Abstract
Purpose
Thygeson’s superficial punctate keratitis (TSPK) is a chronic and recurrent corneal epitheliopathy. Although first described more than 70 years ago, the precise etiological mechanism and optimal treatment approach for TSPK has not been established. In this paper, we present an up-to date review of the literature and propose a step-by-step management protocol.
Method
A literature search was done on PubMed using keywords including Thygeson’s superficial punctate keratitis, punctate keratitis, etiology, management, and treatment. The literature was reviewed and reported.
Results
The main findings of this review include a summary of the main theories behind the cause TSPK; although topical corticosteroids remain the treatment of choice, long-term risks associated with these agents and recent studies have revealed immunomodulatory agents as promising treatment adjuvants or alternatives for TSPK; surgical interventions such as PRK/PTK have been utilized in selected refractory cases; finally we propose a treatment protocol based the best available evidence and clinical experience.
Conclusion
Although the clinical features of TSPK have been well described, the specific cause of TSPK remains inconclusive. Mechanisms proposed including viral infection, immune-mediated, and immune responses to viral infection but require further investigation. More prospective randomized clinical trials comparing efficacy of corticosteroids, tacrolimus, and cyclosporine A (CSA) are required. More evidence is required for surgical interventions such as PRK/PTK.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thygeson’s superficial punctate keratitis (TSPK) is a chronic and recurrent corneal epitheliopathy characterized by small, elevated, round, white–gray intraepithelial lesions that usually presents bilaterally [1, 2]. TSPK was first described by Phillips Thygeson in 1950 [1]. He initially described 26 patients with a superficial keratitis whom he followed up and studied for more than 20 years. At the same time, Braley and Alexander also studied a series of similar patients and postulated together with Thygeson a viral etiology and effective treatment with topical corticosteroids. Here we present an up-to date review of the literature.
Pathogenesis
The exact etiology and pathogenesis of TSPK is unknown, but several theories have been proposed. Thygeson supported a viral etiology based on the absence of bacteria and other microorganisms; resistance to sulfonamides and antibiotics; associated scanty mononuclear cell exudates observed from conjunctival scrapings; and resemblance of the epithelial lesions to those seen in other viral conditions [1]. So far tissue culture and electron microscopy (EM) studies have failed to demonstrate direct evidence of viral infection in TSPK [4]. Sundmacher et al. however suggested that the lack of viral particles on EM may be due to the fact that the virus could be in a latent form within epithelial samples from TSPK patients and therefore not observable [5]. A single study from Lemp et al. isolated varicella zoster virus from the corneal surface of a 10-year-old boy with TSPK but this observation has not been replicated [6]. Polymerase chain reaction (PCR) analysis of samples from patients with TSPK has distinct advantages over tissue culture and EM. A live viral sample is not required and extremely small samples are adequate. Furthermore, viral DNA can be identified whether the virus is intracellular or extracellular. PCR therefore can potentially identify virus in settings where tissue culture and EM studies have previously been negative but does not pick up infectious live virus particles. Two recent studies employing this technology were not able to detect herpes simplex virus 1 (HSV), HSV 2, varicella zoster virus (VZV), or adenovirus present in the epithelium of patients with TSPK [4, 7]. The presence of lymphocytes in corneal lesions under EM, the marked effect of topical corticosteroids, resistance to antiviral agents, the chronic course of TSPK with remissions and exacerbations, and recent reports of the efficacy of immunomodulators suggest an immunological component to this condition [4, 7,8,9]. Another study revealed a significantly increased frequency of HLA-DR3 in patients with TSPK also suggesting a likely immune mechanism playing a role in pathogenesis. It has been proposed that this antigen may alter an individual’s immune response to viral infections and therefore help explain the characteristic long course of exacerbations and remissions of the disease. The authors postulate that TSPK may be caused by a common virus where the clinical effect on the corneal epithelial and underlying stroma is determined by the presence or absence of HLA-DR3 [8]. Laser confocal studies have identified an increased number of Langerhans cells at the basal cell layer of the corneal epithelium and at Bowman’s layer. In combination with these observations and the marked reduction in the number of LCs after treatment with anti-inflammatories, the authors suggest that TSPK might result, at least in part, from immune responses to an unknown inciting agent [10].
Clinical features and diagnosis
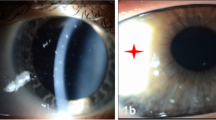
Symptoms of TSPK are ocular irritation, photophobia, pain, discomfort, and blurred vision [11, 12]. At presentation, one study noted that 78.9% of patients were found to have vision of 20/30 or better [3]. The clinical signs include absent to mild conjunctival hyperemia, as well as round or oval shaped clusters of gray granular epithelial opacities that have a central protuberance and occasionally negative or positive stain with fluorescein or rose Bengal [2, 11]. The opacities are usually located in the visual axis and are most commonly bilateral [1, 2]. The number of opacities can range from approximately 3–20 and often change their location from week to week, although in some cases the pattern remains fixed for several months. Corneal sensation is usually normal. Epithelial edema can give rise to what appears to be a faint opacification of the anterior stroma and in some cases smaller round or branched lesions may be the presenting sign and lead to an inappropriate diagnosis of the early stages of HSV/VZV dendritic epithelial keratitis or nummular keratitis [1, 8, 13] (Fig. 1). One study found that symptoms were produced when these corneal lesions were elevated [2].
Differential diagnosis
The differential diagnosis of TSPK includes entities that result in superficial punctate keratopathy, such as viral keratoconjunctivitis, microsporidial keratoconjunctivitis, blepharitis-related keratitis, toxic keratopathy, contact lens related keratitis, and herpetic keratitis [1, 12]. In atypical cases of suspected TSPK, conjunctival and corneal swabs for PCR molecular diagnosis can be useful to rule out adenoviral, HSV, and VZV keratitis in suspicious cases and possibly avoid the use of topical corticosteroids in herpetic epithelial disease.
Histopathology
Laser confocal microscopy studies have revealed that in TSPK, there are highly reflective dots in the corneal epithelium, an increased number of Langerhans cells (LC) in the basal layer of the corneal epithelium as well as in Bowman’s layer, and a decreased subepithelial nerve plexus density [14]. In the affected eyes, the accumulation of dendritic cells was apparent in the focal lesions and visualized in the subepithelial and Bowman’s layer and anterior stroma. The keratocytes in the anterior stroma seen on confocal microscopy were found to have highly reflective cell bodies that were of irregular size, orientation, and shape [14]. These highly reflective materials were found to damage corneal epithelial cell connections resulting in swelling, loss of polygonal structure, widened cells gaps, and destruction of epithelial cells. All these features were believed to be signs of epithelial edema and desquamation and may be responsible for the whitish dots that seen on slit-lamp examination [13, 15]. However, in some patients, these morphologic changes had returned to normal post-treatment [10]. Highly reflective linear lesions were found to be at a level of 110–130 µm deep, corresponding to the intraepithelial and subepithelial corneal layers, and tended to aggregate in a star-burst like appearance. Further pathologic features include disruption of Bowman’s layer with band keratopathy, thickening of Bowman’s layer, subepithelial fibrosis, and in cases with acute inflammation, polymorphonuclear leukocytes were seen in moderate amounts [16, 17].
Management
Multiple therapeutic options have been proposed for TSPK, but it should be noted that no comparative randomized control trials have yet been carried out. Historically, idoxuridine topical therapy was used, but it was associated with an increase in subepithelial opacities and topical antibiotics had no effect on the course of the disease [2]. Other earlier treatments included trifluridine 1% eye drops, but it was found that symptoms and signs of TSPK disappeared more slowly with trifluridine drops than with corticosteroid therapy, and that trifluridine drops were associated with side effects of mild irritation and transient limbal follicle formation [18]. There has been one case series reporting five of six treated eyes with topical trifluridine responding favorably and one patient with an 11-year history of topical corticosteroid dependence experiencing complete resolution which remained for over 1 year without therapy [19]. However, the majority of studies recommend alternative treatments such as soft contact lenses and various topical steroids [2]. Therapeutic contact lenses improved symptoms; however, they did not resolve the corneal lesions which persisted after lens discontinuation [20]. Impaired visual acuity, infection risk, and mechanical damage were issues that needed to be considered [20]. Topical corticosteroids represent the mainstay of treatment for TSPK today and remain very effective in reducing symptoms, signs, and the risk of permanent corneal scarring [3, 16]. However, earlier studies with topical steroids found that the average course of the disease was actually prolonged in patients receiving topical therapy and patients who are not treated with corticosteroids might have a shorter disease course, as has been speculated, although further studies are necessary to confirm this association [2, 3]. Fluorometholone 0.1% eye drops used four times daily and sodium hyaluronate drops given for 1 to 2 weeks were found to reverse abnormal morphology seen on laser confocal microscopy [11]. One case report found that treatment with low-concentration corticosteroid drops and antiviral drugs had recurrence in four out of 21 patients studied; however, the contribution from antivirals was likely minimal [14]. Therapeutic corneal epithelial scraping had resulted in recurrences in the same location approximately 1 week later [2].
More recently, multiple studies examining the use of the immunomodulatory agents cyclosporine A and tacrolimus have suggested an effective new treatment approach for TSPK especially given the risks associated chronic steroid instillation (secondary infections, glaucoma, and cataract). Both these drugs are calcineurin inhibitors which act mainly on T lymphocytes, leading to inhibition of the release of inflammatory cytokines and decreased stimulation of other inflammatory cells. Previous studies have proposed cyclosporine A 2% drops as a long-term treatment of TSPK, noting that it is not associated with any significant side effects, and that it provides a safer long-term alternative to corticosteroid therapy. The only universal side effect reported was a burning sensation at time of instillation [21, 22]. One dosing and tapering regimen proposed using cyclosporine A 2% drops three times daily for 1 month, twice daily for the second month, once daily for the third month, and every other day for the fourth to sixth months, with other studies proposing a similar schedule [9, 22]. With this regimen, corneal opacities were suppressed in 67% of patients mostly after 4 weeks, and of those, about 5% recurred after therapy was stopped at 6 months [9]. Another similar study using cyclosporine A 2% with a 6-month taper was done in both adults and children, concluding that this drop is safe, and finding that about one third of patients had definite healing of corneal lesions, but that in another one third, long-term low-dose cyclosporine drops may be necessary [21]. Other recent studies looked at topical therapy with tacrolimus (0.03% ointment or 0.02% eye drops) which has a more potent immunosuppressant action than CSA and corticosteroids. More specifically the effectiveness may be via direct inhibition of human epidermal LC stimulatory function which as mentioned previously have been implicated in the pathogenesis of TSPK [14]. It has been found to be effective for control of disease, improved visual acuity and symptoms; however, there was recurrence of disease if therapy was stopped [23, 24]. More prospective randomized clinical trials comparing corticosteroids, tacrolimus, and CSA are required. There have been two case reports that have considered excimer laser ablation in patients with TSPK and myopia. One case report of a 20-year-old female with a 2-year history of multiple recurrences of TSPK treated with topical steroids, underwent photorefractive keratectomy (PRK) combined with phototherapeutic keratectomy (PTK), and was found to have no recurrences 8 months post-operatively [25]. Another case of a 49-year-old female with TSPK treated with PRK in her left symptomatic eye reported no recurrence of Thygeson’s keratitis in the central ablation zone but not in the untreated periphery at 17 months post laser. The peripheral recurrence was treated effectively with CSA 2% drops. The mechanism for action is not known but the authors propose that the effect is through the clearing of inflammatory signals (an antigen or chemokine) in the anterior stroma [26]. There is minimal literature on surgical interventions in the treatment of TSPK.
Course of disease
The average duration of TSPK was 11.1 years, with a range of 1 month to 24 years [2, 3]. The longest course reported was up to 40 years. Characteristically, TSPK has a chronic course consisting of multiple episodes of recurrence [8, 14, 27]. Although vision may be mildly decreased during active disease, overall the long-term visual prognosis is excellent. Scarring is not a characteristic of TSPK and there have been only a few cases reported in atypical presentations [1, 2, 16, 20, 28].
Conclusion
-
Although the clinical features of TSPK have been well described, the specific cause of TSPK remains inconclusive. Mechanisms proposed including viral infection, immune-mediated, and immune responses to viral infection and require further investigation.
-
Although topical corticosteroids remain the treatment of choice, long-term risks associated with these agents and recent studies have revealed immunomodulatory agents as promising treatment adjuvants or alternatives for TSPK.
-
More prospective randomized clinical trials comparing corticosteroids, tacrolimus, and CSA are required.
-
More evidence is required for surgical interventions such as PRK/PTK.
References
Thygeson P (1950) Superficial punctate keratitis. J Am Med Assoc. https://doi.org/10.1001/jama.1950.02920180008004
Tabbara KF, Ostler HB, Dawson C et al (1981) Thygeson’s superficial punctate keratitis. Ophthalmology. https://doi.org/10.1016/s0161-6420(81)35089-1
Nagra PK, Rapuano CJ, Cohen EJ et al (2004) Thygeson’s superficial punctate keratitis: ten years’ experience. Ophthalmology. https://doi.org/10.1016/j.ophtha.2003.05.002
Connell PP, O’Reilly J, Coughlan S et al (2007) The role of common viral ocular pathogens in Thygeson’s superficial punctate keratitis. Br J Ophthalmol. https://doi.org/10.1136/bjo.2006.104802
Sundmacher R, Press M, Neumann-Haefelin et al (1977) Keratitis Superficialis Punctata Thygeson. Klin Monatsbl Augenheilkd 170:908–19
Lemp MA, Chambers RW (1974) Lurdy J (1974) Viral isolation in superficial punctate keratitis. Arch Ophthalmol 91:8
Reinhard T, Roggendorf M, Fengler I et al (2004) PCR for varicella zoster virus genome negative in corneal epithelial cells of patients with Thygeson’s superficial punctate keratitis. Eye (Lond). https://doi.org/10.1038/sj.eye.6700621
Darrell RW (1981) Thygeson’s superficial punctate keratitis: natural history and association with HLA DR3. Trans Am Ophthalmol Soc. 79:486–516
Reinhard T, Sundmacher R (1996) Lokale Ciclosporin A Therapie bei Keratitis superficialis punctata Thygeson–eine Pilotstudie [Local cyclosporin A therapy in Thygeson superficial punctate keratitis—a pilot study]. Klin Monbl Augenheilkd. https://doi.org/10.1055/s-2008-1035307
Kawamoto K, Chikama T, Takahashi N et al (2009) In vivo observation of Langerhans cells by laser confocal microscopy in Thygeson’s superficial punctate keratitis. Mol Vis 15:1456–1462
Li J, Qiao J, Cai M et al (2014) Laser confocal microscopy findings of Thygeson’s superficial punctate keratitis. Chin Med J (Engl) 127(3):597–598
Gervasio K (1994) The Wills eye manual: office and emergency room diagnosis and treatment of eye disease. Lippincott, Philadelphia
Kobayashi A, Yokogawa H, Sugiyama K (2011) In vivo laser confocal microscopy findings of Thygeson superficial punctate keratitis. Cornea. https://doi.org/10.1097/ICO.0b013e318200099d
Jiang C, Wang Z, Zhang Y et al (2015) [Clinical analyses of 21 cases of Thygeson’s superficial punctate keratitis]. Zhonghua Yan Ke Za Zhi 51(3):173–177
Cheng LL, Young AL, Wong AK et al (2004) In vivo confocal microscopy of Thygeson’s superficial punctate keratitis. Clin Exp Ophthalmol. https://doi.org/10.1111/j.1442-9071.2004.00783.x
Fintelmann RE, Vastine DW, Bloomer MM et al (2012) Thygeson’s superficial punctate keratitis and scarring. Cornea. https://doi.org/10.1097/ICO.0b013e31823f777f
Hogan MJ, Zimmerman LE (1962) Ophthalmic pathology. An atlas and textbook. WB Saunders, Philadelphia
Nesburn AB, Lowe GH 3rd, Lepoff NJ, Maguen E (1984) Effect of topical trifluridine on Thygeson’s superficial punctate keratitis. Ophthalmology. https://doi.org/10.1016/s0161-6420(84)34170-7
Nesburn AB, Lowe GH, Lepoff NJ et al (1984) Effect of topical trifluridine on Thygeson’s superficial punctate keratitis. Ophthalmology 91(10):1188–1192
Goldberg DB, Schanzlin DJ, Brown SI (1980) Management of Thygeson’s superficial punctate keratitis. Am J Ophthalmol 89:22–24
Reinhard T, Sundmacher R (1999) Topical cyclosporin A in Thygeson’s superficial punctate keratitis. Graefes Arch Clin Exp Ophthalmol. https://doi.org/10.1007/s004170050204
Hasanreisoglu M, Avisar R (2008) Long-term topical cyclosporin A therapy in Thygeson’s superficial punctate keratitis: a case report. Cases J. https://doi.org/10.1186/1757-1626-1-415
Marquezan MC, Nascimento H, Vieira LA et al (2015) Effect of topical tacrolimus in the treatment of Thygeson’s superficial punctate keratitis. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2015.06.019
Shoughy SS, Tabbara KF (2019) Topical tacrolimus in Thygeson superficial punctate keratitis. Cornea. https://doi.org/10.1097/ICO.0000000000002224
Goldstein MH, Feistmann JA, Bhatti MT (2002) PRK-PTK as a treatment for a patient with Thygeson’s superficial punctate keratopathy. CLAO J. https://doi.org/10.1097/01.ICL.0000024359.29208.59
Fite SW, Chodosh J (2001) Photorefractive keratectomy for myopia in the setting of Thygeson’s superficial punctate keratitis. Cornea. https://doi.org/10.1097/00003226-200105000-00018
Reese AB, Mund ML, Iwamoto T (1972) Tapioca melanoma of the iris. Part 1. Clinical and light microscopy studies. Am J Ophthal 74:840–850
Abbott RL, Forster RK (1979) Superficial punctate keratitis of Thygeson associated with scarring and Salzmann’s nodular degeneration. Am J Ophthalmol. https://doi.org/10.1016/0002-9394(79)90066-7
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This submission has not been published anywhere previously and that it is not simultaneously being considered for any other publication.
Rights and permissions
About this article
Cite this article
Mandal, N., Yeung, S.N., Tadrous, C. et al. Thygeson’s superficial punctate keratitis. Graefes Arch Clin Exp Ophthalmol 260, 1837–1841 (2022). https://doi.org/10.1007/s00417-022-05617-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05617-6