Abstract
This study determined whether four self-paced household tasks, conducted in the subjects’ homes and a standardised laboratory environment, were performed at a moderate intensity [3–6 metabolic equivalents (METs)] in a representative sample of thirty-six 35- to 45-year-old females. Energy expenditure was also predicted via indirect methods. Self-paced energy expenditure during sweeping, window cleaning, vacuuming and mowing was measured using the Douglas bag technique. Heart rate, respiratory frequency, Computer Science Applications (CSA) movement counts (hip and wrist), Borg rating of perceived exertion and Quetelet’s index were also recorded as potential predictors of energy expenditure. While the four activities were performed at mean intensities ≥3.0 METs in both the home and laboratory, all comparisons between these two environments were statistically significant (P<0.001). The 95% confidence intervals (CIs) for the home and laboratory prediction equations were ±1.1 METs and ±1.0 MET, respectively. These data suggest that the aforementioned household chores can contribute to the 30 min·day−1 of moderate-intensity activity required to confer health benefits. However, the substantial between-subject variability in energy expenditure resulted in some persons performing these tasks at a light intensity (<3.0 METs). The significant MET differences between the home and laboratory emphasise the effects of ‘environment and terrain’ and the ‘mental approach to a task’ on self-paced energy expenditure. Considering the means for the five activities ranged from 3.1 METs to 6.0 METs, the 95% CIs for the regression equations lack predictive precision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiological research has demonstrated the positive effects of regular physical activity on health outcomes. Health authorities (CDHAC 1999; Fentem and Walker 1994; Pate et al. 1995; USDHHS 1996) have therefore recommended that individuals accumulate at least 30 min of moderate-intensity physical activity [3–6 metabolic equivalents (METs), where 1 MET is ~resting oxygen consumption (V̇O2) of 3.5 ml·kg−1·min−1 or 4.2 kJ·kg−1·h−1] on 5–7 days of the week to reduce the risk of mortality from chronic illnesses, such as cardiovascular disease, non-insulin-dependent diabetes, hypertension and maybe some forms of cancer. Regular moderate-intensity physical activity has also been shown to be an effective treatment for depression (USDHHS 1996) and to assist weight control.
Despite strong evidence suggesting that regular physical activity can protect against several chronic diseases, national physical activity surveys (Armstrong et al. 2000) conducted in 1997, 1999 and 2000 found that the percentage of Australians not reaching the recommended levels of physical activity (150 min·week−1 of moderate exercise) had remained steady at ~40%. This statistic is compounded by the percentage of sedentary Australians (i.e. no physical activity) increasing from 13.4% to 15.3% over the same period. This level of physical inactivity in Australia has led to its classification as the second largest contributor (7%) to the total disease burden after smoking (10%) (Mathers et al. 2000). The corresponding direct health care cost has been estimated at $A 377 million per annum (Stephenson et al. 2000).
Although walking and household chores are commonly reported daily activities, the latter are not always included in the 150 min·week−1 (5×30 min) of moderate-intensity physical activity required to confer health benefits (Armstrong et al. 2000; Gill et al. 2001) because there is doubt as to whether these self-paced activities are performed at an intensity ≥3.0 METs. Recent research (Bassett et al. 2000; Hendelman et al. 2000; Strath et al. 2001; Sujatha et al. 2000; Welk et al. 2000) has addressed these concerns by measuring the energy expenditure during many household activities using portable metabolic measurement devices. However, no investigators have recently measured energy expenditure using the criterion Douglas bag technique and compared self-paced energy expenditure in the home with that in the laboratory environment. Furthermore, only one project (Luke et al. 1997) has examined whether energy expenditure of household activities can be predicted using more than one independent variable via grouped regression analysis. Small sample sizes (Bassett et al. 2000; Strath et al. 2001) and no control over the age-wise decrease in V̇O2max (Bassett et al. 2000; Strath et al. 2001) are further limitations of several recent studies.
Accurate age- and gender-specific energy expenditure data for commonly performed household activities could increase the validity of epidemiological surveys which convert reported activities into estimates of energy expenditure. Furthermore, physical activity surveys that include moderate-intensity household chores will facilitate a more accurate representation of physical activity prevalence in the population and will therefore enable surveys to more sensitively track physical activity trends over time.
This project addressed some of the limitations of previous studies and expanded our previous work on 35- to 45-year-old males (Gunn et al. 2003) by:
-
1.
Measuring the energy expenditure of four of the more intensive household activities (sweeping, window cleaning, vacuuming and mowing lawns) and moderate-paced walking, using the Douglas bag technique, in a representative sample of females aged 35–45 years.
-
2.
Comparing the self-paced energy expenditure of household activities performed in a standardised laboratory environment with that when the activities are performed in the subjects’ homes.
-
3.
Assessing energy expenditure of the household activities and walking expressed in METs and multiples of measured resting metabolic rate (RMR).
-
4.
Evaluating whether energy expenditure can be predicted by a weighted combination of independent variables [heart rate (HR), Computer Science Applications (CSA) accelerometer counts, respiratory frequency, Borg rating of perceived exertion and Quetelet’s index].
Methods
Subjects
Thirty-six Australian women [X̄ (SD) values for age, body mass and height were 39.9 (2.8) years, 66.5 (13.1) kg and 165.1 (5.9) cm, respectively] in the 35- to 45-year age range were recruited (Table 1) from advertisements placed on notice boards in shopping centres, libraries, community centres and universities. Some subjects were also recruited by word of mouth. The Australian Fitness Norms (Gore and Edwards 1992) were used as a guide to select a heterogeneous sample for height and body mass. The sample was screened to exclude: smokers, persons suffering from diseases or taking any medication known to affect energy metabolism and those with a history of any clinical eating disorder. The sample size (n=36) represents an adequate balance between cost effectiveness and precision for estimating the population means for 35- to 45-year-old females. This project was approved by the Clinical Research Ethics Committee of the Flinders Medical Centre. All experimental procedures, possible risks and benefits were explained to the subjects before their written informed consent was obtained.
Experimental design
Each subject was familiarised with the procedure and equipment for measuring RMR and energy expenditure during the activities. At least 1 day after this habituation, RMR was measured in the morning (between 7 and 9 a.m.) on 2 separate days within an interval of ≤10 days. Following RMR measurement on day 1, energy expenditure was measured during over-ground walking and four household activities in standardised conditions in the laboratory and its environs. After RMR measurement on day 2, energy expenditure was measured during four household activities in the subject’s home. Percent body fat (%BF), determined using dual energy X-ray absorptiometry (DXA), was measured within 1 week of energy expenditure measurement. Energy expenditure predictors (HR, respiratory frequency, CSA movement counts, Borg rating of perceived exertion) were recorded during all nine activities (four in the home and five in the laboratory). The order of the activities for each subject was randomised in accordance with a Latin square design and no tests were conducted when the ambient temperature exceeded 28°C.
Resting metabolic rate
Our method for measuring resting V̇O2 using the classical Douglas bag method, together with the procedure for subject preparation and controlling factors that are known to affect the metabolic rate, have been described previously (Gunn et al. 2002). Each day’s RMR measurement was based on the average of two 10-min collections of expired gas. The values for the lower of the 2 days were used in further calculations. Energy expenditure (kJ) was calculated from the respiratory exchange ratio (RER) and V̇O2 data (Elia and Livesey 1992). To control for the effect of menstruation on RMR, subjects were tested between days 7 and 20 (day 1 = start) of their menstrual cycle.
Energy cost of activities
Each activity was performed continuously for 15 min, with expirate being collected between minutes 5 and 10 into Douglas bag 1 and minutes 10–15 into Douglas bag 2. The oxygen (O2) and carbon dioxide (CO2) gas fractions were measured using calibrated analysers and the volume of expirate was determined using a 350-l Tissot spirometer. The total mass of apparatus carried by the subject, including respiratory tubing, was 450 g. A detailed explanation of our technique for measuring V̇O2 during household activities is contained in Gunn et al. (2002). The five activities performed in the laboratory and its environs were: moderate-paced walking, sweeping outdoor paths, window cleaning, vacuuming and lawn mowing with the identical equipment as that used in our pilot study (Gunn et al. 2002). The four household activities were repeated in the subjects’ homes using the same cleaning equipment as previously.
In the laboratory, subjects were instructed to perform the four household activities at ‘a pace you would normally do them at home’ and walking at ‘what you perceive to be a moderate pace’. These instructions were given to the volunteers prior to each task. As previously (Gunn et al. 2002), speeds of walking (km·h−1), window cleaning (m2·min−1), sweeping outdoors on a paved surface (m·min−1) and lawn mowing (km·h−1) were determined in the laboratory environment.
HR, CSA accelerometers, respiratory frequency and Borg rating of perceived exertion
Measurements of HR, respiratory frequency and CSA accelerometer counts were temporally aligned. HR was measured using a Polar X-Trainer Plus (Polar Electro OY, Kempele, Finland) which was calibrated throughout the physiological range of measurement using a pulse generator. Accelerometer counts at the wrist and hip were recorded using two uniaxial accelerometers (model 7164, Computer Science Applications, Shjalimar, Fla.) that were calibrated using a calibration rig (model CAL71) designed by the manufacturer. Respiratory frequency was monitored using a customised device that incorporated a thermistor located just beyond the mouthpiece. This device, which used the cadence channel of the HR monitor’s receiver to record respiratory frequency, was calibrated against a ventilometer (P.K. Morgan, Kent, UK). After completing each activity, a 14-point Borg rating of perceived exertion scale was used to estimate the subject’s perceived exertion of the task.
Body composition, height and mass
Height and mass were determined using a wall stadiometer and electronic balance (model FW-150 K, A&D Mercury, South Australia), respectively. Total body DXA scans were conducted with a Lunar DPX-L (Lunar Corp, Madison, Wis.) for 25 subjects, but a Lunar Prodigy (General Electric, Madison, Wis.) was used for the remaining 11 subjects, because the Flinders Medical Centre’s DXA machine was updated. Repeated trials for fat-free mass (FFM) on 12 (6 male and 6 female) subjects using the Lunar DPX-L yielded an intraclass correlation coefficient and technical error of measurement of 0.99 and 1.5%, respectively.
Statistics
Various dependent t-tests and single-sample, two-tailed t-tests were conducted (P≤0.05). Interclass correlation coefficients were also calculated between speeds for walking, window cleaning, sweeping and lawn mowing and their corresponding METs.
A prediction equation was generated for the activities conducted in each of the laboratory and home settings by fitting random intercept regression models to the data (Healy 2001). Specific physical activity, HRnet (exercise HR−resting HR) and CSAhip, were included as potential predictors because of their known associations with METs. Additional independent variables were selected using a backward elimination procedure, with an elimination value of P>0.05, from among: respiratory frequency, Borg rating of perceived exertion, CSAwrist and Quetelet’s index and all two-factor interactions between the specific physical activity and other potential predictors. The adequacy of the final models was checked by examining linearity of relationships, normality of residuals and independence of random subject effects and predictors.
The predictive ability of the models was examined by calculating interclass correlations (r 2) and standard errors of estimate (SEE) between predicted and measured METs for each physical activity using a leave-one-out (LOO) protocol (Harrell 2001). This method involved fitting the model with one subject’s data omitted, and then using the model to predict the MET intensity of the omitted subject. The process was then repeated for each subject; hence, 36 slightly different equations were required to predict the METs for the complete sample. The LOO method for prediction reduces the bias introduced when assessment of the predictive ability of a model is based on how well it predicts for the same subjects on which it was developed. However, the inflated r 2 and reduced SEEs between predicted and measured METs that are produced when not using the LOO technique have also been included in Table 4.
Results
Descriptive data and RMR
The descriptive statistics for the 36 subjects are presented in Table 1. The measured RMR of 3.0 ml·kg−1·min−1 was significantly less (P<0.001) than the assumed MET constant of 3.5 ml·kg−1·min−1. FFM explained 52% of the between-subject variation in RMR (kJ·h−1). After controlling for the effects of FFM, fat mass explained an additional 16% of the variation. %BF measured using DXA correlated inversely (r 2=0.61) with RMR (ml O2·kg−1·min−1).
The probability is 0.95 (Dobson 1984) that the population means for energy expenditure are within the following MET ranges for the laboratory activities: walking, 3.9–4.3; sweeping, 3.2–3.7; window cleaning, 3.6–4.0; vacuuming, 2.8–3.3; and lawn mowing, 5.6–6.3. Comparable MET ranges for the household activities performed in the subjects’ homes are: sweeping, 3.8–4.3; window cleaning, 3.1–3.5; vacuuming, 3.5–3.9; and lawn mowing, 5.0–5.7.
Are household activities performed at a moderate intensity?
The energy expenditure data are contained in Table 2. While all activities in the laboratory and the home were performed at mean intensities ≥3.0 METs, vacuuming in the laboratory was the only activity performed at a mean intensity not significantly greater than 3.0 METs (P=0.571). Furthermore, this activity was performed at an intensity >3.0 METs by only half of the sample. In contrast, mowing, both in the home and laboratory, and sweeping in the home, were activities performed by all 36 subjects at an intensity ≥3.0 METs.
Table 2 also presents energy expenditure as multiples of measured RMR (mRMR) instead of the assumed constant (3.5 ml O2·kg−1·min−1). Because the RMR for our sample was significantly less than the constant, mRMR was significantly higher (P<0.001) than METs for all activities in the home and laboratory.
There were no significant V̇O2 differences between bags 1 (minutes 5–10) and 2 (minutes 10–15) during sweeping, window cleaning and vacuuming in the laboratory (P≥0.14) and all household activities in the home (P≥0.14). This suggested that the participants were exercising at a steady state during these activities. However, there was a significant increase (P=0.001) in energy expenditure between bags 1 (X̄=4.07 METs) and 2 (X̄=4.14 METs) for walking with a corresponding increase (P<0.001) in walking speed from 5.4 km·h−1 to 5.5 km·h−1. There was also an increase in mowing energy expenditure (P=0.005) between bags 1 (X̄=5.90 METs) and 2 (X̄=6.02 METs), but there was no significant difference in mowing speed.
Home and laboratory comparison
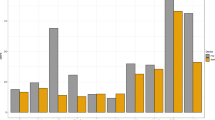
Energy expenditure (METs) data for all activities in the laboratory and home are presented in Fig. 1 and Table 2. Sweeping and vacuuming were performed at a higher mean MET intensity (P<0.001) at home compared with the laboratory; however, two and one subject(s), respectively, went against the trend by performing these activities at a lower MET intensity in their homes. In contrast, window cleaning and mowing were performed at a lower mean MET intensity (P<0.001) at home compared to the laboratory, but five subjects for each of these activities went against this trend and increased their self-paced intensity at home. Mean HR and CSAhip were two predictors that consistently reflected the changes in MET means between the home and laboratory environment (Tables 2, 3). However, there was no significant decline in mean HR (−1 beat·min−1, P=0.76) associated with the MET difference (−0.5 MET) between the laboratory and home environments for window cleaning.
Box plots of self-paced energy expenditures [metabolic equivalents (METs)] during moderate-paced walking and the four household activities. Boxes represent the inter-quartile ranges (25th percentile to the 75th percentile); whiskers of box plots depict the ranges and bold lines within the boxes are the medians. Shaded boxes represent activities performed in the home
Speed and energy expenditure
The mean (SD) moderate-paced walking speed was 5.5 (0.5) km·h−1 with a corresponding intensity of 4.1 (0.7) METs. The correlation between walking speed and energy expenditure was high (r 2=0.70, SEE=0.4 MET). This value increased (r 2=0.78, SEE=0.3 MET) if one outlier was removed from the sample. An energy expenditure of 3·0 METs required a walking speed of 4.4 km·h−1 (Fig. 2).
The self-paced mowing speed in the laboratory setting was 3.7 (0.5) km·h−1 with a corresponding energy expenditure of 6.0 (1.0) METs. The relationship between speed of mowing and energy expenditure in the laboratory was low to moderate (r 2=0.39, SEE=0.8 MET). Multiple regression using ‘mower mass as a percentage of body mass’ and ‘speed of mowing’ produced the following equation to predict the energy expenditure of mowing in the laboratory: METs=−2.062+(0.0706 × percentage mass)+[1.254 × speed (km·h−1)]. This equation increased the explained variance and decreased the SEE to 73% and 0.5 MET, respectively. Mowing speed [2.6 (0.7) km·h−1] and energy expenditure [5.3 (1.0) METs] in the home were significantly lower (P<0.001) than their laboratory counterparts, but introducing ‘mower mass as a percentage of body mass’ into a multiple linear regression with speed increased the explained variance from 14% to 45%. In the laboratory environment, there was a weak relationship (r 2=0.12, P=0.04) and a non-significant correlation (r 2=0.09, P=0.08) between speed and energy expenditure for sweeping and window cleaning, respectively.
Predicting energy expenditure
Table 3 presents the descriptive statistics for the predictors, whilst Table 4 contains the two random-intercept regression equations for the laboratory and home environments. Each equation has been partitioned into activities for ease of interpretation. The significant predictors for both equations were HRnet, CSAhip, CSAwrist and Quetelet’s index. Respiratory frequency was also statistically selected as a significant predictor in the laboratory equation due to its interaction with task. This interaction was caused by a weak positive correlation (r 2=0.09) between METs and respiratory frequency for window cleaning. However, inclusion of respiratory frequency decreased the predictive ability for the other activities and it was excluded from the model because of the difficulties in measuring this variable. Quetelet’s index was included in the models as an expedient surrogate measure of %BF. The effect of %BF (via DXA) on self-paced energy expenditure is highlighted in Fig. 3, where mean METs for all activities except for vacuuming in the home (P=0.09), were significantly lower for the ten fattest subjects (X̄%BF=43%, X̄FFM=44.8 kg, X̄FM=34.8 kg) compared with the ten leanest ones (X̄%BF=23%, X̄FFM=43.7 kg, X̄FM=13.5 kg).
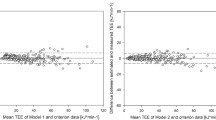
The comparisons between measured and predicted METs for the laboratory and home equations are illustrated in Fig. 4A and C, respectively. Figure 4A and C also highlight the minimal number of subjects who were misclassified by the prediction equation as exercising at a light intensity (<3.0 METs) when they were exercising at a moderate intensity (≥3.0 METs, quadrant 2) and vice versa with predicted METs ≥3 when they were actually exercising at <3 METs (quadrant 1). The predictive abilities of the home and laboratory models were assessed by interclass correlations and SEEs for the comparisons between measured and predicted METs for the overall home (r 2=0.74, SEE=0.54 MET) and laboratory models (r 2=0.84, SEE=0.51 MET), as well as each activity separately (Table 4).
A Bland and Altman plot (Fig. 4B) shows that the laboratory equation under-predicted individuals’ METs by up to 1.7 METs (mowing) and over-predicted by up to 1.4 METs (mowing). Corresponding values for the home equation (Fig. 4D) were an under-prediction of up to 1.6 METs (sweeping) and over-prediction by up to 1.4 METs (mowing). However, 95% of the predictions were within ±1.0 MET and ±1.1 METs of the measured values when using the laboratory and home equations, respectively (Fig. 4B, D).
Discussion
Descriptive data and RMR
Our sample was selected within a narrow 10-year age range (35–45 years) to control for the age-associated decrease in V̇O2max which would increase the relative intensity of an absolute workload. However, we selected a heterogeneous sample to characterise the population within this age range, thereby enhancing the validity of estimating the MET means.
RMR was inversely correlated with %BF (r 2=0.61, P<0.001) because adipose tissue has approximately one-sixth the resting energy expenditure of the FFM (Elia 1992). Our measured RMR (X̄=3.0 ml·kg−1·min−1), which was significantly lower (P<0.001) than the assumed constant (3.5 ml·kg−1·min−1), might therefore be due to the fact that today’s average 35- to 45-year-old female carries a larger percentage of fat mass compared to the sample on which the 1 MET constant is based. Also, our volunteers had their RMRs measured when post-absorptive and supine, whereas the ACSM guidelines (ACSM 1991) state that the 1 MET constant approximates the V̇O2 of a seated individual at rest, with no mention of whether this is for the post-absorptive state. Unfortunately, the origin of the data on which the 1 MET constant is based was untraceable; this infers that it might have been an arbitrary value used to simplify the public health message.
Are household activities performed at a moderate intensity?
All mean energy expenditures for the household activities, whether they were completed in the home or in the laboratory, were performed at an intensity ≥3.0 METs. These data therefore suggest that, for 35- to 45-year-old women, sweeping, window cleaning, vacuuming and mowing are household chores that can contribute to the 30 min·day−1 of moderate-intensity activity required to confer health benefits. However, there was substantial inter-individual variability in energy expenditure during self-paced activities in the home (Table 2: large SDs and ranges), even though tight control was exerted over potential confounding factors, such as previous exercise, smoking, caffeine intake and thermic effect of food. Furthermore, this large inter-individual variation remained when the environment was standardised in the laboratory so that everyone performed the activities on the same windows, patch of lawn, path and carpet. The likely reasons for these large variations include between-subject differences in aerobic fitness and psychological approach. We suggest that someone who is fitter or motivated will tend to self-pace him-/herself at a higher intensity than a less-fit or unmotivated subject. Differences in mechanical efficiency might also contribute to a small percentage of the variation in exercise intensity. Even though all mean energy expenditures were ≥3.0 METs, not all individuals performed these activities at an intensity which was adequate to confer health benefits (Table 2). For instance, sweeping in the home was performed at an intensity >3.0 METs by all subjects, but seven subjects performed sweeping in the laboratory at a light intensity. One should therefore be cautious about applying our findings to individuals but classifying sweeping, vacuuming, window cleaning and lawn mowing in the same category as moderate-paced walking in epidemiological studies appears to be warranted.
Unless the cleaning is for employment purposes, the energy expenditure measured in the subjects’ homes is the most valid representation of the ‘real’ intensity of the four household activities. Our mean METs for sweeping (4.0 METs), window cleaning (3.3 METs), vacuuming (3.7 METs) and mowing (5.3 METs) in the home are comparable to those of 4.0, 3.0, 3.5 and 5.5 METs, respectively, in Ainsworth’s revised compendium (Ainsworth et al. 2000). However, single-sample t-tests revealed our mean METs to be significantly higher than the compendium values for window cleaning (3.3 vs 3.0, P=0.003) and vacuuming (3.7 vs 3.5, P=0.03). The multitude of factors that can affect self-paced energy expenditure (aerobic fitness, environment, equipment, psychological approach, mechanical efficiency) suggest that mean METs for the same activity performed in different environments/terrains and in subjects of different age, gender, fitness and race will be extremely variable. Self-paced vacuuming is an example with mean METs of 2.6 (n=10, Luke et al. 1997), 3.0 (n=25, Hendelman et al. 2000), 3.1 (n=20, Wilke et al. 1995), 3.5 (n=9, Bassett et al. 2000), 3.9 (n=11, Strath et al. 2001) and 4.0 (n=33 to 44, Welk et al. 2000), whereas we measured a mean of 3.7 METs and the compendium assigns a value of 3.5 METs. Even though the rigorous nature of data collection suggests that our mean value is accurate for our group, this value may not necessarily apply to other groups of people (e.g. males, athletes, elderly). Our means of 4.0, 3.3, 3.7 and 5.3 METs for sweeping, window cleaning, vacuuming and mowing, respectively, should therefore only be applied to 35- to 45-year-old females, with similar physical characteristics, who perform the tasks in their homes using comparable equipment (i.e. upright vacuum, push mower).
METs versus multiples of mRMR
When V̇O2 was expressed as multiples of mRMR, the means for all activities increased significantly compared to METs (Table 2). This increase was due to our significantly lower RMR (3.0 ml O2·kg−1·min−1) compared with the 1 MET constant of 3.5 ml O2·kg−1·min−1. Although the MET constant ignores the substantial inter-individual variability in RMR (our range = 2.2 to 3.7 ml·kg−1·min−1), METs can be converted to V̇O2·ml·kg−1·min−1 simply by multiplying by 3.5. We cannot therefore justify a change to mRMR because RMR would have to be measured; furthermore, all physical activity recommendations are based on the 1 MET constant.
Home and laboratory comparison
The four household activities were performed at significantly different intensities at home compared to the laboratory, even though subjects were always instructed to perform the activities ‘at a pace they would normally do them at home’. This suggests that self-paced energy expenditure is somewhat dependent on the terrain or environment in which the activity is performed and that ‘psychological influence’ or ‘mental approach’ during self-paced activities might also play a role in determining the energy expenditure of a task. For example, vacuuming energy expenditure increased by 22% when the subjects performed the task at home compared with the laboratory. In the laboratory, an 18.5-m2 carpet was vacuumed repeatedly for 15 min, which most subjects felt was ‘boring and tedious’. However, in their own homes they were mostly completing some of their weekly housework and were subjectively more motivated to perform the task. Indeed, the increase in CSAhip counts·min−1 in the home (laboratory: 476 counts·min−1; home: 668 counts·min−1) indicates that the subjects’ energy expenditure increase was due to a greater pace. A similar scenario was apparent for sweeping, which the women classified as boring in the laboratory; but, in the home, a 17% increase in energy expenditure was reflected by a doubling of the mean CSAhip count (laboratory: 276 counts·min−1; home: 630 counts·min−1).
In contrast, the mean energy expenditure during mowing and window cleaning decreased in the home environment by 11% and 13%, respectively. It is possible to speculate that during these activities, the restrictive environment in the subjects’ homes (smaller lawn area and smaller, further apart windows) may have overridden the extra motivation for doing the tasks; hence, their energy expenditure decreased. This is demonstrated during mowing where mean speed (laboratory: 3.7 km·h−1; home: 2.6 km·h−1) and CSAhip counts (laboratory: 3,127 counts·min−1; home: 1,513 counts·min−1) were significantly reduced in the home compared with the laboratory setting whereas the higher mowing CSAwrist counts in the home (home: 2,652 counts·min−1; laboratory: 1,562 counts·min−1) reflected the additional manoeuvring of the mower around the home garden.
Although previous investigators have measured household activities in the home or the laboratory, this study and our previous work (Gunn et al. 2003) are the only ones which, to our knowledge, have compared these two environments. Interestingly, the same trend for the laboratory and home comparisons was reported for the same age group of Australian males (Gunn et al. 2003).
Speed and energy expenditure
Speed correlated significantly with energy expenditure (r 2=0.70, P<0.001; Fig. 2) during walking. Our mean ‘moderate’ walking speed of 5.5 km·h−1 (4.1 METs) is comparable to the speed and energy expenditure reported by Hendelman et al. (2001) (5.7 km·h−1, 4.1 METs) and covertly observed walking speed of 82 walkers in a public park (5.6 km·h−1; Murtagh et al. 2002). In contrast, the compendium (Ainsworth et al. 2000) has assigned a lower speed and energy expenditure (4.8 km·h−1; 3.3 METs) to ‘moderate’-paced walking. Furthermore, ‘brisk’-paced walking is reported as 5.6 km·h−1 in the compendium (Ainsworth et al. 2000), whereas measured values are 6.4 km·h−1 (Strath et al. 2001), 6.4 km·h−1 (Murtagh et al. 2002) and 6.7 km·h−1 (Hendelman et al. 2000). These data therefore suggest that the speeds and energy expenditures for moderate- and brisk-paced walking in the compendium need to be revised. Alternatively, the higher values in our and other experiments (Hendelman et al. 2000; Strath et al. 2001) might be due to the subjects pacing themselves at a higher intensity when they are being measured. One way to circumvent this Hawthorne effect is to covertly observe the speed of walkers; however, it is impossible to assign a verbal prompt such as ‘moderate’ and ‘brisk’ to the pace at which covertly observed subjects walk. The speed of walking is therefore primarily influenced by the environment (e.g. shops vs public parks) and/or the purpose of the activity (e.g. general walking vs exercise walking). For example, covertly observed walkers ambulated at 4.5 km·h−1 in a shopping centre (Finley and Cody 1978), whereas substantially higher mean values of 5.6 km·h−1 (Murtagh et al. 2002) and 6.4 km·h−1 (Spelman et al. 1993) have been reported in a public park and around an exercise track, respectively. Compendium estimates for moderate- and brisk-paced walking can therefore only be based upon measured V̇O2 values.
Pushing a 31-kg mower imposed a greater physiological load on the lighter subjects compared with the heavier ones (Fig. 2). The correlation between mowing speed in the laboratory and energy expenditure (r 2=0.39, SEE=0.8 MET) was therefore substantially lower than for walking. The correlation between mowing speed and energy expenditure in the home setting was further attenuated (r 2=0.14, SEE=1.0 MET) by the revolution counter’s inability to accurately measure distance due to the back-and-forward motion for mowing small areas, the slopes of the lawns and variability in the amount of manoeuvring around garden beds.
Predicting energy expenditure
The combination of HRnet, CSAhip, CSAwrist and Quetelet’s index resulted in two equations that predicted energy expenditure in the home and laboratory for 35- to 45-year-old women with 95% confidence intervals (CIs) of ±1.1 METs and ±1.0 MET, respectively, during walking, sweeping, window cleaning, vacuuming and mowing (Fig. 4B, D). HRnet was used in the prediction equations because it explained a greater proportion (44%) of the variation in energy expenditure than HR alone (35%). By themselves, the wrist- (r 2=0.04, P<0.05) and hip- (r 2=0.26, P<0.05) located CSA monitors correlated weakly with energy expenditure. However, when they were included in the prediction models, both CSAhip and CSAwrist significantly (P<0.05) contributed to the prediction of energy expenditure. Our results suggest that %BF influences self-paced energy expenditure (Fig. 3). This is because an increase in %BF may be associated with a decrease in aerobic fitness (Jackson et al. 1990); hence, energy expenditure during self-paced household tasks is also likely to decline. Our 95% CI is somewhat smaller than the ±1.3 (Haskell et al. 1993), ±1.7 (Luke et al. 1997) and ±1.5 METs (Strath et al. 2001) reported by others who have utilised individual analyses to predict the energy expenditure of various activities via combined HR and motion-sensor techniques. Individual analyses require each subject’s HR to be ‘calibrated’ to their V̇O2 at several submaximal workloads using a graded exercise test. Although development of a HR-V̇O2 regression for each subject controls for the effect of aerobic fitness on HR response during submaximal exercise, it is time consuming and thus unsuitable for large-scale epidemiological studies. In comparison, when Luke et al. (1997) and Haskell et al. (1993) performed a single-regression analysis on grouped data, their respective 95% CIs expanded to ±2.4 METs and ±3.0 METs, respectively. Our equations do not require an ergometer and indirect calorimetry system that are essential for generating individual HR-V̇O2 regressions.
Although our random intercept regression model accounts for nested data within an individual and produces an overall best-fit model for the laboratory and home environment, it assigns different coefficients to some predictors that have an interaction with activity (e.g. CSAwrist). Hence, the overall laboratory and home models can be written as five and four separate equations, respectively. The different coefficients for each activity prevent our equations from being validated against other household activities, thereby reducing their generalisability.
In the context of moderate-intensity exercise ranging between 3 METs and 6 METs, a CI of ±1.1 METs lacks predictive precision. The error term is approximately ±15% to ±30% of the upper (6 METs) and lower limits (3 METs) of moderate-intensity exercise, respectively. Also, expressing the 95% CI in METs somewhat conceals the physiological significance of the real error involved. For example, the probability is 0.95 that a subject with a measured V̇O2 of 10 ml·kg−1·min−1 (2.9 METs) will have a predicted V̇O2 within the range of 6.2 ml O2·kg−1·min−1 to 13.9 ml O2·kg−1·min−1 using our equations.
Another limitation of our laboratory equation, which uses a weighted combination of four predictors, is that energy expenditure during level-terrain walking can be predicted with comparable precision using speed only. Also, persons who do not have similar physical characteristics and aerobic fitness levels (including Quetelet’s index) to our sample are likely to have their energy expenditures under- or over-estimated. For example, a subject with a substantially higher Quetelet’s index than the remaining sample had her energy expenditure underestimated using the LOO method by −1.3 METs to −1.6 METs (Fig. 4B, D). This underestimation was due to the fact that the negative regression weight for Quetelet’s index was too high for very large indices. Finally, as measured energy expenditure gets closer to 3.0 METs, the probability of the subject being misclassified into the wrong exercise category (light or moderate) increases (Fig. 4A, C). However, the mean differences between predicted and measured METs for the 20 and 14 misclassified subjects in the laboratory (Fig. 4A) and home models (Fig. 4C) were 0.45 MET and 0.54 MET, respectively.
Conclusions
-
1.
Our data suggest that self-paced lawn mowing (5.3 METs), sweeping outdoor paths (4.0 METs), vacuuming (3.7 METs) and window cleaning (3.3 METs) are all performed in the home at a mean intensity >3.0 METs by 35- to 45-year-old Australian females. These household activities can therefore contribute to their accumulated 30 min·day−1 of moderate-intensity physical activity required to confer health benefits. However, due to large inter-individual variability associated with self-paced energy expenditure, it is unlikely that all individuals will perform these activities at an intensity ≥3.0 METs.
-
2.
We are the first to demonstrate a significant difference (P<0.001) in self-paced energy expenditure between the home and laboratory settings for household activities. This highlights that factors such as environment/terrain and motivation to perform a task affect self-paced energy expenditure.
-
3.
Our regression equations lack predictive precision for estimating energy expenditure from HRnet, CSAhip, CSAwrist and Quetelet’s index.
References
American College of Sports Medicine (ACSM) (1991) ACSM’s guidelines for exercise testing and prescription, 4th edn. Lea and Febiger, Philadelphia, p 287
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO, Jacobs DR Jr, Leon AS (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32:S498-S504
Armstrong T, Bauman A, Davies J (2000) Physical activity patterns of Australian adults. Results of the 1999 national physical activity survey. Australian Institute of Health and Welfare, Canberra
Bassett DR Jr, Ainsworth BE, Swartz AM, Strath SJ, O’Brien WL, King GA (2000) Validity of four motion sensors in measuring moderate-intensity physical activity. Med Sci Sports Exerc 32:S471-S480
Commonwealth Department of Health and Aged Care (CDHAC). (1999) National physical activity guidelines for Australians. CDHAC, Canberra
Dobson AJ (1984) Calculating sample size. Trans Menzies Found 7:75–79
Elia M (1992) Organ and tissue contribution to metabolic rate. In: Kinney JM, Tucker HN (eds) Energy metabolism: tissue determinants and cellular corollaries. Raven Press, New York, pp 61–79
Elia M, Livesey G (1992) Energy expenditure and fuel selection in biological systems: the theory and practice of calculations based on indirect calorimetry and tracer methods. In: Simopoulos AP (ed) Metabolic control of eating, energy expenditure and the bioenergetics of obesity. Karger, Basel, pp 68–131
Fentem P, Walker A (1994) Setting targets for England: challenging measurable and achievable. Moving on: international perspectives on promoting physical activity. Health Education Authority, London, pp 58–79
Finley FR, Cody KA (1978) Locomotive characteristics of urban pedestrians. Arch Phys Med Rehabil 51:423–426
Gill T, Taylor A, Williams M, Starr G (2001) Physical activity in South Australian adults. Department of Human Services, South Australia
Gore CJ, Edwards DA (1992) Australian fitness norms. Health Development Foundation, Adelaide
Gunn SM, Brooks AG, Withers RT, Gore CJ, Owen N, Booth ML, Bauman A (2002) Determining energy expenditure during some household and garden tasks. Med Sci Sports Exerc 34:895–902
Gunn SM, van der Ploeg GE, Withers RT, Gore CJ, Owen N, Bauman AE, Cormack J (2003) Measurement and prediction of energy expenditure in males during household and garden tasks. Eur J Appl Physiol DOI 10.1007/s00421-003-0932-1
Harrell FE Jr. (2001) Regression modeling strategies. With application to linear models, logistic regression, and survival analysis. Springer, Berlin Heidelberg New York, pp 93–94
Haskell WL, Yee MC, Evans A, Irby PJ (1993) Simultaneous measurement of heart rate and body motion to quantitate physical activity. Med Sci Sports Exerc 25:109–115
Healy MJR (2001) Multilevel data and their analysis. In: Goldestein H, Leyland AH (eds) Multilevel modelling of health statistics. Wiley, New York, pp 1–12
Hendelman D, Miller K, Baggett C, Debold E, Freedson P (2000) Validity of accelerometry for the assessment of moderate-intensity physical activity in the field. Med Sci Sports Exerc 32:S442-S449
Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE (1990) Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc 22:863–870
Luke A, Maki KC, Barkey N, Cooper R, McGee D (1997) Simultaneous monitoring of heart rate and motion to assess energy expenditure. Med Sci Sports Exerc 29:144–148
Mathers CD, Vos ET, Stevenson CE, Begg SJ (2000) The Australian burden of disease study: measuring the loss of health from diseases, injuries and risk factors. Med J Aust 172:592–596
Murtagh EM, Boreham CAG, Murphy MH (2002) Speed and exercise intensity of recreational walkers. Prev Med 35:397–400
Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, et al (1995) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 273:402–407
Spelman CC, Pate RR, Macera CA, Ward DS (1993) Self-selected exercise intensity of habitual walkers. Med Sci Sports Exerc 25:1174–1179
Stevenson J, Bauman A, Armstrong T, Smith B, Bellew W (2000) The costs of illness attributable to physical inactivity in Australia. CDHAC, Canberra
Strath SJ, Bassett DR Jr, Swartz AM, Thompson DL (2001) Simultaneous heart rate-motion sensor technique to estimate energy expenditure. Med Sci Sports Exerc 33:2118–2123
Strath SJ, Bassett DR Jr, Thompson DL, Swartz AM (2002) Validity of the simultaneous heart rate-motion sensor technique for measuring energy expenditure. Med Sci Sports Exerc 34:888–894
Sujatha T, Shatrugna V, Venkataramana Y, Begum N (2000) Energy expenditure on household, childcare and occupational activities of women from urban poor households. Br J Nutr 83:497–503
Tanaka H, Monahan KD, Seals DR (2001) Age-predicted maximal heart rate revisited. J Am Coll Cardiol 37:153–156
Welk GJ, Blair SN, Wood K, Jones S, Thompson RW (2000) A comparative evaluation of three accelerometry-based physical activity monitors. Med Sci Sports Exerc 32:S489-S497
Wilke NA, Sheldahl NM, Dougherty SM, Hanna RD, Nickele GA, Tristani FE (1995) Energy expenditure during household tasks in women with coronary artery disease. Am J Cardiol 75:670–674
US Department of Health and Human Services (USDHHS) (1996) Physical activity and health: a report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Atlanta
Acknowledgement
This study was supported by a grant from the National Health and Medical Research Council of Australia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brooks, A.G., Withers, R.T., Gore, C.J. et al. Measurement and prediction of METs during household activities in 35- to 45-year-old females. Eur J Appl Physiol 91, 638–648 (2004). https://doi.org/10.1007/s00421-003-1018-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-003-1018-9