description see Such et al. 2002, 2008): (1) sinus cycle length: the interval between two successive ventricular electrograms during basal sinus rhythm (V–V interval), (2) A–V interval: the interval between an atrial electrogram and its corresponding ventricular electrogram during basal sinus rhythm; (3) Wenckebach cycle length (WCL): the maximum cycle length of atrial pacing that produces A–V Wenckebach block, (4) retrograde WCL (RWCL): the maximum cycle length of ventricular pacing that impedes a 1:1 V–A conduction, (5) atrial effective refractory period (AERP): the maximum atrial extrastimulus coupling interval without atrial capture, (6) atrial functional refractory period (AFRP): the minimum interval between the atrial electrogram produced by the last basic atrial train stimulus and the one triggered by the extrastimulus, (7) ventricular effective refractory period (VERP): the maximum ventricular extrastimulus coupling interval without ventricular capture, (8) ventricular functional refractory period (VFRP): the minimum interval between the ventricle electrogram produced by the last basic ventricular train stimulus and the one triggered by the extrastimulus, (9) A–V conduction system effective refractory period (AVCSERP): the maximum atrial electrogram coupling interval produced by the extrastimulus without ventricular capture, (10) A–V conduction system functional refractory period (AVCSFRP): the minimum interval between the ventricular electrogram produced by the last basic atrial train stimulus and the one triggered by the extrastimulus, (11) effective refractory period of the V–A retrograde conduction system (VACSERP): the maximum ventricular electrogram coupling interval, produced by the extrastimulus, without atrial capture, (12) functional refractory period of the V–A retrograde conduction system (VACSFRP): the minimum interval between the atrial electrogram produced by the last basic ventricular train stimulus and the one triggered by the ventricular extrastimulus, (13) mean dominant frequency (DF) of ventricular fibrillation (VF): the frequency of the power spectrum with the greatest amplitude, analyzed in consecutive segments of 4 s using Welch’s method.
In order to investigate these parameters, we performed several tests according to the following protocol: (1) atrial pacing at increasing frequencies (2 Hz s−1) to calculate WCL, (2) atrial extrastimulus test using basic trains of 10 stimuli at four different pacing cycle lengths: 10% shorter than sinus cycle length, 250, 200 and 150 ms. The pause between trains was 1 s and the extrastimulus was delivered with 5 ms decrements in each of the trains of stimuli starting from the coupling interval 10% lower than the sinus cycle length, 250, 200 and 150 ms. This test was used to determine atrial and A–V conduction refractoriness, (3) ventricular extrastimulus test, using the same technique as in atrial extrastimulus test, was performed to evaluate ventricular and V–A retrograde conduction refractoriness, (4) ventricular pacing at increasing frequencies (2 Hz s−1) to obtain RWCL and induce VF, (5) recording of ventricular electrograms during VF (330 s). Coronary perfusion was maintained during the arrhythmia. After 10 min of stabilization, 1 μM atropine sulphate (Sigma-Aldrich, St. Louis, MO, USA) dissolved in Tyrode, was administered through the aorta in continuous infusion. This concentration has been shown to effectively block myocardial muscarinic receptors in the isolated rabbit heart (Ng et al. 2001; Brack et al. 2011). Maintaining the infusion of atropine, we repeated the electrophysiological protocol to evaluate any possible changes derived from parasympathetic activity in the parameters studied after muscarinic receptors blockade. In the sham-operated group, the same volume of filtered Tyrode without atropine was infused because we wanted to confirm if the course of time or another manoeuvre such as the repetition of stimulation protocol could modify the results. V–V interval was measured after the initial period of stabilization, immediately before and after atropine and/or Tyrode infusion.
Stimuli of 2 ms duration and twice diastolic threshold were used in the stimulation protocol. Mean atrial diastolic threshold was 8.8 ± 5 mA, while the mean ventricular diastolic threshold reached values of 14.2 ± 5 mA.
Coronary flow was weighed after collection for 1 min. Measurements were performed before starting the electrophysiological protocol, before and after the infusion of atropine, and also at the end of the protocol. Each heart was weighed after the experiment had finished.
Data analysis
All data are expressed as mean ± SD. Comparisons of refractory periods and DF of VF were made using a two-way ANOVA with repeated measures. Paired and unpaired Student’s t test were used to compare R–R interval, A–V interval, WCL and RWCL, coronary flow and heart weights between or within groups when necessary. Statistical significance was accepted when P < 0.05.
Results
Sinus automatism
In the sham-operated group, the course of time or the experimental protocol repetition did not modify V–V interval (Table 1). Likewise, cholinergic blockade did not modify V–V interval in the control and trained groups. Sinus cycle length at the beginning of the electrophysiological protocol (basal) was 16% longer in the trained versus the control group (P < 0.05).
A–V and V–A conduction
After atropine administration, no differences in A–V interval and WCL were obtained within the control and trained groups (Table 2). WCL was 10% longer in the trained group with respect to the control group (P < 0.05). In the sham-operated and control groups, RWCL underwent a 4 and 8% increase after Tyrode and atropine infusion, respectively (P < 0.05).
Atrial, ventricular, A–V nodal, and V–A retrograde conduction system refractoriness
Neither the effective nor the functional atrial, ventricular, A–V and V–A conduction system refractory periods were modified by the infusion of atropine (Fig. 1a–f). The functional refractory period of the left ventricle was longer in trained animals vs controls (P < 0.05) at the four pacing cycle lengths: 156 ± 16 versus 138 ± 7 ms at a coupling interval 10% lower than the sinus cycle length, 144 ± 11 versus 129 ± 7 ms at 250 ms pacing cycle length, 133 ± 16 versus 118 ± 7 ms at 200 ms pacing cycle length and 122 ± 5 versus 110 ± 13 ms at 150 ms pacing cycle length (Fig. 1d). Similarly, a larger A–V conduction system functional refractory period was observed in the trained group (P < 0.05 vs. control): 178 ± 17 versus 152 ± 7 ms at a coupling interval 10% lower than the sinus cycle length, 160 ± 13 versus 145 ± 6 ms at 250 ms pacing cycle length and 151 ± 11 versus 140 ± 5 ms at at 200 ms pacing cycle length (Fig. 1e). No significant differences were found in the remaining parameters of refractoriness between trained and untrained animals. AVCSERP and VACSERP were not analyzed because, in most cases, the atrial or ventricular effective refractory period was reached before the conduction system refractory period took place. Results obtained in the sham-operated group indicate that none of these parameters of refractoriness were modified by the course of time or the experimental protocol repetition (Supplementary Tables 1, 2, 3).
Myocardial refractory periods before and after atropine/Tyrode infusion. No differences were obtained after parasympathetic blockade in AERP (a), AFRP (b), VERP (c), VFRP (d), AVCSFRP (e) and VACSFRP (f). 10% SCL = pacing frequency 10% shorter than spontaneous sinus cycle length, 250, 200 and 150 = pacing cycle length of 150, 200 and 150 ms, pre = before Tyrode (sham) and atropine infusion (control and trained groups), post = after Tyrode (sham) and atropine infusion (control and trained groups). *P < 0.05 versus control. Error bars display the standard error of the mean
Dominant frequency of ventricular fibrillation
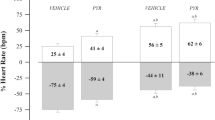
There were no differences in the DF of VF in the sham-operated group when comparisons before and after Tyrode infusion were made. In this group, DF of VF reached values of 22.0 ± 3.0 Hz immediately after VF triggering and decreased to 15.6 ± 3.3 Hz at 300 s. After Tyrode infusion, DF decreased from 24.3 ± 6.2 to 17.4 ± 4.6 Hz. Similar kinetics were observed in the trained and control groups and no changes were found after cholinergic blockade on the mean DF of VF of both groups (Fig. 2). The mean DF of VF was lower in the trained group (Fig. 2). VF reverted spontaneously to sinus rhythm in three trained animals.
Dominant frequency of ventricular fibrillation. Parasympathetic blockade did not modify this parameter in control and trained groups. Furthermore, DF of VF was lower in the trained group *P < 0.05, † P = 0.08, ‡ P = 0.06, § P = 0.09 versus control group. Error bars display the standard error of the mean
Coronary flow and heart weights
Coronary flow was not different between trained and control group (Table 3) when expressed in milliliters per minute per gram (3.36 ± 0.9 in the trained group vs. 3.47 ± 0.9 ml min−1 g−1 in the control group; P > 0.05; Table 3). Likewise, parasympathetic blockade did not modify coronary flow within the control and the trained groups. In the sham-operated group, the course of time or the experimental protocol repetition did not modify this parameter. Heart weights were similar in trained and control rabbits (14.4 ± 2 and 14.2 ± 2 g, respectively; P > 0.05; Supplementary Table 4).
Discussion
We have studied the role of parasympathetic postganglionic neurons on the training-induced modifications of the myocardial electrophysiological properties: automatism, conduction and refractoriness. The main findings of this study are that parasympathetic blockade did not modify the effect of physical training on both sinus node automatism and atrioventricular conduction, and atrioventricular conduction system and ventricular refractoriness.
Effect of parasympathetic blockade on automatism and conduction
As we have shown in “Results”, physical training depressed sinus node automatism and A–V nodal conduction. These results are partially in accordance with those previously obtained in human (Lewis et al. 1980; Katona et al. 1982; Bonaduce et al. 1998; Stein et al. 2000, 2002) and experimental studies (Nylander et al. 1982; Negrao et al. 1992; Such et al. 2002, 2008). Nevertheless, muscarinic receptor blockade with atropine did not modify the negative chronotropic and dromotropic effects produced by physical training. It has been reported that the increase in resting cardiac parasympathetic activity produced by physical training underlies the decrease in resting heart rate and the depression of A–V conduction. As it is well known, the release of ACh from parasympathetic postganglionic terminals causes a muscarinic receptor-mediated opening of specific potassium channels (I KACh) and other effects on several pacemaker currents that result in slowing the firing rate of pacemaker cells and a delay in AV conduction (Carmeliet and Mubagwa 1998; Snyders 1999). In view of the present results, parasympathetic postganglionic neurons activity does not explain the bradycardia and A–V conduction delay in isolated hearts from trained animals. Additionally, we did obtain differences in RWCL in the sham and control groups, an increase being produced after the infusion of Tyrode/atropine, respectively. These results are quite surprising, as parasympathetic blockade should have enhanced impulse conduction and decreased RWCL, given that ACh depresses conduction. Hence, the increase in RWCL does not seem to be an atropine related effect.
Refractoriness and parasympathetic blockade
With respect to the effects of cholinergic blockade, the changes produced by physical training on myocardial refractoriness were not mediated by intrinsic parasympathetic activity, as we did not find modifications by atropine infusion in ventricular or atrioventricular conduction system refractoriness.
The study of ventricular refractoriness was carried out using two different methods: ventricular extrastimulus test and spectrum analysis of VF. Both measures provide a reliable method to assess ventricular refractoriness, not only with a common method used in electrophysiological studies (extrastimulus test) but also with the DF of VF. This last parameter expresses the speed of ventricular activation during the VF and inversely correlates with VFRP, being an indirect measure of ventricular refractoriness (Chorro et al. 2000). Moreover, this procedure let us analyze up to 240 different points of ventricular myocardium in each experiment during VF.
Our results show that the increase in ventricular refractoriness produced by physical training, assessed by the increase in VFRP and the decrease in DF of VF, was not altered after parasympathetic blockade. With respect to the increase of ventricular refractoriness, these results are similar to those obtained in previous studies (Such et al. 2008). The prolongation of ventricular refractoriness could be related to intrinsic parasympathetic activity since parasympathetic postganglionic neurons are also found in the ventricle and their activity can lead to a release of ACh even in the isolated heart (Löffelholz 1981). This is consistent with experimental studies which have reported a prolonging effect of vagal nerve stimulation on ventricular refractoriness (Martins and Zipes 1980; Inoue and Zipes 1987), even without background sympathetic activity (Litovsky and Antzelevitch 1990). Nevertheless, atropine administration did not modify the training-induced increase in ventricular refractoriness, indicating that this cardiac electrophysiological modification is not mediated by the activation of I KACh.
Regarding A–V conduction system refractoriness, we found that physical training increased AVCSFRP and this increase was not abolished after atropine infusion. Consequently, ACh does not seem to be implicated in the A–V conduction system refractoriness increase produced by physical training. These results are consistent with Stein et al. (2002), which found an increase in the intrinsic atrioventricular node effective refractory period in athletes compared to untrained individuals, indicating that these changes were caused by intrinsic electrophysiological modifications. Neither physical training nor parasympathetic blockade modified retrograde conduction system refractoriness.
With respect to atrial refractoriness and its modification by physical training, it has been reported either no change (Brorson et al. 1976) or an increase (Mezzani et al. 1990) in athletes with Wolff–Parkinson–White syndrome. Experimental studies carried out in isolated rabbit heart have shown that although the differences were not statistically significant, AERP tended to increase (P = 0.09) in the hearts of trained animals (Such et al. 2008). In the present study, physical training did not change AERP and AFRP and these parameters were not modified after parasympathetic blockade. Regarding the effect of parasympathetic stimulation, acetylcholine release from parasympathetic postganglionic terminals in the atria activates I KACh, which leads to a shortening of the AERP, a decrease in the action potential duration and an increase in the dispersion of refractoriness (Zipes et al. 1974; Vigmond et al. 2004). These electrophysiological modifications facilitate the induction and maintenance of atrial fibrillation, whose incidence has been reported to be higher in long-term endurance athletes (Mont et al. 2009). Data presented indicate that the training protocol used in the present study does not modify atrial refractoriness and that there is no ACh release from parasympathetic postganglionic terminals to exert any influence in atrial refractoriness in the isolated rabbit heart model.
The results obtained not only in the intrinsic heart rate and atrioventricular conduction but also in myocardial ventricular and atrioventricular node refractoriness, suggest a contributing role of an intrinsic adaptation induced by physical training. The observed electrophysiological modifications are exhibited in an isolated heart preparation and thus not submitted to extrinsic nervous system and/or humoral influences. Regarding the basic mechanisms implied in these modifications, we have discarded a functional implication of I KACh by means of muscarinic blockade with atropine, which implies that these modifications are not dependent on intrinsic parasympathetic activity. Previous studies carried out by our research team reported that these changes do not seem to be related to heart hypertrophy, lipid peroxidation, and/or coronary flow modifications either (Such et al. 2008).
Some other membrane channels could account for the observed electrophysiological remodeling in trained animals, in particular Ca++ and K+ channel species might be involved. Regarding Ca++ channels, no changes have been reported by physical training in the slow inward Ca++ current (I Ca-L) activity (Mokelke et al. 1997) or in Na+/Ca++ exchanger (Mace et al. 2003). On the other hand, Jew et al. (2001) observed an alteration in the characteristics of the outward K+ repolarizing currents I to and I sus, but they did not determine which specific current component contributing to the composite I sus and/or I to was affected by training. Regarding the latter, Stones et al. (2009) also found an alteration of I to in trained animals submitted to voluntary exercise. Furthermore, we can speculate with a possible modification in the characteristics of the inward rectifier K+ current, I K1, which sets the resting membrane potential, controls the approach to threshold upon depolarization and modulates the terminal phase of repolarization (Lopatin and Nichols 2001).
Methodological considerations
It must be noted that the experimental preparation used is not a “working heart” and the differences observed between groups do not result from differences in cardiac work (Such et al. 2008). Moreover, it has been reported that rabbits provide a good experimental model for the investigation of cardiac electrophysiology. As it is known the electrophysiological properties and VF characteristics in the rabbit are more similar to that observed in humans than rats or mice (Panfilov 2006; Gao et al. 2007), which have major limitations in performing cardiac electrophysiological studies (Gaustad et al. 2010). Finally, by using the proper intensity, duration and frequency of exercise, the rabbit obtains a documented cardiovascular training effect rather easily (Di Carlo and Bishop 1990). Indeed, it has been shown that the training protocol used reduces heart rate in vivo and in vitro (Such et al. 2008), which is considered to be one of the most fundamental systemic characteristics of the trained state (Moore and Korzick 1995). Moreover, the training protocol produced myocardial HSP60 and iNOs expression modifications (Such et al. 2008) which are associated with physical training (Hamilton et al. 2001; Gómez-Cabrera et al. 2005).
In conclusion, our findings reveal that the myocardial intrinsic electrophysiological modifications produced by physical training are not mediated by parasympathetic postganglionic activity. As parasympathetic blockade did not modify the electrophysiological properties studied in isolated rabbit heart, other intrinsic modifications must be implied.
References
Armour JA, Hopkins DA (1990a) Activity of in vivo canine ventricular neurons. Am J Physiol Heart Circ Physiol 258:H326–H336. doi:10.1152/ajpregu.00183.2004
Armour JA, Hopkins DA (1990b) Activity of canine in situ left atrial ganglion neurons. Am J Physiol Heart Circ Physiol 259:H1207–H1215
Armour JA (2004) Cardiac neuronal hierarchy in health and disease. Am J Physiol Regul Integr Comp Physiol 287:R262–R271
Armour JA, Murphy DA, Yuan BX, Macdonald S, Hopkins DA (1997) Gross and microscopic anatomy of the human intrinsic cardiac nervous system. Anat Rec 247:289–298
Bedford TG, Tipton CM (1987) Exercise training and the arterial baroreflex. J Appl Physiol 63:1926–1932
Bonaduce D, Petretta M, Cavallaro V, Apicella C, Ianniciello A, Romano M, Breglio R, Marciano F (1998) Intensive training and cardiac autonomic control in high level athletes. Med Sci Sports Exerc 30:691–696
Brack KE, Coote JH, Ng GA (2011) Vagus nerve stimulation protects against ventricular fibrillation independent of muscarinic receptor activation. Cardiovasc Res 91:437–446. doi:10.1093/cvr/cvr105
Brorson L, Conradson TB, Olsson B, Varnauskas E (1976) Right atrial monophasic action potential and effective refractory periods in relation to physical training and maximal heart rate. Cardiovasc Res 10:160–168
Carmeliet E, Mubagwa K (1998) Antiarrhythmic drugs and cardiac ion channels: mechanisms of action. Prog Biophys Mol Biol 70:1–72
Chorro FJ, Cánoves J, Guerrero J, Mainar L, Sanchis J, Such L, López-Merino V (2000) Alteration of ventricular fibrillation by flecainide, verapamil, and sotalol: an experimental study. Circulation 101:1606–1615
Di Carlo SE, Bishop VS (1990) Exercise training enhances cardiac afferent inhibition of baroreflex function. Am J Physiol 258:212–220
Gagliardi M, Randall WC, Bieger D, Wurster RD, Hopkins DA, Armour JA (1988) Activity of in vivo canine cardiac plexus neurons. Am J Physiol Heart Circ Physiol 255:H789–H800
Gao L, Wang W, Liu D, Zucker IH (2007) Exercise training normalizes sympathetic outflow by central antioxidant mechanisms in rabbits with pacing-induced chronic heart failure. Circulation 115:3095–3102. doi:10.1161/CIRCULATIONAHA.106.677989
Gaustad SE, Rolim N, Wisløff U (2010) A valid and reproducible protocol for testing maximal oxygen uptake in rabbits. Eur J Cardiovasc Prev Rehabil 17:83–88. doi:10.1097/HJR.0b013e32833090c4
Gómez-Cabrera MC, Borrás C, Pallardó FV, Sastre J, Ji LL, Viña J (2005) Decreasing xanthine oxidase-mediated oxidative stress prevents useful cellular adaptations to exercise in rats. J Physiol 567:113–120. doi:10.1113/jphysiol.2004.080564
Gray AL, Johnson TA, Ardell JL, Massari VJ (2004) Parasympathetic control of the heart II. A novel interganglionic intrinsic cardiac circuit mediates neural control of heart rate. J Appl Physiol 96:2273–2278. doi:10.1152/japplphysiol
Hamilton KL, Powers SK, Sugiura T, Kim S, Lennon S, Tumer N, Mehta JL (2001) Short-term exercise training can improve myocardial tolerance to I/R without elevation in heat shock proteins. Am J Physiol Heart Circ Physiol 281:1346–1352
Inoue H, Zipes DP (1987) Changes in atrial and ventricular refractoriness and atrioventricular nodal conduction produced by combinations of vagal and sympathetic stimulation that result in a constant spontaneous sinus cycle length. Circ Res 60:942–951
Jew KN, Olsson MC, Mokelke EA, Palmer BM, Moore RL (2001) Endurance training alters outward K+ current characteristics in rat cardiocytes. J Appl Physiol 90:1327–1333
Johnson TA, Gray AL, Lauenstein JM, Newton SS, Massari VJ (2004) Parasympathetic control of the heart I. An interventriculo-septal ganglion is the major source of the vagal intracardiac innervation of the ventricles. J Appl Physiol 96:2265–2272. doi:10.1152/japplphysiol.00620.2003
Katona PG, McLean M, Dighton DH, Guz A (1982) Sympathetic and parasympathetic cardiac control in athletes and nonathletes at rest. J Appl Physiol 52:1652–1657
Lewis SF, Nylander E, Gad P, Areskog N (1980) Non-autonomic component in bradycardia of endurance trained men at rest and during exercise. Acta Physiol Scand 109:297–305
Litovsky SH, Antzelevitch C (1990) Differences in the electrophysiological response of canine ventricular subendocardium and subepicardium to acetylcholine and isoproterenol. A direct effect of acetylcholine in ventricular myocardium. Circ Res 67:615–627
Löffelholz K (1981) Release of acetylcholine in the isolated heart. Am J Physiol 240(4):H431–H440
Lopatin AN, Nichols CG (2001) Inward rectifiers in the heart: an update on I(K1). J Mol Cell Cardiol 33:625–638. doi:10.1006/jmcc.2001.1344
Mace LC, Palmer BM, Brown DA, Jew KN, Lynch JM, Glunt JM, Parsons TA, Cheung JY, Moore RL (2003) Influence of age and run training on cardiac Na+/Ca2+ exchange. J Appl Physiol 95:1994–2003. doi:10.1152/japplphysiol.00551.2003
Martins JB, Zipes DP (1980) Effects of sympathetic and vagal nerves on recovery properties of the endocardium and epicardium of the canine left ventricle. Circ Res 46:100–110
Mezzani A, Giovannini T, Michelucci A, Padeletti L, Resina A, Cupelli V, Musante R (1990) Effects of training on the electrophysiologic properties of atrium and accessory pathway in athletes with Wolff–Parkinson–White syndrome. Cardiology 77:295–302
Mokelke EA, Palmer BM, Cheung JY, Moore RL (1997) Endurance training does not affect intrinsic calcium current characteristics in rat myocardium. Am J Physiol Heart Circ Physiol 273:H1193–H1197
Mont L, Elosua R, Brugada J (2009) Endurance sport practice as a risk factor for atrial fibrillation and atrial flutter. Europace 11:11–17. doi:10.1093/europace/eun289
Moore RL, Korzick DH (1995) Cellular adaptations of the myocardium to chronic exercise. Prog Cardiovasc Dis 37:371–396
Negrao CE, Moreira ED, Santos MC, Farah VM, Krieger EM (1992) Vagal function impairment after exercise training. J Appl Physiol 72:1749–1753
Ng GA, Brack KE, Coote JH (2001) Effects of direct sympathetic and vagus nerve stimulation on the physiology of the whole heart—a novel model of isolated Langendorff perfused rabbit heart with intact dual autonomic innervation. Exp Physiol 86:319–329
Nylander E, Sigvardsson K, Kilbom A (1982) Training-induced bradycardia and intrinsic heart rate in rats. Eur J Appl Physiol Occup Physiol 48:189–199
Panfilov AV (2006) Is heart size a factor in ventricular fibrillation? Or how close are rabbit and human hearts? Heart Rhythm 3:862–864. doi:10.1016/j.hrthm.2005.12.022
Papka RE (1976) Studies of cardiac ganglia in pre- and postnatal rabbits. Cell Tissue Res 175:17–35
Pardini BJ, Patel KP, Schmid PG, Lund DD (1987) Location, distribution and projections of intracardiac ganglion cells in the rat. J Auton Nerv Syst 20:91–101
Scott AS, Eberhard A, Ofir D, Benchetrit G, Dinh TP, Calabrese P, Lesiuk V, Perrault H (2004) Enhanced cardiac vagal efferent activity does not explain training-induced bradycardia. Auton Neurosci 112:60–68. doi:10.1016/j.autneu.2004.04.006
Seals DR, Chase PB (1989) Influence of physical training on HR variability and baroreflex circulatory control. J Appl Physiol 66:1886–1895
Shi X, Stevens GHJ, Foresman BH, Stern SA, Raven PB (1995) Autonomic nervous system control of the heart: endurance exercise training. Med Sci Sports Exerc 27:1406–1413
Snyders DJ (1999) Structure and function of cardiac potassium channels. Cardiovasc Res 42:377–390
Stein R, Moraes RS, Cavalcanti AV, Ferlin EL, Zimerman LI, Ribeiro JP (2000) Atrial automaticity and atrioventricular conduction in athletes: contribution of autonomic regulation. Eur J Appl Physiol 82:155–157
Stein R, Moraes RS, Cavalcanti AV, Ferlin EL, Zimerman LI, Ribeiro JP (2002) Intrinsic sinus and atrioventricular node electrophysiologic adaptations in endurance athletes. J Am Coll Cardiol 39:1033–1038
Stones R, Billeter R, Zhang H, Harrison S, White E (2009) The role of transient outward K+ current in electrical remodelling induced by voluntary exercise in female rat hearts. Basic Res Cardiol 104:643–652. doi:10.1007/s00395-009-0030-6
Such L, Rodríguez A, Alberola A, López L, Ruiz R, Artal L, Pons I, Pons ML, García C, Chorro FJ (2002) Intrinsic changes on automatism, conduction and refractoriness by exercise in insolated rabbit heart. J Appl Physiol 92:225–229. doi:10.1111/j.1748-1716.2008.01851.x
Such L, Alberola AM, Such-Miquel L, López L, Trapero I, Pelechano F, Gómez-Cabrera MC, Tormos A, Millet J, Chorro FJ (2008) Effects of chronic exercise on myocardial refractoriness: a study on isolated rabbit heart. Acta Physiol 193:331–339
Vigmond EJ, Tsoi V, Kuo S, Arevalo H, Kneller J, Nattel S, Trayanova N (2004) The effect of vagally induced dispersion of action potential duration on atrial arrhythmogenesis. Heart Rhythm 1:334–344. doi:10.1016/j.hrthm.2004.03.077
Zipes DP, Mihalick MJ, Robbins GT (1974) Effects of selective vagal and stellate ganglion stimulation of atrial refractoriness. Cardiovasc Res 8:647–655
Acknowledgments
The authors thank Carmen Rams, Ana Díaz, Pilar Navarro and César Avellaneda for their excellent technical assistance. This work has been supported by grants from the Spanish Ministry of Education and Science (DEP2007-73234-C03-01) and Generalitat Valenciana (PROMETEO 2010/093). M Zarzoso was supported by a research scholarship from Generalitat Valenciana (BFPI/2008/003).
Conflict of interest
None of the authors had any conflicts of interest with the funding agencies or professional relationships with companies or manufacturers who may benefit from the results of the present study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Keith Phillip George.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zarzoso, M., Such-Miquel, L., Parra, G. et al. The training-induced changes on automatism, conduction and myocardial refractoriness are not mediated by parasympathetic postganglionic neurons activity. Eur J Appl Physiol 112, 2185–2193 (2012). https://doi.org/10.1007/s00421-011-2189-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-2189-4