Abstract
Purpose
To compare the incidence rate of delayed retinal break or detachment after diagnosis of acute, symptomatic posterior vitreous detachment (PVD) in a resident-run urgent care clinic (UCC) when staffed by a retina attending, non-retina ophthalmology attending, optometrist, or ophthalmology resident only.
Methods
Retrospective consecutive case series. Of the 594 patients with acute, symptomatic PVD evaluated in the UCC at Penn State Eye Center between 1/1/2016 and 10/10/2019, 454 were included in the study; 140 were excluded because they were diagnosed with a retinal break or detachment on presentation to the UCC, had media opacity precluding examination, or had no follow-up within one year. Demographics, presenting examination findings, and type of staffing were recorded; subsequent visits up to 1 year were analyzed for presence of delayed retinal break or detachment.
Results
Among 491 eyes of 454 patients with a mean follow-up of 147 days, ten delayed breaks (10/491, 2.0%) and three delayed detachments (3/491, 0.6%) were discovered. Incidence rates of delayed breaks and detachments were 1.8% (5/282) and 0.7% (2/282), respectively, in the retina attending group, 1.0% (1/105) and 1.0% (1/105) in the non-retina ophthalmology attending group, 4.7% (3/64) and 0% (0/64) in the optometrist group, and 2.5% (1/40) and 0% (0/40) in the ophthalmology resident only group. There was no statistically significant difference in the incidence of delayed break or detachment among the staffing groups (P = 0.7312), but this study was underpowered to detect a statistically significant difference among staffing groups. Patients with a delayed break or detachment were more likely to have lattice degeneration (P = 0.0265) or a history of retinal break in the contralateral eye (P = 0.0014), and most eyes (10 [76.9%]) with a delayed break or detachment were left eyes (P = 0.0466).
Conclusions
The overall rate of delayed retinal break or detachment in the current study is similar to previously published rates among retinal physician and retinal fellow examiners. Although no statistically significant difference among staffing groups in the incidence rates of delayed retinal tears or detachments was identified in the study, it is important to note that the optometry and ophthalmology resident only groups had higher incidence rates of delayed retinal breaks than did the retina and non-retina ophthalmology attending groups, and this may be clinically important. Larger cohort studies would be needed in order to have the power to detect statistically significant differences among staffing groups. Varied staffing for acute, symptomatic PVD may assist with resource allocation in similar settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
Posterior vitreous detachment (PVD) is an age-related process defined as the separation between the posterior vitreous cortex and the internal limiting membrane [1]. Patients with symptomatic PVD typically present with photopsias and/or floaters. During PVD development, persistent vitreoretinal traction can lead to formation of retinal breaks and may predispose the patient to retinal detachment if left untreated [2]. In the USA, patients with acute, symptomatic PVD typically undergo dilated funduscopic evaluation with extended binocular indirect ophthalmoscopy including scleral depression at the presenting and follow-up visits. Approximately 8–22% of patients with acute, symptomatic PVD present with a retinal break on initial examination [2,3,4,5]. The incidence of delayed retinal breaks following the initial PVD examination has been reported to be approximately 2–5%, with follow-up ranging from 6 weeks to over 1 year [3, 5,6,7,8,9,10,11,12,13]. A cost-utility decision analysis model which compared a 1-visit versus 2-visit examination schedule for patients who present with acute, symptomatic PVD demonstrated that when considering the cost of scleral buckle for patients expected to develop delayed retinal detachment (based on previously published incidence rates) and the cost of laser retinopexy for delayed discovery of a retinal tear missed initially, there is a significant benefit of a 2-visit examination schedule [14].
Frequency of follow-up visits is based on the patient’s risk factors for retinal tear or detachment, and may include at least one follow-up visit within 2 months for symptomatic PVD patients without other significant risk factors for retinal breaks or detachments [5, 7, 13]. Reported risk factors associated with the presence or development of retinal breaks or detachments include presence of pigmented cells in the anterior vitreous, history of phacoemulsification in the affected eye, vitreous hemorrhage, lattice degeneration, high myopia, trauma, and the presence of ten or more floaters on initial presentation or follow-up [5, 15,16,17]. Vitreous hemorrhage and male gender were reported to be significantly associated with a higher incidence of delayed retinal breaks following diagnosis of acute, symptomatic PVD in one study [3].
PVD formation is insidious and observational studies have demonstrated that this process occurs over decades [1, 18, 19]. There may still be ongoing vitreous traction past the commonly used 6-week follow-up period [1, 3, 13, 19]. A large retrospective study by Uhr et al. found that a significant proportion of delayed retinal breaks (44.5% of all delayed retinal breaks) and detachments (67.5% of all delayed retinal detachments) are identified more than 6 weeks following presentation with acute, symptomatic PVD [3].
In previous studies investigating the incidence of delayed retinal breaks or detachments, examinations of patients who present with acute, symptomatic PVD are performed by retina attendings or retina fellows; this scenario does not necessarily reflect all academic settings or clinics in which residents examine patients independently or staff patients presenting with PVD with attendings of various subspecialties. A 2019 study including 105 patients investigated the incidence of delayed retinal breaks in a resident-run clinic over one year, but did not record a single case of a delayed retinal break or detachment [4]. In a recent study of 228 patients with acute onset of PVD symptoms who were examined by junior ophthalmology residents on call, a 5.3% (13/246) rate of delayed retinal break was reported [20]. Our study aims to examine a larger cohort of patients and to investigate the association of staffing type in a resident-run urgent care clinic (UCC) with the incidence rates of delayed retinal break and delayed retinal detachment.
Methods
The Penn State University Institutional Review Board deemed this study exempt from review and waived the requirement for informed consent by participants. Electronic health records of all patients evaluated in the Penn State Eye Center UCC with a primary diagnosis of PVD including ICD-10 codes H43.811, H43.812, H43.813, and H43.819 from January 1, 2016, to October 10, 2019, were reviewed. The UCC is a resident-run clinic in the Penn State Eye Center staffed by various ophthalmology subspecialist attendings and optometrists. Patients with a retinal tear or detachment on presentation, with a media opacity precluding thorough peripheral retinal examination, or without a follow-up dilated funduscopic examination within 1 year of presentation were excluded. Patients with atrophic retinal holes on initial examination were included in the study; patients with any other type of retinal break discovered on initial examination were excluded.
The following parameters from each patient were recorded: age, gender, ethnicity, ocular symptoms such as the presence of floaters or flashes of light, laterality of eye with symptoms, history of head trauma, history of a previous retinal break, history of myopia, history of cataract extraction within the past year, history of YAG capsulotomy within the past year, and lens status (phakic, pseudophakic, aphakic) in the affected eye. Ocular examination findings on the initial UCC examination were documented, including the presence or absence of Shafer sign (pigmented cells in the vitreous), associated intraretinal or vitreous hemorrhage, lattice degeneration, vitreoretinal tufts, meridional folds, and atrophic retinal holes.
The type of provider (retina attending, non-retina ophthalmology attending, optometrist, or ophthalmology resident only) who staffed the initial and follow-up visits was recorded. The medical records were reviewed of the presenting examination and of all follow-up examinations through 1 year following the date of presentation with acute PVD in order to identify whether a delayed retinal break or detachment occurred. Patients who presented with a delayed retinal detachment were not also included in the delayed retinal break group. The total length of follow-up, up to the 1-year appointment, was recorded.
Comparisons among the different staffing groups (based on the type of staffing during the patients’ presenting visits in the UCC), and between patients with delayed retinal breaks or detachments versus those without delayed retinal breaks or detachments, were assessed using the Chi-square test for categorical variables and analysis of variance for continuous variables. Log-rank test was performed for comparison of survival time-to-events. For all analyses, a P-value < 0.05 was considered statistically significant. The aforementioned statistical analyses were performed using R software (version 4.0.0, The R Foundation, http://www.r-project.org) with package survival (version 3.1–12).
Results
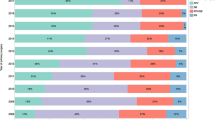
A total of 491 eyes (247 right eyes, 244 left eyes) from 454 patients were included in the study. Demographic and baseline characteristics of the study population are summarized in Table 1. The average age of the patients at presentation was 64.2 years (range: 20–94 years); 295 (65.0%) patients were women and 407 (89.6%) self-identified as white. There were no statistically significant differences in the baseline characteristics among the different staffing groups (all P > 0.1; Table 2). The most common presenting symptoms were floaters (421 eyes, 85.7%) and flashes (321 eyes, 65.4%) (Table 1). Patients who developed a delayed retinal break or detachment were more likely to have lattice degeneration or a history of retinal break in the contralateral eye than those who did not develop a delayed break or detachment (P = 0.0265; P = 0.0014, respectively, Table 1). A significantly higher proportion of delayed retinal breaks or detachments was observed in left eyes (10/13, 76.9%) than in right eyes (3/13, 23.1%) (P = 0.0466, Table 1).
The average follow-up duration was 147.4 days; 452 (92.1%) eyes had follow-up for at least 4 weeks, 384 (78.2%) for at least 6 weeks, and 170 (34.6%) for at least 6 months. There was no significant difference among the staffing groups with respect to follow-up duration (P = 0.2389; Table 2).
Ten delayed retinal breaks and three delayed retinal detachments were identified, yielding an incidence rate of 2.0% for delayed retinal break and 0.6% for delayed retinal detachment in our cohort (Table 3). There was no case in which two delayed retinal breaks were noted in the same eye. There was one patient who presented with a delayed retinal break in the right eye and a delayed retinal break in the left eye; they were counted as two separate delayed retinal breaks in the analysis. Data regarding the type of delayed break identified and the staffing of the initial examination are provided in Table 4. The incidence rates of delayed retinal break and detachment were 1.8% (5/282) and 0.7% (2/282), respectively, in the retina attending group, 1.0% (1/105) and 1.0% (1/105) in the non-retina ophthalmology attending group, 4.7% (3/64) and 0% (0/64) in the optometrist group, and 2.5% (1/40) and 0% (0/40) in the resident only group (Table 3). There was no statistically significant difference in the incidence rate of delayed retinal break or detachment among the different staffing groups (P = 0.7312; Table 3).
The mean duration between presenting examination to identification of a delayed retinal break was 76.8 days (range: 7–322 days) and the mean duration between presenting examination to identification of a retinal detachment was 8.7 days (range: 7–11 days). The mean duration between initial examination to discovery of a delayed retinal break or detachment did not differ significantly among the staffing groups (P = 0.7047). Seven of the ten delayed breaks (70%) and all of the delayed retinal detachments were found within 6 weeks of the initial examination; the remaining three out of ten delayed retinal breaks were discovered at 98 (round hole), 150 (slit tear), and 322 (operculated hole) days after the initial examination.
Of the patients who underwent YAG capsulotomy within 1 year of presentation with PVD, the mean duration between the YAG capsulotomy and the initial PVD exam was 67 days (range: 2–214 days; Table 1). Of the patients with recent phacoemulsification who subsequently developed PVD, the mean duration between phacoemulsification and the initial PVD exam was 118.7 days (range: 2–386 days; Table 1). None of the patients with a delayed retinal break or detachment underwent phacoemulsification or YAG capsulotomy within 1 year of presentation with acute PVD.
Discussion
To our knowledge, and based on a computerized search of the PubMed literature database, this is the largest study to investigate the incidence of delayed retinal break or detachment among different types of providers (retina attendings, non-retina ophthalmology attendings, optometrists, and ophthalmology residents) who staffed the initial examination of patients who presented with acute, symptomatic PVD. We report an overall incidence of delayed retinal break of 2.0% and of delayed retinal detachment of 0.6%; these rates are comparable to other studies which reported an incidence of 2–5% for delayed retinal break and an incidence of about 1% for delayed retinal detachment [3, 5,6,7,8,9,10,11,12,13]. Our study did not identify a statistically significant difference in the incidence of delayed retinal break or detachment among the different staffing groups (P = 0.7312; Table 3), although the power of the comparisons is limited by sample size.
Three (30%) of the delayed retinal breaks were noted more than 6 weeks after presentation in two patients with acute symptomatic PVD (round hole at 98 days, slit tear at 150 days, and operculated hole at 322 days); the remaining delayed retinal breaks (70%) and all three retinal detachments (100%) were discovered within 6 weeks of presentation with acute PVD. One patient was found to have two delayed breaks discovered past 6 weeks: a delayed round hole in the right eye at 98 days and a delayed retinal tear in the left eye at 150 days during the same visit for follow-up of bilateral PVD; she underwent laser barricade for both breaks. Another patient was noted to have an operculated hole at 322 days. Both of these patients with delayed breaks past 6 weeks were female and had a history of myopia. The first patient with a round hole and slit tear was also noted to have lattice degeneration on her initial examination. Neither of these patients had any other known risk factors for retinal break or detachment, and both patients had undergone several dilated fundus examinations with scleral depression prior to the discovery of the delayed retinal break(s).
Although there was not a statistically significant difference in time from initial examination to discovery of a delayed retinal break among the staffing groups, the average time from initial examination to discovery of a delayed break was approximately two to four times larger in the retina attending or non-retina ophthalmology attending groups compared to the optometry attending or resident groups (Table 3). This may suggest that the delayed breaks discovered in the retina attending and non-retina ophthalmology attending groups were more likely new onset breaks rather than missed retinal breaks on the initial examination.
In our study, lattice degeneration was present in a significantly higher proportion of eyes with a delayed retinal break or detachment (30.8%) than in eyes without a delayed retinal break or detachment (8.8%) (P = 0.0265, Table 1). Although lattice degeneration has not been previously associated with formation of delayed breaks or detachments in other studies investigating delayed retinal breaks [3], lattice degeneration has been associated with the presence of a rhegmatogenous retinal detachment, especially in the setting of an acute PVD [21]. Retinal breaks associated with lattice degeneration typically occur at the ends or posterior margins of the lattice lesions, and may result from increased vitreoretinal traction during PVD formation [22].
Our data also demonstrate that a history of a retinal break in the fellow eye was significantly associated with the development of a delayed retinal break or detachment (P = 0.0014, Table 1). Patients with a history of rhegmatogenous detachment in one eye have been shown to have an increased risk of retinal detachment in the fellow eye [23]. Similarly, patients with a history of retinal break in the fellow eye may have a predisposition to formation of a new retinal break or detachment.
Although the proportion of right and left eyes with acute, symptomatic PVD included in our study was approximately equal, a significantly higher proportion of delayed retinal breaks or detachments was observed in left eyes (10/13, 76.1%) than in right eyes (3/13, 23.1%) (P = 0.0466, Table 1). While this may represent a spurious finding due to chance, this might also be because the typical configuration of an eye examination lane for a right-handed eye care provider has the provider’s chair and indirect ophthalmoscope to the patient’s right side so that when binocular indirect funduscopic examination with scleral depression is performed, the examiner’s view may extend further to the nasal periphery for right eyes than left eyes unless the examiner, instead of remaining on the patient’s right side and leaning over the patient to obtain a view to the far nasal periphery in each eye, performs a peripheral retinal examination from both sides of the patient. None of the previously published studies of delayed retinal breaks and detachments consistently reports the laterality of the eyes with delayed retinal break or detachment.
A larger proportion of female (65.0%) compared to male patients (35.0%) was noted among the patients who presented with acute, symptomatic PVD. This phenomenon has been noted in several studies of patients with symptomatic PVDs [7,8,9, 24, 25]. Observational studies using optical coherence tomography (OCT) have demonstrated more rapid PVD progression in female patients compared to age-matched male patients past 60 years of age, and this may explain, at least in part, why women have a higher prevalence of idiopathic macular holes and symptomatic PVD due to vitreoretinal traction [26].
Our study has several limitations. Due to the retrospective nature of this study, data for some variables examined are incomplete. For example, the degree of myopia was not specified in the medical records of all patients, and the presence or absence of Shafer sign was not recorded in all notes. The presence of myopia was based on documentation by the eye care providers who examined the patients (there was no specific study definition for myopia). As there was inconsistent documentation of patients’ refractive correction, it was not possible to determine how many patients had mild, moderate, or high myopia. Further, 107 (21.8%) eyes in our study were followed for less than 6 weeks and this may have led to an underreporting of delayed retinal breaks or detachments; however, the majority of delayed retinal breaks (7/10, 70%) and all of the delayed retinal detachments (3/3, 100%) in our study were discovered before 6 weeks and the proportion of eyes in our study followed for longer than 6 weeks (384/491, 78.2%) is higher than that reported in other studies investigating the incidence of delayed retinal breaks or detachments, with most studies having no follow-up past 6 weeks [3, 6, 10]. Our study included a review of follow-up examinations up to the 1 year visit after presentation with acute PVD, and previous studies demonstrated that almost all delayed retinal breaks or detachments were detected within 1 year (90th percentile of one large-scale study was 307 days) [3, 6,7,8,9,10,11,12,13]. Another potential limitation of this retrospective study is the lack of a standard follow-up protocol among various attendings throughout the study. However, the impact of this potential study limitation on the study results is expected to be small for two reasons: (1) it is standard protocol in the Penn State Eye Center UCC for patients diagnosed with acute, symptomatic PVD to be scheduled for a follow-up examination 4–6 weeks after the presenting examination (beyond this 4–6 week examination, follow-up among attendings may vary); and (2) the majority of delayed retinal breaks (7/10, 70%) and all of the delayed retinal detachments (3/3, 100%) in our study were discovered before 6 weeks. Another study limitation is that our data are derived from a single clinic within an academic institution which may limit the generalizability of our results. We serve a predominantly Caucasian population, as noted in Table 1, and this may not reflect the patient demographics in other regions of the United States. Further, the sample size in each staffing group limits the power of this study to detect statistically significant differences among the groups. For example, based on calculations performed using nQuery + nTerim 4.0 software using a set alpha value of 0.05 and beta value of 0.20, and assuming a two sided Chi-squared test and excluding patients who had a prior tear, a total of 4,854 eye examinations would be required to detect a statistically significant difference in incidence rates of delayed retinal break between experienced ophthalmologists (retina attendings and non-retina ophthalmology attendings) versus less experienced ophthalmologists (residents) and optometrists. Thus, although no statistically significant difference among staffing groups was identified in this study, it is important to note that the optometry (4.7%) and resident (2.5%) groups had a higher overall incidence rate of delayed retinal breaks than the retina (1.8%) and non-retina ophthalmology (1.0%) attending groups, and this may be clinically important. Larger cohort studies would be needed in order to have the power to detect statistically significant differences among staffing groups. Finally, resident comfort level with examination of the peripheral retina likely differs by training level. Most (36/40, 90%) of the resident-only examinations in the current study were performed by residents in their PGY3 year; the patient with a delayed retinal break (operculated hole) in the resident only group was examined by a PGY3 resident. Our study demonstrates a delayed retinal tear rate among ophthalmology residents (2.5%) comparable to previously published rates which included retinal physicians and retinal fellows (2–5%) [3, 5,6,7,8,9,10,11,12,13, 20].
Our study results do not demonstrate a statistically significant difference in incidence rates of delayed retinal breaks or detachments among retina attendings, non-retina ophthalmology attendings, optometrist attendings, or ophthalmology residents. However, the optometrist and ophthalmology resident only groups had higher incidence rates of delayed retinal breaks than did the retina and non-retina ophthalmology attending groups, and this may be clinically important. Patients with lattice degeneration or a history of retinal break in the fellow eye were at higher risk of delayed retinal break or detachment, and most delayed breaks or detachment occurred in left eyes. Future larger studies are warranted and may elucidate other associated risk factors.
Availability of data and material
All data generated or analyzed during this study are included in this article.
Code availability
Not applicable.
References
Johnson MK (2012) Posterior vitreous detachment: evolution and role in macular disease. Retina 32(8):S174–S178
Davis MD (1974) Natural history of retinal breaks without detachment. Arch Ophthalmol 92(3):183–194
Uhr JH, Obeid A, Wibbelsman TD et al (2020) Delayed retinal breaks and detachments after acute posterior vitreous detachment. Ophthalmology 127:516–522
Nassrallah G, Kondoff M, Ross M et al (2019) Posterior vitreous detachment and incidence of delayed retinal breaks: a retrospective, 2-year study at an academic centre. Can J Ophthalmol 54(4):509–512
Flaxel CJ, Adelman RA, Bailey ST et al (2020) Posterior vitreous detachment, retinal breaks, and lattice degeneration preferred practice pattern®. Ophthalmology 127(1):146–181
Coffee RE, Westfall AC, Davis GH et al (2007) Symptomatic posterior vitreous detachment and the incidence of delayed retinal breaks: case series and meta-analysis. Am J Ophthalmol 144:409–413
Dayan MR, Jayamanne DG, Andrews RM et al (1996) Flashes and floaters as predictors of vitreoretinal pathology: is follow up necessary for posterior vitreous detachment? Eye 10(4):456–458
Linder B (1984) Acute posterior detachment and its retinal complications: a clinical biomicroscopic study. Am J Ophthalmol 87:S1–S108
Tasman W (1968) Posterior vitreous detachment and peripheral retinal breaks. Trans Am Acad Ophthalmol Otolaryngol 72(2):217–224
Byer NE (1994) Natural history of posterior vitreous detachment with early management as the premier line of defense against detachment. Ophthalmology 101(9):1503–1513
Jaffe NS (1968) Complications of acute posterior vitreous detachment. Arch Ophthalmol 79(5):568–571
Kanski JJ (1975) Complications of acute posterior vitreous detachment. Am J Ophthalmol 80(1):44–46
Richardson PS, Benson MT (1999) Kirkby GR (1999) The posterior vitreous detachment clinic: do new retinal breaks develop in six weeks following an isolated symptomatic posterior vitreous detachment? Eye 13(2):237–240
Yannuzzi NA, Chang JS, Brown GC et al (2018) Cost-utility of evaluation for posterior vitreous detachment and prophylaxis of retinal detachment. Ophthalmology 125(1):43–50
Brod RD, Lightman DA, Packer AJ et al (1991) Correlation between vitreous pigment granules and retinal breaks in eyes with acute posterior vitreous detachment. Ophthalmology 98(9):1366–1369
Karahan E, Karti O, Er D et al (2018) Risk factors for multiple retinal tears in patients with acute posterior vitreous detachment. Int Ophthalmol 38:257–263
Gishti O, van den Nieuwenhof R, Verhoekx J et al (2019) Symptoms related to posterior vitreous detachment and the risk of developing retinal tears: a systematic review. Acta Ophthalmol 97(4):347–352
Uchino E, Uemara A, Ohba N (2001) Initial stages of posterior vitreous detachment in healthy eyes of older persons evaluated by optical coherence tomography. Arch Ophthalmol 119:1475–1479
Tsukahara M, Mori K, Gehlbach PL et al (2018) Posterior vitreous detachment as observed by wide-angle OCT imaging. Ophthalmology 125:1372–1383
Jarocki A, Durrani A, Zhou Y et al (2021) On-call exams for acute onset of flashes, floaters, or curtain by junior ophthalmology residents: outcomes, safety, and resource utilization. Ophthalmology Retina 5(4):330–336
Byer NE (1992) Rethinking prophylactic therapy of retinal detachment. In: Stirpe M (ed) Advances in Vitreoretinal Surgery. Ophthalmic Communications Society, New York, pp 399–411
Byer NE (1979) Lattice degeneration of the retina. Surv Ophthalmol 23(4):213–248
Sharma MC, Chan P, Kim RU et al (2003) Rhegmatogenous retinal detachment in the fellow phakic eyes of patients with pseudophakic rhegmatogenous retinal detachment. Retina 23(1):37–40
Hayreh SS, Jonas JB (2004) Posterior vitreous detachment: Clinical correlations. Ophthalmologica 218(5):333–343
Chuo JY, Lee TYY, Hollands H et al (2006) Risk factors for posterior vitreous detachment: a case-control study. Am J Ophthalmol 142(6):931–937
Hayashi K, Sato T, Manabe S-I et al (2019) Sex-related differences in the progression of posterior vitreous detachment with age. Ophthalmol Retina 3(3):237–243
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was deemed exempt from further review by the Penn State College of Medicine Institutional Review Board.
Conflict of interest
Dr. Scott serves as Principal Investigator and Chair of the Study of COmparative Treatments in REtinal Vein Occlusion 2 (SCORE2) trial, which is funded by the National Eye Institute, has served as a consultant for Regeneron, and has served on the Data and Safety Monitoring Committee for clinical trials sponsored by Novartis (these disclosures are unrelated to the present work). None of the other authors report any financial disclosures or financial conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, S.N., Lee, C., Cui, D. et al. Association of staffing with Incidence of delayed retinal break or detachment after posterior vitreous detachment in a resident urgent care clinic. Graefes Arch Clin Exp Ophthalmol 260, 791–798 (2022). https://doi.org/10.1007/s00417-021-05437-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05437-0