Abstract
Objectives
To compare the apparent urinary excretion rates of both creatinine and 1-hydroxypyrene (1-OHP) and to assess the value of creatinine normalization for both toxicokinetic analysis and the routine examination of workers.
Methods
All urine samples were collected from individuals who had been exposed to polycyclic aromatic hydrocarbons (PAHs), occupationally and non-occupationally, for at least 24 consecutive hours. Urinary creatinine and 1-OHP were determined. 1-OHP excretion rates were expressed either as a function of creatinine excretion rate or as unadjusted values. Theoretical relationships between creatinine-normalized excretion of metabolites and body weight-adjusted inhaled dose were drawn for men with a constant body mass index.
Results
Creatinine excretion rate paralleled 1-OHP excretion rate. The plot of creatinine excretion rate–adjusted excretion rate of 1-OHP vs time led to smooth curves for determination of toxicokinetic parameters. Creatinine normalization was adequate, even for samples with a urinary creatinine concentration below 0.5 g/l or above 3 g/l. A theoretical analysis revealed that men weighing between 50 kg and 100 kg, exposed to a constant dose of a pollutant producing a urinary metabolite excreted by the same mechanism as creatinine, would exhibit a body weight-adjusted dose span of 2 with an accompanying creatinine-normalized metabolite excretion span of 2.23-fold.
Conclusion
The kinetics of creatinine excretion parallels that of 1-OHP, and a creatinine excretion rate–normalized excretion rate of 1-OHP appears to allow for a better determination of the toxicokinetic parameters of 1-OHP urinary excretion. At least in the case of 1-OHP, creatinine normalization seems valid, even for very dilute or very concentrated urine samples. Finally, because creatinine normalization not only compensates for variable diuresis but also correlates better with the body weight-adjusted dose of the parent compound, it should be used in biological monitoring of exposure to (PAHs) pyrene and to other substances whose urinary biomarker excretion kinetics parallel that of creatinine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Creatine is found mainly (ca. 94%) in the muscle cells of the body. Through non-enzymatic transformation, it is converted into creatinine at an almost steady-state rate of approximately 2% of the creatine pool per day [1]. Creatinine is then excreted into the urine, primarily by glomerular filtration. Daily urinary excretion of creatinine derived from muscles occurs at a ratio of ca. 1 g per 20 kg of muscle mass [2]. As a result, it is frequently used as an indirect measurement of muscular mass. However, physiological studies using this approach have followed a carefully controlled protocol that included a meat-free diet for at least 2 days before the start of urine collection. The measurement itself spreads over 2 or 3 days [3, 4]. Meat consumption has been found to contribute up to a potential 10–35% of daily creatinine excretion in humans [5, 6], 10% being the average [7]. There are at least two reasons for this possible increase: first, it has been observed that protein intake per se has an effect on creatinine excretion [8, 9]; second, creatine intake can also affect creatinine excretion [10]. Furthermore, in subjects at rest, there is a known circadian rhythm in the glomerular filtration rate, oscillating around a mean value ± 10% [11]. Consequently, it can be expected that substances excreted in urine by glomerular filtration, such as creatinine and certain metabolites, will be prone to similar variations in their excretion profiles.
A number of algorithms have been published to predict 24-h creatininuria in normal individuals, based on gender, age, weight and, sometimes, height [2, 5, 7, 12]. For clinical purposes, it has been proposed that a 24-h urine collection should be considered suspect if the measured creatinine in the sample is outside a ±20% interval around the value predicted by the so-called Cockroft and Gault algorithm [13].
Similarly, body weight, and more specifically fat-free mass, is linked to resting energy expenditure [14] and hence to pulmonary ventilation. It has also been shown that there is an age-related decline in basal metabolic rate, owing to the reduction in muscle mass [15]. In an active work situation, however, the main determinant of pulmonary ventilation is the specific energy expenditure required to accomplish a given task [16]. Additionally, since it is common practice in toxicology to express doses as mass per kilogramme of body weight [17], it appears worthwhile to examine the relationships between body weight, inhaled exposure dose to a given pollutant, inhaled dose per kilogramme body weight, and creatinine-normalized excretion of a urinary biomarker of exposure to that same pollutant (see below).
Workplace exposure to chemicals can be assessed by means of biological monitoring, which takes into account the various sources and routes of intake. Most approaches rely on the measurement of the concentration of these chemicals or their metabolites in the urine. Since there can be large variations in urine volume output rate both between individuals and in a given individual during a day, methods have been proposed to account for this effect and thus yield more reliable estimates of exposure to the original chemical. The most common adjustment methods are based on urine density and urine creatinine [18]. Gender and age effects on the urinary output of creatinine have been observed, and formulae have been proposed to convert metabolite excretion from creatinine-normalized to specific gravity-adjusted values [19]. From a toxicokinetic or physiological standpoint, timed urine collections should yield the best information [20], provided that sampling can be performed in a reliable manner that ensures precise time measurement and that it is ensured that collection starts with an empty bladder and that the latter is also completely emptied at the end of each collection period. Although this is routinely performed in a clinical setting, e.g. in the case of glomerular filtration rate measurement, it has generally been considered a difficult endeavour in workplaces, especially for routine measurements.
The value of creatinine normalization to express urinary excretion results has been the subject of contradictory viewpoints in the scientific community. Some have proposed a urine-flow adjusted creatinine normalization because of the urine flow dependence sometimes observed in creatinine excretion rates, a view that has been challenged by others [20, 21, 22]. Overall, the proper use of an adjustment method must be evaluated on the basis of comparison of the kinetics of excretion of the selected biomarker with that of the adjustment parameter. For example, as methanol is distributed in total body water mainly on account of its ability to freely cross biological membranes and because of its water solubility, its excretion in urine should not be normalized for creatinine excretion [18]. When creatinine normalization appears appropriate, another aspect is that it is generally considered that urine samples with creatinine concentrations outside the approximate range of 0.5–3 g/l should be rejected as unsuitable because they are “too diluted” or “too concentrated” [18, 23].
Current biological monitoring of exposure to polycyclic aromatic hydrocarbons (PAHs) relies largely on 1-hydroxypyrene (1-OHP), a pyrene metabolite used as an indicator of exposure to total PAHs [24]. Although most authors have used normalization of creatinine concentration when reporting their results, some have argued that it has little merit in improving the relationships between urinary 1-OHP results and exposure assessment by means of standard workplace air monitoring [25, 26, 27].
The objective of the present study was to compare the apparent urinary excretion rates of creatinine and 1-OHP and to assess the value of creatinine normalization for the purpose of both toxicokinetic analysis and routine examination of workers.
Materials and methods
Study populations and design
Some of the results presented in this report are a re-analysis of previously published data. Workers exposed to PAHs were recruited from various sectors of activity including carbon brake-disc manufacturing, ferrosilicium electrometallurgy, cathode relining in an aluminium plant, and artificial shooting target fabrication [28, 29, 30]. All participating workers were informed of the purpose of the study by both the research team’s industrial hygienist and by the occupational health doctor of each workplace. The workers gave their consent to be included and were free to withdraw at all times.
They were asked to provide the total urine volume of each separate specimen and to note the exact time of urination. The research team supervised compliance with this protocol during the working shift, and the participating workers were encouraged to conform to this protocol outside working hours (i. e. supply aliquots of each sample, carefully noting total volume and time of urination). Urine sampling was started before the work shift on the first observation day and was generally stopped 24 h after the end of the last observation day. For each time interval, the total urine volume allowed for subsequent calculation of total amounts of creatinine and 1-OHP excreted.
To facilitate interpretation of the results, we classified the subjects according to their mode of exposure: mainly respiratory, mainly dermal, and mixed routes of exposure to PAHs. Judgement leading to this classification was based on field observations by an industrial hygienist, the planned protocol of certain specific studies investigating either dermal or pulmonary exposure (e.g. [30]), and the examination of the urinary excretion profile of 1-OHP. Indeed, it has been proposed that when exposure occurs mainly through inhalation, maximum excretion of 1-OHP occurs shortly after the end of the work shift, whereas when dermal exposure prevails, the maximum excretion of the metabolite is delayed by many hours [24, 28, 30]. The selected cases presented in this article as illustrations of urinary excretion of 1-OHP following exposure to various exposure profiles were extracted from a total of 50 archived cases.
Chemical analyses
1-Hydroxypyrene was analysed according to the automated column-switching high performance liquid chromatography (HPLC) method described elsewhere [31]. Creatinine was analysed with a standard kit based on the Jaffe reaction (ABX Diagnostics, Montpellier, France).
Adjustment factor for creatinine excretion rate
Mean creatinine excretion rate was obtained by the summing of the total amount of creatinine excreted over the entire observation period (in milligrammes) and dividing it by the total observation time (in hours). Subsequently, the results of the 1-OHP excretion rates were normalized to the mean creatinine excretion rate obtained for each subject as follows:
where \( {\left[ {\frac{{\Delta 1 - OHP}} {{\Delta t}}} \right]}_{{adj}} \) is the adjusted excretion rate of 1-OHP, \( {\left[ {\frac{{\Delta 1 - OHP}} {{\Delta t}}} \right]}_{i} \) is the observed excretion rate over interval “i”, \( {\left[ {\frac{{\Delta Cr}} {{\Delta t}}} \right]}_{{mean}} \) is the creatinine excretion rate averaged over the entire observation period, and \( {\left[ {\frac{{\Delta Cr}} {{\Delta t}}} \right]}_{i} \) is the observed creatinine excretion rate over interval “i”. Note that the right-hand side of Eq. 1 is equivalent to the standard 1-OHP/creatinine concentration ratio (e.g. in microgrammes per gramme creatinine) multiplied by the mean creatinine excretion rate (e.g. in grammes creatinine per hour), which is taken as a constant for a given individual. The mean creatinine excretion rate is thus useful only when toxicokinetic analysis has to be performed, but is not required for routine field work.
Physiological and anthropometrical data
Additional theoretical considerations were introduced for the appraisal of the merit of creatinine normalization. For that purpose, a number of algorithms were obtained from the literature. Basal daily energy expenditure for men was calculated from the Harris–Benedict equation [32] as follows:
where BEE is the basal energy expenditure in kilocalories per day, W is the weight in kilogrammes, H is the height in centimetres, and Age is the age in years. To limit the number of parameters in the equation, a constant body mass index (BMI=W/H2) of 24 kg/m2 (or 0.0024 kg/cm2) was considered. Hence, since \( H = {\sqrt {W/0.0024} } \), the BEE equation becomes:
Pulmonary ventilation was derived from energy expenditure assuming the utilization of 0.21 l of oxygen per kilocalorie and a constant oxygen extraction coefficient corresponding to the inhalation of 27 l of air per litre of oxygen consumed [33]:
where \( {\mathop V\limits^ \bullet } \) is the pulmonary ventilation rate in cubic metres per day, EE is the energy expenditure in kilocalories per day and 1000 is the conversion factor between litres and cubic metres. We obtain the resulting ventilation at rest, expressed as a function of weight (and age), by replacing EE by BEE in the preceding equation as follows:
We can, of course, obtain the hourly ventilation rate by dividing by 24 h/day.
The absolute dose of an inhaled pollutant is calculated by multiplication of the air concentration of the pollutant by the ventilation rate over a given period of time. The dose per kilogramme body weight is obtained by division of the absolute dose by the weight of the subject. Finally, if it is assumed that, over a given period of time, a constant fraction of the pollutant (kbiot, which includes a factor that takes into account differences in molecular weights between pollutant and metabolite) is excreted in the urine as a metabolite, the amount of metabolite M excreted over a time interval Δt can be obtained from:
where [P] is the air concentration of the pollutant in miligrammes per cubic metre.
The estimated creatinine excretion can be obtained from the following relationship [5]:
where \( {\mathop {Cr}\limits^ \bullet } \) is the urinary excretion rate of creatinine, and W, H and Age are as defined above. Again, if we take \( H = {\sqrt {W/0.0024} } \), the hourly excretion rate can be calculated as:
The latter equation can be used to calculate the total creatinine excretion (Cr) for a given time interval (Δt, in hours):
We can obtain the urinary metabolite concentration expressed, for example, in milligrammes per gramme creatinine, by dividing the excretion rate of the metabolite by that of creatinine over a given time interval, or by dividing the amount of metabolite excreted by the amount of creatinine over the same time interval.
Data analysis
We could find no entirely satisfactory statistical approach to compare the urinary excretion rate profiles of 1-OHP with the corresponding creatinine excretion rate profiles. As a tentative approach, we compared the signs of the slopes of the consecutive segments obtained on the respective excretion rate vs time profiles for both analytes. The percentage of similarity in the sign of the slopes was calculated for each of 50 archived profiles. We performed a t-test to check if the mean percentage calculated from all samples was statistically significantly different from 50%, which is the expected value if the paired slopes are distributed randomly and, therefore, independent of each other.
Results
Comparison of excretion profiles of 1-OHP and creatinine
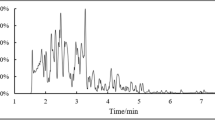
Figure 1 shows the 1-OHP and creatinine excretion rates for various typical individuals. Data are from a non-smoker (A) and a smoker (B) with no occupational exposure to PAHs, one individual with mainly respiratory occupational exposure (C), one individual with mainly dermal occupational exposure (D), and two individuals with mixed respiratory/dermal occupational exposure (E, F). A striking parallelism can clearly be seen between the excretion rates of both substances for a number of subjects. It also appears that the 1-OHP excretion rates are sometimes rather erratic and difficult to exploit for toxicokinetic analysis. As was indicated under the Materials and methods section, these examples, illustrating a variety of exposure conditions, were extracted from a total of 50 profiles obtained from various occupationally and non-occupationally exposed individuals, showing the stated parallelism. Examination of the signs of the slopes on the excretion rate vs time profiles for all 50 cases gave 81% similarity between 1-OHP and creatinine, which is statistically different from 50% (t=15.4, P<0.0001).
Comparative urinary excretion rate profiles for 1-hydroxypyrene (closed squares, left scales) and creatinine (open circles, right scales) in control non-smoker (A) and smoker (B) and in various workers with occupational exposure to PAHs through respiratory (C), dermal (D), and mixed respiratory/dermal (E, F) intake
Creatinine excretion rate as an adjustment parameter for 1-OHP
The smoothing effect is striking when the 1-OHP excretion rates are adjusted for creatinine excretion rate as per Eq. 1, as seen in three typical individuals illustrating each of the three exposure profiles (Fig. 2). Of course, the adjustment has little effect on the appearance of the kinetic profile of individuals with a relatively stable creatinine excretion rate.
“Extreme” creatinine concentration values
Figure 3 shows the creatinine concentrations and the adjusted excretion rates for three individuals. For each pair, the left graph shows the creatinine concentration and the right graph the corresponding 1-OHP excretion rate, with arrows indicating the beginning of a work shift exposure to PAHs. The samples corresponding to Fig. 3A were collected from a subject who drank little water while working in a hot environment. Figure 3B shows data points corresponding to the urine samples of an individual who was observed drinking water frequently. The investigators have serious reasons to think that the worker who provided the urine samples depicted in Fig. 3C tampered with those samples, possibly by adding water to incomplete specimens. It is readily seen that even for “extreme” creatinine concentrations, creatinine normalization yields an adjusted 1-OHP excretion rate that fits well with the observed overall excretion profile and with periods of PAH exposure. For all the individuals whose excretion profiles are presented in Figs. 1, 2, and 3 the creatinine concentrations ranged from 0.14 to 5.3 g/l, with 13% of the values outside the 0.5–3 g/l range. The highest creatinine concentrations that we ever measured in workers were around 7–8 g/l.
Theoretical considerations about the influence of body weight on creatinine excretion and pulmonary ventilation
Figure 4A shows the impact of body weight on the at-rest ventilation in 30-year old men with a BMI of 24 kg/m2. The pulmonary ventilation varies from 0.3 m3/h to 0.53 m3/h between a 50-kg and a 100-kg person. Figure 4B gives the relationship between body mass and creatinine excretion rate for 30-year old men with the same BMI. From 50 kg to 100 kg, creatinine excretion rate rises from 45 to 101 mg/h. Further calculations were performed that assumed resting conditions in 30-year old male subjects with a BMI of 24 kg/m2 and exposed to the same concentration of a pollutant P producing 25% (kbiot) of metabolite M in the urine over 24 h. Figure 4C illustrates the relationship thus found between the 24-h urinary excretion of the metabolite, expressed in milligrammes per gramme creatinine and the inhaled dose (concentration of pollutant set arbitrarily at 1,000 mg/m3 × pulmonary ventilation at rest × 8 h for the work shift) expressed per kilogramme body weight. For a weight factor variation of 2, the dose per kilogramme body weight at rest for exposure to a constant concentration of pollutant varies only from 42.7 to 48.1 mg/kg, i.e. a factor of 1.13. The corresponding variation in creatinine-normalized excretion of the metabolite derived from the pollutant in question under the conditions specified above is from 440 to 553 mg/g creatinine or a factor of 1.26.
Relationships between pulmonary ventilation at rest and body weight (A), creatinine excretion rate and body weight (B), creatinine-normalized metabolite excretion and body weight-adjusted dose resulting from exposure at rest to a constant concentration of 1,000 mg/m3 of a parent pollutant (C), and creatinine-normalized metabolite excretion and body weight-adjusted dose resulting from exposure to a constant absolute dose of 10,000 mg of a parent pollutant (D). All male subjects in these simulations had a constant BMI of 0.0024 kg/cm2
If it is now assumed that all the men inhaled 10 m3 of air for the entire 8-h work shift, no matter their weight (see Discussion section), the relationship between the creatinine-normalized 24-h concentration of metabolite M and the inhalation exposure to 1,000 mg/m3 of pollutant P for men with the same characteristics as above and allowing only weight to vary would be that illustrated in Fig. 4D. For a twofold increase in the inhaled dose per kilogramme body weight (100 to 200 mg/kg), the creatinine-normalized concentration of the metabolite is increased by a factor of 2.23 (1,029 to 2,301 mg/g creatinine).
Discussion
1-OHP and creatinine excretion profiles
In a recent paper, Harris et al. [7] argued that creatinine normalization was of little value in improving dose estimates from pesticide exposure based on 24-h urine collection. However, it is known that 24-h creatinine excretion is much less variable than short-term (<4 h) excretion rates [5]. Since spot urine samples are most commonly used for routine biological monitoring purposes, the question of the value of creatinine normalization remains. Mutti [34] recently argued that creatinine normalization is useful not merely to reduce variance of the data, but because it is based on physiological grounds.
The parallelism between the urinary excretion rates of 1-OHP and creatinine has already been described by Vu-Duc and Lafontaine [29]. As illustrated in Fig. 1, since the publication of this latter paper, more examples have been gathered in people subject to and not subject to occupational exposure to PAHs. Furthermore, exposure to PAHs in the examples given occurs from respiratory, dermal or mixed respiratory/dermal exposures. Because of this accumulating evidence, it was felt that adjustment of the urinary excretion rates of 1-OHP to that of creatinine could perhaps offer a better database for the analysis of the toxicokinetic urinary excretion profile of 1-OHP.
As indicated in the Introduction, some of the variations in creatinine excretion rate over the course of a day are due to variations in glomerular filtration rate. If 1-OHP is mainly excreted through glomerular filtration, it can reasonably be postulated that the variations in its excretion rate, other than those due to variations in exposure rate to the parent compound, pyrene, would parallel those of creatinine. Furthermore, despite the precautions taken to gather all the required urine samples and information to establish the urinary excretion profiles in workers, it is conceivable that certain samples or information pertaining to them might have been missed. For example, a worker might have forgotten to collect a sample, creating a discrepancy between a given sample and its assumed corresponding time interval. Indeed, some morning urine sample volumes of about 100 ml were recorded in individuals with “usual” overnight urination volumes of around 500 ml. Under these circumstances, creatinine normalization may serve to compensate for an incomplete sampling.
Creatinine normalization for kinetic analysis
If the impact of creatine consumption through meat ingestion is neglected, the creatinine excretion rate should be mainly influenced by variations in glomerular filtration rate. In the case of 1-OHP, an important factor explaining variations in its excretion rate is obviously pyrene exposure rate. It could, therefore, be argued that the parallelism described earlier is coincidental. If one considers, more specifically, the excretion profiles in individuals exposed by the inhalation route “only”, it can reasonably be assumed that absorption of pyrene ceases almost at the same time as the end of the work shift, contrary to dermal exposure where the reservoir effect of the skin can prolong systemic exposure [24]. Under these circumstances, the excretion profile of 1-OHP during the elimination phase should be smooth. The unadjusted excretion rate profiles in such cases sometimes exhibit sudden troughs that almost completely disappear when the results are adjusted for creatinine excretion rate (see Fig. 2A). Some profiles also exhibit peaks that could be the result of incorrectly noted time of urination and/or a transient increase in glomerular filtration rate. These also tend to disappear after 1-OHP excretion rate is adjusted for creatinine excretion rate.
These observations lend credence to the hypothesis that both 1-OHP and creatinine are excreted in the urine by similar mechanisms, thus making creatinine normalization appropriate both for spot urine sample collection in routine biomonitoring and for the toxicokinetic analysis of urinary 1-OHP.
“Extreme” creatinine concentrations
Figure 3 suggests that for 1-OHP measurement in the context of biological monitoring, creatinine normalization can be utilized even for very diluted (urine creatinine <0.5 g/l) or very concentrated (urine creatinine >3 g/l) urine samples. This is an important observation, as it reduces the number of rejected samples due to the said “excessively” diluted or concentrated samples. In some workplaces where workers may accomplish their tasks in a hot environment with insufficient hydration, this may be especially interesting. Conversely, some workers drink a lot of water and frequently have “diluted” urine samples that can thus still be used for biomonitoring of exposure to (PAHs) pyrene.
Impact of creatinine normalization for prevention purposes
The main objective of creatinine normalization has always been to provide a means for one to take into account the potentially large intra- and inter-individual differences in diuresis and thus prevent the occurrence of false negative or false positive values due to very dilute or very concentrated urine samples [5, 18]. Guideline values for urinary biomarkers are often given as creatinine-normalized values. However, as very large differences in anthropometrical measurements between workers may be encountered, some have argued that creatinine normalization suffers from the fact that creatinine excretion rate is related to muscle mass and, hence, to body mass.
Under resting conditions, weight is also associated with pulmonary ventilation. From examples of men with weights varying from 50 kg to 100 kg, it was shown that exposure to a given concentration of a pollutant in these conditions should result in small differences in exposure dose, expressed per kilogramme of body weight, and in similarly small differences in creatinine-normalized metabolite excretion. A constant BMI was set for these examples so that the introduction of large inter-individual differences in the proportion of adipose tissue would be avoided.
Of course, at-rest conditions are not representative of working conditions. Therefore, for an example at the other end of the spectrum, it was hypothesized that the effort required to accomplish a given task was the main driving parameter of ventilation and that body weight effect on ventilation could be neglected. This should result in a similar absolute inhaled dose for all individuals having the same pulmonary ventilation. Even under these conditions, the creatinine-normalized concentrations of metabolite follow the body weight-adjusted dose very closely. Indeed, the 50-kg person has twice as high a body weight-adjusted dose and displays a creatinine-normalized metabolite concentration that is 2.23-times higher than in the 100 kg person. Creatinine normalization, therefore, not only serves as an adjustment parameter for the varying degree of dilution of the urine, but also adjusts for the body weight-normalized dose.
Admittedly, this theoretical calculation does not take into account either differences in metabolism or other parameters that could influence the rate of excretion of a metabolite following exposure to a parent compound. It does, however, illustrate that, all other things being equal, creatinine normalization is useful and should be used when it can be considered that the metabolite urinary excretion kinetics parallels that of creatinine, as was shown here for 1-OHP. Although, on a group basis, creatinine-normalized metabolite concentrations may not always lead to better correlations with exposure than non-normalized concentrations, it appears that creatinine normalization will reduce systematic errors that could result from the use of unadjusted values.
Conclusion
Based on a large number (50) of occupationally and non-occupationally exposed individuals, it appears that the creatinine excretion rate-adjusted excretion rate of 1-OHP allows for better determination of the toxicokinetics parameters of 1-OHP urinary excretion. Furthermore, at least in the case of 1-OHP, creatinine normalization can apparently be used even on urine samples with creatinine concentrations smaller than 0.5 g/l or higher than 3 g/l. Finally, because creatinine normalization not only compensates for variable diuresis but also correlates better with body weight-normalized dose of the parent compound, it should be used in biological monitoring of exposure to (PAHs) pyrene and to other substances whose urinary biomarker excretion kinetics parallel that of creatinine.
References
Wyss M, Kaddurah-Daouk R (2000) Creatine and creatinine metabolism (review). Physiol Rev 80:1107–1213
Selberg O, Sel S (2001) The adjunctive value of routine biochemistry in nutritional assessment of hospitalized patients (review). Clin Nutr 20:477–485
Proctor DN, O’Brien PC, Atkinson EJ, Nair KS (1999) Comparison of techniques to estimate total body skeletal muscle mass in people of different age groups. Am J Physiol Endocrinol Metab 40:E489–E495
Virgili F, Maiani G, Zahoor ZH, Ciarapica D, Raguzzini A, Ferroluzzi A (1994) Relationship between fat-free mass and urinary excretion of creatinine and 5-methylhistidine in adult humans. J Appl Physiol 76:1946–1950
Boeninger MF, Lowry LK, Rosenberg J (1993) Interpretation of urine results used to assess chemical exposure with emphasis on creatinine adjustments: a review. Am Ind Hyg Assoc J 54:615–627
Mayersohn M, Conrad KA, Achari R (1983) The influence of a cooked meat meal on creatinine plasma concentration and creatinine clearance. Br J Clin Pharmacol 15:227–230
Harris SA, Purdham JT, Corey PN, Sass-Kortsak AM (2000) An evaluation of 24-hour urinary creatinine excretion for use in identification of incomplete urine collections and adjustment of absorbed dose of pesticides. Am Ind Hyg Assoc J 61:649–657
Levey AS, Bosch JP, Coggins CH, Greene T, Mitch WE, Schluchter MD, Schwab SJ (1996) Effects of diet and antihypertensive therapy on creatinine clearance and serum creatinine concentration in the modification of diet in renal disease study. J Am Soc Nephrol 7:556–566
Palma A, Milan JA, Roa L (1995) Does tubular secretion of creatinine increase after a meat meal?. Nephron 69:116–117
Hultman E, Soderlund K, Timmons JA, Cederblad G, Greenhaff PL (1996) Muscle creatine loading in men. J Appl Physiol 81:232–237
Voogel AJ, Koopman MG, Hart AAM, Van Montfrans GA, Arisz L (2001) Circadian rhythms in systemic hemodynamics and renal function in healthy subjects and patients with nephrotic syndrome. Kidney Int 59:1873–1880
Fournier A, Achard JM (2000) Validation du recueil des urines de 24 heures par l’estimation de la créatininurie des 24 heures d’après la formule de Cockroft et Gault. Nephrologie 21:27–28
Fournier A, Achard JM (2000) Mnemotechnical note on the use of Cockroft creatinine clearance formula for the validation of a 24-h urine collection. Nephrol Dial Transplant 15:1677–1678
Illner K, Brinkmann G, Heller M, Bosy-Westphal A, Muller MJ (2000) Metabolically active components of fat free mass and resting energy expenditure in nonobese adults. Am J Physiol Endocrinol Metab 278:E308–E315
Piers LS, Soares MJ, McCormack LM, O’Dea K (1998) Is there evidence for an age-related reduction in metabolic rate? J Appl Physiol 85:2196–2204
Horwat F, Meyer JP (1998) Débit ventilatoire de travail. Documents pour le Médecin du Travail 76:343–350
Eaton DL, Klaassen CD (2001) Principles of toxicology. In: Klaassen CD (ed) Casarett & Doull’s Toxicology, 6th edn. McGraw-Hill, pp 11–35
Lauwerys RR, Hoet P (2001) Industrial chemical exposure: guidelines for biological monitoring,3rd edn. Lewis, Boca Raton
Carrieri M, Trevisan A, Bartolucci GB (2001) Adjustment to concentration–dilution of spot urine samples: correlation between specific gravity and creatinine. Int Arch Occup Environ Health 74:63–67
Wedeen RP (1996) Commentary on “Adjustment of creatinine-adjusted value to urine flow rate in lead workers”. Arch Environ Health 51:333
Greenberg GN, Levine RJ (1989) Urinary creatinine excretion is not stable: a new method for assessing urinary toxic substance concentrations. J Occup Med 31:832–838
Sata F, Araki S (1996) Adjustment of creatinine-adjusted value to urine flow rate in lead workers. Arch Environ Health 51:329–333
Alessio L, Berlin A, Dell’Orto A, Toffoletto F, Ghezzi I (1985) Reliability of urinary creatinine as a parameter used to adjust values of urinary biological indicators. Int Arch Occup Environ Health 55:99–106
Bouchard M, Viau C (1999) Urinary 1-hydroxypyrene as a biomarker of exposure to polycyclic aromatic hydrocarbons: biological monitoring strategies and methodology for determining biological exposure indices for various work environments. Biomarkers 4:159–187
Järvholm B, Nordström G, Högstedt B, Levin JO, Wahlström J, Östman C, Bergendahl C (1999) Exposure to polycyclic aromatic hydrocarbons and genotoxic effects on nonsmoking Swedish road pavement workers. Scand J Work Environ Health 25:131–136
Kuljukka T, Vaaranrinta R, Mutanen P, Veidebaum T, Sorsa M, Kalliokoski P, Peltonen K (1997) Assessment of occupational exposure to PAHs in an Estonian coke oven plant: correlation of total external exposure to internal dose measured as 1-hydroxypyrene concentration. Biomarkers 2:87–94
Levin JO, Rhén M, Sikström E (1995) Occupational PAH exposure: urinary 1-hydroxypyrene levels of coke oven workers, aluminum smelter pot-room workers, road pavers, and occupationally non-exposed persons in Sweden. Sci Total Environ 163:169–177
Lafontaine M, Payant JP, Delsaut P, Morele Y (2000) Polycyclic aromatic hydrocarbon exposure in an artificial shooting target factory: assessment of 1-hydroxypyrene urinary excretion as a biological indicator of exposure. Ann Occup Hyg 44:89–100
Vu-Duc T, Lafontaine M (1999) Some observations on the kinetics of urinary 1-hydroxypyrene in workers exposed to PAHs and its use to assess exposure. Polycyclic Aromatic Compounds 17:187–195
Lafontaine M, Gendre C, Morele Y, Laffitte-Rigaud G (2002) Excretion of urinary 1-hydroxypyrene in relation to the penetration routes of polycyclic aromatic hydrocarbons. Polycyclic Aromatic Compounds 22:579–588
Simon P, Morele Y, Delsaut P, Nicot T (1999) Automated column-switching high-performance liquid chromatography method for the determination of 1-hydroxypyrene in human urine. J Chromatogr B 732:91–101
Lin PH, Proschan MA, Bray GA, Fernandez CP, Hoben K, Most-Windhauser M, Karanja N, Obarzanek E (2003) Estimation of energy requirements in a controlled feeding trial. Am J Clin Nutr 77:639–645
Layton DW (1993) Metabolically consistent breathing rates for use in dose assessments (comment) (erratum appears in Health Phys 64:561). Health Phys 64:23–36
Mutti A (1999) Biological monitoring in occupational and environmental toxicology. Toxicol Lett 108:77–89
Acknowledgements
This work was carried out while C.V. was on sabbatical leave at the Institut National de Recherche et de Sécurité, Vandoeuvre-les-Nancy, France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Viau, C., Lafontaine, M. & Payan, J.P. Creatinine normalization in biological monitoring revisited: the case of 1-hydroxypyrene. Int Arch Occup Environ Health 77, 177–185 (2004). https://doi.org/10.1007/s00420-003-0495-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-003-0495-9