Abstract
Implantation of tissue-engineered heterotopic cartilage into joint cartilage defects might be an alternative approach to improve articular cartilage repair. Hence, the aim of this study was to characterize and compare the quality of tissue-engineered cartilage produced with heterotopic (auricular, nasoseptal and articular) chondrocytes seeded on polyglycolic acid (PGA) scaffolds in vitro and in vivo using the nude mice xenograft model. PGA scaffolds were seeded with porcine articular, auricular and nasoseptal chondrocytes using a dynamic culturing procedure. Constructs were pre-cultured 3 weeks in vitro before being implanted subcutaneously in nude mice for 1, 6 or 12 weeks, non-seeded scaffolds were implanted as controls. Heterotopic neo-cartilage quality was assessed using vitality assays, macroscopical and histological scoring systems. Neo-cartilage formation could be observed in vitro in all PGA associated heterotopic chondrocytes cultures and extracellular cartilage matrix (ECM) deposition increased in vivo. The 6 weeks in vivo incubation time point leads to more consistent results for all cartilage species, since at 12 weeks in vivo construct size reductions were higher compared with 6 weeks except for auricular chondrocytes PGA cultures. Some regressive histological changes could be observed in all constructs seeded with all chondrocytes subspecies such as cell-free ECM areas. Particularly, but not exclusively in nasoseptal chondrocytes PGA cultures, ossificated ECM areas appeared. Elastic fibers could not be detected within any neo-cartilage. The neo-cartilage quality did not significantly differ between articular and non-articular chondrocytes constructs. Whether tissue-engineered heterotopic neo-cartilage undergoes sufficient transformation, when implanted into joint cartilage defects requires further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular cartilage has only a limited capacity for intrinsic healing. Hence, cartilage tissue engineering raises the hope of finding approaches to treat articular cartilage lesions using in vitro produced autologous neo-cartilage. However, the availability of autologous articular chondrocytes for neo-cartilage production remains the limiting issue. The use of non-articular heterotopic chondrocytes might circumvent this restriction and present a cell source for articular cartilage defect repair (El Sayed et al. 2010). Recently, we found cell–cell compatibility of auricular and articular chondrocytes in co-culture systems and some adjustment in the ECM expression of both chondrocytes types in co-cultures (Kuhne et al. 2010). Getting sufficient cell numbers for tissue engineering requires autologous chondrocytes expansion in monolayer culture which goes along with their dedifferentiation (Benya and Shaffer 1982). Chondrocyte dedifferentiation during monolayer culture has been shown in a similar manner for all heterotopic chondrocytes (El Sayed et al. 2010). Three-dimensional (3D) cultures provide a possibility for redifferentiation of dedifferentiated chondrocytes and long-term chondrocyte cultures (Hauselmann et al. 1992; Schulze-Tanzil et al. 2002, 2004; Domm et al. 2002; Kurz et al. 2005). A variety of 3D culture models have been developed to improve cartilage tissue engineering in the past decades (Schulze-Tanzil 2009; Chung and Burdick 2008). Bioresorbable biomaterials are tools to provide 3D conditions and a transient stability of the tissue engineered constructs up to the point where sufficient neo-matrix is produced by the embedded autologous chondrocytes. PGA is a biodegradable biomaterial with well-characterized biocompatibility (Athanasiou et al. 1995; Gunatillake and Adhikari 2003). The elastic fleece character produced by woven or non woven PGA fiber configurations makes PGA a flexible and formable scaffold with a wide range of applications (Athanasiou et al. 1998). However, the degradation product of PGA, glycolic acid, can accumulate in the tissue and the resulting local shift of the tissue pH might have local inflammatory effects (Stoll et al. 2011). Dynamic culture conditions provide a higher exchange of the growth medium and biomaterial degradation products, a more homogenous cell distribution and mechanostimuli which can improve in vitro cartilage formation compared with static culturing (Schulz and Bader 2007). Hence, different dynamic culturing strategies have been used for cartilage tissue engineering (Schulz and Bader 2007; Kafienah et al. 2002; Chung and Burdick 2008). A more continuous nutrient exchange and probably a more similar oxygen and carbon dioxide pressure compared with the in vitro conditions can be provided by implantation of seeded scaffolds in vivo in the nude mice which, nevertheless, might differ from the intraarticular conditions. Thymic aplastic and hence, immunodeficient nude mice allow the implantation of xenogenic chondrocyte species and ectopic cartilage formation (Isogai et al. 2006; Kafienah et al. 2002; Endres et al. 2007). In the present study, porcine chondrocytes were used since they share several similarities with human chondrocytes (Schulze-Tanzil et al. 2009). It was performed to compare the chondrogenic potential of auricular and nasoseptal chondrocyte species with articular chondrocytes in 3D PGA cultures. Till date, only two studies have analyzed the behavior of porcine heterotopic chondrocytes, in this case, articular and auricular chondrocytes cultured in hyaluronic acid in an in vivo nude mice model for 6 and 12 weeks (Chung et al. 2008). In the other study, performed by Xu et al., fibrin polymers seeded with porcine auricular, articular or costal chondrocytes were implanted for 4, 8 and 12 weeks in nude mice (Xu et al. 2004). Further, only one other study exists which makes use of PGA scaffolds seeded with (human and bovine) nasoseptal and articular chondrocytes for characterization of the in vivo neo-cartilage formation in the nude mice model after 3 and 6 weeks (Kafienah et al. 2002). However, other potential cell sources for cartilage tissue engineering are chondrogenic differentiated mesenchymal stem cells (MSCs), periostal cells and programmable cells of monocytic origin (PCMO) (Nakahara et al. 1990; Pufe et al. 2008; Richter 2009; Zhang and Spector 2009) whereby the chondrogenic differentiation potential of MSCs and periostal cells is donor age-dependent (De Bari et al. 2001; Nakahara et al. 1990; Yoo et al. 1998). In vitro expansion of MSC and their subsequent chondrogenic differentiation process which remains sometimes unstable and incomplete (Pelttari et al. 2008) are more time consuming than the use of autologous chondrocytes.
Hence, the present study was undertaken to provide a detailed and comprehensive characterization of in vitro dynamically pre-cultured and in vivo tissue-engineered heterotopic neo-cartilage. We used three time points (1, 6 and 12 weeks observation time) for in vivo cultivation of the PGA scaffolds seeded with porcine articular, auricular and nasoseptal chondrocytes to assess cartilage-source-specific chondrogenic properties.
Materials and methods
Isolation and culturing of porcine chondrocytes
Porcine cartilage was harvested from the auricle, the cartilaginous nasal septum and the knee joint (articular cartilage from the femoral grove, condyles and patella were pooled) of pigs (3–6 months old hybrid pigs [n = 10]). The connective tissue and perichondrium of auricular and nasoseptal cartilage were carefully removed. Porcine cartilage samples were subsequently minced into 1 mm slices and enzymatically digested with 0.4% pronase (7 U/mg, Roche, Basel, Switzerland) diluted in Ham’s F-12/Dulbecco’s modified Eagle’s (DMEM) medium 1:1 (Biochrom AG, Berlin, Germany) for 1 h at 37°C and subsequently digested with 0.2% (w/v) collagenase (≥0.1 U/mg, SERVA Electrophoresis GmbH, Heidelberg, Germany) diluted in growth medium for 16 h at 37°C. Isolated chondrocytes were resuspended in growth medium (Ham’s F-12/DMEM 1:1 containing 10% fetal calf serum (FCS) [Biochrom AG], 25 μg/mL ascorbic acid [Sigma-Aldrich], 50 IU/mL streptomycin, 50 IU/mL penicillin, 0.5 μg/mL partricin, essential amino acids, 2 mM l-glutamine [all: Biochrom AG]) and seeded at 2.8 × 104 cells/cm2 in culture flasks.
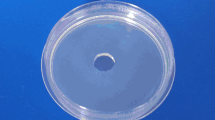
Dynamic 3D PGA cultures
Biodegradable non woven PGA meshes (Biofelt 65 mg/cc, Concordia Medical, USA) 10 × 10 × 3.5 mm were soaked in 5 mL porcine chondrocytes suspension in the growth medium (8 × 106 cells of the second or third monolayer passage) prepared from each of the three heterotopic chondrocyte sources. Dynamic cultures were performed by stirring the cell suspension in a bioreactor filter tube (TPP, Switzerland) under orbital shaking conditions with the floating PGA felt at 36 rpm in a rotatory shaker (digital tube roller Stuart SRT9D, Bibby Scientific, USA) at 37°C and 5% CO2. Growth medium was changed three times a week, every 48–72 h.
Assessment of cell vitality in PGA cultures
After washing with PBS, the 21-day-old scaffolds were incubated in fluorescein diacetate (FDA) (3 μg/mL dissolved in acetone [stock solution], Sigma-Aldrich and further diluted 1:1,000 in PBS [working solution]) for 15 min at 37°C, rinsed three times with PBS before being counterstained with propidium iodide (PI) solution (1 mg/mL dissolved in PBS [stock solution], Sigma-Aldrich further diluted 1:100 in PBS [working solution]) for 1 min in the dark at room temperature. The green or red fluorescence was visualized using fluorescence microscopy (Olympus Soft Imaging Solutions GmbH, Münster, Germany).
Nude mice xenograft model
Porcine articular, auricular and nasoseptal chondrocytes were cultured for 21 days on 1 cm diameter PGA meshes as described above. 6 mm diameter pieces of the chondrocyte-seeded PGA constructs were punched out and were implanted subcutaneously into the dorsal space of female 4- to 8-week-old athymic (nude) mice (Charles River, Sulzfeld, Germany). The mice received Rimadyl (4 mg/kg body weight, Pfizer, Karlsruhe, Germany) subcutaneously as premedication and they were subsequently anesthetized using isoflurane (Forene® 100%, Abbott, Wiesbaden, Germany). A skin incision of 1 cm was made under sterile conditions, a pocket beneath the incision was opened and a single construct was inserted. The incision was closed with 6-0 Prolene® (Ethicon, New Jersey, USA). After 24 h, the mice received Rimadyl (4 mg/kg body weight) again subcutaneously as analgesia. The animals were divided randomly into three different groups depending on the source of chondrocytes (articular, auricular and nasoseptal) implanted. Additionally, a fourth group of mice implanted with non-seeded PGA scaffold served as control. The cell-free scaffolds were soaked 24 h with growth medium before implantation. Animals were killed at 1, 6 or 12 weeks (n = 4 in each group and at each time point) after implantation of the construct. The explanted PGA constructs were macroscopically scored (Table 1) and then measured and documented photographically using a Canon EOS500D camera with a Canon EF-S60 mm macro objective (Canon, Krefeld, Germany). Subsequently, they were fixed for 15 min in 4% paraformaldehyde, dehydrated overnight in 30% sucrose solution before being embedded in Tissue-Tek® O.C.T. Compound medium (Sakura Finetek USA, Inc.). Cryosections were prepared, histologically stained and analyzed using a histological scoring system (Table 2).
Macroscopical score to assess neo-cartilage quality
A macroscopical scoring system was developed to assess the cartilage quality in vivo in the nude mice (Table 1). It entails the examination of color, the constitution of the PGA-construct, structural characteristics and maintenance of original size after 1, 6 and 12 weeks in vivo.
Histological analysis (hematoxylin eosin, alcian blue, von Kossa and resorcin-fuchsin stainings)
For all histological staining procedures cryo-sections (thickness 13 μm) were used. For hematoxylin eosin (HE) staining sections were stained for 4 min in Harris hematoxylin solution (Sigma-Aldrich), rinsed in water and counterstained for 4 min in eosin (Carl Roth GmbH, Karlsruhe, Germany).
For alcian blue (AB) staining, the sections were incubated for 3 min in 1% acetic acid and then stained 30 min in 1% AB (Carl Roth, Karlsruhe, Germany). Subsequently, they were rinsed in 3% acetic acid. Counterstaining of cell nuclei was performed using nuclear fast red aluminum sulfate solution (Carl Roth) for 5 min.
For resorcin-fuchsin staining the sections were stained in Weigert’s resorcin-fuchsin (Waldeck GmbH, Münster, Germany) solution for 10 min, differentiated in hydrochloric acid/ethanol for 1 min. The cell nuclei were counterstained using fast red aluminum sulfate solution (Carl Roth GmbH, Karlsruhe, Germany) for 10 min.
Using the von Kossa staining, the calcium deposition was illustrated with 2.5% silver nitrate (Carl Roth GmbH, Karlsruhe, Germany) for 30 min. The sections were reduced with sodium carbonate (Carl Roth GmbH, Karlsruhe, Germany) for 7 min. The cell nuclei were counterstained with fast red aluminum sulfate (Carl Roth GmbH, Karlsruhe, Germany) for 10 min.
Finally, all sections were rinsed with aqua dest. and subsequently dehydrated in an ascending alcohol series. Then, the sections were embedded with Entellan (Merck, Darmstadt, Germany). All slices were analyzed by light microscopy (Axiophot 40 microscope: Zeiss Jena, Germany). Photos of the sections were taken using an Olympus camera XC30 (Olympus Soft Imaging Solutions GmbH, Münster, Germany). For HE and AB sections a histological scoring system was established to assess the quality of neo-cartilage (Table 2) and for von Kossa to assess tissue ossification (Table 3).
Type II collagen immunolabeling
Cryo-sections of the tissue-engineered constructs were rinsed in Tris buffered saline (TBS: 0.05 M Tris, 0.015 M NaCl, pH 7.6) before incubated with 5 mg/ml pronase (7 U/mg, Roche, Basel, Switzerland) diluted in TBS for 5 min at 37°C. Sections were subsequently rinsed with TBS, blocked with protease-free donkey serum (5% diluted in TBS) for 30 min at room temperature (RT), rinsed and incubated with the polyclonal rabbit anti-type II collagen antibody (27.5 μg/mL, Acris Antibodies, Herford, Germany) in a humidifier chamber overnight at 4°C. Sections were subsequently washed with TBS before incubation with donkey-anti-rabbit-Alexa-Fluor®488 (10 mg/mL, Invitrogen) secondary antibody for 30 min at RT. Negative controls included omitting the primary antibody during the staining procedure. As a positive control served a decalcified subchondral femoral bone-articular cartilage tissue section derived from a pig knee. Cell nuclei were counterstained using 4′,6-diamidino-2-phenylindole (DAPI) (0.1 μg/mL, Roche). Labeled sections were rinsed several times with TBS, embedded with Fluoromount G (Southern Biotech, Biozol Diagnostica, Birmingham, USA) and examined using a fluorescence microscope (Axioskop 40, Carl Zeiss, Jena, Germany). Images were taken using a color view II (Olympus, Europa Holding, Hamburg, Germany).
Statistical analysis
All values were expressed as mean with standard deviation, except for Fig. 5e which shows the mean with SEM. Data were analyzed using unpaired Student’s t test (GraphPad Prism 5, GraphPad software inc., San Diego, USA). Statistical significance was set at a p value of ≤0.05.
Results
Cartilage formation in vitro: cell vitality and neo-cartilage histology
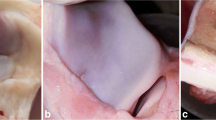
Chondrocytes adhered and spread well on the PGA scaffold. All heterotopic chondrocytes formed cell-ECM sails between the PGA fibers. A high number of vital chondrocytes, irrespective from which cartilage sources (articular, auricular or nasoseptal) they were derived from, could be observed within the PGA scaffolds during the 3 weeks in vitro culture period (Fig. 1a1–c1). Formation of an ECM-rich tissue within the scaffolds was already detectable in vitro (Fig. 1a2–c2): This ECM contained cartilage-specific sulfated proteoglycans as shown by AB staining whereby the ECM containing these proteoglycans formed focal nodules around groups of chondrocytes within the scaffolds (Fig. 1a3–c3, arrows). In these nodules, chondrocytes were embedded in lacunae and surrounded by a dense and homogenous ECM. However, the chondrocytes were arranged at random within the ECM whereby the neo-cartilage revealed no zonality. No major differences between the PGA-cultures of all heterotopic chondrocytes could be observed (Fig. 1a1–c3).
In vitro cartilage formation: chondrocyte vitality, histological structure and cartilage proteoglycan deposition. a 1 –c 1 3-week-old PGA scaffolds seeded dynamically with heterotopic chondrocytes (a articular, b auricular or c nasoseptal chondrocytes) were analyzed with FDA/PI live-death assay. Living cells were stained with FDA (green), dead cells (and PGA fibers) were counter-stained with PI (red). a 2 –c 2 Hematoxylin eosin (HE) staining of cryo-sections revealed cell and ECM distribution of the heterotopic chondrocytes within the PGA constructs. a 3 –c 3 : Cryo-sections of the PGA constructs were stained with alcian blue (AB) to indicate cartilage-specific sulfated proteoglycans within the ECM. It has to be recognized that the degraded PGA fibers stain usually non-specifically for most of the staining solutions. Black arrows cartilage nodules. Scale bars 100 μm
Macroscopical evaluation of cartilage formation in vivo
A macroscopical scoring system was developed (Table 1) to assess the cartilage-like properties of the constructs explanted from the subcutaneous pockets of the nude mice (Fig. 2). This macroscopical score comprised color, maintenance of original size, and other parameters detailed in Table 1. The construct size expressed by measuring its total area was also determined separately (Fig. 2e). A cartilage-like mostly white and translucent appearance was discernible in the articular and auricular chondrocytes PGA-associated constructs at 6 and 12 weeks (Fig. 2a2, a3, b2, b3). Nasoseptal chondrocytes constructs exhibited a varying coloration (yellowish, rose or white color) (Fig. 2c2, c3). Blood vessels were visible at the surface of nasoseptal chondrocytes at 6 weeks (Fig. 2c2) and 1-week-old auricular chondrocytes (Fig. 2b1) constructs. The non-seeded constructs had generally a brownish or rose color (Fig. 2d1, d2). At 12 weeks the non-seeded PGA scaffold was generally resorbed in the nude mice and not any longer detectable (Fig. 2d3). To assess size reduction of the constructs, the overall areas of all explanted constructs were measured. Most of them revealed a size reduction (Fig. 2e). Shrinkage was less pronounced in all constructs explanted after 1 week and in the constructs prepared from auricular chondrocytes after 6 weeks in vivo compared with those from articular and nasoseptal chondrocytes at 6 and 12 weeks. Non-seeded constructs showed a slight swelling after 1 week of in vivo incubation. So the constructs were significantly larger compared with the other constructs explanted after 1 week. However, after 6 weeks in vivo a severe size reduction of the non-seeded constructs could be detected which was significantly higher compared with the constructs seeded with articular or auricular chondrocytes explanted at the same investigation time point. The explant size reduction was also significantly higher in constructs seeded with nasoseptal chondrocytes compared with auricular chondrocytes at 6 weeks (Fig. 2e).
Macroscopical evaluation of in vivo cartilage formation. Neo-cartilage explants grown subcutaneously in the nude mice deriving from a articular; b auricular, c nasoseptal, chondrocytes seeded on PGA scaffolds or from PGA scaffolds which had not been seeded with chondrocytes (d non-seeded) are shown. Scaffolds remained implanted for either 1 (a 1 –d 1 ), 6 (a 2 –d 2 ) or 12 weeks (a 3 –d 3 ) in the nude mice. e The percentage of construct size reduction (the total areas of the constructs were measured) is displayed compared with the size in the beginning of the PGA culture. f Results of the macroscopical scoring are summarized for each time point. Non-seeded constructs were only detectable at 1 and 6 weeks but were resorbed at 12 weeks and hence no scoring results were available at 12 weeks, n = 4
The PGA scaffolds seeded with all heterotopic chondrocyte species exhibited significantly higher macroscopical scores at 1 and 6 weeks compared with the non-seeded PGA scaffolds (Fig. 2f) at each time point of explantation. The macroscopical scores of the PGA scaffold prepared from the investigated heterotopic chondrocytes sources differed only significantly between auricular and nasoseptal chondrocytes at 6 weeks, but not when heterotopic (nasoseptal and auricular) chondrocytes were compared with articular chondrocytes (Fig. 2f).
At 12 weeks the macroscopical scoring results of all chondrocyte species revealed a higher variation compared with 6 weeks. The macroscopical properties of nasoseptal chondrocytes constructs, summarized by the scoring results, were significantly inferior after 6 weeks compared with 1 week in vivo.
Histological evaluation of cartilage formation in vivo
The cartilage formation of the PGA constructs was clearly increased in vivo in the mice (Fig. 3) compared with in vitro results after 21 days (Fig. 1). The cellularity in the neo-cartilage in vivo decreased compared with the in vitro observations (Figs. 1a2–c3, 3a1–d3, HE-stainings not shown). The non-seeded scaffolds contained different immigrated mice-derived host cells and a few non-specific ECM deposits produced by immigrated subcutaneous fibroblasts (Fig. 3d1, d2). Groups of inflammatory cells could be detected still at 6 weeks in the non-seeded constructs but hardly in the chondrocytes seeded PGA constructs (Fig. 3d2). After 6 weeks in vivo, PGA fibers were nearly completely degraded.
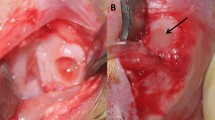
In vivo cartilage formation (Alcian Blue staining) and results of histological scoring. Histological pictures of cartilage explants produced with PGA scaffolds seeded with a articular, b auricular, c nasoseptal chondrocytes or d non-seeded were shown after subcutaneous implantation for 1 (a 1 –d 1 ), 6 (a 2 –d 2 ) and 12 weeks (a 3 –d 3 ) in the nude mice. The white double-head arrows indicate cell-free ECM areas. d 1 The black arrow hints at fibrin deposits as an early inflammatory host response. c 3 The asterisk marks regions of ossificated cartilage and the black double-head arrows indicate bone-marrow-like cavities containing blood-cells and mesenchymal-like tissue. e Results of histological scoring based on HE and alcian blue staining are summarized. Non-seeded constructs were only detectable at 1 and 6 weeks but were resorbed at 12 weeks and hence no scoring results were available at 12 weeks, n = 4. Scale bars 100 μm
After 1-week incubation in the nude mice, first areas of a proteoglycan-rich ECM were discernable (Fig. 3a1–c1), except for the non-seeded PGA scaffolds (Fig. 3d1). Cartilage formation substantially increased after 6 weeks (non-significant): in all cell-seeded constructs a dense ECM could be detected with the chondrocytes surrounded by lacunae (Fig. 3a2–c2). However, particularly at 12 weeks more and more regressive changes could already be observed histologically within the cell-seeded constructs: such as areas of cell-free ECM in articular and auricular chondrocyte cultures (Fig. 3b2, a3 and b3, white arrows). In nasoseptal chondrocyte cultures, ECM ossification was evident as well as the occurrence of bone-marrow-like holes (Fig. 3c3, black arrows). However, the histological analysis of the neo-cartilage formed by heterotopic chondrocyte PGA constructs revealed only non-significant differences between the investigated chondrocyte sources at 1 and 12 weeks investigation time points, but auricular chondrocytes containing PGA constructs at 6 weeks revealed in vivo significantly higher histological scores than nasoseptal or articular neo-cartilage constructs (Fig. 3e). To prove the presence of calcium deposits as a feature of ossification, von Kossa staining was performed which was positive in explants containing nasoseptal chondrocytes on PGA, but also some focal staining was evident in some constructs (Fig. 5a1–d2). Hypertrophic chondrocytes and ossificated ECM areas could be found more often in nasoseptal chondrocyte constructs at 12 weeks compared with the other samples (non-significant, Fig. 5a1–d2). It was significantly higher in 12-week-old nasoseptal constructs compared with 1-week-old nasoseptal neo-cartilage (Fig. 5e). A deeper look at the 12-week-old explants with nasoseptal chondrocytes revealed several features of the onset of enchondral ossification with hypertrophic chondrocytes with calcified ECM, bony spicules containing osteocytes which were surrounded by osseous lacunae as well as bone-marrow cavities (Fig. 5c2, black arrows) with invading blood vessels (Fig. 5c2, white arrow) and bone-marrow-like mesenchymal tissue could be also detected.
No elastic fibers could be detected by resorcin-fuchsin staining of the in vitro cultured heterotopic chondrocytes (not shown). After in vivo subcutaneous implantation some elastic fibers were detectable, but only at the outer margin of some constructs and not within the neo-cartilage indicating that the auricular neo-cartilage did not contain mature elastic fibers (not shown).
Type II collagen immunolabeling
All heterotopic chondrocyte PGA constructs revealed an intensive type II collagen immunolabeling after 6 weeks in vivo which was nearly comparable with the type II collagen staining in porcine articular cartilage in situ (Fig. 4a–f).
Type II collagen immunolabelling after 6 weeks in vivo incubation. Immunolabeling of the cartilage-specific matrix protein type II collagen was performed in constructs either seeded with heterotopic chondrocytes or cell-free explanted after 6 weeks in vivo to assess cartilage quality (a–d). A paraffin section of a porcine subchondral bone-articular cartilage segment, immunolabeled for type II collagen in a similar manner served as a positive control (e). f Isotype control. Scale bars 100 μm
Discussion
Successful in vitro cartilage formation could be achieved using cultured heterotopic chondrocytes, but it can be improved in vivo after ectopic subcutaneous implantation of chondrocyte cultures in nude mice. A more continuous nutrient supply is provided in the nude mice compared with the in vitro conditions. Athymic nude mice possess a reduced immune system and hence allow the implantation of xenogenic cell sources such as porcine chondrocytes which were used in the present study. The nude mice xenograft model has been used to study cartilage formation of chondrocytes derived from different animal species or human, diverse biomaterials and culture systems by several groups (Chung et al. 2008; El Sayed et al. 2010). So the expression profile of heterotopic auricular, nasoseptal and articular chondrocytes was investigated in lapine, bovine and human chondrocytes using different 3D culture systems (Isogai et al. 2006). Only one study compared the in vivo chondrogenesis by human and bovine articular and nasoseptal chondrocytes cultured on PGA scaffolds (Kafienah et al. 2002). In the present study, the time course of in vitro and in vivo cartilage ECM synthesis by porcine heterotopic (articular, auricular and nasoseptal) chondrocytes seeded on PGA was monitored at 1, 6 and 12 weeks. A dynamic chondrocyte-seeding technique was chosen for PGA scaffold culture, which leads to a mostly homogenous cell distribution within the construct. For this reason, other additives which are usually applied to achieve a more homogenous cell distribution such as fibrin glue could be omitted. Fibrin might influence in vitro and in vivo chondrogenesis (Schmal et al. 2008). A construct size reduction could be generally observed after 6 weeks in vivo, except for the explants containing auricular chondrocytes. The reason for the construct shrinkage remains unclear: it might altogether be mostly influenced by the PGA fibers degradation, reduction of water content within the ECM, contraction of ECM fibers such as collagen or direct ECM degradation by mice host cells such as macrophages and foreign body cells or during enchondral ossification (Fig. 5). Not surprisingly, the non-seeded scaffolds, which contained sparse extracellular matrix revealed the most rapid decrease in construct size after implantation. This fact suggests that an in vitro preformed cartilaginous ECM produced by chondrocytes seeded onto the scaffolds which covers the fibers might somehow protect them from degradation by macrophages and other host tissue-derived cells. This observation is in agreement with the study by Kusahara et al. who used another biomaterial (Kusuhara et al. 2009).
In vivo von Kossa staining at 6 and 12 weeks. To indicate the presence of ECM ossification within the cartilage constructs, von Kossa staining of 6 (a 1 –d 1 ) and 12-week-old (a 2 –d 2 ) constructs explanted from mice is shown. Cryo-sections of PGA scaffolds seeded with a articular, b auricular, c nasoseptal chondrocytes or d non-seeded scaffolds are compared after subcutaneous implantation in the nude mice. The white arrow in c 2 hints at tissue, which invades into a bone marrow cavity-like hole (black double-head arrow) in the ossificated ECM. e Results of von Kossa scoring are summarized, n = 4. Scale bars 100 μm
Accordingly, the non-seeded PGA scaffolds contained many more inflammatory cells compared with the chondrocyte-seeded constructs. It indicates first, that the ECM produced by chondrocytes which covers the fibers might by less immunogen compared with the naked PGA fibers. Second and more importantly, the PGA fiber degradation products might cause a local pH shift which cannot be buffered in the non-seeded constructs by some ECM coating the fibers and which hence might induce a sterile inflammation. Isogai et al., used a similar model with bovine chondrocytes on poly(l-lactide-ecaprolactone)(P[LA/CL]) and found no size reduction during the 20-week-observation period (Isogai et al. 2006). Only the non-seeded constructs showed some size reduction similar to the present study. The more rapid degradation course of PGA in comparison to (P[LA/CL]) (Freed et al. 1993; Honda et al. 2000) might be probably responsible for these differences in addition to chondrocyte species differences, since Isogai et al. (2006) used bovine and not porcine chondrocytes. A nearly complete PGA fiber degradation could be observed after 6 weeks in vivo. Hence, the neomatrix formation by implanted bovine chondrocytes might be almost synchronized with the slow (P[LA/CL]) degradation rate in the study of Isogai et al. (2006). On the contrary, the PGA fibers might degrade more rapid than the porcine chondrocytes can produce a stabilizing neomatrix. This fact could explain the shrinkage of the tissue-engineered constructs in vivo. Recently, we could confirm the PGA degradation time of 6–12 weeks in vivo in another tissue, the healing rabbit tendon (Stoll et al. 2011).
Regressive changes of the cartilage constructs could be observed after 6 weeks in vivo: the ECM becomes obviously so dense that the nutrition per diffusion in the subcutaneous milieu in vivo might be insufficient leading to increased hypoxia and subsequent cell death. Accordingly, cell-free ECM areas became more and more visible. Despite this, some constructs were covered by blood vessels adhering to their surface; no blood vessels were discernible within the construct apart from the constructs seeded with nasoseptal chondrocytes which underwent more or less complete enchondral ossification. Within these constructs, blood vessels and also a bone-marrow-like mesenchymal tissue were detectable. Blood vessel endothelial cells and mesenchymal cells might probably be host derived; however, it was not further investigated in this study. Cartilage enchondral ossification and bone-like tissue formation could be observed in these samples starting at 6 weeks and proceeding at 12 weeks. Calcium deposits were predominantly, but not exclusively observed using nasoseptal chondrocytes and hence, might be an intrinsic characteristic of this particular heterotopic chondrocytes source. One might speculate about the factors contributing to the osteogenesis by nasoseptal chondrocytes such as the production of a very dense ECM leading to hypoxia in the center of the implant, a high sensitivity of nasoseptal chondrocytes to hypoxia activating hypoxia-dependent transcription factors and Vascular Endothelial Growth Factor or last but not least a higher content of stem cells capable for osteogenic differentiation compared with the other chondrocyte sources. Kusuhara et al. reported ossification for bovine costal chondrocytes ECM, but they did not find this feature in bovine nasoseptal chondrocyte-seeded biodegradable polymer constructs after explantation from nude mice (Kusuhara et al. 2009). The question arises whether ossification is confined to porcine nasoseptal chondrocytes and influenced by the host, the mice. Hypertrophy and ECM ossification of premature nasoseptal chondrocytes have also been reported for rat chondrocytes in vitro by others (Kergosien et al. 1998; Loty et al. 2000). Elastic fibers are a typical feature of elastic auricular cartilage, for this reason not only neo-cartilage produced with porcine auricular but also nasoseptal and articular chondrocytes were further assessed for elastic fibers synthesis using resorcin-fuchsin staining. The lack of elastic fibers in all constructs might be caused by the absence of sufficient mechanostimuli in the mice subcutaneous mileu. This finding is in agreement with the study of Naumann et al. who did not detect elastin protein expression in 3-week-old macroaggregate cultures using human nasoseptal and auricular chondrocytes (Naumann et al. 2004). In contrast, Kusuhara et al. could observe elastic fibers in bovine auricular, but not in articular, nasoseptal or costal chondrocytes constructs after 10 or 40 days in the nude mice (Kusuhara et al. 2009). At gene expression level, elastin could be demonstrated in diverse culture systems of auricular chondrocytes and to a lesser degree also in articular chondrocytes (Malicev et al. 2009; Kuhne et al. 2010). On the other side, the full synthesis of elastic fibers, which consist of elastin and microfibrils, might require more time and the time requirement might be species-dependent. However, our own experience with healing tendon tissue revealed a rapid neo-formation of elastic fibers (6 weeks) (Stoll et al. 2011). It could be possible that oxytalan fibers, which represent a kind of immature elastic fibers consisting of microfibrils, without elastin, are present in auricular neo-cartilage. Oxytalan fibers are more difficult to detect. In some tissues, these fibers appearing before mature elastic fibers can be recognized (Bradamante and Svajger 1977).
A pronounced type II collagen and proteoglycan expression could be detected in all PGA-constructs seeded with chondrocytes. However, the characteristic zonality naturally observed in articular cartilage in vivo was completely lacking in neo-cartilage, probably since the impulse from the subchondral bone and adequate mechanical stimuli are absent in the nude mice model. In this study, biomechanical analyses of the PGA-associated neo-cartilage were not performed which are also essential to assess the functional properties of heterotopic cartilage.
In conclusion, we demonstrated cartilage formation with all studied porcine heterotopic cartilage sources and we developed and used a detailed macroscopical and histological scoring system to assess cartilage quality in vitro and in vivo in the nude mice model. The 6 weeks in vivo incubation period was obviously the most illuminative investigation time point for all studied cartilage subspecies since lesser macroscopical construct size reduction in articular and auricular chondrocyte-seeded explants and fewer regressive histological changes compared with 12 weeks were evident. Furthermore, slightly more convenient histological scoring results and lesser inter-sample variation of the microscopical and macroscopical scoring results for each cartilage species compared with 12 weeks and significant histological differences between some of the investigated heterotopic chondrocytes species could be recognized at 6 weeks.
Only a few cell-specific characteristics of heterotopic chondrocytes in the PGA cultures in vivo, e.g., ossification in nasoseptal chondrocytes cultures could be detected. Heterotopic chondrocytes might lose other source-specific features: since elastic fiber formation by auricular chondrocyte cultures was lacking. Elastic fibers are normally expected in auricular cartilage. Neo-cartilage produced by porcine heterotopic nasoseptal and auricular chondrocytes was not inferior compared with that synthesized by articular chondrocytes in PGA-scaffolds suggesting that tissue-engineered cartilage using heterotopic chondrocytes should be further analyzed, e.g., for biomechanical quality as a possible interesting source for articular cartilage repair.
References
Athanasiou KA, Niederauer GG, Agrawal CM, Landsman AS (1995) Applications of biodegradable lactides and glycolides in podiatry. Clin Podiatr Med Surg 12(3):475–495
Athanasiou KA, Agrawal CM, Barber FA, Burkhart SS (1998) Orthopaedic applications for PLA-PGA biodegradable polymers. Arthroscopy 14(7):726–737
Benya PD, Shaffer JD (1982) Dedifferentiated chondrocytes reexpress the differentiated collagen phenotype when cultured in agarose gels. Cell 30(1):215–224
Bradamante Z, Svajger A (1977) Pre-elastic (oxytalan) fibres in the developing elastic cartilage of the external ear of the rat. J Anat 123(Pt 3):735–743
Chung C, Burdick JA (2008) Engineering cartilage tissue. Adv Drug Deliv Rev 60(2):243–262
Chung C, Erickson IE, Mauck RL, Burdick JA (2008) Differential behavior of auricular and articular chondrocytes in hyaluronic acid hydrogels. Tissue Eng Part A 14(7):1121–1131
De Bari C, Dell’Accio F, Luyten FP (2001) Human periosteum-derived cells maintain phenotypic stability and chondrogenic potential throughout expansion regardless of donor age. Arthritis Rheum 44(1):85–95
Domm C, Schunke M, Christesen K, Kurz B (2002) Redifferentiation of dedifferentiated bovine articular chondrocytes in alginate culture under low oxygen tension. Osteoarthritis Cartilage 10(1):13–22
El Sayed KE, Haisch A, John T, Marzahn U, Lohan A, Muller RD, Kohl B, Ertel W, Stoelzel K, Schulze-Tanzil G (2010) Heterotopic autologous chondrocyte transplantation—a realistic approach to support articular cartilage repair? Tissue Eng Part B Rev 16(6):603–616
Endres M, Neumann K, Schroder SE, Vetterlein S, Morawietz L, Ringe J, Sittinger M, Kaps C (2007) Human polymer-based cartilage grafts for the regeneration of articular cartilage defects. Tissue Cell 39(5):293–301
Freed LE, Marquis JC, Nohria A, Emmanual J, Mikos AG, Langer R (1993) Neocartilage formation in vitro and in vivo using cells cultured on synthetic biodegradable polymers. J Biomed Mater Res 27(1):11–23
Gunatillake PA, Adhikari R (2003) Biodegradable synthetic polymers for tissue engineering. Eur Cell Mater 5:1–16 discussion 16
Hauselmann HJ, Aydelotte MB, Schumacher BL, Kuettner KE, Gitelis SH, Thonar EJ (1992) Synthesis and turnover of proteoglycans by human and bovine adult articular chondrocytes cultured in alginate beads. Matrix 12(2):116–129
Honda M, Yada T, Ueda M, Kimata K (2000) Cartilage formation by cultured chondrocytes in a new scaffold made of poly(l-lactide-epsilon-caprolactone) sponge. J Oral Maxillofac Surg 58(7):767–775
Isogai N, Kusuhara H, Ikada Y, Ohtani H, Jacquet R, Hillyer J, Lowder E, Landis WJ (2006) Comparison of different chondrocytes for use in tissue engineering of cartilage model structures. Tissue Eng Part A 12(4):691–703
Kafienah W, Jakob M, Demarteau O, Frazer A, Barker MD, Martin I, Hollander AP (2002) Three-dimensional tissue engineering of hyaline cartilage: comparison of adult nasal and articular chondrocytes. Tissue Eng Part A 8(5):817–826
Kergosien N, Sautier J, Forest N (1998) Gene and protein expression during differentiation and matrix mineralization in a chondrocyte cell culture system. Calcif Tissue Int 62(2):114–121
Kuhne M, John T, El-Sayed K, Marzahn U, Aue A, Kohl B, Stoelzel K, Ertel W, Blottner D, Haisch A, Schulze-Tanzil G (2010) Characterization of auricular chondrocytes and auricular/articular chondrocyte co-cultures in terms of an application in articular cartilage repair. Int J Mol Med 25(5):701–708
Kurz B, Lemke AK, Fay J, Pufe T, Grodzinsky AJ, Schunke M (2005) Pathomechanisms of cartilage destruction by mechanical injury. Ann Anat 187(5–6):473–485
Kusuhara H, Isogai N, Enjo M, Otani H, Ikada Y, Jacquet R, Lowder E, Landis WJ (2009) Tissue engineering a model for the human ear: assessment of size, shape, morphology, and gene expression following seeding of different chondrocytes. Wound Repair Regen 17(1):136–146
Loty S, Foll C, Forest N, Sautier JM (2000) Association of enhanced expression of gap junctions with in vitro chondrogenic differentiation of rat nasal septal cartilage-released cells following their dedifferentiation and redifferentiation. Arch Oral Biol 45(10):843–856
Malicev E, Kregar-Velikonja N, Barlic A, Alibegovic A, Drobnic M (2009) Comparison of articular and auricular cartilage as a cell source for the autologous chondrocyte implantation. J Orthop Res 27(7):943–948
Nakahara H, Bruder SP, Haynesworth SE, Holecek JJ, Baber MA, Goldberg VM, Caplan AI (1990) Bone and cartilage formation in diffusion chambers by subcultured cells derived from the periosteum. Bone 11(3):181–188
Naumann A, Dennis JE, Aigner J, Coticchia J, Arnold J, Berghaus A, Kastenbauer ER, Caplan AI (2004) Tissue engineering of autologous cartilage grafts in three-dimensional in vitro macroaggregate culture system. Tissue Eng Part A 10(11–12):1695–1706
Pelttari K, Steck E, Richter W (2008) The use of mesenchymal stem cells for chondrogenesis. Injury 39(Suppl 1):S58–S65
Pufe T, Petersen W, Fandrich F, Varoga D, Wruck CJ, Mentlein R, Helfenstein A, Hoseas D, Dressel S, Tillmann B, Ruhnke M (2008) Programmable cells of monocytic origin (PCMO): a source of peripheral blood stem cells that generate collagen type II-producing chondrocytes. J Orthop Res 26(3):304–313
Richter W (2009) Mesenchymal stem cells and cartilage in situ regeneration. J Intern Med 266(4):390–405
Schmal H, Mehlhorn AT, Kurze C, Zwingmann J, Niemeyer P, Finkenzeller G, Dauner M, Sudkamp NP, Kostler W (2008) In vitro study on the influence of fibrin in cartilage constructs based on PGA fleece materials. Orthopade 37(5):424–434
Schulz RM, Bader A (2007) Cartilage tissue engineering and bioreactor systems for the cultivation and stimulation of chondrocytes. Eur Biophys J 36(4–5):539–568
Schulze-Tanzil G (2009) Activation and dedifferentiation of chondrocytes: implications in cartilage injury and repair. Ann Anat 191(4):325–338
Schulze-Tanzil G, de Souza P, Villegas Castrejon H, John T, Merker HJ, Scheid A, Shakibaei M (2002) Redifferentiation of dedifferentiated human chondrocytes in high-density cultures. Cell Tissue Res 308(3):371–379
Schulze-Tanzil G, Mobasheri A, de Souza P, John T, Shakibaei M (2004) Loss of chondrogenic potential in dedifferentiated chondrocytes correlates with deficient Shc-Erk interaction and apoptosis. Osteoarthritis Cartilage 12(6):448–458
Schulze-Tanzil G, Muller RD, Kohl B, Schneider N, Ertel W, Ipaktchi K, Hunigen H, Gemeinhardt O, Stark R, John T (2009) Differing in vitro biology of equine, ovine, porcine and human articular chondrocytes derived from the knee joint: an immunomorphological study. Histochem Cell Biol 131(2):219–229
Stoll C, John T, Conrad C, Lohan A, Hondke S, Ertel W, Kaps C, Endres M, Sittinger M, Ringe J, Schulze-Tanzil G (2011) Healing parameters in a rabbit partial tendon defect following tenocyte/biomaterial implantation. Biomaterials (in press)
Xu JW, Zaporojan V, Peretti GM, Roses RE, Morse KB, Roy AK, Mesa JM, Randolph MA, Bonassar LJ, Yaremchuk MJ (2004) Injectable tissue-engineered cartilage with different chondrocyte sources. Plast Reconstr Surg 113(5):1361–1371
Yoo JU, Barthel TS, Nishimura K, Solchaga L, Caplan AI, Goldberg VM, Johnstone B (1998) The chondrogenic potential of human bone-marrow-derived mesenchymal progenitor cells. J Bone Joint Surg Am 80(12):1745–1757
Zhang L, Spector M (2009) Comparison of three types of chondrocytes in collagen scaffolds for cartilage tissue engineering. Biomed Mater 4(4):045012
Acknowledgments
We thank Dr. Katharina Stoelzel for her support. The authors also thank Ms. Hannah Gough for proof reading of the manuscript. This study was supported by grants from Bayer Innovation GmbH and the Sonnenfeld Foundation, Berlin.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. Lohan and U. Marzahn contributed equally to the manuscript.
G. Schulze-Tanzil and T. John: joined senior authorship.
Rights and permissions
About this article
Cite this article
Lohan, A., Marzahn, U., El Sayed, K. et al. In vitro and in vivo neo-cartilage formation by heterotopic chondrocytes seeded on PGA scaffolds. Histochem Cell Biol 136, 57–69 (2011). https://doi.org/10.1007/s00418-011-0822-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-011-0822-2