Abstract
It has been suggested that a critically high body core temperature may impair central neuromuscular activation and cause fatigue. We investigated the effects of passive hyperthermia on maximal isometric force production (MVC) and voluntary activation (VA) to determine the relative roles of skin (T sk) and body core temperature (T c) on these factors. Twenty-two males [V̇O2max=64.2 (8.9) ml kg−1 min−1, body fat=8.2 (3.9)%] were seated in a knee-extension myograph, then passively heated from 37.4 to 39.4°C rectal temperature (T re) and then cooled back to 37.4oC using a liquid conditioning garment. Voluntary strength and VA (interpolated twitch) were examined during an isometric 10-s MVC at 0.5°C intervals during both heating and cooling. Passive heating to a T c of 39.4oC reduced VA by 11 (11)% and MVC by 13 (18)% (P<0.05), but rapid skin cooling, with a concomitant reduction in cardiovascular strain [percentage heart rate reserve decreased from 64 (11)% to 29 (11)%] and psychophysical strain did not restore either of these measures to baseline. Only when cooling lowered T c back to normal did VA and MVC return to baseline (P<0.05). We conclude that an elevated T c reduces VA during isometric MVC, and neither T sk nor cardiovascular or psychophysical strain modulates this response. Results are given as mean (SD) unless otherwise stated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High environmental temperatures (Galloway and Maughan 1997) and internal heat storage (Gonzalez-Alonso et al. 1999) have both been demonstrated to accelerate fatigue during prolonged and voluntary submaximal exercise. Gonzalez-Alonso et al. (1999) observed that, despite different initial body core temperature (T c) or different rates of heat storage, highly fit subjects reached voluntary exhaustion at a similar 40.1–40.2°C oesophageal temperature. A consistent endpoint T c has also been reported in animals (Fuller et al. 1998; Walters et al. 2000), while Cheung and McLellan (1998) found a clear separation in endpoint T c between highly and moderately fit individuals, suggesting a benefit in heat tolerance through aerobic fitness.
The mechanisms underlying hyperthermia-induced exhaustion are not well understood. Recently, support has developed for the hypothesis that a critically high internal T c directly precipitates fatigue and can cause exhaustion. Nielsen et al. (1990) originally suggested that when exercising in a hot environment, a high T c (>39°C) causes fatigue through a direct effect on the central nervous system, since little difference existed in leg blood flow or oxygen consumption during exercise in either hot or cool conditions. Recent research from that laboratory has indeed demonstrated reductions in cerebral blood flow of approximately 20% (Nybo et al. 2002) along with frequency shifts in brain wave activity that occur at elevated hypothalamic temperatures (Nielsen et al. 2001). However, these cerebral changes occur prior to the impairment of exercise performance, and there is no existing direct causal evidence linking hyperthermia and central fatigue.
Only one study has demonstrated that the ability to generate force and voluntarily activate muscle in exercised (legs) and non-exercised (hand) limbs during a prolonged MVC is reduced with hyperthermia after prolonged exercise in the heat in humans (Nybo and Nielsen 2001a). However, the use of both exercise and heat to elicit hyperthermia resulted in near maximal cardiovascular strain, with heart rates exceeding 95% of maximum predicted values. Together, the combination of changes in hydration, cardiovascular strain, and baroreceptor feedback could be such that the critical temperature at fatigue was coincidental with high cardiovascular strain and not directly causing fatigue. In this same study (Nybo and Nielsen 2001a) two subjects were also passively heated and the same fatigue trends were evident as in the exercise-induced hyperthermia experiment, though the low subject number makes it difficult to draw firm conclusions. In addition, the passive heating protocol used by Nybo and Nielsen (2001a) only heated subjects to an oesophageal temperature of 39°C, which was lower than the critical temperatures (~40°C) they reported to be coincidental with exhaustion. The heating protocols of this and other studies also preclude determining whether the hyperthermia-induced fatigue was a result of hot skin, a hot core, or some combination of both. Since skin temperature (T sk) can markedly affect cerebral blood flow (Wilson et al. 2002), it would seem important to investigate the influence of peripheral versus central thermal input on central fatigue.
It was therefore the purpose of this study to determine if passive hyperthermia impairs maximum voluntary isometric contractions and voluntary activation, and to determine the relative roles of T sk and T c on these factors. Specifically, this study examined the effects of passive hyperthermia on the ability of participants to elicit a maximal voluntary contraction of the quadriceps femoris muscle group. At T c intervals of 0.5°C during heating from 37.5 to 39.5°C (warm skin), and then during cooling back down from 39.5 to 37.5°C (cool skin) subjects performed 10 s of maximal isometric knee extensions with simultaneous assessment of voluntary activation. It was hypothesized that maximal isometric force production and voluntary activation would be impaired by hyperthermia, even with relatively low cardiovascular strain, and that both T sk and T c would interact to impair neuromuscular function.
Methods
This study was conducted following the Canadian Tri-Council Policy for the ethical treatment of human participants as part of the Helsinki Declaration II and institutional research ethics board approval was obtained prior to any experimentation.
Subjects
After signing informed consent, 26 males between 18 and 30 years of age participated in this study. Four of these subjects were unable to complete the heating protocol, reducing the sample size to 22.
Subject characterization
In an initial familiarization session both height (m) and nude body weight (kg) were taken and body fatness was estimated using skinfold measurements and a seven-site skinfold formula (Jackson and Pollack 1978). Subjects then performed a maximal graded exercise test on a treadmill in order to directly assess their aerobic power. The protocol began with a submaximal running pace that the subject thought they could maintain for 20–30 min. The treadmill grade was increased by 2° every 2 min until exhaustion. Heart rate was monitored continuously by a Polar Vantage NV heart rate monitor (Polar Electro, Port Washington, N.Y., USA). During exercise, subjects breathed into a mouthpiece to determine respiratory measures through open circuit spirometry. Expired air was sampled every 20 s using a TrueMax 2400 Metabolic Measurement System (version 3.3; Parvo Medics, Sandy, Utah, USA). Prior to the exercise test, the gas analyzers were calibrated with known oxygen (O2) and carbon dioxide (CO2) gas concentrations. The volume transducer was also calibrated with a 3-l syringe.
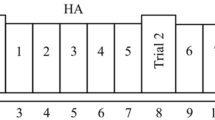
Experimental design
Subjects’ ability to produce maximal force and recruit the knee extensor was examined at T c intervals of 0.5°C spanning the range from normothermia (~37.5°C) to hyperthermia (~39.5°C). With each increase in T c of 0.5°C, the neuromuscular, cardiovascular and psychophysical status of the subjects was tested. Subjects were gradually warmed to a temperature of approximately 39.5°C by running fluid at 52°C through the tubing of a Liquid Conditioning Garment (LCG), with early termination upon (1) the subject’s request or (2) concern for the subject’s safety. After attaining a T c of 39.5°C, subjects were then cooled back down to their initial temperature by running fluid at 8°C through the LCG. Muscle force, voluntary activation (VA) and cardiovascular and psychophysical strain were then measured in an identical fashion to the warming protocol, again at every 0.5°C decrease in T c until a temperature of ~37.5°C was reached.
Thermal control
For the duration of the experimental session, testing was conducted in an environmental chamber set to sustain an ambient air temperature of ~35°C during the heating protocol. During cooling, the chamber was immediately turned off and the door opened to circulate room air into the chamber (~22°C). Body temperature (T b)was also controlled using a LCG (DTI, Ottawa, Canada). Subjects wore this LCG, which consisted of a 3-piece suit made of black elastic cotton that covered the head, neck, trunk and arms, and they also wore an impermeable rain suit over-top. Small polyvinyl chloride tubing (41.15 m×2.5 mm internal diameter and 4.2 mm outer diameter) is sewn to the inside of the LCG. In order to maximize heat exchange between the LCG and the participant’s skin surface, a form-fitting bathing suit or workout shorts (i.e. cycling spandex) were required for the testing session and no shirts were worn under the LCG. Water was pumped through the tube network during both heating and cooling using a pneumatic pump (DTI, Ottawa, Canada) at a flow rate of 800 ml min−1. Water temperature was controlled using a water heater with an accuracy of ~0.5°C.
Instrumentation
Heart rate was monitored throughout the experimental session using a 12-lead electrocardiograph (Quinton Instrument, Bothell, Wash., USA) and heart rate is expressed as a percentage of the range between resting and known maximum heart rate (heart rate reserve, HRR). Blood pressure was measured manually with a stethoscope and sphygmomanometer at each 0.5°C increment in T c. Both T c and T sk were monitored continuously over the course of this experiment using an 8-channel data logger (SmartReader 8 Plus; ACR Systems, Surrey, B.C., Canada) that sampled data every 8 s. Rectal temperature (T re) was monitored using disposable temperature probes (negative temperature coefficient thermistors) specifically designed for biological monitoring of T re (Mon-a-Therm General Purpose; Mallinckrodt, St. Louis, USA). Subjects were required to insert the rectal thermistor in the anal canal to a depth of 10 cm.
T sk was monitored at four sites (chest, upper arm, thigh, calf) using biomedical ceramic chip thermistors (MA 100, 10 kΩ negative temperature coefficient; Thermometrics, N.J., USA) and area-weighted mean T sk was subsequently calculated (Ramanathan 1964). Mean T c was calculated using a T c- and T sk-weighted formula: T b=(T re×0.65)+(T sk×0.35) (Ramanathan 1964).
To get a more accurate indication of the magnitude of physiological strain experienced by each of the subjects during the heating and cooling protocol, the physiological strain index (PSI) was calculated (Moran et al. 1998). This index runs from 0 (no/little strain) to 10 (high physiological strain). The PSI did not take into account changes in T sk; however, it was seen as a reasonable indication of overall strain combining heart rate and T c measurements. Additionally, the subjective comfort levels of the individual being tested were assessed. A rating of thermal comfort and a measure of thermal sensation were collected at every T c stage throughout the testing protocol (Gagge et al. 1967).
Hydration status
Naked body mass was determined at the start and end of the experimental testing session. Participants emptied their bladder before the testing session began and the amount of water consumed during the trial was monitored with the intention that all subjects were to remain normally hydrated. The amount of water available for each participant was unlimited; only the amount of fluid ingested and excreted was recorded. Sweat loss was not measured directly in this study; consequently only changes in body mass are reported.
Force and VA measurement
The testing protocol involved systematically measuring the participant’s maximum sustained (10 s) voluntary contraction (MVC) for unilateral knee extension with every T c change of 0.5°C. MVC was tested on a custom-made isometric knee extensor myograph. A sustained contraction of 10 s was used rather than the more usual 3–5 s MVC, because it has been previously demonstrated that VA is not impaired in the first 5 s of a sustained MVC with exercise induced hyperthermia (Nybo and Nielsen 2001a). The right leg was attached to a metal plate lined with high-density foam coupled to a force transducer (ST-250; Precision Transducers, Castle Hill, Australia), upon which the participant exerted their maximal isometric knee extension. Straps were also placed around the chest and right thigh at the time of contraction to ensure that any extraneous movements were restricted. Force signals were amplified, sent through an A/D board and sampled at a frequency of 2 kHz by data-acquisition hardware (DI-720; DATAQ Instruments, Akron, USA) and software (Windaq; DATAQ Instruments, Akron, USA). The average MVC force was calculated as the average force between the 1st and 9th second of the contraction, excluding the interpolated twitches and corresponding antidromic effect the stimulation procedure elicited in some subjects.
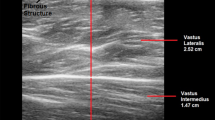
VA of the knee extensors was determined using percutaneous muscle stimulation and the interpolated twitch technique. The muscle stimulation protocol used a supramaximal 200 μs duration square-shaped pulse delivered to the knee extensors using a modified constant current (maximum 1 A) electrical stimulator (Digitimer DS7A; Hertfordshire, UK). Carbon rubber electrodes (5.08×10.2 cm) were placed both proximally (anode) and distally (cathode) on the thigh. The intensity of the supramaximal pulse was determined at the start of the experiment by increasing the current of the stimulus in 25-mA increments (beginning at 25 mA) until no further increase in twitch force was observed. To determine VA a supramaximal stimulus was delivered twice during each MVC (coincident with visually identified peak force levels and usually between 3 and 7 s) and immediately after each MVC. VA was calculated in the standard fashion (Merton 1954) as:
The superimposed twitch used was the smaller of two twitches elicited over the MVC so as not to underestimate central activation. The control twitch was the twitch elicited immediately (5 s) after the contraction. Contractile characteristics of the knee extensors (peak twitch force, time to peak force and half-relaxation time) were also calculated from the control twitch at each T c level.
Data analysis
Mean and standard deviation were used to describe all data. A one-way repeated measures analysis of variance (ANOVA) was used to determine whether T b influenced the ability to maximally produce force and activate the knee extensors. Bonferroni post hoc comparisons were used to determine where specific differences occurred when a significant main effect was present. Due to the number of potential significance tests that could be run, the analysis was limited to contrasting four thermal states: (1) initial T c and T sk; (2) hot T c, hot T sk; (3) hot T c, cool T sk ; and (4) end of the protocol where T c returned to normal and T sk was cool. All statistics were protected from type I error at the P<0.05 level of significance. Statistical analysis was performed using the statistical software package SPSS version 9.0 for Windows (SPSS, Chicago, Ill., USA).
Results
Twenty-two men completed the heating and cooling protocol used in this study. Five of these subjects requested the heating session end when their T c reached 39.0°C. The physical characteristics of these five men [mean (SD): age 22 (3) years, 1.79 (0.04) m height, 73.0 (11.1) kg mass, 1.90 (0.12) m2 body surface area, 8.2 (5.2)% body fat, 63.1 (4.7) ml kg−1 min−1 V̇O2max) were similar to the characteristics of the 18 men that were able to tolerate core heating to 39.5°C [age 22 (3) years, 1.79 (0.08) m height, 72.3 (8.7) kg mass, 1.90 (0.15) m2 body surface area, 8.2 (3.6)% body fat, 64.5 (9.8) ml kg−1 min−1 V̇O2max) . These five have been included in the mean data, but have been dropped (listwise comparison) in the ANOVA analyses, which include the 18 subjects reaching the highest T c (39.5°C).
Thermal strain
The mean total time spent in the chamber for all subjects was 153.3 (18.5) min, with 82.6 (15.7) min passive heating time and 74.3 (15.3) min cooling time. During the heating protocol, T re increased (P<0.001) from 37.3 (0.3)°C to 39.4 (0.1)°C for 17 of the 22 subjects, with 5 individual’s T c increasing to 39.0 (0.1)°C, at which point they requested termination of the heating portion of the experiment. T sk also rapidly increased (P<0.001) with the heating protocol from its initial temperature of 35.4 (0.7)–40.3°(0.4)°C. With the introduction of active cooling, T sk was rapidly reduced [32.7 (2.2)°C] and T c became slightly more elevated [39.6 (0.2)°C], but generally stable. This allowed us to partition the separate effects of elevated T c and T sk on neuromuscular function. With further cooling T c returned to normal by the end of the protocol and T sk decreased to 26.3°(2.3)°C, a significantly lower value (P<0.01) than that of the starting T sk. T b mirrored the changes observed in both the T re and T sk measurements. T b increased from 36.6°(0.3)°C to 39.7°(0.2)°C before decreasing to 33.6°(0.8)°C by the end of the protocol (P<0.001) (Fig. 1).
In addition to T b, changes to both the thermal comfort and thermal sensation of subjects were significantly influenced by passive heating and cooling (P<0.001). Specifically, thermal comfort was markedly worsened with passive heating, but returned quickly to baseline with the initiation of cooling, even though T c remained elevated. With further cooling thermal comfort worsened, but never approached the same level of discomfort as during hyperthermia. Thermal sensation generally mirrored the changes in T sk (Fig. 2).
Cardiovascular strain
HRR increased from 11.1 (10.5)% to 64.4 (10.9)% during passive heating (P<0.001). With the introduction of the cold water and the rapid skin cooling there was a substantial reduction in HRR (P<0.001), and by the end of the cooling period there was no significant difference in HRR when compared to the values at the start of the protocol, indicating a return to baseline. The heating and cooling protocol elicited no significant effect on mean arterial pressure (Fig. 3).
Physiological strain index
PSI significantly changed across the heating and cooling protocol. PSI increased significantly from start to hot (P<0.001) corresponding to a ‘high strain’ reading on the index. With the introduction of the cold water and the rapid reduction in T sk but not T c, PSI decreased significantly (P<0.001) to an average reading of 6.5±0.8 or ‘moderate strain’ and returned to baseline by the end of the protocol (Fig. 4).
Hydration status
Mean subject body mass pre and post-experiment slightly decreased from the start [70.7 (8.9] kg] to the end [69.8 (8.9] kg] of the protocol (P<0.001). In general, subjects lost 1.26 (1.14)% of their total body mass during the heating/cooling protocol.
Neuromuscular function
MVC was significantly influenced by passive heating and decreased significantly (P<0.05) from the start [322 (66) N] to the end of passive heating [281 (85) N]. Upon the introduction of skin cooling there was no significant change in MVC [283 (63) N] but MVC returned to its baseline value [322 (61) N] by the end of the protocol, once T c had returned to normal (Fig. 5, top). There were some changes in the contractile characteristics of the knee extensors over the course of the experiment. Although peak twitch force did not change over the course of the experiment half-relaxation time and time to peak twitch force decreased with heating and then returned to baseline with cooling (Fig. 6). Passive heating also significantly reduced VA from 83 (10)% to 72 (13)% (P<0.01). Upon the introduction of skin cooling there was no significant change in VA (75 (10%.) but VA returned to its baseline value [84 (6)%] by the end of the protocol, once T c had returned to normal (Fig. 5, bottom).
Discussion
The first major finding of this study was that MVC and VA were impaired by hyperthermia, even when cardiovascular strain was only moderate. Secondly, it appears that T c is the primary thermal input causing hyperthermia-induced fatigue, since when the skin was rapidly cooled (by ~8°C) and T c held stable at ~39.5°C, there was no recovery of MVC or VA, despite dramatic decreases in cardiovascular and psychophysical strain. Additionally, force and VA levels returned to baseline values upon core cooling, indicating the ability to activate the muscle and produce force was not depressed as a result of fatigue accumulating over the protocol, but likely directly influenced by T c. Thus, these data support the work done by Nybo and Nielsen (2001a), who found decreases in force production and VA in hyperthermic subjects, and expand on their findings by differentiating the influences of T c and T sk, and cardiovascular and psychophysical strain, on hyperthermic fatigue. It also differs from their study in that we observed force and VA decrements in short-duration maximum isometric contractions of only 10 s, whereas they only reported decrements after 30 s. This may be because of the larger sample size and greater statistical power in the present study.
Others have also reported decrements in isometric force production and muscle activation during hyperthermia (Ftaiti et al. 2001), but in that study the hyperthermia-induced fatigue was specific to isometric and slow velocity isokinetic muscle actions, and not present during higher velocity contractions. Another recent study (S.S. Cheung and G.G. Sleivert, 2004) has also reported that passive heating does not impair isokinetic force production, and it seems plausible that muscle activation deficits as a result of elevated T c are offset by the enhancement of muscle power through direct peripheral effects of an elevated muscle temperature. Further work is required to understand the interactions of T c and muscle temperature on neuromuscular function.
Typically, studies use exercise as a mean of increasing T c (active hyperthermia) before testing the influence of temperature on various measures of cardiovascular and neuromuscular function (Bigland-Ritchie et al. 1992; Ftaiti et al. 2001; Nybo and Nielsen 2001a). As previously stated, active hyperthermia can confound interpretation of the influence of temperature on neuromuscular fatigue because in addition to the high thermal strain, cardiovascular strain is usually very high. For example, Gonzalez-Alonso et al. (1999) reported heart rate values of 98–99% of maximum [198 (4) beats min–1] at exhaustion during their cycling protocol and other studies have used an experimental end-point of >95% heart rate during exercise in the heat (Cheung and McLellan 1998; Nybo and Nielsen 2001a; Selkirk and McLellan 2001). By using a passive heating protocol, we produced a heart rate of only 65% of HRR and thereby avoided maximal cardiovascular strain. Consequently, changes in force and VA could be attributed directly to changes in T c.
In the present study, maximum T rs were between 39 and 39.5°C, while in similar hyperthermia and exercise studies, oesophageal T c was reported to be ~40°C at the time of exhaustion (Gonzalez-Alonso et al. 1999; Nybo and Nielsen 2001a). Although these temperatures appear higher than the ones attained in this study, oesophageal temperature responds faster than T re to increases in T c, and oesophageal temperature is typically higher than T re (Moran and Mendal 2002). Other hyperthermia studies using rectal T c measurements have reported values coincident with the time of exhaustion as low as 38.6 (0.2)°C and 38.7 (0.2)°C in non-fit subjects (Cheung and McLellan 1998; Latzka et al. 1998). Therefore, the T cs attained in this study are consistent with others cited at exhaustion using active methods of inducing hyperthermia, although a direct measure of brain temperature would have been preferable, given that the brain is the most likely site for critical temperature effects.
It has been proposed that there is a threshold or critical internal temperature of approximately 40°C at which hyperthermia causes exhaustion (Ftaiti et al. 2001; Fuller et al. 1998; Gonzalez-Alonso et al. 1999; Nybo and Nielsen 2001a, 2001b; Walters et al. 2000), but our data would not support this. Figure 5 clearly shows that the decreases in MVC and VA with hyperthermia, and the subsequent return to baseline with cooling, appear to be gradual effects that are not clearly precipitated at a single high T c. There was no apparent threshold where VA dropped suddenly from normal values. Rather, decreases occurred throughout the heating protocol. The decreases in force and VA observed in the present study occurred at only moderate cardiovascular strain [64 (11)% of HRR] and our subjects were not dehydrated, therefore these factors should not have been the primary moderators of the diminished VA. Additionally, with the introduction of skin cooling HRR decreased substantially to 29 (11)% HRR even while T c remained elevated. Although stroke volume was not measured directly in this study, the decrease in HRR was probably a result of a restoration in stroke volume, which would have decreased during hyperthermia due to cutaneous blood pooling in the periphery (Rowell et al. 1969). Therefore, a substantial reduction in cardiovascular strain was observed during initial skin cooling, but this decrease had no effect on force or VA measures.
Since we did not observe any restoration of VA or MVC with skin cooling during hyperthermia (T re=39.5°C), it seems unlikely that T sk influences hyperthermic fatigue. Mean arterial pressure was not compromised in our subjects, and during exercise in the heat the muscle pump would maintain venous return. Therefore, in the absence of an orthostatic challenge, it is doubtful that skin cooling will minimize hyperthermia-induced fatigue. This is supported by the work of Gonzalez-Alonso et al. (1999) who studied a sub-sample of four subjects performing two cycle ergometer tests at high temperature (66% V̇O2max, 41°C) until volitional fatigue. The researchers manipulated trunk skin temperatures using a water-perfused jacket with water at 42°C and 19°C circulating to represent high and low rates of heat storage, respectively. Although muscle function via twitch interpolation was not directly measured, they observed rates of fatigue to occur at similar T c and muscle temperatures and different mean T sk [38.4 (0.4)°C versus 35.6 (0.2)°C]. The experimenters speculated that fatigue mainly responded to the rise of T c first, and to signals being sent from active muscles, the central nervous system or other internal organs second.
Although we did not measure muscle temperature, it is possible that it also could have influenced VA and MVC. Isometric force production has been shown to decrease when muscle temperature is elevated to 38.6°C (Edwards et al. 1972) and consequently a warmer muscle fatigues earlier than a slightly cooler muscle at the same absolute force. This is because the muscle twitch responds at a faster rate in the heat, and consequently it takes an increase in firing rate of the motor neurons at the same relative frequency to produce enough summation to maintain a given contraction over longer durations (Enoka 2002). Although muscle temperature was not measured directly in this study, half-relaxation time and time to peak twitch force for the knee extensors decreased with heating and this may have precipitated the need for a higher motor-unit firing frequency in order to maintain MVC. Thus, our results suggest that during hyperthermia the peripheral properties of a heated muscle may contribute to the reduction in MVC. Muscle temperature was measured in Nybo and Nielsen’s (2001a) experiment involving fatiguing contractions in both normothermic and hyperthermic states and they concluded that differences in muscle temperature did not influence the ability to produce a MVC and that an elevation in T c was the primary moderator for decreases in force production, but they did not report evoked contractile characteristics of the muscle, which may have been altered by their protocol.
Fatigue is a complex process that has been described as “a conscious awareness of changes in subconscious homeostatic control systems” (Gibson et al. 2003). It has been shown that electrical brain waves shift to a lower frequency, indicating a reduced state of arousal when prolonged exercise is performed in the heat (Nielsen et al. 2001). Indeed, if subjects perceive themselves to be more tired, hot, frustrated and weak, their rating of perceived exertion may be elevated at a given work rate and they may feel that they are producing maximal exertion when in reality they are not. Consequently force production and activation of a muscle may become impaired. Along these lines, an alternative explanation to that of a direct effect of a high T c accelerating fatigue has been recently proposed by Marino et al. (2004). These researchers observed that there was an anticipatory reduction in running speed of larger Caucasian athletes the moment they were exposed to running in hot conditions in which they could not maintain heat balance as well as in cool conditions. Thus, they slowed their running speed long before they became hot as predicted by the model of central fatigue resulting from the attainment of some limiting T b. These researchers propose that it is not so much a fatigue process that limits exercise performance in the heat, but an anticipatory regulation process influenced by rates of heat storage that is activated the moment exercise begins. This would prevent excessive heat production in hot conditions and ensure that a critical limiting T b is not reached prematurely during voluntary exercise. Our results would lend some support to this hypothesis as we observed a gradual reduction in MVC and VA as T b rose, not a sudden marked drop at some critical temperature.
The association between brain activity, perceived exertion and hyperthermia were explored by Nybo and Nielsen (2001b) who observed that there were differences in subjects’ perceived exertion during hyperthermia such that they had increased difficulty in maintaining power output. Perhaps the perception of difficulty is exacerbated by a hot brain, an ancient evolutionary defense mechanism that attempts to minimize heat injury to the organism by making the activity feel more difficult than it was before. Behavioral changes are often one’s first defense to prevent suffering heat illness and an increase in perceived exertion may be one strategy the brain uses to halt exercise. Various animals will cease exercise when their T c exceeds safe limits (Caputa et al. 1986; Taylor and Rowntree 1973) and there may be a similar response in humans.
We did not measure ratings of perceived exertion, because all trials required maximal effort, but it is possible that subjects perceived maximal effort was lower with hyperthermia. We did measure other psychophysical indices in this experiment, and there were dramatic increases in both thermal comfort and sensation scores with passive heating, followed by dramatic decreases towards baseline with the introduction of cooling. Even though skin cooling markedly reduced psychophysical strain, it had no immediate influence on VA or MVC; therefore, these data do not suggest that these psychophysical variables are important to hyperthermia-induced fatigue. These data do demonstrate however that skin plays an important role in the whole-body perception of how hot or cold one feels, regardless of actual T c, which is consistent with other hyperthermia studies in the literature (Cotter et al. 1996; Gagge et al. 1967).
In conclusion, we have clearly demonstrated that an elevated T c is the primary factor contributing to central fatigue during isometric contractions and hyperthermia, and that T sk, cardiovascular and psychophysical strain do not appear to be major modulators of hyperthermia-induced fatigue.
References
Bigland-Ritchie B, Thomas C, Rice C, Howarth J, Woods J (1992) Muscle temperature, contractile speed, and motoneuron firing rates during human voluntary contractions. J Appl Physiol 73:2457–2461
Caputa M, Feistkorn G, Jessen C (1986) Effects of brain and trunk temperatures on exercise performance in goats. Pflugers Arch 406:184–189
Cheung SS, McLellan TM (1998) Influence of heat acclimation, aerobic fitness, and hydration effects on tolerance during uncompensable heat stress. J Appl Physiol 84:1731–1739
Cheung SS, Sleivert GG (2004) Lowering of skin temperature decreases isokinetic maximal force production independent of core temperature, DOI 10.1007/s00421-004-1062-0
Cotter JD, Zeyl A, Keizer E, Taylor NAS (1996) The role of local skin temperature in determining the perception of local and whole-body thermal state. In: Shapiro Y, Moran DS, Epstein Y (eds) Environmental ergonomics: recent progress and new frontiers. Freund, London, pp 85–88
Edwards RH, Harris RC, Hultman E, Kaijser L, Koh D, Nordesjo LO (1972) Effect of temperature on muscle energy metabolism and endurance during successive isometric contractions, sustained to fatigue, of the quadriceps muscle in man. J Physiol (Lond) 220:335–352
Enoka R (2002) Neuromechanics of human movement, 3rd edn. Human Kinetics, Champaign, Ill.
Ftaiti F, Grelot L, Coudreuse JM, Nicol C (2001) Combined effect of heat stress, dehydration and exercise on neuromuscular function in humans. Eur J Appl Physiol 84:87–94
Fuller A, Carter RN, Mitchell D (1998) Brain and abdominal temperatures at fatigue in rats exercising in the heat. J Appl Physiol 84:877–883
Gagge AP, Stolwijk JA, Hardy JD (1967) Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res 1:1–20
Galloway SD, Maughan R.J (1997) Effects of ambient temperature on the capacity to perform prolonged cycling exercise in man. Med Sci Sports Exerc 29:1240–1249
Gibson ASC, Baden DA, Labert MI, Lambert EV, Harley YXR, Hampson D, Russell VA, Noakes TD (2003) The conscious perception of the sensation of fatigue. Sports Med 33:167–176
Gonzalez-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B (1999) Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol 86:1032–1039
Jackson AS, Pollack ML (1978) Generalized equations for predicting body density of men. Br J Nutr 40:497–504
Latzka WA, Sawka MN, Montain SJ, Skrinar GS, Fielding RA, Matott RP, Pandolf KB (1998) Hyperhydration: tolerance and cardiovascular effects during uncompensable exercise-heat stress. J Appl Physiol 84:1858–1864
Marino FE, Lambert, MI, Noakes TD (2004) Superior performance of African runners in warm humid but not in cool environmental conditions. J Appl Physiol 96:124–130
Merton PA (1954) Voluntary strength and fatigue. J Physiol (Lond) 123:553–564
Moran DS, Mendal L (2002) Core temperature measurement, methods and current insights. Sports Med 32:879–885
Moran DS, Shitzer A, Pandolf KB (1998) A physiological strain index to evaluate heat stress. Am J Physiol 275:R129–R134
Nielsen B, Savard G, Richter EA, Hargreaves M, Saltin B (1990) Muscle blood flow and muscle metabolism during exercise and heat stress. J Appl Physiol 69:1040–1046
Nielsen B, Hyldig T, Bidstrup F, Gonzalez-Alonso J, Christoffersen GR (2001) Brain activity and fatigue during prolonged exercise in the heat. Pflugers Arch 442:41–8
Nybo L, Nielsen B (2001a) Hyperthermia and central fatigue during prolonged exercise in humans. J Appl Physiol 91:1055–60
Nybo L, Nielsen B (2001b) Perceived exertion is associated with an altered brain activity during exercise with progressive hyperthermia. J Appl Physiol 91:2017–2023
Nybo L, Moller K, Voliantitis S, Nielsen B, Secher S (2002) Effects of hyperthermia on cerebral blood flow and metabolism during prolonged exercise in humans. J Appl Physiol 93:58–64
Ramanathan NL (1964) A new weighting system for mean surface temperature of the human body. J Appl Physiol 19:531–533
Rowell LB, Murray JA, Brengelmann GL, Kraning KK (1969) Human cardiovascular adjustments to rapid changes in skin temperature during exercise. Circulation 14:711–724
Selkirk GA, McLellan TM (2001) Influence of aerobic fitness and body fatness on tolerance to uncompensable heat stress. J Appl Physiol 91:2055–2063
Taylor CR, Rowntree VJ (1973) Temperature regulation and heat balance in running cheetahs: a strategy for sprinters? Am J Physiol 224:R848–R851
Walters TJ, Ryan KL, Tate LM, Mason PA (2000) Exercise in the heat is limited by a critical internal temperature. J Appl Physiol 89:799–806
Wilson TE, Cui J, Zhang R, Witkowski S, Crandall CG (2002) Skin cooling maintains cerebral blood flow velocity and orthostatic tolerance during tilting in heated humans. J Appl Physiol 93:85–91
Acknowledgements
The authors wish to express their gratitude to the subjects who participated in the experiments. The project was supported by a Discovery Grant (S.S.C. and G.G.S.) from the Natural Sciences and Engineering Research Council (NSERC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morrison, S., Sleivert, G.G. & Cheung, S.S. Passive hyperthermia reduces voluntary activation and isometric force production. Eur J Appl Physiol 91, 729–736 (2004). https://doi.org/10.1007/s00421-004-1063-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-004-1063-z