Abstract
The effects of voluntary isocapnic hyperpnea (VIH) training (10 h over 4 weeks, 30 min/day) on ventilatory system and running performance were studied in 15 male competitive runners, 8 of whom trained twice weekly for 3 more months. Control subjects (n = 7) performed sham-VIH. Vital capacity (VC), FEV1, maximum voluntary ventilation (MVV), maximal inspiratory and expiratory mouth pressures, \({\dot{{V}}\hbox{O}_{{2{\rm max}}},}\) 4-mile run time, treadmill run time to exhaustion at 80% \({\dot{{V}}\hbox{O}_{{2 {\rm max}}},}\) serum lactate, total ventilation \({(\dot{{V}}_{\rm E}),}\) oxygen consumption \({(\dot{{V}}\hbox{O}_{2}),}\) oxygen saturation and cardiac output were measured before and after 4 weeks of VIH. Respiratory parameters and 4-mile run time were measured monthly during the 3-month maintenance period. There were no significant changes in post-VIH VC and FEV1 but MVV improved significantly (+10%). Maximal inspiratory and expiratory mouth pressures, arterial oxygen saturation and cardiac output did not change post-VIH. Respiratory and running performances were better 7- versus 1 day after VIH. Seven days post-VIH, respiratory endurance (+208%) and treadmill run time (+50%) increased significantly accompanied by significant reductions in respiratory frequency (−6%), \({\dot{{V}}_{\rm E}}\) (−7%), \({\dot{{V}}\hbox{O}_{2}}\) (−6%) and lactate (−18%) during the treadmill run. Post-VIH 4-mile run time did not improve in the control group whereas it improved in the experimental group (−4%) and remained improved over a 3 month period of reduced VIH frequency. The improvements cannot be ascribed to improved blood oxygen delivery to muscle or to psychological factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trained endurance athletes have a less fatigable ventilatory system than untrained persons (Johnson et al. 1996), yet even highly trained individuals are sensitive to inspiratory muscle fatigue (Babcock et al. 1996; Romer et al. 2002c). Voluntary isocapnic hyperpnea (VIH), a form of respiratory muscle training (RMT) that requires subjects to maintain high target levels of ventilation, improves respiratory muscle endurance (Markov et al. 2001; Stuessi et al. 2001; McMahon et al. 2002) and has been shown to improve cycling endurance (Boutellier et al. 1992; Boutellier and Piwko 1992; Markov et al. 2001; Stuessi et al. 2001; McMahon et al. 2002).
Some studies have failed to find RMT ergogenic. Reasons may include insufficient statistical power (Morgan et al. 1987; Fairbarn et al. 1991; Hanel and Secher 1991), inadequate training stimuli (Hart et al. 2001; Sonetti et al. 2001), the use of exercise tests insensitive to the effects of RMT (Fairbarn et al. 1991; Hanel and Secher 1991; Inbar et al. 2000; Hart et al. 2001), inadequate rest to allow the respiratory muscles to recover after intense training (Sonetti et al. 2001) or to training effects in the placebo group (Sonetti et al. 2001). On the other hand, some of the studies showing an ergogenic effect have been criticized for not employing placebo or control groups (Boutellier et al. 1992; Boutellier and Piwko 1992) or for not using repeated trials of constant workload performance outcomes to account for familiarization (Boutellier et al. 1992; Boutellier and Piwko 1992). Several controlled VIH trials have demonstrated improved endurance during constant-intensity “open ended” exercise protocols (Markov et al. 2001; Stuessi et al. 2001). Nevertheless, these tests have been criticized as being unreliable (Jeukendrup et al. 1996) and lacking external validity to human competitive situations (McConnell and Romer 2004). Time trials, conversely, are considered to have greater external validity and relevance for athletic performance (McConnell and Romer 2004). The few controlled RMT studies employing time trials have demonstrated statistically significant (3.1–4.7%) improvements in cycling (Sonetti et al. 2001; Romer et al. 2002a; Holm et al. 2004) and rowing (Volianitis et al. 2001) performance. Only one of these studies has employed VIH training (Holm et al. 2004) and none have studied running.
The mechanisms for the RMT ergogenic effect are not entirely clear. Studies have shown that RMT does not improve stroke volume (Markov et al. 2001), oxygen delivery (Stuessi et al. 2001) or dynamic airway function (Kohl et al. 1997). It is therefore likely that VIH causes the ergogenic effect by enhancing respiratory muscle function to make the ventilatory system more resistant to fatigue during exercise (Verges et al. 2006). Inspiratory pressure threshold (IPTL) RMT has been shown to increase respiratory muscle maximal force production and maximal velocity of shortening (Romer et al. 2002a, b, c) and both VIH (Boutellier et al. 1992; Boutellier 1998; Markov et al. 2001; Stuessi et al. 2001; McMahon et al. 2002) and IPTL (Inbar et al. 2000; Williams et al. 2002) training improve respiratory muscle endurance. Delaying respiratory muscle fatigue may attenuate reflex vasoconstrictor signals sent to the limb vasculature and improve locomotor muscle blood flow and lactate clearance during exercise (Harms et al. 1997; St Croix et al. 2000; Dempsey et al. 2006) and some studies have measured reduced lactates post-RMT (Spengler et al. 1999; Romer et al. 2002b). As exercise intensity increases to maximum, the work of breathing can require up to 10–15% of exercise \({\dot{{V}}\hbox{O}_{2}}\) (Aaron et al. 1992; Dempsey et al. 1996; Harms et al. 1998) and some (Boutellier et al. 1992; Boutellier and Piwko 1992) but not all (Spengler et al. 1999; Stuessi et al. 2001; Williams et al. 2002) studies have demonstrated reduced exercise ventilation after RMT. If RMT attenuates exercise ventilation, the reduced energy cost of breathing and/or reduced respiratory muscle blood flow requirements during exercise could make more blood and oxygen available to the limb muscles.
Runners have not been tested for the benefits of VIH RMT in a controlled study using either a constant intensity exercise test or a time trial. We therefore performed a placebo controlled trial to test the following hypotheses that (a) VIH RMT would improve the performance of competitive male runners during a treadmill run to exhaustion at 80% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) and during a 4-mile time trial run; (b) ventilatory and exercise performance measured 7 days post-VIH would be significantly improved when compared with both pre-VIH and 1 day post-VIH values and (c) a maintenance phase of reduced frequency RMT would preserve the improvements attained during the initial period of more intense RMT.
Methods
Subjects
A total of 22 experienced male distance runners participated in this study, 15 in the experimental VIH groups and 7 in the control group (Table 1). In the first phase, subjects were randomly allocated to the experimental (n = 8) or control (n = 7) groups. Both groups performed treadmill endurance and time trial runs before and after VIH but only the experimental subjects (n = 8) participated in a 3-month maintenance program of VIH twice per week with monthly time trial runs performed during the maintenance period. Upon completion of this phase, a second group of runners (n = 7) was recruited to specifically test the reproducibility of the treadmill endurance runs as well as the effects on treadmill endurance performance day 1 versus day 7 post-VIH. This method of recruitment was done to keep subjects’ time commitments reasonable so as to insure compliance. Subjects were recruited from the local running community. The study was limited to males as a requirement by the study sponsor. All had previous experience in long distance competitive running events and all maintained a regular training program (35–55 miles/week at a pace of 70–80% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\)). The University at Buffalo Human Subjects Institutional Review Board approved the study protocol which was applied in observance of the ethical standards of the 1964 Declaration of Helsinki. All subjects signed written informed consent and agreed to maintain their usual running routines constant for the duration of the study.
Baseline pulmonary function
All subjects delivered a medical history and underwent physical examination, including a resting electrocardiogram. Pulmonary function tests (PFT) were performed by spirometry (P.K. Morgan Ltd. Spiroflow, model #131, Gillingham, Kent, England).The following measurements were performed according to ATS (1987) standards: slow vital capacity (VC), forced expired volume in 1 s (FEV1) and 15 s maximum voluntary ventilation (MVV). A respiratory endurance test (RET) was performed with the same device as used for VIH. This was a timed isocapnic breathing test during which subjects were required to breathe at approximately 60% MVV using tidal volumes that were about 50% of VC at a breathing frequency of approximately 30 breaths/min until exhaustion (defined as inability to maintain the target ventilation) (Boutellier et al. 1992). Maximal inspiratory pressure (P Imax) at residual volume (RV) and expiratory pressure (P Emax) at total lung capacity (TLC) were measured with a manometer connected to a mouthpiece. A small hole in the manometer system generated a leak that prevented the use of buccal muscles to generate false pressure readings.
Baseline exercise performance
All subjects (n = 22) performed a progressive treadmill (Quinton Instruments Model #24–72, Seattle, Washington) test to exhaustion (see below) to determine \({\dot{{V}}\hbox{O}_{{2{\rm max}}}.}\) Preparing for these measurements, subjects warmed up on the treadmill for 2 min at 4 mph at 0% grade. After warm up, the speed was increased to 6.5 mph at a grade of 2.5% for 3 min. At 6.5 mph the grade was increased by 2.5% increments every 2 min until exhaustion. Expired gas was collected in Douglas bags and gas exchange \({(\dot{{V}}\hbox{O}_{2}\, {\rm and}\, \dot{{V}}\hbox{CO}_{2})}\) was analyzed for the last minute using a dry gas meter (Harvard Dry Gas Meter, Model #AH-50–6164, Harvard Apparatus Inc., Holliston, Ma) for expired volume. A mass spectrometer (MGA1100, Perkin-Elmer, Pomona, CA) analyzed gas concentrations at each successive work rate. Standard equations were used to calculate \({\dot{{V}}\hbox{O}_{2}}\) and \({\dot{{V}}\hbox{CO}_{2}.}\) The \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) was defined as a plateau in oxygen consumption (< 150 ml/min increase) despite increasing exercise intensity and a respiratory exchange ratio (RER) ≥ 1.1 (Franklin 2000). Exhaustion was defined as the inability of the subject to maintain the treadmill speed combined with a subjective sensation of exhaustion. The \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) value was used to determine the 80% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) treadmill workload (running speed for the endurance tests). During the treadmill run, expired gas collections were performed and analyzed at 5 min and every 15 min thereafter until exhaustion, and then a final measurement was made during the minute following exhaustion.
During the treadmill runs, cardiac output (Impedance method, CardioDynamics International Corp., BZ4110-101D, San Diego, CA), arterial O2 saturation (ear probe, Ohmeda Biox 3700, Boulder, CO) and end-tidal O2 and CO2 (mass spectrometer) were determined, recorded and analyzed by a BIOPAC Systems (MP150CE, Goleta, CA) coincident with the measurements of oxygen consumption.
Experimental (n = 8) and control (n = 7) subjects performed a 4-mile time trial run on an indoor circular track [radius = 36.5 feet (11.12 m) and circumference = 229.22 feet (69.8 m)]. The total number of laps during the 4-mile run was recorded with an automatic lap counter and the run times were recorded to the nearest second. The subjects were unaware of these recordings and received no time cues or other information until all tests had been completed in all subjects. Subjects’ heart rates were recorded (Polar Heart Rate Monitor, Polar Electro Inc., Kempele, Finland) continuously during the treadmill and the 4-mile track runs.
Procedures
Three weeks before the start of the experiment, the following baseline measurements were completed in all subjects (n = 22): VC, FEV1, MVV, RET and maximal inspiratory and expiratory mouth pressures. The following performance tests were measured in the first experimental group (n = 8) and in the control group (n = 7): one treadmill endurance run to exhaustion at 80% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) and three repeat 4-mile track runs (attempting the shortest possible time, with the fastest time being used in the data analysis). All measurements and performance tests were repeated 7 days post-VIH, except that only two 4-mile track runs were performed. Repeated tests were separated by 1 week.
In addition to the baseline measurements described above, the second subset of experimental subjects (n = 7) performed two pre-VIH treadmill runs (separated by 1 week) and a 1-day post-VIH treadmill run (in addition to the 7-day post-VIH run). They performed mouth pressures and RET before and after VIH within a minute after completing the treadmill runs. These subjects did not perform the 4-mile time trial runs or participate in the maintenance phase. All subjects (n = 22) rested for 1 week after VIH to allow for recovery of the respiratory muscles (Boutellier et al. 1992; Kohl et al. 1997) although they continued with their weekly running routines.
Experimental VIH groups
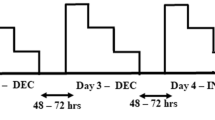
Upon completion of all baseline measurements, subjects (n = 15) started experimental VIH. The training was carried out using devices built in-house (Fig. 1). The purpose of these devices was (a) to prevent hypocapnia during voluntarily increased breathing, (b) to help the subject to adhere to a pre-selected breathing frequency and (c) to allow confirmation of protocol adherence by review of recordings on floppy discs of each VIH session in terms of date, duration, breathing frequency and the volume of the rebreathing bag. The adjusted volume of the rebreathing bag was entered manually into the computer by the subject at each session but could be verified at weekly review sessions with the subjects in the laboratory. Essentially, the devices provided for partial rebreathing of the expired air from the rebreathing bag, the volume of which was set at about 50% of the subject’s vital capacity. Taking breaths larger than the bag volume allowed inhalation of fresh air via a lightly spring-loaded valve and expiration of part of the alveolar air to the surroundings via another valve. Thus, it was possible for subjects to generate high levels of ventilation and adequate alveolar ventilation without dizziness (no hypocapnia) or shortness of breath (no hypercapnia) during 30 min long hyperpnea sessions. In a subset of ten subjects, normocapnia during VIH was verified by continuous analysis of end-tidal ventilation during VIH (mass spectrometer). The mean PCO2 for the ten subjects was 38 ± 4 mmHg. The mouthpiece/valve assembly was connected to a pressure transducer, which via a laptop computer, allowed recording on a floppy disk the subject’s breathing pattern. The computer generated a metronome signal (visual on screen and audio) to pace the subject’s breathing. The frequency was first set at 30 breaths/min so that, given the selected bag volume, the total ventilation amounted to about 50% of the subject’s MVV. This level of ventilation would typically be barely sustainable for 30 min at the beginning of the VIH period. On each training day the subject was required to increase the metronome-guided frequency by 1–2 breaths/min thus steadily increasing the training ventilation. The VIH was performed in the subject’s home for 30 min/day, 5 days/week for 4 weeks and the subject continued his weekly running routine. Once a week the VIH recording on the floppy disc was copied and the ventilatory performance and running mileage were reviewed by study staff in the laboratory. The subjects had been informed that this was done to check their adherence to the training protocol. In the first experimental group (n = 8), the schedule was changed after 4 weeks to reduce the total time spent on VIH. This “maintenance phase” lasted 3 months and consisted of doing VIH for 30 min, 2 days/week (separated by 2–3 days) at the highest ventilation level achieved during the preceding full-intensity VIH period. Each subject’s performance on the 4-mile track run was tested once a month during this 4-month period. Computer-stored VIH training records were reviewed on a monthly basis.
Control, i.e., sham-VIH group (n = 7)
Upon completion of all baseline measurements, subjects performed a modified VIH referred to as “sham-VIH”. Sham-VIH was performed on the same breathing device that the experimental group used, except that the mouthpiece and breathing valve device were not connected to a rebreathing bag. The control group underwent this placebo training for 4 weeks, which was designed so as to have a very low likelihood of affecting respiratory muscle performance. Each subject was instructed, using the breathing valve assembly (without the bag), to inhale, as timed by the computer program/recorder, to total lung capacity and hold his breath for 10 s. Breath holds were interspaced by rest intervals of normal breathing. This procedure was repeated every 90 s for 30 min during the first week. The rest interval was decreased to 80-, 70- and 60-s during weeks 2, 3 and 4, respectively. The training protocol for the control subjects was explained to them as based on a physiological hypothesis suggesting that a certain ventilatory pattern might enhance running performance. The training was practiced 30 min/day, 5 days/week for 4 weeks. During this time subjects continued their regular weekly running routines and running mileage was reviewed by weekly interview to confirm that they had maintained their customary training volume. Measurements in control subjects were obtained at baseline and after 4 weeks of sham-VIH. The respiratory training maneuvers of the control subjects were guided by and recorded by the computer, and reviewed by study staff, in exactly the same manner as for the experimental subjects. Control subjects did not perform a maintenance phase of respiratory training.
Twenty-four subjects initially agreed to participate (17 in the experimental groups and 7 in the control group). Two experimental group subjects (one in the first group and one in the second) were, however, unable to maintain their normal weekly running routine due to work conflicts or injury and their data have been excluded. All eight subjects in the experimental maintenance group subset participated in the 4-mile track runs.
Statistics
Baseline characteristics and pre- and post-VIH physiologic and exercise performance variables in both the experimental group and its subsets and the control group were tested for a significant difference in mean values using a Paired Student’s t test. A one way repeated measures ANOVA was used to evaluate the effect of VIH on 4-mile run times. Tukey’s HSD post hoc analysis was applied when the effect was significant. Reproducibility of treadmill run testing pre-VIH training was determined by Paired Student’s t test and the reproducibility of the 4-mile run times was calculated with an intraclass correlation coefficient (ICC). Physiologic and exercise performance differences between the experimental and control groups were analyzed with two-way repeated measures ANOVA and Tukey’s post hoc analysis of significant effects. All statistics were calculated using SPSS 11.5 (Chicago, Illinois). Probability values ≤ 0.05 were considered statistically significant.
Results
There were no statistically significant differences in anthropometrics, physiological data, pulmonary function, weekly running mileage (before, during and after VIH training) or initial performance times between the experimental and control groups (Table 1).
Treadmill run test reliability (n = 7)
The data for the two treadmill endurance runs to exhaustion prior to respiratory training are shown in Table 2. In summary, run time, \({\dot{{V}}\hbox{O}_{2}}\) averaged across the run time, post-exercise lactates, post-exercise mouth pressures and post-exercise RETs were not significantly different from the first to the second pre-VIH endurance runs. Steady state \({\dot{{V}}_{\rm E}}\) and heart rate were significantly reduced but by only 4 and 1%, respectively.
VIH training
The computer records demonstrated objectively that all of the experimental subjects used in the data analysis (n = 15) completed the intense respiratory training as prescribed. Experimental group subjects were able to significantly increase rebreathing minute ventilation and sustain it for 30 min during VIH from week 1 to week 4 as shown in Fig. 2. There were no significant differences in the rate of improvement in minute ventilation for subgroups of subjects that started below 100, about 100, or above 100 l/min.
Sham VIH
A comparison of the control group’s pre-sham VIH (Table 1) with the post-sham VIH (Table 3) values showed no significant differences in VC, FEV1, MVV, RET, \({\dot{{V}}\hbox{O}_{{2{\rm max}}},}\) treadmill run performance, \({\dot{{V}}\hbox{O}_{2}}\) or \({\dot{{V}}_{\rm E}}\) during the treadmill runs. Mean heart rate during the treadmill run (156 ± 7 vs. 154 ± 16 bpm (or beats/min)) also did not change after sham VIH.
Day 1 post-VIH results
Table 3 presents the results measured 1 day after completing VIH in the second experimental group (n = 7). Compared with pre-VIH values, treadmill run time increased significantly by 29%. There were significant but small reductions in \({\dot{{V}}\hbox{O}_{2}}\) (5%), lactate (18%) and HR (3%). While pre-run and post-run mouth pressures did not change significantly after VIH, the RET was significantly longer (91%).
Day 7 post-VIH results
The entire experimental group’s (n = 15) pre-VIH versus day 7 post-VIH within group values and the comparison with the control group (n = 7) are shown in Table 3. Comparing pre-VIH with day 7 post-VIH values in the experimental group, there were no significant changes in VC, FEV1 or FVC following the treadmill run; however, there was a significant increase in MVV (10%) and in the pre-run RET (122%). Neither maximal inspiratory nor expiratory mouth pressures measured before or after running changed significantly after VIH. The experimental group’s treadmill run time increased significantly by 50%, 7 days after VIH. Post-VIH \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) increased significantly, but by only a small percentage (3%). Cardiac output (22.97 ± 3.07 vs. 23.03 ± 3.72 l/min), stroke volume (142 ± 19 vs.143 ± 23 ml), heart rate (161 ± 16 vs. 161 ± 19 bpm) and O2 saturation (90 ± 3 vs. 90 ± 3%) did not vary significantly during the endurance runs and therefore were averaged as a function of time and were not significantly different post-VIH. Seven days post-VIH, the experimental group had significantly higher pre-run breathing endurance by 208% and treadmill running time by 50% when compared with the control group.
Figure 3 shows the reduction in breathing endurance induced by treadmill running before and 1- and 7-day after VIH in the second experimental subset (n = 7) of subjects. Both before and after VIH, breathing endurance was significantly reduced after the treadmill run. Although post-exercise respiratory endurance declined in VIH trained subjects (at both 1- and 7 days) it was nevertheless significantly greater than the level where non-respiratory trained subjects started pre-exercise; this despite up to a 50% greater treadmill running time.
The mean ±SD values of the respiratory endurance test (RET) are plotted as a function of run time for pre-voluntary isocapnic hyperpnea (VIH) (filled circle), 1-day post-VIH (filled inverted triangle) and 7 days post-VIH (circle) for prior to (0 min) and immediately after the treadmill run to exhaustion in the second experimental group of subjects (n = 7). The vertical error bars are for RET and the horizontal bars for running time. Asterisks indicate a significant difference (P ≤ 0.05) between pre- and post-exercise for each condition. † indicates a significant difference (P ≤ 0.05) between post-VIH and pre-VIH for RET
The increased treadmill run time 7 days post-VIH was accompanied by a significantly reduced average \({\dot{{V}}\hbox{O}_{2}}\) (6%) and \({\dot{{V}}_{\rm E}}\) (7%) (Table 3). The \({\dot{{V}}\hbox{O}_{2}}\) and \({\dot{{V}}_{\rm E}}\) are plotted as functions of treadmill run time in Figs. 4 and 5, respectively. As seen in these figures, both \({\dot{{V}}\hbox{O}_{2}}\) (by 6%) and \({\dot{{V}}_{\rm E}}\) (by 5%) significantly increased pre-VIH as a function of time. During the 7-day post-VIH runs measured at the same points in time as during the pre-VIH runs, neither \({\dot{{V}}\hbox{O}_{2}}\) nor \({\dot{{V}}_{\rm E}}\) had increased and they were lower at the maximal run time. Not at any time points in the runs were there differences in tidal volumes pre- to post-VIH (2.41 ± 0.33 l pre-VIH vs. 2.41 ± 0.49 l post-VIH). The reduction in \({\dot{{V}}_{\rm E}}\) was due to a significant reduction in breathing frequency post-VIH. The pre-VIH frequencies increased from 38 ± 5 breaths/min at 5 min into the run to 50 ± 5 breaths/min at the end of the run, while post-VIH the values increased from 37 ± 8 to 45 ± 6 breaths/min, respectively. End-tidal CO2 (43 ± 2.5 mmHg pre-VIH vs. 46.7 ± 1.7 mmHg post-VIH) was sustained at baseline levels during the endurance runs before and after VIH. Lactate levels were reduced by 18% after VIH.
Expressing the increased \({\dot{{V}}\hbox{O}_{2}}\) as a function of the increased \({\dot{{V}}_{\rm E}}\) during the pre-VIH run (figures 4 and 5) yielded an average value of 0.11 ± 0.01 ml/l/kg. Expressing the reduced \({\dot{{V}}\hbox{O}_{2}}\) as a function of the reduced \({\dot{{V}}_{\rm E}}\) post-VIH yielded a similar value of 0.080 ± 0.11 ml/l/kg.
When comparing the 1- and 7-day post-VIH experimental group data, there was a small but significant reduction in treadmill run \({\dot{{V}}\hbox{O}_{2}}\) day 7 compared with day 1 (Table 3). RET increased to 108% after day 7 compared with 85% after day 1 and RET after exercise was 20% higher after day 7 than day 1. The differences between days 1 and 7, however, did not achieve statistical significance. The treadmill run time increased by 24% on day 7 (60.6 ± 30.2 min) compared with day 1 (49 ± 20.56 min) but the difference did not quite attain statistical significance (P = 0.06).
Table 4 presents the 4-mile run data in the control and experimental subjects. The within group comparison showed that the experimental group ran significantly faster after VIH (4%), but there was no significant difference between the experimental and control groups. The experimental subjects, however, were running at a greater mean and last minute heart rate during the run after VIH compared with sham training.
Maintenance phase (n = 8)
The 4-mile run times increased significantly after the maintenance phase when compared with the initial post-VIH times (28.2 ± 4.47 vs. 27.59 ± 4.32 min, P = 0.008); however, the maintenance phase times still remained significantly lower than the pre-VIH times (27.59 ± 4.32 vs. 28.79 ± 4.35 min, P = 0.045).
Discussion
To our knowledge, this is the first controlled study to show that isocapnic VIH can improve both the breathing performance and the whole body exercise performance of competitive male runners during a laboratory treadmill run to exhaustion at 80% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}.\) There were no significant improvements in the control group’s breathing or exercise performance. Maximum oxygen consumption increased slightly (2%) but exercise heart rates, cardiac output, stroke volume and oxygen saturation did not change during the treadmill run after VIH. VIH therefore did not improve exercise performance by affecting oxygen transport or the aerobic fitness of the runners, which is consistent with the results of prior studies (Inbar et al. 2000; Markov et al. 2001). Oxygen consumption and serum lactates during the run were lower after VIH in association with reduced exercise breathing frequency and minute ventilation, suggesting that VIH reduced the work of breathing and/or improved ventilatory system efficiency. Immediate post-run breathing endurance improved significantly after VIH, consistent with reduced ventilatory system fatigue, and the VIH-trained runners ran 50% longer on the treadmill than before respiratory training. Our data also show that a period of respiratory muscle rest after VIH is required to observe its ergogenic effect.
In order to establish the benefit of VIH on running performance it was important to test the reproducibility of the laboratory treadmill run. The consistent results of the two pre-VIH runs to exhaustion showed that the 80% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) treadmill run was a reproducible measure of endurance performance in these runners. Gething et al. (2004) also demonstrated reproducibility between two cycling exercise trials at 75% \({\dot{{V}}\hbox{O}_{{2{\rm peak}}}}\) to exhaustion before inspiratory resistive loading (IRL) RMT.
VIH improved breathing endurance almost threefold when compared with runners performing sham-VIH. This highly significant improvement in respiratory endurance, coupled with the improved MVV after VIH, shows that the respiratory training was effective in enhancing ventilatory system performance. The “endurance” VIH employed in this study did not improve respiratory muscle strength (maximal inspiratory or expiratory pressures). Others have shown that resistive loading improves respiratory strength but not endurance (Leith and Bradley 1976; Fairbarn et al. 1991). Nor did VIH improve pulmonary airflows, which is also consistent with the findings of other studies (Hanel and Secher 1991; Kohl et al. 1997). Both before and after VIH, runners had reduced post-run breathing performance immediately after exercise when compared with pre-run values, consistent with ventilatory system fatigue. The post-VIH, post-run breathing performance values, however, were better than the pre-VIH, pre-run breathing performance values. This further supports the notion that VIH attenuated the exercise-induced reduction in breathing performance by reducing ventilatory system fatigue.
Although there was no significant difference between the VIH and control groups in 4-mile run performance, the significant VIH within group improvement (4%) is of equal magnitude as the time trial improvements reported in cyclists after both VIH (4.7%) (Holm et al. 2004) and IPTL (3.8–4.6%) (Romer et al. 2002a) and in rowers after IPTL (3.1%) (Volianitis et al. 2001). Using the energy cost of running during the treadmill runs, we calculated that the VIH subjects ran the 4-mile time trials at 85% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) pre-VIH and at 90% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) post-VIH. The mechanism for the improved 4-mile run performance of the VIH group may therefore relate to data which show that the diaphragm fatigues during exercise up to 90% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) (Johnson 1993; Johnson et al. 1993). We demonstrated that our VIH protocol prevented a decline in ventilatory system performance, which may be crucial to the ergogenic enhancement by RMT. The effect on time trial running performance is significantly less than that for the endurance run reported here and elsewhere (Boutellier et al. 1992; Boutellier and Piwko 1992; Spengler et al. 1999; Markov et al. 2001; Stuessi et al. 2001). The treadmill endurance and 4-mile runs are very different measures of running performance reflecting different aspects of exercise physiology. The treadmill run, performed at 80% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}},}\) is a measure of aerobic endurance whereas the 4-mile run, performed at approximately 90% of \({\dot{{V}}\hbox{O}_{{2{\rm max}}},}\) depends to a much greater degree upon anaerobic metabolism. At higher exercise intensities (> 85% of maximal) cardiovascular limitations impact exercise performance and (before respiratory system limitations become operative) RMT has been shown not to be effective (Morgan et al. 1987; Fairbarn et al. 1991; Inbar et al. 2000). It would therefore be expected that a short duration high intensity run would not improve to the same degree as a long duration lower intensity run.
While it has been claimed that the effects of RMT on exercise performance are psychological (Sonetti et al. 2001), our results and those of others (Volianitis et al. 2001; Romer et al. 2002a; Gething et al. 2004; Holm et al. 2004) suggest otherwise. One controlled study (Sonetti et al. 2001) that reported a lack of ergogenic effect of RMT was confounded by a significant improvement in the control group, contrary to our results and to those of other placebo controlled RMT trials (Volianitis et al. 2001; Romer et al. 2002a; Gething et al. 2004; Holm et al. 2004). Furthermore, the relatively modest respiratory and exercise performance improvement within the RMT training group in that study (Sonetti et al. 2001) was most likely the result of testing subjects only 1 day after completing a fatiguing course of mixed resistive and endurance RMT. Others have suggested (Boutellier et al. 1992), as also observed in the present study, that a period of respiratory muscle rest after RMT is required to observe the full ergogenic effect. In the present study, a subset of subjects tested 1 day after the end of RMT demonstrated modest improvements consistent with those reported by Sonetti et al. (2001). When re-tested post-VIH after a 7-day rest, however, the ergogenic effect was much greater and consistent with that reported by others (Boutellier et al. 1992; Boutellier and Piwko 1992; Spengler et al. 1999; Markov et al. 2001; Stuessi et al. 2001).
We measured a reduction in minute ventilation and oxygen consumption during the 80% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) treadmill run after VIH but not after sham-VIH. The reduced oxygen consumption during the post-VIH treadmill run is consistent with previously reported data for the energy cost of breathing (Levitzky 1995), suggesting that the post-VIH lower \({\dot{{V}}\hbox{O}_{2}}\) was a result of the reduced \({\dot{{V}}_{\rm E}}.\) An alternative hypothesis is that the post-VIH reduced \({\dot{{V}}\hbox{O}_{2}}\) was due to an increased running efficiency. It has been shown that during maximal exercise the respiratory load due to high-intensity contractions causes respiratory muscle fatigue and a sympathetically-mediated reduction in blood flow to locomotor muscles with resultant fatigue (Harms et al. 2000). It has also been shown that respiratory muscle fatigue produced by cycling at 90% of peak \({\dot{{V}}\hbox{O}_{2}}\) exacerbates exercise-induced quadriceps muscle fatigue and is associated with a significant reduction in peripheral muscle quadriceps twitch force (Romer et al. 2006). These data are consistent with the observation that fatiguing exercise impairs neuromuscular performance, which is believed to be due to, among other factors, fatigue-induced joint and muscle stiffness and reflex inhibition that reduce muscle maximal force production and time to peak tension (Komi 2000). The combination of these effects on locomotor muscle performance could have reduced running efficiency and increased the energy cost of running during the pre-VIH runs. Since VIH RMT has recently been shown to reduce the development of respiratory muscle fatigue during intensive exercise (Verges et al. 2006), an improved running economy may have resulted from better locomotor muscle performance associated with the VIH-induced reduction in respiratory muscle fatigue. There was, however, in the present study, no significant change in \({\dot{{V}}\hbox{O}_{2}}\) within each treadmill run as the subjects fatigued, before or after VIH, whereas there was a significant reduction in mean \({\dot{{V}}\hbox{O}_{2}}\) measured after VIH when compared with before VIH.
Prior studies of the effects of endurance RMT have been performed on cyclists. Of those demonstrating significantly improved cycling performance, some (Boutellier et al. 1992; Boutellier and Piwko 1992) but not all (McMahon et al. 2002; Holm et al. 2004) have reported a reduced exercise minute ventilation while none to our knowledge have reported a reduction in exercise \({\dot{{V}}\hbox{O}_{2}}\) post-VIH. Our results are unique perhaps because the energy cost of running is more sensitive to VIH than is the energy cost of cycling. Although exercise ventilation was reduced in our subjects after VIH, P ETCO2 and O2 saturation were sustained throughout the exercise, suggesting that adequate alveolar ventilation was maintained, which is consistent with the observation that a reduction in breathing frequency and not in tidal volume was responsible for the reduced ventilation.
In the only other study to examine the effects of RMT in runners, Williams et al. (2002) employed an uncontrolled design and found no ergogenic effect of inspiratory strength RMT on open-ended running performance. The performance effects of RMT, however, are sensitive to the type of RMT employed and to the exercise test utilized (McConnell and Romer 2004) and may explain the discrepant results between their study and ours. Their subjects ran at a greater exercise intensity (85% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\)) than ours and therefore ran less than 20 min both before and after inspiratory resistive training, consistent with the observation that RMT is less effective at near maximal exercise intensities.
We had objective proof (via the computer records of ventilatory performance) that the subjects completed the prescribed intense respiratory training. Electronically documented compliance with the training regimen has been shown to be critical for the ergogenic effects of IPTL (Romer et al. 2002a, c). Improvements in tests requiring volitional effort may also be due to learning effects. There was, however, very little variability in either our experimental or control runners during the repeated 4-mile time trials prior to VIH (intraclass correlation coefficients were 0.9851 and 0.9988 for the experimental and control groups, respectively). This suggests that there was no significant learning effect to account for improved performance after VIH. The profound improvement of treadmill endurance time in the experimental group 7- versus 1 day after VIH, when compared with the lack of improvement in the control group, strongly suggests that the effects of VIH were not the result of random variation or a placebo or learning effect.
Most studies have shown improved respiratory and locomotor muscle performance after both resistive and endurance RMT and those results do not appear to be explainable on the basis of deficiencies in the study protocols. A practically important but open question is whether the effects of RMT are sustainable at a reduced training frequency. In answer to this, we found that a significant improvement in the 4-mile run times persisted during the maintenance period when the frequency of VIH was reduced to twice per week.
In summary, 4 weeks of VIH significantly improved the overall ventilatory capacity and the 80% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\) treadmill running performance of competitive male runners when compared with a control group performing sham VIH. There was a significant within group improvement in 4-mile run performance after VIH. Our data suggest that 7 days of rest from ventilatory training following the intense 4 week VIH is important to reveal the ergogenic effect gained by VIH and that this gain can be maintained during a subsequent period of reduced frequency VIH training. The data are consistent with the interpretation that the ergogenic effect was the result of improved ventilatory system performance and not the result of cardiovascular adaptations or a placebo effect. Taken together, the performance data in cyclists and in our runners show that various forms of RMT have a sliding scale of effectiveness that inversely parallels exercise intensity: more effective at lower exercise intensities (< 85% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\)), less effective at higher intensities (85–90% \({\dot{{V}}\hbox{O}_{{2{\rm max}}}}\)) and ineffective at closer-to-maximal efforts.
References
(1987) Standardization of spirometry—1987 update. Statement of the American Thoracic Society. Am Rev Respir Dis 136:1285–1298
Aaron EA, Seow KC, Johnson BD, Dempsey JA (1992) Oxygen cost of exercise hyperpnea: implications for performance. J Appl Physiol 72:1818–1825
Babcock MA, Pegelow DF, Johnson BD, Dempsey JA (1996) Aerobic fitness effects on exercise-induced low-frequency diaphragm fatigue. J Appl Physiol 81:2156–2164
Boutellier U (1998) Respiratory muscle fitness and exercise endurance in healthy humans. Med Sci Sports Exerc 30:1169–1172
Boutellier U, Piwko P (1992) The respiratory system as an exercise limiting factor in normal sedentary subjects. Eur J Appl Physiol Occup Physiol 64:145–152
Boutellier U, Buchel R, Kundert A, Spengler C (1992) The respiratory system as an exercise limiting factor in normal trained subjects. Eur J Appl Physiol Occup Physiol 65:347–353
Dempsey JA, Harms CA, Ainsworth DM (1996) Respiratory muscle perfusion and energetics during exercise. Med Sci Sports Exerc 28:1123–1128
Dempsey JA, Romer L, Rodman J, Miller J, Smith C (2006) Consequences of exercise-induced respiratory muscle work. Respir Physiol Neurobiol 151:242–250
Fairbarn MS, Coutts KC, Pardy RL, McKenzie DC (1991) Improved respiratory muscle endurance of highly trained cyclists and the effects on maximal exercise performance. Int J Sports Med 12:66–70
Franklin B (ed) (2000) ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Williams
Gething AD, Williams M, Davies B (2004) Inspiratory resistive loading improves cycling capacity: a placebo controlled trial. Br J Sports Med 38:730–736
Hanel B, Secher NH (1991) Maximal oxygen uptake and work capacity after inspiratory muscle training: a controlled study. J Sports Sci 9:43–52
Harms CA, Babcock MA, McClaran SR, Pegelow DF, Nickele GA, Nelson WB, Dempsey JA (1997) Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol 82:1573–1583
Harms CA, Wetter TJ, McClaran SR, Pegelow DF, Nickele GA, Nelson WB, Hanson P, Dempsey JA (1998) Effects of respiratory muscle work on cardiac output and its distribution during maximal exercise. J Appl Physiol 85:609–618
Harms CA, Wetter TJ, St Croix CM, Pegelow DF, Dempsey JA (2000) Effects of respiratory muscle work on exercise performance. J Appl Physiol 89:131–138
Hart N, Sylvester K, Ward S, Cramer D, Moxham J, Polkey MI (2001) Evaluation of an inspiratory muscle trainer in healthy humans. Respir Med 95:526–531
Holm P, Sattler A, Fregosi RF (2004) Endurance training of respiratory muscles improves cycling performance in fit young cyclists. BMC Physiol 4:9
Inbar O, Weiner P, Azgad Y, Rotstein A, Weinstein Y (2000) Specific inspiratory muscle training in well-trained endurance athletes. Med Sci Sports Exerc 32:1233–1237
Jeukendrup A, Saris WH, Brouns F, Kester AD (1996) A new validated endurance performance test. Med Sci Sports Exerc 28:266–270
Johnson AT (1993) How much work is expended for respiration? Front Med Biol Eng 5:265–287
Johnson BD, Babcock MA, Suman OE, Dempsey JA (1993) Exercise-induced diaphragmatic fatigue in healthy humans. J Physiol 460:385–405
Johnson BD, Aaron EA, Babcock MA, Dempsey JA (1996) Respiratory muscle fatigue during exercise: implications for performance. Med Sci Sports Exerc 28:1129–1137
Kohl J, Koller EA, Brandenberger M, Cardenas M, Boutellier U (1997) Effect of exercise-induced hyperventilation on airway resistance and cycling endurance. Eur J Appl Physiol Occup Physiol 75:305–311
Komi PV (2000) Stretch-shortening cycle: a powerful model to study normal and fatigued muscle. J Biomech 33:1197–1206
Leith DE, Bradley M (1976) Ventilatory muscle strength and endurance training. J Appl Physiol 41:508–516
Levitzky MG (1995) Pulmonary physiology. McGraw-Hill, New York, p. 54
Markov G, Spengler CM, Knopfli-Lenzin C, Stuessi C, Boutellier U (2001) Respiratory muscle training increases cycling endurance without affecting cardiovascular responses to exercise. Eur J Appl Physiol 85:233–239
McConnell AK, Romer LM (2004) Respiratory muscle training in healthy humans: resolving the controversy. Int J Sports Med 25:284–293
McMahon ME, Boutellier U, Smith RM, Spengler CM (2002) Hyperpnea training attenuates peripheral chemosensitivity and improves cycling endurance. J Exp Biol 205:3937–3943
Morgan DW, Kohrt WM, Bates BJ, Skinner JS (1987) Effects of respiratory muscle endurance training on ventilatory and endurance performance of moderately trained cyclists. Int J Sports Med 8:88–93
Romer LM, McConnell AK, Jones DA (2002a) Effects of inspiratory muscle training on time-trial performance in trained cyclists. J Sports Sci 20:547–562
Romer LM, McConnell AK, Jones DA (2002b) Effects of inspiratory muscle training upon recovery time during high intensity, repetitive sprint activity. Int J Sports Med 23:353–360
Romer LM, McConnell AK, Jones DA (2002c) Inspiratory muscle fatigue in trained cyclists: effects of inspiratory muscle training. Med Sci Sports Exerc 34:785–792
Romer LM, Lovering AT, Haverkamp HC, Pegelow DF, Dempsey JA (2006) Effect of inspiratory muscle work on peripheral fatigue of locomotor muscles in healthy humans. J Physiol 571:425–439
Sonetti DA, Wetter TJ, Pegelow DF, Dempsey JA (2001) Effects of respiratory muscle training versus placebo on endurance exercise performance. Respir Physiol 127:185–199
Spengler CM, Roos M, Laube SM, Boutellier U (1999) Decreased exercise blood lactate concentrations after respiratory endurance training in humans. Eur J Appl Physiol Occup Physiol 79:299–305
St Croix CM, Morgan BJ, Wetter TJ, Dempsey JA (2000) Fatiguing inspiratory muscle work causes reflex sympathetic activation in humans. J Physiol 529(Pt 2):493–504
Stuessi C, Spengler CM, Knopfli-Lenzin C, Markov G, Boutellier U (2001) Respiratory muscle endurance training in humans increases cycling endurance without affecting blood gas concentrations. Eur J Appl Physiol 84:582–586
Verges S, LenHerr O, Haner A, Schulz C, Spengler C (2006) Increased fatigue resistance of respiratory muscles during exercise after respiratory muscle endurance training. Am J Physiol Regul Integr Comp Physiol (in press)
Volianitis S, McConnell AK, Koutedakis Y, McNaughton L, Backx K, Jones DA (2001) Inspiratory muscle training improves rowing performance. Med Sci Sports Exerc 33:803–809
Williams JS, Wongsathikun J, Boon SM, Acevedo EO (2002) Inspiratory muscle training fails to improve endurance capacity in athletes. Med Sci Sports Exerc 34:1194–1198
Acknowledgments
This study was funded in part by the US Special Operations Command, project#USZA2200C0002, Naval Sea Coastal Systems Contract 1031419-1-28298, UB Summer Medical School Research Fund and the Center for Research and Education in Special Environments. Skillful technical support from Messrs. Andrew Barth, Christopher Eisenhardt, Dean Markey, as well as the efficient administrative work by Ms. Dusti Dean is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leddy, J.J., Limprasertkul, A., Patel, S. et al. Isocapnic hyperpnea training improves performance in competitive male runners. Eur J Appl Physiol 99, 665–676 (2007). https://doi.org/10.1007/s00421-006-0390-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-006-0390-7