Abstract
Pneumatic retinopexy (PR) is a minimally invasive, non-incisional procedure for repairing uncomplicated rhegmatogenous retinal detachment. It consists of an intravitreal gas injection followed by the maintenance of a postoperative head position and the use of laser or cryopexy to seal the retinal breaks. It was initially indicated for a single or a group of retinal breaks no larger than 1 clock hour involving the superior 8 clock hours in phakic eyes with no proliferative vitreoretinopathy. We aim to perform a narrative review on pneumatic retinopexy since the last major review of 2008, based on a Medline search up to June 20 2021 using multiple search words including pneumatic retinopexy, pneumoretinopexy, retinal detachment, and pars plana vitrectomy. Indications for PR have been expanded and include pseudophakic eyes, eyes with mild PVR, and even breaks in the inferior fundus. Depending on the case selection, PR has a single-operation success rate ranging from 45 to 80%. Despite the lower single operation success rate, the functional outcomes of those eyes repaired successfully by primary PR exceed those of scleral buckling (SB) and pars plana vitrectomy (PPV). Best corrected visual acuity, metamorphopsia scores, mental health scores, and vision-related functioning scores were all better in PR-treated eyes compared to PPV-treated eyes. PR should be strongly considered for eligible patients with a primary uncomplicated rhegmatogenous retinal detachments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
Rhegmatogenous retinal detachment (RRD) if left untreated causes blindness. Its incidence has been reported to vary between 6.3 and 17.9 cases per 100,000 inhabitants [1, 2]. The key to a successful retinal repair is the identification of all breaks and their appropriate treatment [3]. Currently, there are several methods of repairing a RRD including pneumatic retinopexy (PR), scleral buckling (SB), and pars plana vitrectomy (PPV). In the past two decades, there has been a generalized trend in favor of PPV as the primary treatment modality for primary un-complicated RRD [4,5,6].
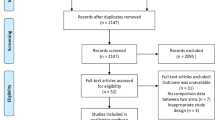
PR is an office-based, minimally invasive, non-incisional procedure for repairing uncomplicated RRD [7]. It consists of an intravitreal injection of an expandable gas bubble, post-injection head positioning to tamponade the retinal breaks and the application of cryopexy or laser retinopexy to the retinal breaks. The most recent comprehensive review on the subject was published in 2008 [7]. The current critical narrative review, based on a MEDLINE search up to 20 June 2021 using multiple search words including pneumatic retinopexy, pneumoretinopexy, retinal detachment, and pars plana vitrectomy, aims to update the literature since 2008.
History
In 1911, Ohm [8] injected intravitreal air as a treatment for RRD. Since this was prior to Gonin’s [3] communication that retinal breaks were the cause of the RRD, the procedure failed. In 1938, Rosengren [9] treated RRD by draining subretinal fluid followed by retinal tear localization and treatment with surface diathermy. Air was then injected into the vitreous cavity to restore intraocular volume and the patient was positioned so that the breaks were superior and tamponaded by the air bubble. Using this method, he obtained a success rate of 76% in his surgical series [6]. Despite these results, this technique did not gain favor among retinal surgeons and remained practically forgotten. Almost half a century later, Dominguez [10] proposed repeated insufflation of an expansile gas bubble into the vitreous cavity followed by laser retinopexy or cryopexy and post-operative positioning. Concurrently, Hilton and Grizzard [11] introduced the concept of an intravitreal gas injection, transconjunctival cryotherapy and post-operative positioning. The modern era of pneumatic retinopexy was thus born. In 2008, Chan and colleagues [7] thoroughly reviewed the literature on the subject.
Evolving treatment preferences in the management of primary RRD
Since its introduction into clinical practice in the late 1980s [11], PR slowly gained popularity. By 1997, PR became the treatment of choice for uncomplicated RRD in the USA [12]. With time, regional differences in the use of PR also began to evolve. Whereas in 1990 within the USA there were no differences in the popularity of PR, by 1997 there was a clear preference for PR in the far west region of the USA [12, 13]. By 2009 vitreoretinal surgeons in the Northeast had a greater preference for PR [14]. However, by this time, an analysis using the fee for service Medicare data from 2000 to 2014 showed that 83% of cases in the USA were treated with PPV, 12% with PR and only 5% with SB [15]. Another larger and more recent study based on administrative claims for beneficiaries in a large managed care network in the USA confirms the preference of PPV in the repair of primary non-complex RRD [6]. USA commercial insurance claims data from 2008 to 2016 revealed that the choice of the initial treatment modality for an uncomplicated primary RRD was based more on patient characteristics and the individual provider than on the particular region [16]. The 2019 ASRS PAT Survey documents a decreasing trend in the use of PR worldwide as well [17]. In the UK, PR is rarely performed [5]. In 2013, only 5% of primary RRD were treated with PR in Northern Ireland [18]. Similarly in Norway, PR accounts for < 1% of primary RRD cases [19]. In Korea, there has been an increasing trend to favor PPV in detriment of PR and SB in eyes with primary uncomplicated RRD [20]. In contrast, PR is a key tool in the arsenal of Canadian vitreoretinal surgeons for the management of primary RRD [21]. Recently, Canadian investigators reported that more than 50% of the primary RRD that presented to their practice fulfilled PR criteria. Around 80% were treated with primary PR [22].
The reasons behind the increasing preference of PPV over SB and PR in most of the world, probably consist of a combination of reimbursement issues, operating room access, technological advances in PPV and less exposure to SB and PR during fellowship training.
Despite having a limited experience with PR, the outcomes of contemporary vitreoretinal fellows in the USA is comparable to those of the more experienced vitreoretinal surgeons. Not surprisingly fellows with > 15 PR procedures had better outcomes than those with < 15 PR procedures [23].
A commercial claims database from the USA has shown troubling gender disparities in the treatment of RRD during the time period of 2007–2015. Women were shown to be less likely to receive surgical repair of a RRD than men. If they were treated, women were more likely to have their RRD repaired with SB, laser barricade or PR than men [24]. Interestingly, in the IRIS Registry of the American Academy of Ophthalmology, female patients were more likely to have a single operation anatomic success rate (SOASR) with PR than male patients [25].
Some have questioned the relevance of PR in developing countries [26]. According to them, the PR criteria are too stringent and few eyes with RRD would be appropriate candidates for primary PR. Patients in developing countries tend to present later and consequently many eyes present with advanced PVR [26]. However, as correctly pointed out by Hillier and Muni [26], late presentation in developing countries may indicate barriers in access to care which usually is due to the financial burden of surgery and/or the lack of vitreoretinal equipped operating rooms. These low resource areas may actually benefit from PR.
Patient selection
Patient selection is the most important factor for a successful outcome using PR to treat RRD. Favorable characteristics include an uncomplicated RRD with a single break or a group of breaks no larger than 1 clock hour. The retinal breaks should be in the superior 8 clock hours of the fundus. Furthermore a clear media that allows complete visualization of the retinal periphery would be ideal [7]. With increased experience, many surgeons expanded the indications for pneumatic retinopexy. Eyes with non-traditional criteria included eyes with visible traction gaping a break open or mild vitreous hemorrhage or > 1 retinal break > 1 clock hour apart or mild proliferative vitreoretinopathy (PVR) or a giant retinal break or extensive lattice degeneration or a bridging vessel or an inferior retinal break or the absence of an identifiable break [27].
In highly motivated patients who are able to place their head in extreme positions, RRD with inferior retinal breaks may be treated successfully with PR [7]. Hwang et al. [28] proposed a less physically demanding position where the patient assumes a lateral recumbent position with the head tilted at 10 cm to 30 cm below the horizontal level. In this position the eye with the retinal break lies at an angle of inclination of 30° to 60° which permits the intravitreal gas bubble to move 1 or 2 clock hours to reach those inferior breaks. Alternatively sequential pneumatic retinopexies with lateral decubitus positioning may be performed instead. Using this technique, Canadian surgeons were able to repair 65% of their 26 cases of RRD with inferior breaks [29].
RRD associated with choroidal colobomas have also been successfully treated with PR [30, 31]. Since the floor of the coloboma is formed by very thin sclera, care must be taken to avoid increases in intraocular pressure. Scleral rupture is a real possibility [31].
Unlike PPV and SB, PR does not relieve vitreoretinal traction and may thus serve as an ideal complementary rescue therapy for failed SB or PPV [32, 33]. A retrospective review of 42 consecutive cases of retinal re-detachment following SB or PPV were managed by a secondary PR. In all the cases of failed SB compared to 90% of all the failed PPV, the retina was re-attached following a single gas injection [33]. In a smaller series, Modi et al. [32] reported similar results. Previously vitrectomized eyes with a limited posterior retinal detachment may be ideally suited for rescue PR [34].
PR has been proposed as an initial procedure in eyes with RRD combined with choroidal detachment [35]. These eyes have a bad prognosis and are typically characterized by hypotony and a high propensity to develop PVR. Although the SOASR in this small series of 9 eyes was only 33%, the intravitreal gas bubble facilitates subsequent vitreous surgery by rapidly restoring intraocular pressure, resolving choroidal detachment and diminishing inflammation. Others have suggested using PR as a temporary measure to protect the macula while waiting for a more definite procedure [36].
PR should be avoided in patients with ocular albinism since the RPE pump in these patients is impaired [37]. PR should also be avoided in eyes without a posterior vitreous detachment since long-lasting gases can cause vitreoretinal traction at the vitreous base leading to new retinal breaks.
Surgical technique
The technique of PR has been reviewed extensively [7, 11]. We hereby provide some tips that may not have been covered in the prior reviews. Injecting an expanding gas intravitreally may potentially lead to not only a rise in intraocular pressure but to central retinal artery occlusion. To avoid these potential complications, one should perform a pre-injection paracentesis. Following the intravitreal gas injection, the surgeon must monitor the optic nerve and central retinal artery ophthalmoscopically. If the artery pulsates, a paracentesis should be repeated.
PR may be performed as a one-step procedure or a two-step procedure. In the one-step procedure, cryopexy is performed prior to intravitreal gas injection, whereas in the two-step procedure, gas is injected intravitreally first. Once the retina is re-attached, laser retinopexy is performed.
In eyes with a bullous RRD that are going to be subjected to PR with cryopexy, a reduction of subretinal fluid prior to cryopexy would be advantageous. Positioning the patient on a reclining chair in a manner where the retinal breaks are placed at the lowest point of the globe for an hour prior to cryopexy accomplishes this objective [38]. Care must be exercised to avoid treating the bare RPE with cryopexy because cryopexy enhances intravitreal dispersion of viable retinal pigment epithelial cells which may lead to PVR. Excessive cryotherapy may also lead to this complication [39]. Due to these potential complications, some surgeons prefer laser retinopexy. The chorioretinal adhesion formed by laser retinopexy may be firmer and form quicker than with cryopexy. Excessive laser may lead to ERM formation.
Following retinal re-attachment, visualization of the retinal break may be impaired by the gas bubble making laser retinopexy extremely difficult. Marking the retinal breaks with laser retinopexy prior to the intravitreal injection of gas may facilitate their identification through the gas bubble after the retina re-attaches [40].
Although most surgeons prefer to use expansile gases such as C3F8 (0.3 mL) or SF6 (0.5 mL), air (0.8 mL) may also be used successfully as an intravitreal tamponading agent in PR [7, 41, 42]. A double blind randomized clinical trial from Thailand compared the retinal re-attachment rate and the final visual recovery following PR with filtered air or perfluoropropane gas. In this small trial, the filtered air was non-inferior to perfluoropropane gas [42]. The main drawback is the larger volume that needs to be injected (0.8 mL) [41]. Larger eyes such as highly myopic ones need to be injected a larger volume of gas to adequately cover the increased retinal area [43]. On occasion, the gas may be re-absorbed before an adequate chorioretinal scar forms around the retinal breaks. In these circumstances, prolongation of the duration of the intravitreal gas bubble would be advantageous. Hsu and colleagues [44] explored the effect of topical aqueous suppressants in the duration of a C3F8 bubble. Unfortunately, they do not prolong the life of the C3F8 bubble. On the other hand, once the retina is attached and the chorioretinal scar is formed, the presence of a long acting gas may be detrimental by causing traction at the vitreous base leading to new ruptures and inflammation.
The steam roller maneuver has been recommended to avoid migrating subretinal fluid to detach the macula following PR. In eyes with the macula already detached, the steamroller maneuver facilitates rapid retinal re-attachment [45]. Following the intravitreal gas injection, the patient is asked to immediately assume a face down positioning for 4–6 h. The buoyancy of the intravitreal gas bubble will help express the subretinal fluid through the open retinal break. This reduces the overall amount of subretinal fluid that needs to be reabsorbed by the RPE pump. Thereafter, the head is elevated 30° every hour until the head is upright. Once the head is upright, the patient is positioned so that the apex of the intravitreal bubble covers the retinal breaks [45]. It is important to emphasize to the patient that the steamroller maneuver needs to be performed just once. A pneumatic pump mechanism has been described whereby retinal detachment extension occurred after repeated steamroller maneuvers by a same patient [46].
Retinal re-attachment
Bansal et al. [47] used swept source OCT to characterize the in vivo retinal re-attachment process of 15 consecutive patients that underwent successful PR into 5 specific stages. With closure of the retinal break by the gas bubble, there is no longer liquefied vitreous entering the subretinal space. Re-absorption and re-distribution of the subretinal fluid ensues, which causes a reduction in the height of the retinal detachment allowing an approximation of the neurosensory retina and the RPE (stage 1). In stage 2, the outer retinal corrugations and the cystoid macular edema improve. Eventually, the RPE and the neurosensory retina come into physical contact signaling stage 3. Stage 4 is characterized by the deturgescence of the photoreceptor inner and outer segments. Recovery of the photoreceptor integrity starts with the external limiting membrane (stage 5A) followed by the ellipsoid zone (stage 5B) and finally the interdigitation zone/foveal bulge (stage 5C). Not all patients progressed at the same rate. For instance some eyes had delayed re-absorption of subretinal fluid [47].
Anatomic outcomes
Chan and colleagues [7] comprehensively reviewed the literature from 1986 to 2007. They identified 4138 eyes. In this time period, the SOASR was reported to be 75%, the final operation anatomic success 96%, new retinal breaks occurred in 12% and PVR in 6% [7]. Since then, several studies have reported on over 12,000 patients with similar outcomes [25, 27, 41, 46, 48,49,50,51,52,53,54,55,56]. These are summarized in Table 1.
Day et al. [57] compared the re-operation rate among a 5% random sample of Medicare beneficiaries > 67 years of age who underwent retinal detachment repair from 1991–2007. They reported that eyes treated with a primary PR were twice as likely to undergo a second repair procedure than eyes that were treated with a primary SB or PPV. Most of the eyes that failed primary PR underwent a secondary PPV. Interestingly, eyes that were treated primarily with PPV were most likely to develop severe complications [57]. A 2015 Cochrane review reported that there was a lower retinal re-attachment rate and a higher recurrence rate with PR when compared to SB [58].
Goldman et al. [27] reported a series of 141 eyes that included eyes with non-traditional indications in 55.3%. The SOASR were not statististically different between eyes with traditional indications (84.1%) compared to non-traditional indications (74.4%). The final anatomic success rate was 97.6% [27]. Similarly, Jung et al. [51] reported no difference between traditional and expanded indications.
The PIVOT was a single center, randomized clinical trial that compared the outcomes of primary PR in 77 eyes versus primary PPV in 73 eyes with primary RRD [52] The inclusion criteria included eyes with a single retinal break or group of breaks ≤ 1 clock hour in detached retina; all the breaks in detached retina had to be between the 8 and 4 meridians; lattice degeneration and breaks in attached retina at any location were allowed. Exclusion criteria included inferior breaks in detached retina, PVR grade B or worse or inability to perform a complete peripheral retina examination. SOASR was significantly better in PPV (93.2%) compared to PR (80.8%). The final anatomic success rate was similar in both groups (98.7% and 98.6% respectively) [52].
A recent report of almost 10,000 patients with a non-complex RRD that underwent PR with at least 3 months of follow-up from the IRIS Registry, showed a SOASR of 68.5%. Female and non-smokers had a higher SOASR. The main limitations of this study were the inability to determine the selection criteria by which these patients were selected to undergo PR and the pre-operative macular status [25].
Functional outcomes
Previously, Chan et al. [7] summarized the visual outcomes from 1986 to 2007. They reported that in RRD with the macula detached pre-operatively, anywhere from 35 to 90% of eyes achieved a post-operative visual acuity (VA) ≥ 20/50. In eyes with the macula attached, 22.2 to 100% of eyes had an improvement of post-operative VA over pre-operative VA. In addition, 56.2 to 94% of eyes with the macula attached obtained a post-operative VA of ≥ 20/40 [7].
The visual outcomes of studies since 2007 are summarized in Table 1 [22, 23, 41, 42, 48, 51, 52, 55, 56, 59,60,61]. The final reported VA varied from 20/158 to 20/25. In eyes with a SOASR, the final VA varied from 20/50 to 20/25. In contrast, eyes that failed primary PR had a final VA of 20/27.5 to 20/324 [22, 23, 41, 42, 48, 51, 52, 55, 56, 59,60,61]. The PIVOT trial demonstrated that the visual acuity outcomes with PR were superior to those obtained with PPV [52]. The ETDRS best corrected VA was better at 3, 6, and 12 months of follow-up. The mean best corrected VA at 12 months was 79.9 letters in the PR group compared to 75 letters in the PPV group. In addition the proportion of eyes achieving ≥ 20/40 was 90.3% compared to 75.3% in the PPV group [52].
Most failures of primary PR occur during the first month following PR, the vast majority during the first 10 days [46, 62]. Pseudophakia [22, 46, 49, 51, 55, 59], male gender [46, 49], vitreous hemorrhage [62] tears > 1 clock hour [55], RD involving the inferior quadrants [51], PVR grades C or D [51, 55], new or missed breaks [49, 62], and smoking [25] have all been identified as increasing the risk of failure in SOASR in primary PR [46, 49, 51, 59]. The SOASR for primary PR in pseudophakic eyes ranges from 41 to 67% [7, 63]. Pseudophakic eyes are more likely to have multiple, small, and anteriorly located breaks. Optical aberrations due to the presence of the intraocular lens and capsular opacity may limit the view of the peripheral retina. These factors may be responsible for the increased risk of failure of PR in pseudophakic eyes [51, 64]. In pseudophakic eyes, the extent of the RRD correlates with SOASR [50, 63]. More extensive RRD may “hide” some breaks dooming the SOASR for primary PR. Others have not found pseudophakia as a risk factor for PR failure [27, 52, 59, 61, 65]. Male patients apparently are less compliant with instructions [46]. The most common causes of a failed primary PR are a new inferior RRD in previously attached retina and increasing subretinal fluid associated with the original RRD [62].
PR failure was not associated with significant differences in functional or anatomic outcomes between eyes who had a successful primary PR and those that failed and were fixed with one additional procedure [63]. Table 2 summarizes the outcomes of eyes that had failure of primary PR. Up to 90% may be repaired with one additional procedure [48, 62, 65,66,67]. Demircan et al. [67] compared the outcomes of 42 eyes that failed primary PR and were treated subsequently with PPV to 29 eyes that were treated primarily with PPV. They found that there were no statistically significant differences between both groups in terms of primary retinal re-attachment (90.5% vs 93.1% respectively) or visual outcomes underscoring the fact that a failed primary PR does not predispose to a worse outcome. However, if the eye needed ≥ 2 additional procedures or complications occurred, the visual outcomes were significantly worse [48, 66]. Eyes that require ≥ 1 additional procedure are more likely to develop complications such as new or missed breaks, cataracts (65%), ERM (16%), CME (4%), and macular hole (2%) [66]. These eyes also required additional non-reattachment procedures such as vitrectomy for removal of ERM and silicone oil removal. A repeat PR was significantly worse than SB or PPV in re-attaching the retina [66]. Anaya et al. [65] reported that in their series of 73 eyes that failed primary PR, the anatomic success rates for the secondary procedure were lower than the published success rates for primary repair using those procedures. They suggest that a failed primary PR selects for RRDs that are inherently more difficult to repair [65]. Multivariate analysis in a large retrospective study identified new or missed breaks and poor pre-operative VA as the only determinants that affected both SOASR and visual outcome [49].
Gauthier and Adelman [68] compared the quality of life between PR and SB. They reported similar outcomes in both groups. There was a trend towards preferring PR over SB if the fellow eye developed a new RRD. The main limitation of this study was that subjects completed their surveys up to 8 years following the surgical repair. The PIVOT trial showed that eyes that underwent PR scored higher in mental health and vision-related functioning scores than eyes subjected to PPV during the first 6 months following the respective procedure [69, 70].
Unintentional retinal displacement following retinal re-attachment has been described. Fundus autofluorescence (FAF) may be used to assess the degree of retinal displacement by comparing the hyper FAF lines located superior and parallel to the retinal vessels [71]. This retinal displacement may account for the post-operative vertical metamorphopsia experienced by some patients. In the PIVOT trial, FAF images were used to demonstrate that the retinal displacement induced by PR to those induced by PPV was significantly less [72]. Vertical metamorphopsia scores were also superior in the eyes treated with PR than those treated with PPV in the PIVOT trial [52]. At 12 months, eyes subjected to PPV exhibited less photoreceptor integrity as documented on SD-OCT when compared to eyes treated with PR. PPV treated eyes had more ellipsoid zone (24% vs 7%) and external limiting membrane (20% vs 6%) discontinuity in comparison to eyes treated with PR [73].
Complications
PR is a relatively safe procedure if performed correctly. Several complications associated to PR have been reported over the years [7]. These include new or missed retinal breaks, cataract progression, subconjunctival gas, vitreous loss, subretinal gas, gas entrapment in the pre-hyaloid space, anterior chamber gas entrapment, endophthalmitis, macular hole, iris and vitreous incarceration, uveitis, CME, intraocular hemorrhage, ERM, PVR, musculoskeletal complications, macular folds, and elevation of intraocular pressure leading to corneal wound dehiscence [7]. A corneal graft dehiscence has even been reported following PR [74]. A pre-injection paracentesis will avoid this complication. Giant retinal breaks have been reported after PR [75, 76]. New breaks have been attributed to additional vitreoretinal traction caused by the expanding gas bubble in an eye with an incomplete posterior vitreous detachment. The most common complications reported since 2008 are summarized in Table 1, and include new or missed breaks, CME, ERM, cataract progression, persistent SRF, macular hole, and PVR. These do not appear to be significantly different from Chan et al.’s [7] review.
Some patients complain of post-operative aniseikonia regardless of the surgical technique employed to re-attach the retina. In eyes treated with PR, post-operative aniseikonia is associated with the pre-operative macular status. Eyes with macula off RRD are more commonly affected with aniseikonia than eyes with macula on RRD. All the eyes that developed aniseikonia had micropsia [77].
Cost utility analysis
Since patients do not need to be taken to the operating room, PR is a cost-effective option to repair primary non-complex RRD. Estimates suggest that PR may result in a 50.9% savings when compared to SB and a 59.4% savings when compared to PPV [27, 51]. The costs involved with primary PR and subsequent procedures to achieve final anatomic success in both traditional and expanded indications for PR are not significantly different suggesting that expanded indications for PR are cost-effective [51]. Elhusseiny et al. [78] performed a cost-utility analysis comparison between PR and PPV using the data from the PIVOT study. They concluded that both methods of retinal re-attachment were highly cost-effective with PR being approximately 50% more favorable than PPV. In 2014, Goldman et al. [27] estimated that by increasing utilization of PR as a primary repair for uncomplicated primary RRD, the USA could save up to US$30 million in annual health costs. These figures actually underestimate the savings since the costs of cataract surgery were not taken into account. A very high percentage of eyes that undergo PPV will require cataract extraction [27].
A comparison of the quality-adjusted life years (QALY) of PR, SB, and PPV showed that the US dollars per QALY ranged from $1053 to $1667 on the assumption of a SOASR of 60 to 90%. In contrast the US dollars per QALY for SB and PPV were $1912 and $2243 respectively. Overall, regardless of the method employed to repair a RRD, treatment of RRD is extremely cost-effective [79].
Conclusions
Prior reviews have emphasized the quickness, minimal invasivess, lower cost, in office procedure characteristics of PR. These advantages need to be put on a balance with the lower SOASR associated with primary PR. We are in complete disagreement with Chronopoulos et al.’s [80] highly critical assessment of PR and their recommendation to abandon PR altogether except in extreme circumstances where PPV or SB can't be performed in a timely fashion and only in eyes with favorable characteristics.
There is an increasing body of evidence suggesting that PR should be the treatment of choice in eligible eyes. Recent data from the PIVOT trial demonstrate the superior visual outcomes obtained with PR over PPV. Not only did the BCVA but metamorphopsia scores, mental health scores and vision-related functioning scores were all better in PR-treated eyes compared to PPV-treated eyes. Promoting PR in eligible patients worldwide may improve their functional outcomes. As Yorston [81] recently pointed out, it is time to consider additional clinical trials comparing PPV to PR that confirm the PIVOT trial results. In addition to visual acuity, SOASR and other anatomic outcomes, patient centered functional outcomes such as vision-related function and quality of life in retinal and macular diseases need to be measured and incorporated into future trials as recommended by Weng [70].
References
Li JQ, Welchowski T, Schmid M, Holz FG, Finger RP (2019) Incidence of rhegmatogenous retinal detachment in Europe - a systematic review and meta-analysis. Ophthalmologica 242:81–86. https://doi.org/10.1159/000499489
Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J (2010) The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol 94:678–684. https://doi.org/10.1136/bjo.2009.157727
Gonin J (1921) Le traitement du décollement rétinien. Ann d’Ocul 158:175
Seider MI, Nomides RE, Hahn P, Mruthyunjaya P, Mahmoud TH (2016) Scleral buckling with chandelier illumination. J Ophthalmic Vis Res 11:304–309. https://doi.org/10.4103/2008-322X.188402
Jackson TL, Donachie PH, Sallam A, Sparrow JM, Johnston RL (2014) United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 3, retinal detachment. Ophthalmology 121:643–648. https://doi.org/10.1016/j.ophtha.2013.07.015
Reeves MG, Pershing S, Afshar AR (2018) Choice of primary rhegmatogenous retinal detachment repair method in US commercially insured and Medicare advantage patients, 2003–2016. Am J Ophthalmol 196:82–90. https://doi.org/10.1016/j.ajo.2018.08.024
Chan CK, Lin SG, Nuthi AS, Salib DM (2008) Pneumatic retinopexy for the repair of retinal detachments: a comprehensive review (1986–2007). Surv Ophthalmol 53:443–478. https://doi.org/10.1016/j.survophthal.2008.06.008
Ohm J (1911) Über die Behandlung der Netzhautablösung durch operative Entleerung der subretinalen Flüssigkeit und Einspritzung von Luft in den Glaskörper. Albrecht von Graefes Archiv für Ophthalmologie 79:442–450
Rosengren B (1938) Results of treatment of detachment of the retina with diathermy and injection of air into the vitreous. Acta Ophthalmol (Copenh) 16:573–579
Dominguez A (1985) Cirugia Precoz y Ambulatoria del Desprendimiento de Retina. Arch Soc Esp Oftal 48:47–54
Hilton GF, Grizzard WS (1986) Pneumatic retinopexy. A two-step outpatient operation without conjunctival incision. Ophthalmology 93:626–641. https://doi.org/10.1016/s0161-6420(86)33696-0
Benson WE, Chan P, Sharma S, Snyder WB, Bloome MA, Birch DG (1999) Current popularity of pneumatic retinopexy. Retina 19:238–241
Snyder WB, Bloome MA, Birch DG (1992) Pneumatic retinopexy versus scleral buckle. Preferences of Vitreous Society members, 1990. Retina 12:43–45
Hwang JC (2012) Regional practice patterns for retinal detachment repair in the United States. Am J Ophthalmol 153:1125–1128. https://doi.org/10.1016/j.ajo.2011.11.034
McLaughlin MD, Hwang JC (2017) Trends in vitreoretinal procedures for Medicare beneficiaries, 2000 to 2014. Ophthalmology 124:667–673. https://doi.org/10.1016/j.ophtha.2017.01.001
Vail D, Pershing S, Reeves MG, Afshar AR (2020) The relative impact of patient, physician, and geographic factors on variation in primary rhegmatogenous retinal detachment management. Ophthalmology 127:97–106. https://doi.org/10.1016/j.ophtha.2019.04.019
Hillier RJ, Felfeli T, Juncal VR, Muni RH (2020) Re: Elhusseiny et al.: Cost analysis of pneumatic retinopexy versus Pars Plana Vitrectomy for rhegmatogenous retinal detachment (Ophthalmol Retina. 2019;3:956–961). Ophthalmol Retina 4:e3–e4. https://doi.org/10.1016/j.oret.2019.12.007
Mikhail MA, Mangioris G, Casalino G, McGimpsey S, Sharkey J, Best R, Chan WC (2017) Outcome of primary rhegmatogenous retinal detachment surgery in a tertiary referral centre in Northern Ireland - A regional study. Ulster Med J 86:15–19
Haugstad M, Moosmayer S, Bragadomicronttir R (2017) Primary rhegmatogenous retinal detachment - surgical methods and anatomical outcome. Acta Ophthalmol 95:247–251. https://doi.org/10.1111/aos.13295
Cho GE, Kim SW, Kang SW, Korean Retina S (2014) Changing trends in surgery for retinal detachment in Korea. Korean J Ophthalmol 28:451–459. https://doi.org/10.3341/kjo.2014.28.6.451
Arjmand P, Murtaza F, Eshtiaghi A, Popovic MM, Kertes PJ, Eng KT (2020) Impact of the COVID-19 pandemic on characteristics of retinal detachments: the Canadian experience. Can J Ophthalmol. https://doi.org/10.1016/j.jcjo.2020.12.008
Juncal VR, Bamakrid M, Jin S, Paracha Q, Ta Kim DT, Marafon SB, Francisconi CLM, Muni RH (2021) Pneumatic retinopexy in patients with primary rhegmatogenous retinal detachment meeting PIVOT trial criteria. Ophthalmol Retina 5:262–269. https://doi.org/10.1016/j.oret.2020.07.022
Emami-Naeini P, Deaner J, Ali F, Gogte P, Kaplan R, Chen KC, Nudleman E, Grewal DS, Gupta M, Wolfe JD, Klufas M, Yiu G, Academic Vitreoretinal Training Centers Study G (2019) Pneumatic Retinopexy Experience and Outcomes of Vitreoretinal Fellows in the United States: A Multicenter Study. Ophthalmol Retina 3:140–145. https://doi.org/10.1016/j.oret.2018.09.010
Callaway NF, Vail D, Al-Moujahed A, Ludwig C, Ji MH, Mahajan VB, Pershing S, Moshfeghi DM (2020) Sex Differences in the Repair of Retinal Detachments in the United States. Am J Ophthalmol 219:284–294. https://doi.org/10.1016/j.ajo.2020.06.039
Yannuzzi NA, Li C, Fujino D, Kelly SP, Lum F, Flynn HW, Jr., Parke III W (2021) Clinical outcomes of rhegmatogenous retinal detachment treated with pneumatic retinopexy. JAMA Ophthalmol Published online June 17, 2021. https://doi.org/10.1001/jamaophthalmol.2021.1860
Kumawat D, Sachan A (2019) Re: Hillier et al.: The pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial (PIVOT) (Ophthalmology. 2019;126:531–539). Ophthalmology 126: e84. https://doi.org/10.1016/j.ophtha.2019.05.003
Goldman DR, Shah CP, Heier JS (2014) Expanded criteria for pneumatic retinopexy and potential cost savings. Ophthalmology 121:318–326. https://doi.org/10.1016/j.ophtha.2013.06.037
Hwang JF, Chen SN, Lin CJ (2011) Treatment of inferior rhegmatogenous retinal detachment by pneumatic retinopexy technique. Retina 31:257–261. https://doi.org/10.1097/IAE.0b013e3181e586f9
Alali A, Bourgault S, Hillier RJ, Muni RH, Kertes PJ (2020) Sequential pneumatic retinopexies for the treatment of primary inferior rhegmatogenous retinal detachments with inferior breaks: the double-bubble approach. Retina 40:299–302. https://doi.org/10.1097/IAE.0000000000002369
Rishi E, Rishi P, Govindarajan MV (2016) Pneumatic retinopexy for the treatment of shallow retinal detachment caused by a retinal break in the intercalary membrane of macula sparing retinochoroidal coloboma. Retin Cases Brief Rep 10:187–190. https://doi.org/10.1097/ICB.0000000000000222
Giansanti F, Giuntoli M, Mazzini C, Pieretti G, Abbruzzese G, Menchini U (2012) Pneumatic retinopexy for retinal detachment associated with choroidal coloboma. Eur J Ophthalmol 22:680–682. https://doi.org/10.5301/ejo.5000065
Modi YS, Townsend J, Epstein AE, Smiddy WE, Flynn HW Jr (2014) Pneumatic retinopexy for retinal detachment occurring after prior scleral buckle or pars plana vitrectomy. Ophthalmic Surg Lasers Imaging Retina 45:409–413. https://doi.org/10.3928/23258160-20140909-05
Petrushkin HJ, Elgohary MA, Sullivan PM (2015) Rescue pneumatic retinopexy in patients with failed primary retinal detachment surgery. Retina 35:1851–1859. https://doi.org/10.1097/IAE.0000000000000546
Bastion ML (2012) Pneumatic retinopexy for treatment of posterior pole detachment following vitreoretinal surgery for diabetic tractional retinal detachment threatening the fovea. BMJ Case Rep 2012:bcr2012006303. https://doi.org/10.1136/bcr-2012-006303
Yeung L, Kokame GT, Brod RD, Lightman DA, Lai JC (2011) Pneumatic retinopexy for retinal detachment associated with severe choroidal detachment. Retina 31:87–92. https://doi.org/10.1097/IAE.0b013e3181e0974c
Stewart S, Chan W (2018) Pneumatic retinopexy: patient selection and specific factors. Clin Ophthalmol 12:493–502. https://doi.org/10.2147/OPTH.S137607
Felfeli T, Mandelcorn MS, Yan P, Jeffery G, Mandelcorn ED (2017) Failed pneumatic retinopexy for rhegmatogenous retinal detachment repair in ocular albinism: clues to the role of melanin in retinal pigment epithelium pump function. Ophthalmic Surg Lasers Imaging Retina 48:1016–1020. https://doi.org/10.3928/23258160-20171130-10
Dorrepaal SJ, Gale J (2014) Using patient positioning to promote resorption of subretinal fluid in rhegmatogenous retinal detachment before pneumatic retinopexy. Retina 34:477–482. https://doi.org/10.1097/IAE.0b013e31829f73d5
Campochiaro PA, Kaden IH, Vidaurri-Leal J, Glaser BM (1985) Cryotherapy enhances intravitreal dispersion of viable retinal pigment epithelial cells. Arch Ophthalmol 103:434–436. https://doi.org/10.1001/archopht.1985.01050030130038
Muni RH, Kertes PJ (2009) Marking of retinal breaks in detached retina with laser photocoagulation before pneumatic retinopexy: a prospective case series. Retina 29:405–408. https://doi.org/10.1097/IAE.0b013e31819a6019
Yee KM, Sebag J (2011) Long-term results of office-based pneumatic retinopexy using pure air. Br J Ophthalmol 95:1728–1730. https://doi.org/10.1136/bjophthalmol-2011-300114
Sinawat S, Ratanapakorn T, Sanguansak T, Prompol S, Laopaiboon M, Yospaiboon Y (2010) Air vs perfluoropropane gas in pneumatic retinopexy: a randomized noninferiority trial. Arch Ophthalmol 128:1243–1247. https://doi.org/10.1001/archophthalmol.2010.230
Williamson TH, Guillemaut JY, Hall SK, Hutter JC, Goddard T (2018) Theoretical gas concentrations achieving 100% fill of the vitreous cavity in the postoperative period. Retina 38(Suppl 1):S60–S64. https://doi.org/10.1097/IAE.0000000000001963
Hsu J, Gerstenblith AT, London NJ, Garg SJ, Spirn MJ, Maguire JI, Park C, Sivalingam A (2014) Effect of topical aqueous suppression on intraocular gas duration after pure perfluoropropane injection in nonvitrectomized eyes with retinal detachment. Retina 34:2458–2461. https://doi.org/10.1097/IAE.0000000000000244
Muni RH, Francisconi CLM (2020) Pneumatic Retinopexy: The Steamroller Maneuver and Head Positioning. https://www.aaoorg/clinical-video/pneumatic-retinopexy-steamroller-maneuver-head-pos. Accessed 18 June 2021
Gorovoy IR, Eller AW, Friberg TR, Coe R (2014) Characterization of pneumatic retinopexy failures and the pneumatic pump: a new complication of pneumatic retinopexy. Retina 34:700–704. https://doi.org/10.1097/IAE.0000000000000002
Bansal A, Lee WW, Felfeli T, Muni RH (2021) Real-time in vivo assessment of retinal reattachment in humans using swept-source optical coherence tomography. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2021.02.013
Fabian ID, Kinori M, Efrati M, Alhalel A, Desatnik H, Hai OV, Katz G, Platner E, Moisseiev J (2013) Pneumatic retinopexy for the repair of primary rhegmatogenous retinal detachment: a 10-year retrospective analysis. JAMA Ophthalmol 131:166–171. https://doi.org/10.1001/2013.jamaophthalmol.361
Gilca M, Duval R, Goodyear E, Olivier S, Cordahi G (2014) Factors associated with outcomes of pneumatic retinopexy for rhegmatogenous retinal detachments: a retrospective review of 422 cases. Retina 34:693–699. https://doi.org/10.1097/IAE.0b013e3182a2e6ee
Cohen E, Zerach A, Mimouni M, Barak A (2015) Reassessment of pneumatic retinopexy for primary treatment of rhegmatogenous retinal detachment. Clin Ophthalmol 9:2033–2037. https://doi.org/10.2147/OPTH.S91486
Jung JJ, Cheng J, Pan JY, Brinton DA, Hoang QV (2019) Anatomic, visual, and financial outcomes for traditional and nontraditional primary pneumatic retinopexy for retinal detachment. Am J Ophthalmol 200:187–200. https://doi.org/10.1016/j.ajo.2019.01.008
Hillier RJ, Felfeli T, Berger AR, Wong DT, Altomare F, Dai D, Giavedoni LR, Kertes PJ, Kohly RP, Muni RH (2019) The pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial (PIVOT). Ophthalmology 126:531–539. https://doi.org/10.1016/j.ophtha.2018.11.014
Rahat F, Nowroozzadeh MH, Rahimi M, Farvardin M, Namati AJ, Sarvestani AS, Sharifi F (2015) Pneumatic retinopexy for primary repair of rhegmatogenous retinal detachments. Retina 35:1247–1255. https://doi.org/10.1097/IAE.0000000000000434
Hazzazi MA, Al Rashaed S (2017) Outcomes of Pneumatic Retinopexy for the Management of Rhegmatogenous Retinal Detachment at a Tertiary Care Center. Middle East Afr J Ophthalmol 24:143–147. https://doi.org/10.4103/meajo.MEAJO_137_15
Rootman DB, Luu S, S MC, Mandell M, Devenyi R, Lam WC, Kertes PJ, (2013) Predictors of treatment failure for pneumatic retinopexy. Can J Ophthalmol 48:549–552. https://doi.org/10.1016/j.jcjo.2013.05.002
Schaal S, Sherman MP, Barr CC, Kaplan HJ (2011) Primary retinal detachment repair: comparison of 1-year outcomes of four surgical techniques. Retina 31:1500–1504. https://doi.org/10.1097/IAE.0b013e31820d3f55
Day S, Grossman DS, Mruthyunjaya P, Sloan FA, Lee PP (2010) One-year outcomes after retinal detachment surgery among medicare beneficiaries. Am J Ophthalmol 150:338–345. https://doi.org/10.1016/j.ajo.2010.04.009
Hatef E, Sena DF, Fallano KA, Crews J, Do DV (2015) Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev 5(5):CD008350. https://doi.org/10.1002/14651858.CD008350.pub2
Davis MJ, Mudvari SS, Shott S, Rezaei KA (2011) Clinical characteristics affecting the outcome of pneumatic retinopexy. Arch Ophthalmol 129:163–166. https://doi.org/10.1001/archophthalmol.2010.352
Ellakwa AF (2012) Long term results of pneumatic retinopexy. Clin Ophthalmol 6:55–59. https://doi.org/10.2147/OPTH.S22063
Dhami A, Shah KK, Ratra D (2018) Pneumatic retinopexy outcomes as primary or secondary surgical option for treating rhegmatogenous retinal detachment. Indian J Ophthalmol 66:420–425. https://doi.org/10.4103/ijo.IJO_999_17
Mudvari SS, Ravage ZB, Rezaei KA (2009) Retinal detachment after primary pneumatic retinopexy. Retina 29:1474–1478. https://doi.org/10.1097/IAE.0b013e3181ae70f3
Ling J, Noori J, Safi F, Eller AW (2018) Pneumatic retinopexy for rhegmatogenous retinal detachment in pseudophakia. Semin Ophthalmol 33:198–201. https://doi.org/10.1080/08820538.2016.1190849
Gupta D, Ching J, Tornambe PE (2018) Clinically undetected retinal breaks causing retinal detachment: a review of options for management. Surv Ophthalmol 63:579–588. https://doi.org/10.1016/j.survophthal.2017.08.002
Anaya JA, Shah CP, Heier JS, Morley MG (2016) Outcomes after failed pneumatic retinopexy for retinal detachment. Ophthalmology 123:1137–1142. https://doi.org/10.1016/j.ophtha.2016.01.017
Vidne-Hay O, Abumanhal M, Elkader AA, Fogel M, Moisseiev J, Moisseiev E (2020) Outcomes of rhegmatogenous retinal detachment repair after failed pneumatic retinopexy. Retina 40:805–810. https://doi.org/10.1097/IAE.0000000000002483
Demircan A, Alkin Z, Cakir I, Kesim C, Erdogan G (2019) Comparison of pars plana vitrectomy for retinal detachment after failed pneumatic retinopexy and primary pars plana vitrectomy. J Fr Ophtalmol 42:146–152. https://doi.org/10.1016/j.jfo.2018.09.004
Gauthier AC, Adelman RA (2017) A quality of life study comparing scleral buckle and pneumatic retinopexy for the treatment of rhegmatogenous retinal detachment. Clin Ophthalmol 11:1069–1071. https://doi.org/10.2147/OPTH.S137227
Muni RH, Francisconi CLM, Felfeli T, Mak MYK, Berger AR, Wong DT, Altomare F, Giavedoni LR, Kohly RP, Kertes PJ, Figueiredo N, Zuo F, Thorpe KE, Hillier RJ (2020) Vision-related functioning in patients undergoing pneumatic retinopexy vs vitrectomy for primary rhegmatogenous retinal detachment: a post hoc exploratory analysis of the PIVOT randomized clinical trial. JAMA Ophthalmol 138:826–833. https://doi.org/10.1001/jamaophthalmol.2020.2007
Weng CY (2020) Vision-related function following retinal detachment repair-looking beyond the letter chart. JAMA Ophthalmol 138:833–834. https://doi.org/10.1001/jamaophthalmol.2020.2023
Shiragami C, Shiraga F, Yamaji H, Fukuda K, Takagishi M, Morita M, Kishikami T (2010) Unintentional displacement of the retina after standard vitrectomy for rhegmatogenous retinal detachment. Ophthalmology 117(86–92):e81. https://doi.org/10.1016/j.ophtha.2009.06.025
Brosh K, Francisconi CLM, Qian J, Sabatino F, Juncal VR, Hillier RJ, Chaudhary V, Berger AR, Giavedoni LR, Wong DT, Altomare F, Kadhim MR, Newsom RB, Marafon SB, Muni RH (2020) Retinal displacement following pneumatic retinopexy vs pars plana vitrectomy for rhegmatogenous retinal detachment. JAMA Ophthalmol. https://doi.org/10.1001/jamaophthalmol.2020.1046
Muni RH, Felfeli T, Sadda SR, Juncal VR, Francisconi CLM, Nittala MG, Lindenberg S, Gunnemann F, Berger AR, Wong DT, Altomare F, Giavedoni LR, Kohly RP, Kertes PJ, Sarraf D, Hillier RJ (2021) Postoperative photoreceptor integrity following pneumatic retinopexy vs pars plana vitrectomy for retinal detachment repair: a post hoc optical coherence tomography analysis from the pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial. JAMA Ophthalmol 139:620–627. https://doi.org/10.1001/jamaophthalmol.2021.0803
Wu L, Flikier D (2006) Corneal graft dehiscence during pneumatic retinopexy. Retina 26:707. https://doi.org/10.1097/01.iae.0000220487.69420.07
Yam JC, Liu DT, Lee VY, Lam PT, Lam DS (2008) Giant retinal tear after pneumatic retinopexy. Acta Ophthalmol 86:232–233. https://doi.org/10.1111/j.1600-0420.2007.01027.x
Sinkar SN, Simon SJ, Gilhotra JS (2012) Giant retinal tear after pneumatic retinopexy. Retin Cases Brief Rep 6:151–152. https://doi.org/10.1097/ICB.0b013e318216460a
Lee HN, Lin KH, Tsai HY, Shen YC, Wang CY, Wu R (2014) Aniseikonia following pneumatic retinopexy for rhegmatogenous retinal detachment. Am J Ophthalmol 158:1056–1061. https://doi.org/10.1016/j.ajo.2014.08.005
Elhusseiny AM, Yannuzzi NA, Smiddy WE (2019) Cost Analysis of pneumatic retinopexy versus pars plana vitrectomy for rhegmatogenous retinal detachment. Ophthalmol Retina 3:956–961. https://doi.org/10.1016/j.oret.2019.06.003
Chang JS, Smiddy WE (2014) Cost-effectiveness of retinal detachment repair. Ophthalmology 121:946–951. https://doi.org/10.1016/j.ophtha.2013.11.003
Chronopoulos A, Hattenbach LO, Schutz JS (2020) Pneumatic retinopexy: a critical reappraisal. Surv Ophthalmol. https://doi.org/10.1016/j.survophthal.2020.12.007
Yorston D (2021) Do we really need more clinical trials of pneumatic retinopexy? JAMA Ophthalmol Published online June 17, 2021. https://doi.org/10.1001/jamaophthalmol.2021.1850
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
Lihteh Wu has received speaker honoraria from Bayer, Roche, and Quantel Medical. Mia Mikowski and Chyong-Yng Huang declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, CY., Mikowski, M. & Wu, L. Pneumatic retinopexy: an update. Graefes Arch Clin Exp Ophthalmol 260, 711–722 (2022). https://doi.org/10.1007/s00417-021-05448-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05448-x