Abstract
Di-(2-ethylhexyl)-phthalate (DEHP), the plasticizer employed in the fabrication of polyvinyl chloride, is known to be released by many medical devices, namely endotracheal tubes currently utilised for pulmonary ventilation of pre-term newborns. When experimentally administered, especially to rodents, the phthalate reportedly causes alterations to several tissues, immature animals being even more responsive targets than adult ones. In the present research, female rats were fed with DEHP in the last week of pregnancy and after delivery, and lung of their pups was morphologically and immunohistochemically analysed. We detected significant alveolar simplification (larger but fewer alveoli with decreased septation), with consequent sensible reduction of gas-exchange surface, at several stages of postnatal development, in distal lung parenchyma of DEHP-treated rats. Moreover, the quantification of PCNA-expressing cells demonstrates that in treated pups the proliferation rates of epithelial and mesenchymal cells progressively increased during the first two postnatal weeks, at difference with controls animals, where the highest proliferation levels were reached at postnatal day 7. The obtained results strongly support the hypothesis that DEHP profoundly affects the alveolarization process in mammalian lung.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Humans are exposed to di-(2-ethylhexyl)-phthalate (DEHP), a plasticizer released by polyvinylchloride (PVC), which is able to cross the placental barrier (Singh et al. 1972; Tomita et al. 1988) and to act via breast feeding (Cimini et al. 1994; Stefanini et al. 1995). After absorption, DEHP undergoes conversion into 2-ethylhexanol and mono-(2-ethylhexyl)-phthalate (MEHP), further processed through glucuronidation (Tickner et al. 2001). In rats, DEHP administration (3–14 days, 1–2.5 g/Kg/day) causes peroxisomal proliferation and increased activities of several enzymes both in liver and in kidney, and suckling animals appear especially sensitive to lethal and growth retardation effects (Osumi and Hashimoto 1978; Lake et al. 1984; Dostal et al. 1987; Sharma et al. 1989; Reubsaet et al. 1990; Cimini et al. 1994; Stefanini et al. 1995). In adult rats, moreover, respiratory distress and dose-dependent lethality occur after a single intravenous injection of 200–300 mg/Kg Tween-solubilised DEHP (Schulz et al. 1975), while a 4-week-long aerosol treatment (estimated dose 230 mg/Kg/day) causes relative lung weight increase, accompanied by foam-cell proliferation and alveolar septa thickening (Klimisch et al. 1992). DEHP-induced release of lysosomal enzymes from cultured alveolar macrophages, as well as constriction and oedema of pulmonary vessels in isolated perfused rat heart–lung preparations, has also been reported (Bally et al. 1980; Shertzer et al. 1982; Labow et al. 1990).
Human population was presumed not at risk of acute airway effects from environmental, non-occupational levels of DEHP or MEHP (Larsen et al. 2004, 2007) and urinary MEHP concentration was found not adversely associated with pulmonary function parameters (Hoppin et al. 2004). However, long-term damages to patients chronically submitted to blood transfusions, hemodialysis or oral/nasal feeding by means of PVC medical devices were not ruled out (Jaeger and Rubin 1972; Lewis et al. 1978; Khaliq et al. 1992). In pre-term newborns, whose glucuronidation pathway is immature (de Wildt et al. 1999), critical MEHP concentrations are presumably reached (see Latini 2000). MEHP urinary concentration was several fold over the general population value in premature infants submitted to intensive care (Calafat et al. 2004) and, moreover, in endotracheally intubated newborns was significantly higher than in those receiving nasal continuous positive airway pressure (Green et al. 2005). Finally, a correlation between endotracheal intubation with PVC tubes and incidence of chronic lung diseases has long been established (Stern et al. 1970; Roth et al. 1988; Poets and Sens 1996; Kamper 1999; Latini and Avery 1999).
In a previous work (Magliozzi et al. 2003), we orally administered DEHP to female rats during pregnancy and breast feeding and examined 2-day-old pup lungs, i.e. at a maturation stage closely comparable to that found in 26–36-week-old pre-term babies (Burri 1991).
In the present study, qualitative and quantitative observations were extended to the whole period of lung alveolarization and the proliferation rate of different cell populations in lung parenchyma was evaluated by means of immunolocalization of the proliferating cell nuclear antigen (PCNA). In order to identify the cell types undergoing active proliferation, catalase, a highly specific marker for type II pneumocytes (Farioli-Vecchioli et al. 2001), and α-smooth muscle actin (α-SMA), transiently expressed by interstitial myofibroblasts during septal formation (Yamada et al. 2005), were immunodetected.
Materials and methods
Animals and treatment
Albino Wistar rats (Charles River, Italy) were kept at 20–22°C, with a dark/light cycle of 12/12 h. Females were placed with males overnight and examined in the following morning for presence of sperm in the vaginal smear. All pregnant rats were fed ad libitum with standard diet till the 15th day of pregnancy; in the week preceding delivery, as well as during the breast feeding, ten of them received food containing 1% (w/w) DEHP (Sigma-Aldrich, Milan, Italy).
The food intake was measured at the end of treatment and only animals which had assumed at least 1 g/kg/day were utilised. At 2, 7 and 14 days after delivery, three pups from each one of five treated and five untreated females were anaesthetised with Farmotal (100 mg/Kg) (Amersham Pharmacia Biotech Italia, Cologno Monzese, Milan, Italy) and endotracheally instilled with 50–80 μl of Bouin’s solution. After trachea ligation, lungs were removed and immersed in the same solutions; few minutes later, they were cut into fragments, which were further fixed for 2–4 h, dehydrated and embedded in paraffin.
The fixative, its amount for each developmental stage, as well as paraffin embedding and immunohistochemistry by ABC method were chosen on the basis of preliminary experiments, in which immunofluorescence results had not been exhaustive, especially due to the relatively poor tissue preservation found in cryostatic specimens.
After lung resection, liver was excised and the relative liver weight (g/100 g body weight) was calculated. All animal work was conducted according to the European Communities Council Directive of 24 November 1986 (86/609/EEC) and the Italian Health Ministry guidelines.
Morphology of respiratory spaces
In the present paper a unit of distal lung parenchyma comprehending a canalicular portion and its terminal expansions (saccules or alveoles, depending on the stage) is named respiratory space. Three randomly chosen specimens from each animal were serially sectioned 7-μm-thick. For every single specimen only two sections, situated at a reciprocal distance of at least 200 μm, were utilised for quantitative evaluations; this distance in fact had been previously determined as sufficient to avoid measuring the same respiratory space twice. According to these schedules, for each developmental stage 90 test and 90 control sections were examined as follows: two randomly chosen non-overlapping fields for each section were photographed and digitised images were analysed by a Zeiss KS-300-SW image analyser. Profiles corresponding to arteries, veins and bronchioles were manually traced and their area was subtracted from the total area of the field; the remaining area, corresponding to distal parenchyma, was called “reference area”.
For all the profiles of respiratory spaces, the following parameters were determined:
-
mean area and perimeter,
-
mean circularity shape factor (Fcircle = 4πA/P 2, where A = profile area and P = profile perimeter), which allows to evaluate the irregularity of structures,
-
number per mm2 of reference area,
-
total perimeter per mm2 of reference area.
Values obtained from individual fields were utilised for calculating the mean values, which were submitted to variance analysis (ANOVA).
Immunohistochemistry
Freshly deparaffinised sections were treated with 0.3% H2O2 in methanol for 30 min at RT to inactivate endogenous peroxidases; after rehydration, they were transferred to PBS containing 0.2% Triton X-100 and 5% non-fat dry milk for 1 h at RT, and then incubated for 24 h at 4°C, in the primary antibodies diluted in PBS added with 0.1% Triton X-100 and 2.5% non-fat dry milk.
Dilutions were as follows: mouse monoclonal anti-rat PCNA (Dako, Milan, Italy) 1:200; mouse monoclonal anti α-SMA (Sigma Chemical Co., St. Louis, USA) 1:500; rabbit polyclonal anti-beef liver catalase (Rockland, Gilbertsville, USA) 1:1,000.
For the revelation of immunocomplexes through the conventional ABC method, sections were sequentially incubated in
-
1.
1:200 biotinylated goat anti-rabbit or rabbit anti-mouse IgG, for 1 h at RT,
-
2.
avidin-biotin-horseradish peroxidase complex, for 1 h at RT,
-
3.
0.05% 3,3′-diaminobenzidine (DAB) in PBS containing 0.01% H2O2 for 2-5 min at RT.
In the amplified ABC procedure the step 2 was followed by
-
incubation in biotinylated tyramine, 1:100 diluted in PBS containing 0.01% H2O2 for 10 min at RT,
-
avidin-biotin-horseradish peroxidase complex, for 30 min at RT.
Microwave treatment was carried out incubating freshly rehydrated sections with citrate buffer pH 6 (10 min at RT, 8 min in microwave oven at 750 W and 30 min at RT).
For negative control, the primary antibody was omitted or substituted with preimmune serum.
Couples of adjacent sections were utilised for the identification of cells co-expressing PCNA and α-SMA or PCNA and catalase.
Unstained and haematoxylin counterstained sections were examined in a Zeiss Axioskop2. Representative images were electronically captured; contrast and brightness were adjusted by Adobe Photoshop 6.0.
Quantitative analysis of proliferation rate
The analysis was carried out in lung sections submitted to standard ABC immunocytochemistry and haematoxylin counterstaining. For each developmental age six sections obtained from three normal rats and the same numbers from treated animals were observed at 40× magnification. In two microscopic fields, randomly chosen inside each section, the PCNA-positive and PCNA-negative nuclei were counted with the aid of a grid located in the eyepiece of the microscope; for each field an actual area of 0,096 mm2 was so examined. The nuclei in the distal parenchyma were counted separately from those belonging to airways and large vessels. In the distal parenchyma, nuclei of cells directly lining the respiratory spaces (presumed type II pneumocytes) were counted separately from those belonging to cells situated inside the intersaccular walls (presumed mesenchymal cells). Values were expressed as the mean ± SD. Intergroup differences were assessed by analysis of variance (ANOVA).
Chemicals
DEHP was from Sigma-Aldrich (Milan, Italy); Farmotal was from Amersham Pharmacia Biotech Italia (Cologno Monzese, Milan, Italy); mouse monoclonal anti-rat PCNA was from Dako (Milan, Italy); mouse monoclonal anti α-SMA and DAB were from Sigma Chemical Co. (St. Louis, USA); rabbit polyclonal anti-beef liver catalase was from Rockland (Gilbertsville, USA).
Results
At all the examined stages, the body weight of treated animals was significantly lower with respect to age-matched controls, the higher decrease (50%) being observed at postnatal day 14. The relative liver weight of treated animals was significantly higher (P < 0.01) over the corresponding controls at every examined stage (7.04 vs. 5.09 at 2 days; 4.17 vs. 3.68 at 7 days and 3.12 vs. 2.44 at 14 days). These values, besides confirming the presence of DEHP in neonatal and suckling rats, are in agreement with those previously reported for adult and neonatal rodents treated with phthalates (Osumi and Hashimoto 1978; Lake et al. 1984; Dostal et al. 1987; Reubsaet et al. 1990; Cimini et al. 1994).
Morphology of distal lung parenchyma
In the lung of 2-day-old normal pups, the transitory air spaces, separated by relatively thick primary septa, typically consisted of smooth-walled channels and saccules, delimited by small ridges. At 7 days the primary septa were sensibly thinner and some small ridges had elongated to form secondary septa; at 14 days, secondary saccules were very numerous and some true alveoli could be recognised (Fig. 1a–c). At all the examined stages, the respiratory spaces of treated pups appeared less numerous and more expanded than in controls (Fig. 1d–f). Remarkably, treated lungs showed practically unchanged histological features between 7 and 14 days; consequently, at the latter stage, differences with control samples were especially strong.
Lung of suckling rats. a–c Normal animals. d–f DEHP-treated animals. a, d Postnatal day 2. b, e Postnatal day 7. c, f Postnatal day 14. B bronchiole, V vessel, c canalicular portion of respiratory space, s saccule, a alveolus. Bar 50 μm. a Respiratory spaces are formed by channels and saccules. Primary septa are thick. b Primary septa are sensibly thinner than in the previous stage, few secondary septa are present. c Saccules are very numerous and small and septa are extremely thin. Some mature alveoli are also recognisable. d Respiratory spaces are sensibly fewer and larger than in control; septa are also fewer. e Respiratory spaces are sensibly larger than in control, saccules and secondary septa are very few. All septa appear thinner than in control. f Respiratory spaces are extremely less numerous and more dilated than in controls, saccules are very few and mature alveoli are absent
Morphometry of respiratory spaces
During the 2 weeks after birth (Fig. 2), normal animals showed (1) gradual increase of the number and total perimeter of respiratory space profiles, (2) gradually decreased mean area and mean perimeter, (3) significantly different values between each stage and the preceding one, with the highest variations between days 2 and 7.
Morphometric parameters of respiratory space profiles in distal lung parenchyma of normal and DEHP-treated suckling rats. For each experimental condition, data are mean ± SD. Number and total perimeter are expressed per mm2 of reference area (see “Material and methods”). * Significantly different from the previous stage (P < 0.01). ° Significantly different from the corresponding control (P < 0.01)
In treated animals, points in (1) and (2) were also true and all the evaluated parameters, with the exception of mean perimeter and Fcircle, significantly varied from one stage to the subsequent one. With respect to controls, respiratory space profiles of test animals showed significantly higher mean area at all the examined stages (between 157 and 180%), significantly higher mean perimeter at 7 and 14 days (between 126 and 136%), and significantly lower number at all ages (between 55 and 67%). Their total perimeter, dramatically low (50% of control) in 2-day-old animals, remained below control values (between 83 and 74%) during development, while the Fcircle at 2 days was significantly higher than control.
Immunolocalization of PCNA
Following either the standard or the amplified ABC method and independent of the microwave treatment, at each examined stage labelling was restricted to the nuclear compartment of different cell populations; all control sections were free of labelling.
In both normal and DEHP-treated animals:
-
at 2 days, many labelled nuclei are found in the bronchial and bronchiolar epithelia and in the adjacent stroma; in the distal parenchyma, PCNA-positive cells are few (Fig. 3) and most of them are located at the tips of the developing septa;
Fig. 3 Lung of 2-day-old rats. PCNA immunolocalization by standard ABC method and haematoxylin counterstaining. a Normal animal. b Treated animal. c Canalicular portion of respiratory space, s saccule, B bronchiole, v vessel. Bar 20 μm. PCNA-positivity is restricted to nuclei, located both in the canalicular portion of respiratory space and in intersaccular walls
-
at 7 days, in the bronchial and bronchiolar epithelia labelling is scarce; by contrast, in the distal parenchyma, PCNA-positive cells are numerous and preferentially found at the saccular corners, i.e. at the base of the developing secondary septa, besides than at their apices; several positive nuclei were also found in the vascular endothelium and in the adjacent stroma;
-
at 14 days the number and position of proliferating cells are similar to those described at the previous stage; in the distal parenchyma, their preferential localization at the septal tips is even more evident.
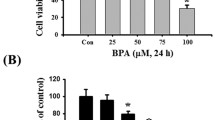
Proliferative index
In both normal and treated rats of all ages (Fig. 4), mesenchymal cells showed a higher proliferation rate than epithelial cells. In normal animals, proliferation was especially active at day 7, with sensible decreases at day 14, and all values were significantly different from those found in the previous stage. In treated animals, at contrast, the proliferation rates progressively increased. In 7-day-old animals, test value for epithelial cells was significantly different from the corresponding control.
Proliferation rates of epithelial and mesenchymal cells in distal lung parenchyma of normal and DEHP-treated suckling rats. For each experimental condition, data are mean ± SD. ** Significantly different from the previous stage (P < 0.01). * Significantly different from the previous stage (P < 0.05). °° Significantly different from the corresponding control (P < 0.01). ° Significantly different from the corresponding control (P < 0.1)
Catalase and α-SMA immunolocalization
In all the examined specimens, independent of the incubation conditions, labelling was found in the cytoplasmic compartment of specific cell types; all control sections were free of labelling.
In both control and treated lung, at all the examined stages, catalase immunoreactivity was restricted to the cytoplasm of type II pneumocytes, many of which were characteristically located at the saccular corners, while all the other cell types were negative. This result, besides confirming and extending our previous data (Farioli-Vecchioli et al. 2001; Magliozzi et al. 2003), further supports the idea that peroxisomes play a key role in synthesis, transport and reutilization of surfactant lipid moiety; moreover, catalase immunocytochemistry was confirmed as a method for automated detection and counting of type II pneumocytes.
Concerning α-SMA, a strong and specific positivity was present in the smooth muscle of bronchial, bronchiolar and vessel walls, as well as in the myocytes in the canalicular portions of respiratory spaces. In intersaccular walls, many labelled cells were found at the tips of the developing secondary septa and around the venules at the junctions of three septa (Fig. 5). Consistent with data from other authors (Pua et al. 2005; Yamada et al. 2005), the majority of these cells are presumed myofibroblasts.
In agreement with the above described quantitative results (higher proliferation rate shown by mesenchymal than by epithelial cells), both in normal and in treated lung the comparison between adjacent sections revealed that the majority of PCNA-labelled cells also contained α-SMA, while only few of them were found to express catalase. Results were similar at all the examined stages; significant examples are shown in Figs. 6, 7, 8.
Lung of normal 2-day-old rats. Adjacent sections submitted to standard ABC method and haematoxylin counterstaining. c Canalicular portion of respiratory space, s saccule. Bar 20 μm. a PCNA immunolocalization. Positivity is restricted to nuclei, located both in the canalicular portion of respiratory space and in intersaccular walls. b Catalase immunolocalization. Positivity is restricted to the cytoplasm of cells identified as type II pneumocytes. Cells containing both PCNA and catalase are extremely scarce (arrows)
Lung of normal 7-day-old rat. Adjacent sections submitted to standard ABC method and haematoxylin counterstaining. B bronchiole, v vessel. Bar 50 μm. a α-SMA immunolocalization. A strong labelling is found in many cells located in the walls of respiratory spaces, as well as in the vascular and bronchiolar walls. b PCNA immunolocalization. The majority of labelled cells are in the walls of respiratory spaces; several PCNA-positive cells are also found in the endothelium of vessels, while only few are present in the bronchiolar epithelium. Cells containing both PCNA and α-SMA are very numerous and practically all of them are situated in the distal parenchyma (arrows). No double-labelled cell can be detected in the smooth muscle of vascular and bronchiolar walls
Lung of DEHP-treated 7-day-old rat. Adjacent sections submitted to standard ABC method and haematoxylin counterstaining. Respiratory spaces are sensibly larger than in control, saccules and secondary septa are very few. Moreover, septa appear thinner than in control. B bronchiole, v vessel. Bar 50 μm. a α-SMA immunolocalization. As in control specimens, myocytes of vascular and bronchiolar walls are strongly labelled and many positive cells are found in the walls of respiratory spaces. b PCNA immunolocalization. As in control specimens, the majority of labelled cells are in the walls of respiratory spaces, while only few are in the bronchiolar epithelium. As in control lung, the cells containing both PCNA and α-SMA are very numerous and are situated in distal parenchyma (arrows)
Discussion
In agreement with results obtained for liver and kidney (Cimini et al. 1994; Stefanini et al. 1995), lung of neonatal rats was found to be especially sensible to DEHP effects. The respiratory space profiles measured in lung sections from DEHP-treated rats, in fact, were significantly lower in number, larger in size and less convoluted in shape, in comparison with those measured in specimens from normal animals. A similar alveolar simplification and lack of septation, with consequent sensible reduction of gas-exchange surface, had been already described in autoptic specimens from children affected by chronic lung diseases (Sobonya et al. 1982; Hislop et al. 1986; Margraf et al. 1991; Husain et al. 1998; Lassus et al. 2001), as well as in lung of hyperoxia-exposed laboratory animals (Coalson et al. 1995; Boros et al. 1997; Pierce et al. 1997; Warner et al. 1998; Albertine et al. 1999); both in pathologic and in experimental conditions these histological alterations had been considered as due to impairment in alveolar maturation.
In agreement with these data and our previous results (Magliozzi et al. 2003), we therefore suggest that in rats delivered and breast-fed by DEHP-treated females the maturation of distal lung parenchyma is severely affected; the septation and the alveolarization processes are impaired not only during the strictly perinatal period but also throughout the following remodelling phase.
Concerning lung parenchyma cellular homeostasis, in normal suckling animals the proliferation rates of both mesenchymal and epithelial cells increased between birth and postnatal day 7 before declining by day 14. Moreover, during the first two postnatal weeks, the proliferation rate of mesenchymal cells was constantly higher than that of type II pneumocytes; these results are partially consistent with previous data (Pua et al. 2005; Yee et al. 2006). The preferential localization of PCNA- and α-SMA-co-expressing cells at the tips of the developing secondary septa and around the venules at the junctions of three septa strongly support the identification of these cells as septal myofibroblasts, which in this postnatal period are especially active in elastogenesis and more generally in septal elongation (Yamada et al. 2005). The high proliferation rates shown at 7 days of life by both epithelial and mesenchymal cells are obviously linked to the strong increase in number of respiratory spaces and the even more dramatic growth of the gas-exchange surface (the total perimeter of respiratory spaces reaching at 14 days a sixfold value over the 2-day value).
In the lung of DEHP-treated rats the percentages of PCNA-positive elements, both for mesenchymal and epithelial cells, progressively increased, differing from control animals, where the highest levels of proliferation were reached at 7 days of life. We suggest that this different trend and, particularly, the lower proliferative rates especially shown by epithelial cells at 7 days are due to the aforementioned impairment in alveolar maturation, mainly consisting in delayed elongation of secondary septa. The proliferation rates here obtained are hardly comparable with those referred for newborn mice and premature primates exposed to hyperoxia (Bonikos et al. 1975; Coalson et al. 1992; Maniscalco et al. 2002), as well as for premature infants with bronchopulmonary dysplasia (Coalson 2000). Similar to the results obtained in adult mammals (Tryka et al. 1986), also in immature lung, the proliferative answer to stress might be species-specific. In any case, the results here obtained in rats delivered and breast-fed by DEHP-treated females suggest that the phthalate adversely affects lung alveolar development by disrupting the proper timing of epithelial and mesenchymal cell proliferation.
Concerning the possible mechanism of action of DEHP, this phthalate, which is able to bind α and γ isotypes of peroxisomal proliferator activated receptor (PPAR) (Maloney and Waxman 1999), was proved to exert toxic effects even in PPARα-null mice (Peters et al. 1997; Ward et al. 1998). As significant levels of PPARγ have been reported in mammalian lung (Chen et al. 1998; Chang and Szabo 2000), we suggested that DEHP effects on immature mammal lung might really be mediated by PPARγ (Magliozzi et al. 2003). In rat lung myofibroblasts, PPARγ expression was found to accompany the transcription of genes involved in triglyceride hydrolysis and fatty acid transport (Chen et al. 1998); notably, the same cells respond to PPAR ligands by increasing their lipid droplet accumulation and lowering the expression of matrix and cytoskeletal components (McGowan et al. 1997). We previously suggested that in immature lung of suckling rats a DEHP-induced increase in translocation of triglycerides from myofibroblasts to pneumocytes, together with alterations in the composition of extracellular matrix, crucial for pneumocytic phenotype achievement and maintenance (Rannels et al. 1987; Mc Gowan 1992), might keep these cells in the surfactant-secreting phenotype, impairing their migration and conversion into flattened elements (Magliozzi et al. 2003). Based on our results, we confirm that in immature rodent lung, DEHP treatment affects the septal myofibroblasts, not only impairing their secretion pattern, but also modifying their proliferation rate. These alterations in myofibroblasts might be crucial in causing the aforementioned impairment in elongation of secondary septa and maturation of alveoli.
References
Albertine KH, Jones GP, Starcher BC, Bohnsack JF, Davis PL, Cho S, Carlton DP, Bland RD (1999) Chronic lung injury in preterm lambs. Am J Respir Crit Care Med 159:945–958
Bally MB, Opheim DJ, Shertzer HG (1980) Di-(2-ethylhexyl)phthalate enhances the release of lysosomal enzymes from alveolar macrophages during phagocytosis. Toxicology 18:49–60
Bonikos DS, Bensch KG, Ludwin SK, Northway WH (1975) Oxygen toxicity in the newborn. The effect of prolonged 100 per cent O2 exposure on the lungs of newborn mice. Lab Invest 32:619–635
Boros V, Burghardt JS, Morgan CJ, Olson DM (1997) Leukotrienes are indicated as mediators of hyperoxia-inhibited alveolarization in newborn rats. Am J Physiol 16:L433–L441
Burri PH (1991) Postnatal development and growth. In: Crystal RG, West JB, Weibel ER, Barnes PJ (eds) The lung: scientific foundations. Lippincott-Raven, Philadelphia, pp 677–687
Calafat AM, Needham LL, Silva MJ, Lambert G (2004) Exposure to di-(2-ethylhexyl) phthalate among premature neonates in a neonatal intensive care unit. Pediatrics 113:e429–e434
Chang TH, Szabo E (2000) Induction of differentiation and apoptosis by ligands of peroxisome proliferator-activated receptor γ in non-small cell lung cancer. Cancer Res 60:1129–1138
Chen H, Jackson S, Doro M, McGowan S (1998) Perinatal expression of genes that participate in lipid metabolism by lipid-laden fibroblast. J Lipid Res 39:2483–2492
Cimini AM, Sulli A, Stefanini S, Serafini B, Moreno S, Rossi L, Giorgi M, Cerù MP (1994) Effects of di-(2-ethylhexyl)phthalate on peroxisomes of liver, kidney and brain of lactating rats and their pups. Cell Mol Biol 40:1063–1076
Coalson JJ (2000) Pathology of chronic lung disease in early infancy. In: Bland R, Coalson JJ (eds) Chronic lung disease in early infancy. Marcel Dekker, New York, pp 85–124
Coalson JJ, Winter VT, Gerstmann DR, Idell S, King RJ, Delemos RA (1992) Pathophysiologic, morphometric, and biochemical studies of the premature baboon with bronchopulmonary dysplasia. Am Rev Respir Dis 145:872–881
Coalson JJ, Winter VT, deLemos RA (1995) Decreased alveolarization in baboon survivors with bronchopulmonary dysplasia. Am J Respir Crit Care Med 152:640–646
de Wildt SN, Kearns GL, Leeder JS, van den Anker JN (1999) Glucuronidation in humans. Pharmacogenetic and developmental aspects. Clin Pharmacokinet 36:439–452
Dostal LA, Jenkins WL, Schwetz BA (1987) Hepatic peroxisome proliferation and hypolipidemic effects of di-(2-ethylhexyl)phthalate in neonatal and adult rats. Toxicol Appl Pharmacol 87:81–90
Farioli-Vecchioli S, Nardacci R, Falciatori I, Stefanini S (2001) Catalase immunocytochemistry allows automatic detection of lung type II alveolar cells. Histochem Cell Biol 115:333–339
Green R, Hauser R, Calafat AM, Weuve J, Schettler T, Ringer S, Huttner K, Hu H (2005) Use of di(2-ethylhexyl) phthalate-containing medical products and urinary levels of mono(2-ethylhexyl) phthalate in neonatal intensive care unit infants. Environ Health Perspect 113:1222–1225
Hislop AA, Wigglesworth JS, Desai R (1986) Alveolar development in the human fetus and infant. Early Hum Dev 13:1–11
Hoppin JA, Ulmer R, London SJ (2004) Phthalate exposure and pulmonary function. Environ Health Perspect 112:571–574
Husain NA, Siddiqui NH, Stocker JR (1998) Pathology of arrested acinar development in post surfactant bronchopulmonary dysplasia. Hum Pathol 29:710–717
Jaeger RJ, Rubin RJ (1972) Migration of a phthalate ester plasticizer from polyvinyl chloride blood bags into stored human blood and its localization in human tissues. N Engl J Med 287:1114–1118
Kamper J (1999) Early nasal continuous positive airway pressure and minimal handling in the treatment of very low birth weight infants. Biol Neonate 76:22–28
Khaliq MA, Alam MS, Srivastava SP (1992) Implications of physico-chemical factors on the migration of phthalate esters from tubing commonly used for oral/nasal feeding. Bull Environ Contam Toxicol 48:572–578
Klimisch HJ, Gamer AO, Hellwig J, Kaufmann W, Jackh R (1992) Di-(2-ethylhexyl)phthalate: a short-term repeated inhalation toxicity study including fertility assessment. Food Chem Toxicol 30:915–919
Labow RS, Barry YA, Tocchi M, Keon WJ (1990) The effect of mono-(2-ethylhexyl)phthalate on an isolated perfused rat heart–lung preparation. Environ Health Perspect 89:189–193
Lake BG, Gray TJBB, Foster JR, Stubberfield CR, Gancolli SD (1984) Comparative studies on di-(2-ethylhexyl)phthalate-induced hepatic peroxisome proliferation in the rat and hamster. Toxicol Appl Pharmacol 72:46–60
Larsen ST, Hansen JS, Hammer M, Alarie Y, Nielsen GD (2004) Effects of mono-2-ethylhexyl phthalate on the respiratory tract in BALB/c mice. Hum Exp Toxicol 23:537–545
Larsen ST, Hansen JS, Hansen EW, Clausen PA, Nielsen GD (2007) Airway inflammation and adjuvant effect after repeated airborne exposures to di-(2-ethylhexyl)phthalate and ovalbumin in BALB/c mice. Toxicol 235:119–129
Lassus P, Turanlahti M, Heikkila P, Andersson LC, Nupponen I, Sarnesto A, Andersson S (2001) Pulmonary vascular endothelial growth factor and Flt-1 in fetuses, in acute and chronic lung disease, and in persistent pulmonary hypertension of the newborn. Am J Respir Crit Care Med 164:1981–1987
Latini G (2000) Potential hazards of exposure to di-(2-ethylhexyl)phthalate in babies. A review. Biol Neonate 78:269–276
Latini G, Avery GB (1999) Material degradation in endotracheal tubes: a potential contributor to bronchopulmonary dysplasia. Acta Paediatr 88:1174–1175
Lewis LM, Flechtner TW, Kerkay J, Pearson KH, Nakamoto S (1978) Bis(2-ethylhexyl)phthalate concentrations in the serum of hemodialysis patients. Clin Chem 24:741–746
Magliozzi R, Nardacci R, Scarsella G, Di Carlo V, Stefanini S (2003) Effects of the plasticiser DEHP on lung of newborn rats: catalase immunocytochemistry and morphometric analysis. Histochem Cell Biol 120:41–49
Maloney EK, Waxman DJ (1999) Trans-activation of PPARα and PPARγ by structurally diverse environmental chemicals. Toxicol Appl Pharmacol 161:209–218
Maniscalco WM, Watkins RH, O’Reilly MA, Shea CP (2002) Increased epithelial cell proliferation in very premature baboons with chronic lung disease. Am J Physiol Lung Cell Mol Physiol 283:L991–L1001
Margraf LR, Tomashefski JF, Bruce MC, Dahms BB (1991) Morphometric analysis of the lung in bronchopulmonary dysplasia. Am Rev Respir Dis 143:391–400
Mc Gowan SE (1992) Extracellular matrix and the regulation of lung development and repair. FASEB J 6:2895–2904
McGowan SE, Jackson SK, Doro MM, Olson PJ (1997) Peroxisome proliferators alter lipid acquisition and elastin gene expression in neonatal rat lung fibroblast. Am J Physiol 17:L1249–L1257
Osumi T, Hashimoto T (1978) Enhancement of fatty acyl-CoA oxidizing activity in rat liver peroxisomes by di-(2-ethylhexyl)phthalate. J Biochem 83:1361–1365
Peters JM, Taubeneck MW, Keen CL, Gonzalez FJ (1997) Di-(2-ethylhexyl)phthalate induces a functional zinc deficiency during pregnancy and teratogenesis that is independent of peroxisome proliferator-activated receptor-alpha. Teratol 56:311–316
Pierce RA, Albertine KH, Starcher BC, Bohnsack JF, Carlton DP, Bland RD (1997) Chronic lung injury in preterm lambs: disorder pulmonary elastin deposition. Am J Physiol 16:L452–L460
Poets CF, Sens B (1996) Changes in intubation rates and outcome of very low birth weight infants: a population study. Pediatrics 98:24–27
Pua ZJ, Stonestreet BS, Cullen A, Shahsafaei A, Sadowska GB, Sunday ME (2005) Histochemical analyses of altered fetal lung development following single vs. multiple courses of antenatal steroids. J Histochem Cytochem 53:1469–1479
Rannels SR, Yarnell JA, Fisher CS, Fabisiak JP, Rannels DE (1987) Role of laminin in maintenance of type II pneumocyte morphology and function. Am J Physiol 253:C835–C845
Reubsaet FAG, Veerkamp JH, Dirven HAAM, Brückwilder MLP, Hashimoto T, Trijbels JMF (1990) The effect of di-(2-ethylhexyl)phthalate on fatty acid oxidation and carnitine palmitoyltransferase in various rat tissue. Biochim Biophys Acta 1047:264–270
Roth B, Herkenrath P, Lehmann HJ, Ohles HD, Hömig HJ, Benz-Bohm G (1988) Di-(2-ethylhexyl)phthalate as plasticizers in PVC respiratory tubing system: indication of hazardous effects on pulmonary function in mechanically ventilated, preterm infants. Eur J Pediatr 147:41–46
Schulz CO, Rubin RJ, Hutchins GM (1975) Acute lung toxicity and sudden death in rats following the intravenous administration of the plasticizer di-(2-ethylhexyl)-phthalate, solubilized with tween surfactant. Toxicol Appl Pharmacol 33:514–525
Sharma RK, Lake BG, Makowski R, Bradshaw D, Dale W, Gibson GG (1989) Differential induction of peroxisomal and microsomal fatty-acid-oxidizing enzymes by peroxisome proliferators in rat liver and kidney. Eur J Biochem 184:69–78
Shertzer HG, Bally MB, Opheim DJ (1982) Inhibition of alveolar macrophages killing by di-(2-ethylhexyl)phthalate. Arch Environ Contam Toxicol 14:605–608
Singh AR, Lawrence WH, Autian J (1972) Teratogenicity of phthalate esters in rats. J Pharm Sci 61:51–55
Sobonya RE, Logvinoff MM, Toussing LR, Teriault A (1982) Morphometric analysis of the lung in prolonged bronchopulmonary dysplasia. Pediatr Res 16:969–972
Stefanini S, Serafini B, Nardacci R, Farioli Vecchioli S, Moreno S, Sartori C (1995) Morphometric analysis of liver and kidney peroxisomes in lactating rats and their pups after treatment with the peroxisomal proliferator di-(2-ethylhexyl)phthalate. Biol Cell 85:167–176
Stern L, Ramos A, Outerbridge EW, Beaudry PH (1970) Negative pressure artificial respiration. Use in treatment of respiratory failure of the newborn. Can Med Assoc J 102:595
Tickner JA, Schettler T, Guidotti T, McCally M, Rossi M (2001) Health risks posed by use of Di-2-ethylhexyl phthalate (DEHP) in PVC medical devices: a critical review. Am J Ind Med 39:100–111
Tomita I, Nakamura Y, Yagi Y, Tutikawa K (1988) Fetotoxic effects of mono-2-ethylhexyl phthalate (MEHP) in mice. Environ Health Perspect 65:249–254
Tryka AF, Witschi H, Gosslee DG, McArthur AH, Clapp NK (1986) Patterns of cell proliferation during recovery from oxygen injury. Species differences. Am Rev Respir Dis 133:1055–1059
Ward JM, Peters JM, Perella CM, Gonzalez FJ (1998) Receptor and nonreceptor-mediated organ-specific toxicity of di-(2-ethylhexyl)phthalate (DEHP) in peroxisome proliferator-activated receptor α-null mice. Toxicol Pathol 26:240–246
Warner BB, Stuart LA, Papes RA, Wispé JR (1998) Functional and pathological effects of prolonged hyperoxia in neonatal mice. Am J Physiol Lung Cell Mol Physiol 275:L110–L117
Yamada M, Kurihara H, Kinoshita K, Sakai T (2005) Temporal expression of alpha-smooth muscle actin and drebrin in septal interstitial cells during alveolar maturation. J Histochem Cytochem 53:735–744
Yee M, Vitiello PF, Roper JM, Staversky RJ, Wright TW, McGrath-Morrow SA, Maniscalco WM, Finkelstein JN, O’Reilly MA (2006) Type II epithelial cells are critical target for hyperoxia-mediated impairment of postnatal lung development. Am J Physiol Lung Cell Mol Physiol 291:L1101–L1111
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosicarelli, B., Stefanini, S. DEHP effects on histology and cell proliferation in lung of newborn rats. Histochem Cell Biol 131, 491–500 (2009). https://doi.org/10.1007/s00418-008-0550-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-008-0550-4