Abstract
Athletes with spinal cord injury often experience high heat storage due to reduced sweating capacity below the spinal injury. Spray bottle (SB) maybe used to apply mist for evaporative cooling during breaks in competitions. This study examined the efficacy of SB during rest breaks. Seven participants, four female and three males, (mean ± SD age 24 ± 4.1 year, weight 56.2 ± 7.0 kg, upper-body VO2 peak 2.4 ± 0.6 l/min) volunteered for the study. Participants were paraplegic athletes (T3–T12/L1) with both complete and incomplete lesions. Participants arm-cranked using a ramp protocol in an environment of 21 ± 1.5°C and 55 ± 3% rh once using a SB during 1-min rest between 7-min stages of increasing intensity and once without the SB (CON). Mean total work was similar (p = 0.86) for the SB and CON (2495.7 ± 914.6 vs. 2407.1 ± 982.3 kJ, respectively). Likewise, the mean work times were similar between trials (27 ± 6 and 26 ± 7 min for SB and CON, respectively). Furthermore, there were no significant differences detected between trials for skin temperature, rectal temperature, esophageal temperature (p > 0.05). There were no statistically significant differences detected between trials for RPE (p > 0.05). In conclusion, the application of artificial sweat via SB was ineffective in attenuating the onset of uncompensable heat strain during high-intensity arm exercise in a comfortable environment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adaptive sport and exercise programs are assuming a larger role in rehabilitation of the spinally injured, which has resulted in an increase in participation in sporting events traditionally available for able-bodied athletes (AB). Similar to AB athletes, individuals with spinal cord injuries (SCI) experience fitness gains and health benefits from exercise. However, many of these activities require high-intensity activity for extended periods, which places severe demands on the thermoregulatory system. When paraplegics expose themselves to such environmental stress and physiological strain, they may experience greater difficulty in regulating their body temperature, dependent on their level of lesion. Studies of paraplegic individuals have shown that at rest and during exercise, thermoregulatory responses are proportional to the level of lesion, reflecting the amount of sympathetic nervous system available for sweating and blood redistribution (Guttman et al. 1958; Petrofsky 1992; Price and Campbell 1997).
There has been extensive literature compiled on AB with regard to thermoregulation during exercise as well as the mechanisms that aid in heat dissipation (Marino 2002). However, published research regarding thermoregulation in SCI is very limited (Webborn et al. 2005). Only a few studies have addressed the topic of artificial cooling strategies for SCI during exercise (Armstrong et al. 1994; Hagobian et al. 2004; Webborn et al. 2005).
Armstrong et al. (1994) examined two different methods of artificial exogenous cooling in SCI. Each participant underwent two treatments, icepack vest, and refrigerated headpiece. Each treatment was applied during 30 min of strenuous exercise using both tetraplegic (n = 1) and paraplegic (n = 4) participants. Both cooling methods showed cooler rectal, skin, and mean body temperatures when compared to the control, no significant difference in core temperature was observed between trials.
Hagobian et al. (2004) examined the use of a foot-cooling device on a group (n = 6) of SCI athletes during exercise in the heat. The authors found that foot cooling was successful in attenuating the rise in core temperature during exercise (1.0 ± 0.2°C) compared with no cooling control (1.6 ± 0.2°C). In a study done on tetraplegic athletes, Webborn et al. (2005) examined thermoregulatory responses to heat exposure in eight SCI athletes with no cooling, pre-cooling, and during-exercise cooling conditions using a commercially available ice vest. Authors concluded that both ice-vest interventions reduced thermal strain and perceived exertion during the intermittent sprint exercise protocol.
However, it has been observed that the most commonly used artificial exogenous cooling device in the field is a water spray bottle. The water spray bottle is an exogenous cooling device that is intended to partially mimic the sweat response experienced by an AB athlete.
Since little is known regarding thermoregulation in SCI athletes, and because thermal strain at any point is a product of heat production as well as removal. The major objective of this particular protocol was to maintain high ecological validity, in order to evaluate the common practice of artificial cooling (spay water application) to reduce thermal strain during high-intensity intermittent activity, i.e. wheelchair basketball. It is common for wheelchair basketball competitions to be performed in climate-controlled environments. For example, the Paralympic training center (Birmingham, Alabama) is kept much cooler than is common due, in part, to the additional challenges SCI athletes face with respect to thermoregulation. Therefore, our study was designed to match the intense nature of wheelchair basketball, where athletes maintain high levels of metabolic output to match their competitive counterparts, yet in a realistic environment. Therefore, the purpose of this study was to evaluate the application of artificially induced sweating (sprayed water) on heat strain in SCI athletes. It was hypothesized that the application of artificial sweat would reduce heat strain.
Methods
Experimental design
A within-subjects repeated-measures counterbalanced design was utilized with dependent variables of HR, exercise duration, heat storage, mean skin temperature, and rectal and esophageal temperatures for both spray bottle (SB) and control (CON) (no spray bottle) conditions. For a power of 0.80 and an alpha of 0.05 an effect size of 0.2ºC (Lenth 2006), it was determined a priori that seven participants were required to detect a difference between CON and SB.
Participants
Seven unacclimatized participants (three male and four female) gave their informed consent to participate in this investigation which had received approval from The University of Alabama medical review board. Unacclimatized participants were used because most SCI athletes in the USA spend the majority of the year competing without the benefit of heat acclimatization. The group was comprised of seven spinal cord injured athletes (SCI) (T11–C7; Table 1). All were of similar training status, competing in collegiate wheelchair basketball.
Participants visited the laboratory on three separate occasions. On the first occasion, participants performed an incremental arm-crank exercise (ACE) test to determine VO2 peak with open-circuit spirometry (Vacumed, Vista mini-cpx, Ventura, CA, USA). This involved, initially, two sub-maximal exercise stages of ACE (30 and 50 W) separated by 1 min passive recovery (modified from Price and Campbell 2003). Once the second sub-maximal stage and rest stage had been completed, participants exercised to volitional exhaustion (unable to maintain required revolution rate) at a ramp rate of 20 W every 2 min from an initial level of 90 W. All tests were conducted on a cycle ergometer (Monarch, Varberg, Sweden) adapted for upper-body exercise. Participants were required to maintain a cadence of 60 rev/min throughout the exercise. Participants were asked every minute to estimate their perceived exertion on a 15-point rating of perceived exertion (RPE) chart (Borg 1973). Heart rate (HR) was recorded every minute throughout the entire test. On the first visit, participants were randomly assigned to one of two protocols: spray bottle (SB) or control (CON). All trials were undertaken in an environment representative of a climate-controlled gymnasiums (22 ± 1°C, 45–50 ± 0.1% relative humidity), selected to represent a typical wheelchair-playing environment. All participants completed each exercise protocol in regular exercise clothing, typical of competition and practice.
Spray bottle (SB) lab test
On arrival at the laboratory for the incremental test, thermocouples (Physitemp Instruments Inc. Clifton, NJ, USA) were positioned for measurement of rectal (T rec) and esophageal (T es) temperatures. The esophageal thermocouple was inserted using the following procedure: a light covering of 7.5% benzocaine gel was placed on the distal end of the thermocouple. A single spray of topical anesthetic (cetacaine, 14% benzocaine, Cetylite Industries, INC. Pennsauken, NJ) was sprayed onto the back of the throat. After a few minutes, the participant, with verbal instructions, advanced the esophageal probe up through the nose and to the pharynx. At this point the probe was withdrawn slightly, the participant was then requested to drink water at the same time the probe was advanced into the esophagus to a length equal to one-fourth of the participant’s supine height, and then the wire was taped to the nose (Gass et al. 1988). A flexible rectal thermocouple (T rec) probe covered by a sterile sheath was self-inserted ~8 cm beyond the anal sphincter. The rectal probe was securely taped, and the thermocouple wire was passed over the back of the wheelchair to minimize interference.
Skin temperature (T sk) was continuously monitored from thermocouples placed at the following sites: forearm, upper-arm, back, chest, thigh, and calf. These sites were chosen to adequately represent both upper- and lower-body skin temperature changes. Thermocouples were attached to the skin using adhesive tape that was cut around the thermocouples so as not to add insulation. Mean skin temperature (M skmean) and temperature weighting was calculated using the equation of Ramanathan (1964). T rec, T sk, and T es temperatures were recorded using a digital meter (TH-8, Physitemp Instruments, Inc. NJ, USA) every minute for the duration of the exercise protocol. Heart rate (HR) was recorded using an HR monitor (Polar, Stamford, CN, USA). Rating of perceived exertion (RPE) was assessed and differentiated between overall (RPE-O), arms (RPE-A) and chest (RPE-C) in which participants were asked to estimate their feelings of exertion every minute using a 6–20 numerical scale (Borg 1973). Participants were asked to differentiate their rating of perceived exertion between their overall, chest (breathing) and arms (Pandolf 1982). Participants were also asked to rate their thermal sensation level (Robertson 2004).
The exercise test consisted of 7-min stages beginning at a work load of 30 W. At the end of each stage, participants had a 1-min passive recovery where they were asked to spray themselves, as per usual competitive game procedure, with water, using a commercially available (340 ml) spray bottle (Apothecary Products, Minneapolis, MN). Participants were required to spray themselves ad libitum during the standardized 1-min rest periods. They were not told to spray any particular areas, just to spray themselves.
Resistance for each exercise stage was increased by 20-W increments until heat production exceeded heat dissipation. The test was terminated if a rise in T es of more than 0.2°C/min was observed, or the participant voluntarily terminated the test. Participants were asked to maintain 60 rev/min throughout the entire test.
CON lab trial
The control trial was completed in exactly the same way as the SB trial; however, participants were not permitted to use the spray bottle during their 1-min recovery periods. CON and SB were counterbalanced to control for effects of ordering.
Statistical analyses
SB and CON trials were compared using within-subjects, repeated-measures ANOVA for each dependent variable: watts, T rec, T es, T skmean, RPE, heat storage, HR. T skmean was calculated using an unweighted average temp of all T sk (forearm, back, chest, thigh, and calf) (Price and Mather 2004). T skmean was calculated using the formulae of Ramanathan (1964). A Bonferroni post hoc procedure was utilized. Results were considered significant at alpha <0.05. T sk for upper body was calculated using a weighted average of forearm (20%), chest (40%), and back (40%), whereas lower-body T sk was calculated as thigh (60%) and calf (40%).
Results
Physiological responses
Table 1 presents the physiological data obtained from the peak arm ergometry as well as anthropometric measurements. As can be seen in Fig. 1, the mean total work performed was similar (p = 0.86) for the spray bottle and CON trials (2,495.7 ± 914.6 vs. 2,407.1 ± 982.3 kJ, respectively). Likewise, the mean work times were similar between trials (27 ± 6 min and 26 ± 7 min for SB and CON, respectively).
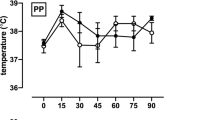
Throughout the exercise protocol, T rec for SB and CON followed a similar pattern. As apparent in Fig. 2, repeated-measures ANOVA showed no significant difference between trials (p > 0.05). Furthermore, as seen in Fig. 3, there were no significant differences detected between trials for T es (p > 0.05). Significant changes in HR occurred over the ~27 min of exercise for both conditions. As seen in Fig. 4, repeated measure ANOVA revealed no significant difference for HR response across time between CON and SB. HR, at rest was similar for SB (117 ± 17 beats/min) and CON (117 ± 9 beats/min); however, increased significantly by the end of the exercise period SB (160 ± 9 beats/min) and CON (168 ± 16 beats/min). Similarly, there was no statistically significant difference detected between SB and CON for mean skin temperature across time (p > 0.05). However, there was an observed trend (p = 0.067) indicating that the application of artificial sweat resulted in slightly less heat strain than for the control.
Perceptual responses
Repeated-measures ANOVA revealed no significant differences between SB and CON for RPE-O, RPE-A and RPE-C (p > 0.05). Similarly, there was no significant difference between SB and CON for thermal sensation; however, a trend toward a split in thermal comfort sensation (Fig. 5) toward the conclusion of the exercise bout can be observed.
Discussion
The aim of this study was to identify the point where artificial sweat would be ineffective in attenuating the rise in core temperature. Although there have been other studies that have observed effectiveness of exogenous cooling mechanisms for athletes with SCI, the approach of this particular study was to look at a cost effective, non-invasive, and popular field-cooling method. The mean total work performed was similar during the SB trial. Likewise, the mean work times were similar between SB and CON trials. The duration of the protocol in the present study was consistent with previous studies done using SCI athletes (Price and Mather 2004; Webborn et al. 2005) and approximates the actual play time for a basketball half.
In the current study, a ramped protocol was employed, in order to elicit continuous metabolic stress to elicit a rise in core temperature. However, we selected environmental conditions simulating a climate-controlled gymnasium to enhance the ecological validity. Consequently, we observed a smaller rise in core temperature compared to previous research studies (Dawson et al. 1994; Hopman et al. 1993), which have used constant intensity protocols in a hot environment (~38 ± 70% rh).
Webborn et al. (2005) looked at SCI athletes during intermittent exercise bouts in the heat using a pre-cooling and during-exercise cooling. All participants in that study were cooled via a commercially available cooling vest and placed in a warm environment (32 ± 0.1°C). Participants underwent 26 min of passive rest prior to their intermittent exercise bout of 28 min duration. The “during” cooling treatment and the pre-cooling treatments elicited significantly lower core temperature measures (36.5 ± 0.6 and 37.0 ± 0.5°C). Participants underwent 28 min of intermittent sprint exercise (compared to ~27 min in present study) which elicited a greater response, as the mechanism (commercially available ice vest) for cooling was much more aggressive than that of the current study. However, the practicality of “pre” and “during” cooling vests does not quite fit the paradigm of wheelchair basketball and other sports, where donning a cooling vest would hinder performance of the players. The time utilized to provide exogenous cooling during the current study was limited to the 1 min during rest periods between each 7-min stage. Three out of the seven participants showed no improvement at all in work capacity between trials using the spray bottle (Fig. 1). This is indicative of the individual differences experienced within the participant cohort. However, four of the eight subjects improved slightly, which is evidence that the effectiveness of an artificial sweat application could be investigated further. Whereas the aggregate data show no significant differences, if a spray bottle is effective, or perceived to be effective, for an individual, the lack of statistical significance should not preclude spray bottle use for such a person. We did not note any harm from the use of sprayed water.
The current study observed no difference in M sk temperature; however, there was a slightly lower (p = 0.067) skin temperature observed for the spray bottle (Fig. 6). The small difference between treatment and control could have been due to the amount of clothing worn by the athletes, and the consequent limited the amount of surface area that was sprayed and therefore, available for evaporative cooling. Furthermore, the sprayed water was not refrigerated; therefore it was of typical tap water temperature (±17°C). The thermal mass of the sprayed water was low, but colder water might have improved comfort.
Tsk was measured at five sites: two lower-body sites (calf and thigh) and three upper body sites (forearm, back, and chest). The consequence of these changes is difficult to identify, although two of the three participants with the highest level spinal cord lesions demonstrated quite a different trend from the rest of the participants who had lower level spinal cord lesion. The cutaneous thermoregulatory response, which is reflected by skin temperature measures, is subject to large individual variation, particularly in lower level spinal cord lesions (Normell 1974). The individual difference could be indicative of a change in the arrangements of the sympathetic outflow, and in the extent of reinnervation, in response to exercise (Normell 1974). Participants with the highest and complete spinal cord lesion level are less able to vasodilate or sweat in the calf region in response to central effecter stimulus (Gass et al. 1988). It has been suggested that for AB participants vasodilation of vessels in the skin is the result of withdrawal of sympathetic vasoconstriction, which could be linked to sudomotor activity (Rowell 1986).
It is also possible that the practical exercise challenge, and ecologically valid environmental conditions utilized in this study played a larger part in minimizing thermal strain than did the intervention. Similar, core temperature responses, between SB and CON, suggests that the cooling technique applied did not result in central cooling. Similar HR suggests that SB did not reduce cardiovascular strain either (Fig. 4).
Armstrong et al. (1994) hypothesized that the intervention of two cooling mechanisms, ice vest and refrigerated head piece, would result in significantly lower body temperature and physiological strain in their SCI participants; however, similar to the current study, they found no significant difference between treatments when compared to control. All subjects were thoracic-12 to cervical-6 wheelchair athletes. Likewise, in the current study it was observed that the changes in skin temperatures did not reach significance between the treatment (artificial sweat application) and the control. However, in the present study, there was little difference between T rec and T es measures, which is consistent with Price and Mather (2004) and Armstrong et al. (1994).
In our study, athletes limited their spray area to their back of the head, neck, forearms and faces. These areas represent a very small surface area available for evaporation. Furthermore, athletes were asked to wear similar game playing clothing, which was a further hindrance to maximizing skin surface area available for evaporation, but maintained ecological validity. It has also been found that cooling the torso and the upper-arms had no effect on thermal strain during upper-arm ergometry in AB athletes in warm conditions, due to the cooling of only a small segment (6%) of the body surface area (Young et al. 1987).
This study had limitations. The nature of the protocol and environment (22 ± 1°C, 45–50 ± 0.1% relative humidity), were selected to represent a typical wheelchair-playing environment. As mentioned previously, participants limited their spray area to what they were accustomed to during typical game play situation. The limited surface area available for artificial sweat application, due to clothing could have further hindered the magnitude of effect from the spray bottle. Furthermore, the water used in the spray bottle was not refrigerated prior to or during the protocol and was therefore typical tap water temperature (+17°C).
Further research is needed to identify more effective, practical ways of enhancing heat dissipation in SCI athletes. Looking at dispersing artificial sweat over a larger body surface area might be more effective during a constant intensity or longer duration exercise bout than used in the current investigation.
Conclusion
In summary, the current study examined the thermoregulatory response to artificial sweat application during upper-body high-intensity exercise using the application of water misting. In a simulated gymnasium temperature environment it appears that the cooling strategy employed had little effect on attenuating the rise of core temperature. Furthermore, there was also little affect on cardiovascular strain and perceptual responses. However, this continues to be a common method of cooling for SCI athletes playing wheelchair basketball.
References
Armstrong LE, Maresh CM, Riebe D, Kenefick RW, Castellani JW, Senk JM, Echegaray M, Foley MF (1994) Local cooling in wheelchair athletes during exercise-heat stress. Med Sci Sports Exerc 27:211–216
Borg GAV (1973) Perceived exertion: a note on history and methods. Med Sci Sports Exerc 5:90–93
Dawson B, Bridle J, Lockwood RJ (1994) Thermoregulation of paraplegic and able bodied men during prolonged exercise in hot and cool climates. Paralegia 32:860–870
Gass GC, Camp EN, Nadel ER, Gwinn TH, Engel P (1988) Rectal and rectal vs. esophageal temperatures in paraplegic men during prolonged exercise. J Appl Physiol 64(6):2265–2271
Guttman WL, Silver J, Wyndham CH (1958) Thermoregulation in spinal man. J Physiol 142:406–419
Hagobian TA, Jacobs KA, Kiratli J, Friedlander AL (2004) Foot cooling reduces exercise-induced hyperthermia in men with spinal cord injury. Med Sci Sports Exerc 36:411–417
Hopman MTE, Oeseburg B, Binkhors RA (1993) Cardiovascular responses in persons with paraplegia to prolonged arm exercise and thermal stress. Med Sci Sports Exerc 25:577–583
Lenth RV (2006) Java applets for power and sample size (computer software). Retrieved 17 Nov 2006 http://www.stat.uiowa.edu/~rlenth/Power.
Marino F (2002) Methods, advantages and limitation of body cooling for exercise performance. Br J Sports Med 36:89–94
Normell LA (1974) Distribution of impaired cutaneous vasomotor and sudomotor function in paraplegic man. Scand J Clin Lab Investig 33:25–41
Pandolf KB (1982) Differentiated ratings of perceived exertion during physical exercise. Med Sci Sports Exerc 14:397–405
Petrofsky JS (1992) Thermoregulatory stress during rest and exercise in heat in patients with a spinal cord injury. Eur J Appl Physiol 64:503–507
Price MJ, Campbell IG (1997) Thermoregulatory responses of paraplegic and able-bodied athletes at rest, during exercise and into recovery. Eur J Appl Physiol 76:552–560
Price MJ, Campbell IG (2003) Effects of spinal cord lesion level upon thermoregulation during exercise in the heat. Med Sci Sports Exerc 35:1100–1107
Price MJ, Mather MI (2004) The effects of two cooling strategies during prolonged arm crank exercise in the heat. Med Sci Sports Exerc 75:220–226
Ramanathan NL (1964) A new weightings system for mean surface temperature of the human body. J Appl Physiol 19:531–533
Robertson RJ (2004) Perceived exertion for practitioners: rating effort with the OMNI picture system. Human Kinetics, Chicago, IL
Rowell LB (1986) Human circulatory regulation during physical stress. Oxford University Press, New York
Webborn N, Price MJ, Castle PC, Goosey-Tolfrey VL (2005) Effects of two cooling strategies on thermoregulatory responses of tetraplegic athletes during repeated intermittent exercise in the heat. J Appl Physiol 98:2101–2107
Young AJ, Sawka MN, Epstein Y (1987) Cooling different body surfaces during upper and lower body exercise. J Appl Physiol 63:1218–1223
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Tatsuo Watanabe.
Rights and permissions
About this article
Cite this article
Pritchett, R.C., Bishop, P.A., Yang, Z. et al. Evaluation of artificial sweat in athletes with spinal cord injuries. Eur J Appl Physiol 109, 125–131 (2010). https://doi.org/10.1007/s00421-010-1371-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-010-1371-4