Abstract
Diacylglycerol kinase (DGK) plays a key role in pathophysiological cellular responses by regulating the levels of a lipid messenger diacylglycerol. Of DGK isozymes, DGKζ localizes to the nucleus in various cells such as neurons. We previously reported that DGKζ translocates from the nucleus to the cytoplasm in hippocampal CA1 pyramidal neurons after 20 min of transient forebrain ischemia. In this study, we examined the underlying mechanism of DGKζ translocation using hippocampal slices exposed to oxygen-glucose deprivation (OGD) to simulate an ischemic model of the brain. DGKζ-immunoreactivity gradually changed from the nucleus to the cytoplasm in CA1 pyramidal neurons after 20 min of OGD and was never detected in the nucleus after reoxygenation. Intriguingly, DGKζ was detected in the nucleus at 10 min OGD whereas the following 60 min reoxygenation induced complete cytoplasmic translocation of DGKζ. Morphometric analysis revealed that DGKζ cytoplasmic translocation correlated with nuclear shrinkage indicative of an early process of neuronal degeneration. The translocation under OGD conditions was blocked by NMDA receptor (NMDAR) inhibitor, and was induced by activation of NMDAR. Chelation of the extracellular Ca2+ blocked the translocation under OGD conditions. These results show that DGKζ cytoplasmic translocation is triggered by activation of NMDAR with subsequent extracellular Ca2+ influx. Furthermore, inhibition of PKC activity under OGD conditions led to nuclear retention of DGKζ in about one-third of the neurons, suggesting that PKC activity partially regulates DGKζ cytoplasmic translocation. These findings provide clues to guide further investigation of glutamate excitotoxicity mechanisms in hippocampal neurons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To maintain normal function and viability, the brain requires a continuous supply of oxygen and glucose. Cessation of blood supply attributable to arterial occlusion or cardiac arrest can engender neuronal death (Dirnagl et al. 1999). The molecular mechanisms responsible for neuronal damage are incompletely understood, although glutamate is widely accepted as playing a key role in the early phase of ischemic brain injury (Ikegaya et al. 2001; Lau and Tymianski 2010). Glutamate excitotoxicity causes a massive influx of Ca2+ that activates various catabolic processes, culminating in neuronal cell death (Choi 1985, 1995; Lau and Tymianski 2010). Furthermore, previous reports show that prominent changes in lipids are accompanied in the ischemic brain, in which a rapid decrease in phosphatidylinositol-4,5-bisphosphate (PIP2) levels together with a parallel accumulation of diacylglycerol (DG) occurs (Kunievsky et al. 1992). These findings suggest that phosphoinositide (PI) pathway is involved in this process. Of the PI-related enzymes, DG kinase (DGK), an enzyme responsible for phosphorylation of second messenger DG to phosphatidic acid, plays a central role in controlling DG-dependent signaling pathways (Kanoh et al. 1990).
The DGK family constitutes of several isozymes, which show distinct properties including structural motif, enzymatic characteristics, subcellular localization, and binding partner (Goto et al. 2007; Merida et al. 2008; Sakane et al. 2007; Topham and Epand 2009). We have isolated several DGK isozymes from rats and examined their gene expression in the brain using in situ hybridization histochemistry (Goto et al. 1992, 1994, 2007; Goto and Kondo 1993, 1996, 1999; Ito et al. 2004). Intriguingly, the mRNA for each isozyme is expressed in a distinct pattern in the brain, suggesting that each isozyme plays a unique role in various signaling pathways under a distinct regulatory mechanism.
Of DGKs, DGKζ is characterized by the presence of a nuclear localization signal (NLS). It localizes primarily to the nucleus of neurons in various regions of the brain under normal conditions, including the olfactory bulb, cerebral and cerebellar cortices, and hippocampus (Goto and Kondo 1996; Hozumi et al. 2003). However, we previously reported that, in 20 min of transient forebrain ischemia, DGKζ translocates from the nucleus to the cytoplasm in pyramidal neurons of the hippocampal CA1 region and that it is never relocated to the nucleus during the time course of reperfusion (Ali et al. 2004). Delayed neuronal death in the hippocampal CA1 neurons is well known to occur after 48–72 h reperfusion in a transient ischemia model (Kirino 1982). Our data suggest that the translocation of DGKζ might be involved in the early process of selective vulnerability of hippocampal neurons in the post-ischemic brain. However, the detailed mechanism of DGKζ translocation and its functional significance remain to be elucidated.
In this study, we approached these issues using acute hippocampal slices, a common experimental system for a model of analyses such as histochemical, physiological, and pharmacological examinations. An acute slice system confers an advantage not only in maintaining neuronal connectivity and relation with glial cells but also in manipulating the environmental conditions (Gahwiler et al. 1997). We used hippocampal slices exposed to oxygen–glucose deprivation (OGD) to simulate an ischemic model of the brain, and evaluated the triggering cascade and detailed time course of DGKζ translocation by immunohistochemical analysis using pharmacological agents. Here we show that DGKζ cytoplasmic translocation is well recapitulated in hippocampal slices exposed to OGD, which reveals that the translocation is triggered by activation of N-methyl-D-aspartate (NMDA) receptor followed by extracellular Ca2+ influx. These results suggest that DGKζ cytoplasmic translocation is closely involved in glutamate excitotoxicity in hippocampal neurons.
Materials and methods
Acute hippocampal slices
All experiments were conducted in accordance with the Yamagata university guide for the care and use of laboratory animals and were approved by the Yamagata university institutional animal care and use committee. Male Sprague–Dawley rats (4–7 weeks old) were anesthetized with ether and decapitated. Immediately after decapitation, the brain was removed from the skull; within 2 min, the right hippocampus was placed in chilled (4°C) artificial cerebrospinal fluid (ACSF) equilibrated with 95% O2 and 5% CO2. The composition of the solution was (mM): NaCl 124, NaH2PO4 1.25, KCl 3.0, MgSO4 2.0, NaHCO3 22, CaCl2 2.5, and glucose 10. The hippocampus was sliced to thickness of 500 μm using a rotor slicer (DTY-7700; Dosaka EM Co. Ltd., Osaka), transferred to a regular chamber containing oxygenated ACSF, and incubated for 2 h at temperature of 30°C before use in experiments (Yamazaki et al. 2007). About ten slices were obtained from one hippocampus. At least eight slices were used for each experiment. Control experiments in each condition were performed on slices derived from the one and the same hippocampus. We used at least three slices in each group of the experiment. One slice provided 5–10 cryostat sections suitable for immunohistochemistry.
Oxygen–glucose deprivation
To simulate an ischemic model of the brain, the hippocampal slices were transferred to an oxygen–glucose deprivation (OGD) chamber containing glucose-deficient ACSF equilibrated with 95% N2 and 5% CO2 at 30°C. Subsequently, to simulate a reperfusion model of the brain, some hippocampal slices were returned to a regular chamber containing oxygenated (95% O2 and 5% CO2) ACSF with 10 mM glucose (designated simply as ‘reoxygenation’).
Glutamatergic receptor, VDCC, and enzyme inhibition
Hippocampal slices were exposed to 10 min OGD, with subsequent incubation in a regular chamber for 30 min, under which conditions DGKζ translocated to the cytoplasm. To investigate the relevance to glutamate signaling pathways, glutamate receptor antagonists, including d,l-2-amino-5-phosphonopentanoic acid (AP5, 50 μM) (Sigma, St. Louis, MO, USA), methyl-4-carboxyphenylglycine (MCPG, 500 μM) (Tocris Bioscience, Bristol, UK), and 6,7-dinitroquinoxaline-2,3-dione (DNQX, 20 μM) (Sigma, St. Louis, MO, USA) were added to the chamber (Yamazaki et al. 2005). CdCl2 (200 μM) (Wako Pure Chemical Industries Ltd., Osaka, Japan) was used to block voltage-dependent calcium channels (VDCC). The hippocampal slices were incubated with agents 10 min before the experiment was started. Ca2+ free conditions were established by superfusing the slices with ACSF in which CaCl2 was replaced by MgCl2. In some experiments, enzyme inhibitors such as 1-[N,O-bis(5-isoquinolinesulfonyl)-N-methyl-L-tyrosyl]-4-phenylpiperazine (KN-62, 10 μM) (Biomol International, Plymouth Meeting, PA, USA), Tacrolimus (FK506, 10 μM) (Sigma, St. Louis, MO, USA) (Yamazaki et al. 2011), N-(6-aminohexyl)-5-chloro-1-naphthalenesulfonamide hydrochloride (W7, 100 μM) (Calbiochem, San Diego, CA), and bisindolylmaleimide I (GF 109203X, 1 μM) (Calbiochem, San Diego, CA) were used.
Glutamatergic receptor stimulation and VDCC activation
Hippocampal slices were incubated in a regular chamber for 30 min, under which conditions DGKζ remained in the nucleus. To stimulate VDCC by depolarization, the concentration of potassium in ACSF was changed from 3.0 to 52 mM together with AP5 (50 μM) and DNQX (20 μM) to inhibit other receptors. To stimulate α-amino-3-hydroxy-5-methyl-4-isoxazole propionate (AMPA) receptors (AMPAR), AMPA (100 μM) was added together with CdCl2 (200 μM), AP5 (50 μM) and tetrodotoxin (TTX, 0.5 μM) (Sigma, St. Louis, MO, USA) to inhibit other receptors. To stimulate NMDAR, NMDA (1 mM) was added together with CdCl2 (200 μM), DNQX (20 μM), and TTX (0.5 μM) to inhibit other receptors. In addition, the concentration of MgSO4 in ACSF was changed from 2.0 to 0.1 mM to relieve Mg2+ block of NMDAR (Yamazaki et al. 2006). Moreover, KCl was changed from 3.0 to 5.0 mM to maintain equilibrium. In some experiments, calcium ionophore (A23187, 1 μM) (Sigma, St. Louis, MO, USA) was added to raise the intracellular calcium.
Immunohistochemistry
Hippocampal slices were fixed by immersion for 2 h in 4% phosphate-buffered (pH 7.4) paraformaldehyde at 4°C immediately after the end of the experiment. They were kept in 30% sucrose in 0.1 M phosphate buffer until use. The slices were cut into sagittal sections (30 μm) on a cryostat (Leica CM1900; Leica Microsystems). Free-floating sections were soaked with 0.5% Triton-X in phosphate-buffered saline (PBS) for 15 min at room temperature (RT) to facilitate antibody penetration. Non-specific binding sites were blocked with 10% normal horse serum in PBS for 30 min at RT. The primary antibodies used were rabbit anti-DGKζ (1.0 μg/ml) (Hozumi et al. 2003) and goat anti-PKCγ (1.0 μg/ml) (Hozumi et al. 2010; Yoshida et al. 2006) antibodies in PBS containing 0.1% Tween-20 (PBS-T). Incubation was performed overnight at RT in a moist chamber. After washing in PBS-T several times, slices were incubated with anti-rabbit IgG-Alexa 546 (red) (Molecular Probes Inc., Eugene, OR, USA) for anti-DGKζ antibody, or anti-goat IgG-Alexa 488 (green) (Molecular Probes Inc.) for anti-PKCγ antibody in PBS-T for 2 h at RT. To stain nuclei, some slices were also incubated with TO-PRO-3 (2.5 μM) in the same solution for 2 h at RT in the dark. The images were taken under a confocal laser-scanning microscope (LSM 510META; Carl Zeiss Inc.) and processed using Adobe Photoshop (Adobe Systems Inc.). For morphometric analysis of nuclear shrinkage, a fluorescence photomicrograph was taken at high magnification within the CA1 pyramidal cell layer. The well-focused cell nuclei areas (n > 100) were delineated and measured using Image J software. Student’s t test was used to compare the degrees of shrinkage.
Results
We previously reported that in a transient cerebral ischemia model of rats DGKζ translocates from the nucleus to the cytoplasm and is never relocated to the nucleus after reperfusion (Ali et al. 2004). To simulate an ischemic model of the brain, we used acute hippocampal slices exposed to oxygen–glucose deprivation (OGD) and evaluated the triggering cascade and detailed time course of DGKζ translocation using immunohistochemical analysis with pharmacological agents.
Cytoplasmic translocation of DGKζ induced by OGD
Hippocampal slices were incubated for 2 h in a chamber containing oxygenated ACSF with glucose at 30°C before the experiments. Under these conditions (control), DGKζ immunoreactivity was detected predominantly in the nucleus of hippocampal CA1 neurons in slice (Fig. 1a). This pattern of DGKζ subcellular localization is principally similar to that in the brain (Hozumi et al. 2003), but the immunoreactivity in hippocampal slices under normal conditions was also observed to some degree in the cytoplasm. A slight difference of subcellular localization pattern might simply reflect different conditions between in vivo and in slices.
Subcellular localization of DGKζ in hippocampal slices exposed to continuous oxygen-glucose deprivation (OGD). Immunofluorescent photomicrographs of DGKζ in hippocampal CA1 neurons exposed to OGD for 0 (a), 10 (b), 20 (c), and 30 (d) min. Under control conditions (a), DGKζ is detected predominantly in the nucleus in hippocampal CA1 neurons. After 20 min OGD DGKζ gradually translocates to the cytoplasm (c, arrows) and is predominantly detected in the cytoplasm at 30 min OGD (d, arrows). Scale bars 20 μm
Under continuous OGD conditions, DGKζ immunoreactivity remained nuclear at 10 min OGD (Fig. 1b). However, after 20 min OGD, the immunoreactivity changed gradually from the nucleus to the cytoplasm (Fig. 1c) and was detected predominantly in the cytoplasm at 30 min OGD (Fig. 1d). This result shows that nucleocytoplasmic translocation of DGKζ was induced after 20 min of continuous OGD in hippocampal CA1 neurons. It should be noted that DGKζ cytoplasmic translocation was not observed in CA2, CA3, and dentate gyrus neurons at least under 30 min OGD conditions (data not shown).
DGKζ cytoplasmic translocation induced by transient OGD followed by reoxygenation
Delayed neuronal cell death is well known to occur in CA1 neurons after 48–72 h reperfusion in a transient ischemia model (Kirino 1982). Therefore, we investigated whether DGKζ cytoplasmic translocation would be induced by transient OGD followed by reoxygenation (Fig. 2). Hippocampal slices were subjected to 10 min OGD, which was insufficient to induce translocation. They were subsequently returned to a regular chamber containing oxygenated ACSF with glucose (simply ‘reoxygenation’ hereinafter). As presented in Fig. 1b, DGKζ remained in the nucleus at 10 min OGD, although it gradually changed from the nucleus to the cytoplasm after 10 min reoxygenation (Fig. 2c, arrowheads). After 20 min reoxygenation, DGKζ was detected almost entirely in the cytoplasm (Fig. 2d, e, arrows). DGKζ cytoplasmic translocation under conditions of transient OGD followed by reoxygenation appeared more extensive than that under continuous OGD (Fig. 1c, d). Furthermore, it is noteworthy that DGKζ was never detected in the nucleus during the course of reoxygenation at least until 60 min (Fig. 2f), a phenomenon similar to that observed in our previous study of a transient ischemic brain (Ali et al. 2004).
Subcellular localization of DGKζ in hippocampal slices exposed to 10 min OGD followed by varying times of reoxygenation. Immunofluorescent photomicrographs of DGKζ in hippocampal CA1 neurons exposed to 10 min OGD followed by reoxygenation for 0 (b), 10 (c), 20 (d), 30 (e), and 60 (f) min. Under control conditions (a), DGKζ is detected predominantly in the nucleus in hippocampal CA1 neurons. After 10 min reoxygenation DGKζ gradually translocates to the cytoplasm (c, arrowheads) and is entirely detected in the cytoplasm at 30 min OGD (e, arrows). DGKζ is never relocated to the nucleus during the course of reoxygenation until 60 min (f). Scale bars 20 μm
Next, to investigate the minimum duration of OGD sufficient to induce DGKζ cytoplasmic translocation, hippocampal slices were subjected to varying times of OGD followed by 60 min reoxygenation. 6 min of OGD/reoxygenation did not induce translocation (Fig. 3b), although 8 min OGD induced the translocation in about half of the CA1 neurons after 60 min reoxygenation (Fig. 3c), and 10 min OGD was sufficient to induce the translocation in almost all the neurons (Fig. 3d). Taken together, these results can be summarized as follows: (1) 8–10 min OGD is sufficient to trigger the signaling cascade to induce DGKζ cytoplasmic translocation in CA1 neurons after 60 min reoxygenation in slices; (2) DGKζ is never relocated to the nucleus during the course of reoxygenation; and (3) its cytoplasmic translocation under conditions of transient OGD followed by reoxygenation appears more extensive than that under continuous OGD, suggesting that the translocation should be an energy-requiring process.
Subcellular localization of DGKζ in hippocampal slices exposed to varying times of OGD followed by 60 min reoxygenation. Immunofluorescent photomicrographs of DGKζ in hippocampal CA1 neurons exposed to 6 (b), 8 (c), and 10 (d) min OGD followed by 60 min reoxygenation. Under control conditions (a), DGKζ is detected predominantly in the nucleus in hippocampal CA1 neurons. 6 min OGD/reoxygenation does not induce DGKζ cytoplasmic translocation (b), whereas 8 min OGD/reoxygenation induces the translocation in about half of the CA1 neurons (c, arrows). 10 min OGD/reoxygenation completely induces the translocation in almost all of the CA1 neurons. Scale bars 20 μm
OGD-induced DGKζ cytoplasmic translocation correlates with nuclear shrinkage
OGD induces morphological and biochemical changes in hippocampal slices, which engender neuronal cell death (Bonde et al. 2005; Frantseva et al. 1999; Kass and Lipton 1982). Nuclear shrinkage is an early and easily quantifiable indicator of neuronal degeneration in hippocampal slices (Bonde et al. 2002). We therefore examined whether DGKζ translocation induced by OGD would correlate with neuronal degeneration. Hippocampal slices subjected to continuous or transient OGD were stained with nuclear marker TO-PRO-3, and cross-sectional areas of all well-focused neuronal nuclei in CA1 pyramidal layer were delineated and measured using morphometric analysis. Continuous OGD gradually induced nuclear shrinkage of CA1 neurons. At 15 min OGD, when DGKζ remained in the nucleus, nuclear shrinkage was not significant, although it became statistically evident at 30 and 45 min OGD when DGKζ was observed predominantly in cytoplasm (Fig. 4a, b; p < 0.005). In an experiment of transient OGD followed by 60 min reoxygenation, 5 min OGD/reoxygenation induced no changes in DGKζ localization and the cross-sectional area of CA1 pyramidal cell nuclei whereas 10 min OGD/reoxygenation clearly induced its cytoplasmic translocation and nuclear shrinkage of CA1 neurons (Fig. 4c, d; p < 0.005). These results demonstrate a correlation between DGKζ cytoplasmic translocation and nuclear shrinkage, suggesting a functional link between translocation and neuronal degeneration induced by OGD.
Nuclear shrinkage correlates with DGKζ cytoplasmic translocation under OGD conditions. Nuclear staining (TO-PRO-3) of hippocampal CA1 neurons exposed to continuous OGD for 0 (a1), 15 (a2), 30 (a3), and 45 (a4) min or to 5 (c2) and 10 (c3) min OGD followed by 60 min reoxygenation. Cross-sectional areas of all well-focused neuronal nuclei (n > 100) in CA1 pyramidal layer were delineated and measured by morphometric analysis (b continuous OGD, d OGD/reoxygenation). Representative shrunk nuclei were indicated by arrows, and peculiar or elongated nuclei (arrowheads) were removed from the analysis. Inset shows DGKζ immunofluorescence in each condition. The control value was arbitrarily set 100%. The presented data are mean ± SD of at least three separate experiments. Asterisks indicate significance, *p < 0.005 (Student’s t test); n.s. not significant. Scale bars 20 μm
DGKζ cytoplasmic translocation is triggered by NMDA receptor activation followed by extracellular Ca2+ influx
Glutamate excitotoxicity is widely acknowledged to be linked inextricably to neuronal dysfunction and degeneration induced by ischemic brain injury and experimental OGD stress (Choi 1995; Lau and Tymianski 2010). We first examined which glutamate receptor is involved in DGKζ cytoplasmic translocation under OGD conditions using glutamate receptor antagonists. For this purpose, the experiment was performed under conditions of 10 min OGD followed by 30 min reoxygenation, which are confirmed to induce DGKζ cytoplasmic translocation (Fig. 2e). An application of metabotropic glutamate receptor (mGluR) antagonist MCPG failed to block the translocation (Fig. 5a), although AMPAR antagonist DNQX and NMDAR antagonist AP5 inhibited the translocation under OGD/reoxygenation conditions (Fig. 5b, c).
Subcellular localization of DGKζ in hippocampal slices exposed to OGD/reoxygenation in the presence of glutamate receptor antagonists. Immunofluorescent photomicrographs of DGKζ in hippocampal CA1 neurons exposed to 10 min OGD followed by 30 min reoxygenation in the presence of MCPG (a mGluR antagonist), DNQX (b AMPAR antagonist), or AP5 (c MNDAR antagonist). Inset shows DGKζ immunofluorescence in each condition without antagonist (vehicle only). An application of MCPG (a) fails to block DGKζ cytoplasmic translocation, whereas DNQX (b) and AP5 (c) inhibit the translocation under OGD/reoxygenation conditions (arrows). Scale bars 20 μm
We next performed the reverse experiment and stimulated glutamate receptors using their agonists. For this purpose, hippocampal slices were incubated under normal conditions including oxygen and glucose. An application of NMDA clearly induced DGKζ cytoplasmic translocation (Fig. 6a), although AMPA failed to induce the translocation (Fig. 6b). These data suggest that NMDAR triggers activation DGKζ cytoplasmic translocation.
Subcellular localization of DGKζ in hippocampal slices under normal conditions in the presence of glutamate receptor agonists. Immunofluorescent photomicrographs of DGKζ in hippocampal CA1 neurons under normal conditions for 30 min in the presence of NMDA (a NMDAR agonist) and AMPA (b AMPAR agonist). Inset shows DGKζ immunofluorescence in each condition without agonist (vehicle only). An application of NMDA clearly induces DGKζ cytoplasmic translocation (a arrows) whereas AMPA fails to induce the translocation (b). Scale bars 20 μm
Once activated by excessive levels of glutamate, the NMDAR allows excessive Ca2+ influx (Lau and Tymianski 2010). Elevated intracellular Ca2+ levels engender overactivation of several deleterious enzymes and signaling processes that impair neuronal function, culminating in cell death (Choi 1985). Major routes of Ca2+ entry into neurons after ischemia are via NMDAR and voltage-dependent Ca2+ channel (VDCC) (Bertolino and Llinas 1992; Miller 1987). We next investigated whether DGKζ cytoplasmic translocation would also be induced by Ca2+ influx through the other routes using CdCl2 (VDCC blocker) and A23187 (Ca2+ ionophore) or under conditions of high K+ concentration ACSF sufficient to open VDCC. Results show that an incubation in Ca2+ eliminated ACSF inhibited translocation under OGD conditions (Fig. 7a, arrowheads), suggesting that the translocation process requires extracellular Ca2+ influx. An application of CdCl2 failed to inhibit the translocation under OGD/reoxygenation conditions (Fig. 7b), and a high concentration of K+ did not induce translocation under normal conditions (Fig. 7c), showing that the translocation process is not triggered by Ca2+ influx through VDCC. Similarly, an application of Ca2+ ionophore A23187 did not induce translocation under normal conditions (Fig. 7d). Collectively, these results suggest that DGKζ cytoplasmic translocation is triggered by extracellular Ca2+ influx almost entirely via NMDAR activation.
Effect of Ca2+ on subcellular localization of DGKζ. a Immunofluorescent photomicrograph of DGKζ in hippocampal CA1 neurons exposed to 10 min OGD/30 min reoxygenation in Ca2+-free medium. Inset shows DGKζ immunofluorescence under the same conditions in 2.5 mM Ca2+-containing medium. b Immunofluorescent photomicrograph of DGKζ in hippocampal CA1 neurons exposed to 10 min OGD/30 min reoxygenation in the presence of CdCl2 (VDCC inhibitor). Inset shows DGKζ immunofluorescence under the same conditions without inhibitor (vehicle only). c Immunofluorescent photomicrograph of DGKζ in hippocampal CA1 neurons under normal conditions in high (52 mM) K+-containing medium. Inset shows DGKζ immunofluorescence under the same conditions in low (3.0 mM) K+-containing medium. d Immunofluorescent photomicrograph of DGKζ in hippocampal CA1 neurons under normal conditions in the presence of A23187 (Ca2+ ionophore). Inset shows DGKζ immunofluorescence under the same conditions without A23187 (vehicle only). Note that chelation of extracellular Ca2+ inhibits DGKζ cytoplasmic translocation (a arrowheads). Scale bars 20 μm
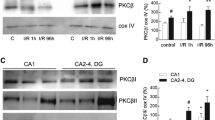
DGKζ cytoplasmic translocation is partially regulated by PKC
Extracellular Ca2+ influx in neurons is well known to activate various molecules such as calmodulin (CaM), calcium–calmodulin-dependent protein kinase II (CaMKII), protein kinase C (PKC), and calcineurin (CaN) (Orrenius et al. 2003; Szydlowska and Tymianski 2010). Therefore we examined the mechanisms of Ca2+ signal transduction pathway to induce DGKζ translocation using inhibitors. For this purpose, hippocampal slices were subjected to 10 min OGD followed by 30 min reoxygenation to induce DGKζ cytoplasmic translocation. As presented in Fig. 8, an application of CaM inhibitor W7 (a), CaMKII inhibitor KN-62 (b) or CaN inhibitor FK-506 (c) failed to inhibit the translocation under OGD/reoxygenation conditions. However, GF109203X, selective PKC inhibitor, suppressed the translocation in 34.1% of the CA1 neurons (Fig. 8d; n > 200), suggesting that DGKζ cytoplasmic translocation is partially, if not entirely, regulated by PKC activity under OGD conditions.
Effect of intracellular Ca2+ signaling on subcellular localization of DGKζ. Immunofluorescent photomicrograph of DGKζ in hippocampal CA1 neurons exposed to 10 min OGD/30 min reoxygenation in the presence of W7 (a CaM inhibitor), KN-62 (b CaMKII inhibitor), FK-506 (c CaN inhibitor), and GF 109203X (d PKC inhibitor). Inset shows DGKζ immunofluorescence under the same conditions without inhibitor (vehicle only). Note that an application of W7 (a), KN-62 (b) or FK-506 (c) fails to inhibit DGKζ cytoplasmic translocation under OGD/reoxygenation conditions whereas GF109203X suppresses the translocation in about half of the CA1 neurons (d, arrowheads). Scale bars 20 μm
PKCγ disappears before DGKζ cytoplasmic translocation
Ca2+-dependent PKCs, which are designated as classical PKCs, include PKCα, PKCβI, PKCβII, and PKCγ. They are fully activated in the presence of DG (Newton 1995; Nishizuka 1995). Because DGK is an enzyme responsible for phosphorylation of DG and because it plays a central role in controlling PKC activity (Sakane and Kanoh 1997), we examined a functional relation between the PKC pathway and DGKζ cytoplasmic translocation. Especially, PKCγ is expressed solely in neurons in the central nervous system (Saito and Shirai 2002) and is shown to be involved in ischemic brain injury (Aronowski et al. 2000; Aronowski and Labiche 2003; Wieloch et al. 1991). Therefore, we first investigated the time course of the immunoreactivities of DGKζ and PKCγ under continuous OGD conditions using immunohistochemical double staining (Fig. 9). Under control conditions, PKCγ was detected mainly at the plasma membrane of CA1 neurons and appeared to draw the outline of neuronal somata; DGKζ was detected predominantly in the nucleus (Fig. 9a). An initial change was observed in PKCγ-immunoreactivity, which became fragmented at 10 min OGD (Fig. 9c, arrowheads) and was greatly reduced at 15 min OGD, whereas DGKζ remained in the nucleus (Fig. 9d). At 20 min OGD, PKCγ-immunoreactivity almost disappeared and DGKζ was detected predominantly in the cytoplasm (Fig. 9e, arrows).
Subcellular localization of DGKζ and PKCγ in hippocampal slices exposed to OGD. Double immunofluorescent photomicrographs of DGKζ (red) and PKCγ (green) in hippocampal CA1 neurons exposed to OGD for 0 (a), 5 (b), 10 (c), 15 (d), and 20 (e) min. Under control conditions (a), DGKζ is detected predominantly in the nucleus and PKCγ localizes to the plasma membrane in hippocampal CA1 neurons. PKCγ becomes gradually fragmented at 10 min OGD (c arrowheads) and almost disappears at 20 min OGD, where DGKζ is detected predominantly in the cytoplasm (e arrows). f Double immunofluorescent photomicrographs of DGKζ and PKCγ in hippocampal CA1 neurons exposed to 10 min OGD/30 min reoxygenation in the presence of GF 109203X (PKC inhibitor). Inset shows the immunofluorescence under the same conditions without inhibitor (vehicle only). Note that in the presence of PKC inhibitor PKCγ remains at the plasma membrane in about half of the CA1 neurons, in which DGKζ also remains in the nucleus (f arrowheads). In contrast, CA1 neurons, in which PKCγ disappears, exhibit cytoplasmic DGKζ (f arrows). Scale bars 20 μm
In an experiment related to OGD/reoxygenation, under conditions of 10 min OGD followed by 30 min reoxygenation, DGKζ translocated entirely to the cytoplasm, whereas PKCγ-immunoreactivity completely disappeared (Fig. 9f, inset). However, under identical conditions but in the presence of selective PKC inhibitor (GF109203X), PKCγ-immunoreactivity remained at the plasma membrane in about one-third of the CA1 neurons, in which DGKζ also remained in the nucleus (arrowheads). In contrast, CA1 neurons showing no PKCγ-immunoreactivity exhibited cytoplasmic DGKζ (arrows). These findings showed that PKCγ disappears prior to DGKζ cytoplasmic translocation under OGD conditions.
Discussion
Cessation of blood supply to the brain during ischemia results in oxygen and glucose deprivation and engenders depletion of cellular energy (Dirnagl et al. 1999). Neurons become unable to maintain the ion gradients for normal function and viability. Glutamate excitotoxicity is widely accepted as induced by massive release and reduced reuptake after ischemia/reperfusion, culminating in neuronal degeneration (Choi 1985, 1995; Lau and Tymianski 2010). We previously reported that DGKζ translocates from the nucleus to the cytoplasm in hippocampal CA1 neurons in 20 min of transient forebrain ischemia. It is never relocated to the nucleus during the course of reperfusion (Ali et al. 2004), suggesting that DGKζ is involved in processes of ischemic injury. However, the detailed mechanism of DGKζ translocation and its functional significance remained to be elucidated. In this study, we addressed these issues using hippocampal slices exposed to OGD to simulate an ischemic model of the brain.
Our immunohistochemical study reveals that DGKζ cytoplasmic translocation is well recapitulated in hippocampal slices exposed to transient OGD. Detailed time course analysis shows that a minimum of 8–10 min OGD is sufficient to induce the translocation in CA1 neurons after following reoxygenation. In addition, cytoplasmic DGKζ is never relocated to the nucleus after reoxygenation. These findings confirm that acute hippocampal slice system we employed here is suitable to simulate DGKζ cytoplasmic translocation observed in an animal model of transient ischemia (Ali et al. 2004). However, it should be noted that the cytoplasmic localization pattern of DGKζ is somewhat different in acute hippocampal slice model of OGD compared with animal model of ischemia. It is presumed to depend on the duration and severity of stress and energy deprivation.
How is DGKζ translocation implicated in neuronal cell death? A well-known histological marker for neuronal degeneration and cell death in hippocampal slices is cellular uptake of the fluorescent dye propidium iodide (PI), which enters cell nucleus after loss of cell membrane integrity (Macklis and Madison 1990). Other markers are staining of degenerating neurons with Fluoro-Jade B (Schmued and Hopkins 2000), release of cytosolic lactate dehydrogenase (LDH) (Noraberg et al. 1999; Ogura et al. 1994), and dendritic loss of immunostaining for microtubule-associated protein 2 (MAP2) (Kwei et al. 1993; Noraberg et al. 1999). However, significant loss of MAP2 staining is detected 6 h after OGD, and other markers can detect neuronal death well after 24 h after exposure to various toxic insults. They are inappropriate in this study to evaluate the correlation between neuronal degeneration and DGKζ translocation that occurs within an hour after OGD. In this regard, nuclear shrinkage is shown to be an early indicator of neuronal injury in hippocampal slices (Bonde et al. 2002). Our morphometric analysis reveals that DGKζ cytoplasmic translocation correlates with nuclear shrinkage, suggesting that DGKζ translocation is presumably an indicator of an early process of neuronal degeneration.
Glutamate excitotoxicity is well known to mediate neuronal cell death after ischemic injury, as explained above. In ischemic brain, overactivated NMDAR allows massive influx of Ca2+, which results in uncontrolled, exaggerated activation of intracellular pathways culminating in neuronal cell death (Choi 1985, 1995; Lau and Tymianski 2010). The present pharmacological approach reveals that DGKζ cytoplasmic translocation is triggered by extracellular Ca2+ influx via NMDAR according to the findings that (1) NMDAR antagonist inhibits the translocation under OGD conditions; (2) NMDAR agonist induces the translocation under normal conditions; and (3) elimination of extracellular Ca2+ blocks translocation under OGD conditions. The reason that AMPAR antagonist DNQX alone inhibits the translocation under OGD conditions (Fig. 5b) might be that AMPAR mediates the fast excitatory component of glutamate. It is thought to relieve the Mg2+ block of NMDAR upon glutamate challenge (Burnashev et al. 1995; Hollmann et al. 1991). In this respect, it should be described that Ca2+ influx via other routes such as VDCC and Ca2+ ionophore fails to induce the translocation under normal conditions. These observations are compatible with the concept known as the ‘source-specificity’ hypothesis that Ca2+ toxicity is linked to the route of Ca2+ entry and the distinct second messenger pathways activated by Ca2+ entry (Arundine and Tymianski 2004; Tymianski et al. 1993). Some routes of Ca2+ entry, such as VDCC, did not elicit cell death, whereas others, such as NMDAR, were associated with significant Ca2+ dependent toxicity (Sattler et al. 1998).
How extracellular Ca2+ influx engenders DGKζ cytoplasmic translocation remains unclear. Ca2+ cytotoxicity is likely to be mediated through various pathways (Manev et al. 1989; Marcoux et al. 1990; Sattler et al. 1998; Tymianski et al. 1993). Major components activated by Ca2+ in neurons include CaMKII, CaN, and PKC. In this regard, we show that selective PKC inhibitor suppresses DGKζ cytoplasmic translocation in about one-third of the CA1 neurons under OGD conditions, suggesting that DGKζ cytoplasmic translocation is partially, if not all, regulated by PKC activity. One mechanism is suggested by a previous study: in cultured cells, phosphorylation of the myristoylated alanine-rich C-kinase substrates (MARCKS) domain that overlaps an NLS of DGKζ (Bunting et al. 1996; Goto and Kondo 1996) can affect its subcellular localization (Topham et al. 1998).
Another finding remains unexplained: disappearance of PKCγ-immunoreactivity from the plasma membrane in the course of OGD before DGKζ cytoplasmic translocation (Fig. 9). Considering that PKCγ is particularly susceptible to proteolytic degradation such as through massive activation of calpains by Ca2+-overload after ischemia (Szydlowska and Tymianski 2010) and that irreversible inactivation of PKC always precedes neuronal damage (Aronowski et al. 2000; Wieloch et al. 1991), overactivation of PKCγ followed by its degradation might induce DGKζ cytoplasmic translocation through unknown mechanisms under OGD conditions.
The functional implication of DGKζ cytoplasmic translocation under ischemia/OGD conditions is expected to be closely related to perturbation of the homeostatic balance of DG metabolism in both the nucleus and the cytoplasm. As described, prominent changes in lipids are reportedly accompanied in the ischemic brain, where a rapid decrease in phosphatidylinositol-4,5-bisphosphate (PIP2) levels together with a parallel accumulation of diacylglycerol (DG) is observed (Kunievsky et al. 1992). In addition, levels of PIP, PIP2, and DG approach plateau values after 10 min of ischemia (Ikeda et al. 1986), a 30 min recirculation period after 15 min of ischemia engenders increases in PIP and PIP2, whereas levels of DG decrease promptly toward control values (Moto et al. 1991; Yoshida et al. 1986). Detailed analysis of lipid changes in distinct subcellular compartments should help to determine how DGKζ cytoplasmic translocation is implicated in DG metabolism, although it might be difficult because of the rapid changes.
The pathophysiological role of DGKζ cytoplasmic translocation remains unclear. Does the translocation exert a protective or destructive effect under stressed conditions? In this regard, our present data on PKCγ might provide a clue to address the question. As described, PKCγ is particularly susceptible to proteolytic degradation after ischemia, and irreversible inactivation of PKC always precedes neuronal damage (Aronowski et al. 2000; Wieloch et al. 1991). Although a positive or negative role of PKCγ in neuroprotection after ischemic insults remains controversial at different stages of injury, PKCγ knockout mice demonstrate worsened injury after a transient ischemia, suggesting that PKCγ might mediate beneficial signaling processes during reperfusion injury (Bright and Mochly-Rosen 2005). Given that DGKζ cytoplasmic translocation correlates with nuclear shrinkage and that it is blocked by PKC inhibitor, presumably DGKζ translocation can be a protective stress response. In this respect, studies of transgenic mice show that cardiac-specific overexpression of DGKζ prevents pathological changes of cardiac muscle induced by Gq protein-coupled receptor agonist (Arimoto et al. 2006) and attenuates left ventricular remodeling after myocardial infarction (Niizeki et al. 2007) and pressure overload-induced cardiac hypertrophy (Harada et al. 2007) whereas these DGKζ-TG mice are indistinguishable from wild type mice in terms of appearance, physiological and histological analyses, and cardiac function under normal conditions.
In addition, pathophysiological implication of DGKζ disappearance from the nucleus should be discussed. Previous study shows that nuclear DGKζ is a negative regulator of cell cycle progression in C2C12 mouse myoblasts (Evangelisti et al. 2007). Furthermore, it is also demonstrated that nuclear DGKζ downregulates the expression of cyclin D through upregulation of BTG, a transcriptional regulator of cyclin D1 with a strong anti-proliferative function (Evangelisti et al. 2009). These studies suggest that downregulation of DGKζ would lead to cell cycle progression. In this regard, neurons are highly differentiated cells that normally never enter a cell cycle, and a number of studies suggests that cell cycle reentry of neurons usually causes cell death (Yang et al. 2003; Herrup and Yang 2007). Therefore it is plausible that DGKζ disappearance from the nucleus would promote cell cycle reentry in postmitotic neurons. Collectively, these findings suggest that DGKζ serves as a sentinel and exerts a beneficial effect on cellular pathophysiology by strictly controlling levels of DG produced in various stresses. Further studies are necessary to address the issues raised above.
In summary, we showed that DGKζ cytoplasmic translocation is well recapitulated in hippocampal slices exposed to OGD and revealed that the mechanism inducing DGKζ cytoplasmic translocation under OGD conditions is clearly compatible with that occurring in ischemic brain injury, i.e., NMDA-mediated Ca2+ influx, suggesting that DGKζ translocation is closely involved in glutamate excitotoxicity. The findings reported herein provide clues that will spur further examination and insight into the mechanism of glutamate excitotoxicity in hippocampal neurons.
References
Ali H, Nakano T, Saino-Saito S, Hozumi Y, Katagiri Y, Kamii H, Sato S, Kayama T, Kondo H, Goto K (2004) Selective translocation of diacylglycerol kinase ζ in hippocampal neurons under transient forebrain ischemia. Neurosci Lett 372:190–195
Arimoto T, Takeishi Y, Takahashi H, Shishido T, Niizeki T, Koyama Y, Shiga R, Nozaki N, Nakajima O, Nishimaru K, Abe J, Endoh M, Walsh RA, Goto K, Kubota I (2006) Cardiac-specific overexpression of diacylglycerol kinase ζ prevents Gq protein-coupled receptor agonist-induced cardiac hypertrophy in transgenic mice. Circulation 113:60–66
Aronowski J, Labiche LA (2003) Perspectives on reperfusion-induced damage in rodent models of experimental focal ischemia and role of gamma-protein kinase C. ILAR J 44:105–109
Aronowski J, Grotta JC, Strong R, Waxham MN (2000) Interplay between the gamma isoform of PKC and calcineurin in regulation of vulnerability to focal cerebral ischemia. J Cereb Blood Flow Metab 20:343–349
Arundine M, Tymianski M (2004) Molecular mechanisms of glutamate-dependent neurodegeneration in ischemia and traumatic brain injury. Cell Mol Life Sci 61:657–668
Bertolino M, Llinas RR (1992) The central role of voltage-activated and receptor-operated calcium channels in neuronal cells. Annu Rev Pharmacol Toxicol 32:399–421
Bonde C, Noraberg J, Zimmer J (2002) Nuclear shrinkage and other markers of neuronal cell death after oxygen-glucose deprivation in rat hippocampal slice cultures. Neurosci Lett 327:49–52
Bonde C, Noraberg J, Noer H, Zimmer J (2005) Ionotropic glutamate receptors and glutamate transporters are involved in necrotic neuronal cell death induced by oxygen-glucose deprivation of hippocampal slice cultures. Neuroscience 136:779–794
Bright R, Mochly-Rosen D (2005) The role of protein kinase C in cerebral ischemic and reperfusion injury. Stroke 36:2781–2790
Bunting M, Tang W, Zimmerman GA, McIntyre TM, Prescott SM (1996) Molecular cloning and characterization of a novel human diacylglycerol kinase ζ. J Biol Chem 271:10230–10236
Burnashev N, Zhou Z, Neher E, Sakmann B (1995) Fractional calcium currents through recombinant GluR channels of the NMDA, AMPA and kainate receptor subtypes. J Physiol 485:403–418
Choi DW (1985) Glutamate neurotoxicity in cortical cell culture is calcium dependent. Neurosci Lett 58:293–297
Choi DW (1995) Calcium: still center-stage in hypoxic-ischemic neuronal death. Trends Neurosci 18:58–60
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22:391–397
Evangelisti C, Tazzari PL, Riccio M, Fiume R, Hozumi Y, Fala F, Goto K, Manzoli L, Cocco L, Martelli AM (2007) Nuclear diacylglycerol kinase-ζ is a negative regulator of cell cycle progression in C2C12 mouse myoblasts. FASEB J 21:3297–3307
Evangelisti C, Astolfi A, Gaboardi GC, Tazzari P, Pession A, Goto K, Martelli AM (2009) TIS21/BTG2/PC3 and cyclin D1 are key determinants of nuclear diacylglycerol kinase-ζ-dependent cell cycle arrest. Cell Signal 21:801–809
Frantseva MV, Carlen PL, El-Beheiry H (1999) A submersion method to induce hypoxic damage in organotypic hippocampal cultures. J Neurosci Methods 89:25–31
Gahwiler BH, Capogna M, Debanne D, McKinney RA, Thompson SM (1997) Organotypic slice cultures: a technique has come of age. Trends Neurosci 20:471–477
Goto K, Kondo H (1993) Molecular cloning and expression of a 90-kDa diacylglycerol kinase that predominantly localizes in neurons. Proc Natl Acad Sci USA 90:7598–7602
Goto K, Kondo H (1996) A 104-kDa diacylglycerol kinase containing ankyrin-like repeats localizes in the cell nucleus. Proc Natl Acad Sci USA 93:11196–11201
Goto K, Kondo H (1999) Diacylglycerol kinase in the central nervous system–molecular heterogeneity and gene expression. Chem Phys Lipids 98:109–117
Goto K, Watanabe M, Kondo H, Yuasa H, Sakane F, Kanoh H (1992) Gene cloning, sequence, expression and in situ localization of 80 kDa diacylglycerol kinase specific to oligodendrocyte of rat brain. Brain Res Mol Brain Res 16:75–87
Goto K, Funayama M, Kondo H (1994) Cloning and expression of a cytoskeleton-associated diacylglycerol kinase that is dominantly expressed in cerebellum. Proc Natl Acad Sci USA 91:13042–13046
Goto K, Hozumi Y, Nakano T, Saino SS, Kondo H (2007) Cell biology and pathophysiology of the diacylglycerol kinase family: morphological aspects in tissues and organs. Int Rev Cytol 264:25–63
Harada M, Takeishi Y, Arimoto T, Niizeki T, Kitahara T, Goto K, Walsh RA, Kubota I (2007) Diacylglycerol kinase ζ attenuates pressure overload-induced cardiac hypertrophy. Circ J 71:276–282
Herrup K, Yang Y (2007) Cell cycle regulation in the postmitotic neuron: oxymoron or new biology? Nat Rev Neurosci 8:368–378
Hollmann M, Hartley M, Heinemann S (1991) Ca2+ permeability of KA-AMPA–gated glutamate receptor channels depends on subunit composition. Science 252:851–853
Hozumi Y, Ito T, Nakano T, Nakagawa T, Aoyagi M, Kondo H, Goto K (2003) Nuclear localization of diacylglycerol kinase ζ in neurons. Eur J Neurosci 18:1448–1457
Hozumi Y, Watanabe M, Goto K (2010) Signaling cascade of diacylglycerol kinase β in the pituitary intermediate lobe: dopamine D2 receptor/phospholipase Cβ4/diacylglycerol kinase β/protein kinase Cα. J Histochem Cytochem 58:119–129
Ikeda M, Yoshida S, Busto R, Santiso M, Ginsberg MD (1986) Polyphosphoinositides as a probable source of brain free fatty acids accumulated at the onset of ischemia. J Neurochem 47:123–132
Ikegaya Y, Kim JA, Baba M, Iwatsubo T, Nishiyama N, Matsuki N (2001) Rapid and reversible changes in dendrite morphology and synaptic efficacy following NMDA receptor activation: implication for a cellular defense against excitotoxicity. J Cell Sci 114:4083–4093
Ito T, Hozumi Y, Sakane F, Saino-Saito S, Kanoh H, Aoyagi M, Kondo H, Goto K (2004) Cloning and characterization of diacylglycerol kinase ι splice variants in rat brain. J Biol Chem 279:23317–23326
Kanoh H, Yamada K, Sakane F (1990) Diacylglycerol kinase: a key modulator of signal transduction? Trends Biochem Sci 15:47–50
Kass IS, Lipton P (1982) Mechanisms involved in irreversible anoxic damage to the in vitro rat hippocampal slice. J Physiol 332:459–472
Kirino T (1982) Delayed neuronal death in the gerbil hippocampus following ischemia. Brain Res 239:57–69
Kunievsky B, Bazan NG, Yavin E (1992) Generation of arachidonic acid and diacylglycerol second messengers from polyphosphoinositides in ischemic fetal brain. J Neurochem 59:1812–1819
Kwei S, Jiang C, Haddad GG (1993) Acute anoxia-induced alterations in MAP2 immunoreactivity and neuronal morphology in rat hippocampus. Brain Res 620:203–210
Lau A, Tymianski M (2010) Glutamate receptors, neurotoxicity and neurodegeneration. Pflugers Arch 460:525–542
Macklis JD, Madison RD (1990) Progressive incorporation of propidium iodide in cultured mouse neurons correlates with declining electrophysiological status: a fluorescence scale of membrane integrity. J Neurosci Methods 31:43–46
Manev H, Favaron M, Guidotti A, Costa E (1989) Delayed increase of Ca2+ influx elicited by glutamate: role in neuronal death. Mol Pharmacol 36:106–112
Marcoux FW, Probert AW Jr, Weber ML (1990) Hypoxic neuronal injury in tissue culture is associated with delayed calcium accumulation. Stroke 21:III71–III74
Merida I, Avila-Flores A, Merino E (2008) Diacylglycerol kinases: at the hub of cell signalling. Biochem J 409:1–18
Miller RJ (1987) Multiple calcium channels and neuronal function. Science 235:46–52
Moto A, Hirashima Y, Endo S, Takaku A (1991) Changes in lipid metabolites and enzymes in rat brain due to ischemia and recirculation. Mol Chem Neuropathol 14:35–51
Newton AC (1995) Protein kinase C: structure, function, and regulation. J Biol Chem 270:28495–28498
Niizeki T, Takeishi Y, Arimoto T, Takahashi H, Shishido T, Koyama Y, Goto K, Walsh RA, Kubota I (2007) Cardiac-specific overexpression of diacylglycerol kinase ζ attenuates left ventricular remodeling and improves survival after myocardial infarction. Am J Physiol Heart Circ Physiol 292:H1105–H1112
Nishizuka Y (1995) Protein kinase C and lipid signaling for sustained cellular responses. FASEB J 9:484–496
Noraberg J, Kristensen BW, Zimmer J (1999) Markers for neuronal degeneration in organotypic slice cultures. Brain Res Brain Res Protoc 3:278–290
Ogura A, Tominaga K, Nakazawa M, Sugaya K, Inouye ST, Kudo Y (1994) Automated collection of conditioned medium from organotypically cultured brain slice. Neurosci Res 20:299–307
Orrenius S, Zhivotovsky B, Nicotera P (2003) Regulation of cell death: the calcium-apoptosis link. Natl Rev Mol Cell Biol 4:552–565
Saito N, Shirai Y (2002) Protein kinase Cγ (PKCγ): function of neuron specific isotype. J Biochem 132:683–687
Sakane F, Kanoh H (1997) Molecules in focus: diacylglycerol kinase. Int J Biochem Cell Biol 29:1139–1143
Sakane F, Imai S, Kai M, Yasuda S, Kanoh H (2007) Diacylglycerol kinases: why so many of them? Biochim Biophys Acta 1771:793–806
Sattler R, Charlton MP, Hafner M, Tymianski M (1998) Distinct influx pathways, not calcium load, determine neuronal vulnerability to calcium neurotoxicity. J Neurochem 71:2349–2364
Schmued LC, Hopkins KJ (2000) Fluoro-Jade B: a high affinity fluorescent marker for the localization of neuronal degeneration. Brain Res 874:123–130
Szydlowska K, Tymianski M (2010) Calcium, ischemia and excitotoxicity. Cell Calcium 47:122–129
Topham MK, Epand RM (2009) Mammalian diacylglycerol kinases: molecular interactions and biological functions of selected isoforms. Biochim Biophys Acta 1790:416–424
Topham MK, Bunting M, Zimmerman GA, McIntyre TM, Blackshear PJ, Prescott SM (1998) Protein kinase C regulates the nuclear localization of diacylglycerol kinase-ζ. Nature 394:697–700
Tymianski M, Charlton MP, Carlen PL, Tator CH (1993) Source specificity of early calcium neurotoxicity in cultured embryonic spinal neurons. J Neurosci 13:2085–2104
Wieloch T, Cardell M, Bingren H, Zivin J, Saitoh T (1991) Changes in the activity of protein kinase C and the differential subcellular redistribution of its isozymes in the rat striatum during and following transient forebrain ischemia. J Neurochem 56:1227–1235
Yamazaki Y, Jia Y, Hamaue N, Sumikawa K (2005) Nicotine-induced switch in the nicotinic cholinergic mechanisms of facilitation of long-term potentiation induction. Eur J Neurosci 22:845–860
Yamazaki Y, Jia Y, Niu R, Sumikawa K (2006) Nicotine exposure in vivo induces long-lasting enhancement of NMDA receptor-mediated currents in the hippocampus. Eur J Neurosci 23:1819–1828
Yamazaki Y, Hozumi Y, Kaneko K, Sugihara T, Fujii S, Goto K, Kato H (2007) Modulatory effects of oligodendrocytes on the conduction velocity of action potentials along axons in the alveus of the rat hippocampal CA1 region. Neuron Glia Biol 3:325–334
Yamazaki Y, Sugihara T, Goto J, Chida K, Fujiwara H, Kaneko K, Fujii S, Mikoshiba K (2011) Role of inositol 1, 4, 5-trisphosphate receptors in the postsynaptic expression of guinea pig hippocampal mossy fiber depotentiation. Brain Res 1387:19–28
Yang Y, Mufson EJ, Herrup K (2003) Neuronal cell death is preceded by cell cycle events at all stages of Alzheimer’s disease. J Neurosci 23:2557–2563
Yoshida S, Ikeda M, Busto R, Santiso M, Martinez E, Ginsberg MD (1986) Cerebral phosphoinositide, triacylglycerol, and energy metabolism in reversible ischemia: origin and fate of free fatty acids. J Neurochem 47:744–757
Yoshida T, Fukaya M, Uchigashima M, Miura E, Kamiya H, Kano M, Watanabe M (2006) Localization of diacylglycerol lipase-α around postsynaptic spine suggests close proximity between production site of an endocannabinoid, 2-arachidonoyl-glycerol, and presynaptic cannabinoid CB1 receptor. J Neurosci 26:4740–4751
Acknowledgments
We are thankful to Mr. Kenya Kaneko for his technical help in preparing hippocampal slices. This work was supported by Grants-in-Aid from The Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan (YY, YH, MO, KI, SF, KG).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, Y., Yamazaki, Y., Hozumi, Y. et al. NMDA receptor-mediated Ca2+ influx triggers nucleocytoplasmic translocation of diacylglycerol kinase ζ under oxygen–glucose deprivation conditions, an in vitro model of ischemia, in rat hippocampal slices. Histochem Cell Biol 137, 499–511 (2012). https://doi.org/10.1007/s00418-011-0907-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-011-0907-y