Abstract
Purpose
To investigate how the central visual field would be changed after fornix-based trabeculectomy with mitomycin C in Japanese normal-tension glaucoma (NTG) patients monitored for more than 10 years including before surgery.
Methods
This is a retrospective cohort study. We identified twenty-eight eyes of 28 NTG cases regularly monitored for more than 5 years and examined static visual field (VF) tests for more than five times before and after fornix-based trabeculectomy (including combined surgery). Based on preoperative data for 6.3 years, we evaluated postoperative changes for 6.0 years in 10–2 VF and 30–2 VF.
Results
Six patients were male and 22 females, the mean age was 57.9 years, and the mean deviation was − 13.7 decibels. After surgery, mean IOP decreased from 13.9 to 9.0 mmHg (P ≤ 0.01), and medication score also did. The rate of 10–2 VF deterioration was significantly suppressed from − 1.0 dB/year preoperatively to − 0.4 dB/year postoperatively (P ≤ 0.01). And when 30–2 VF was divided into six relevant sectors, the rate of deterioration at cecocentral and arcuate areas of the superior hemifield was suppressed postoperatively (P ≤ 0.01 and P = 0.042, respectively).
Conclusion
Based on long-term preoperative data, a significant positive change in 10–2 VF was observed after fornix-based trabeculectomy with mitomycin C in Japanese NTG patients with a mean IOP of 13.9 mmHg. Central vision could be expected to be maintained for NTG patients even if its preoperative IOP is low after successful trabeculectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Normal-tension glaucoma (NTG) is the most common type of primary open-angle glaucoma (POAG); its prevalence is reported to be approximately 3.6%, and it accounts for 70% of glaucoma cases in Japan [1]. Although factors independent of intraocular pressure (IOP) are thought to be associated with the occurrence and progression of NTG [2], the main strategy to maintain the visual field (VF) in NTG is to reduce IOP by 30% from the baseline value [3]. With a reduction in IOP of less than 30%, it is more likely that the optic disk and/or visual field (VF) will not be maintained. The rate of VF deterioration in NTG is reported to be generally slow. Studies of medicated NTG patients have found the rate to be in the range of − 0.3 to − 0.8 dB/year [4,5,6,7,8,9,10], irrespective of the study design. Prospective follow-up studies of untreated NTG patients have reported the following rates of deterioration: − 0.41 dB/year in the Collaborative Normal Tension Glaucoma Study (CNTGS) [11], − 0.36 dB/year in the Early Manifest Glaucoma Trial (EMGT) [12], and − 0.33 dB/year in a study of Japanese NTG patients with lower than average IOP [13].
In cases where glaucoma progresses despite the maximal possible use of medical treatment, glaucoma surgery is generally selected, especially when there is significant central VF deterioration. Among the many surgical options for glaucoma, trabeculectomy with an antimetabolite such as mitomycin C (MMC) is one of the most reliable and powerful techniques for reducing IOP. In fact, studies indicate that IOP can be safely reduced to below 10 mmHg with this technique [14, 15]. Some studies have reported that trabeculectomy in NTG has led to a sufficient decrease in IOP to significantly reduce the speed of VF deterioration [16,17,18,19]. However, unfortunately, appropriate progression assessment at 10–2 VF has never been done before.
Thinking of local patterns of visual impairment, NTG patients are reportedly more susceptible to visual impairment near the fixation point and more prone to a deep decrease in sensitivity than high-tension glaucoma (HTG) patients [20]. There is little possibility of overlooking abnormal points because 30–2 VF program has few measurement points in the central visual field, while 10–2 VF program has as many as 68 points.
Further, the surgical methods, surgeon, and use of antimetabolites were not always consistent within previous studies, and not all included reliable long-term preoperative IOP and VF data. This makes it difficult to accurately calculate postoperative changes, especially in the VF. Against this background, we especially focused on cases that were followed-up for more than 5 years before and after initial fornix-based trabeculectomy with MMC by a single surgeon. This time, we evaluated the deterioration rate of central VF (10–2 VF) mainly and 30–2 VF the same as similar previous reports.
Materials and methods
In this cohort study, we retrospectively reviewed the medical records of Japanese NTG patients who underwent initial fornix-based trabeculectomy with MMC between January 2011 and December 2013 at the Yotsuya Shirato Eye Clinic (Tokyo, Japan). This study was performed according to the tenets of the Declaration of Helsinki, and Institutional Review Board (IRB) approval was provided by the Riverside Internal Medicine Cardiology Clinic (approval ID: RSC-1811RB01) in advance of the study. Since there was no ethics committee in this clinic, we asked an external organization to examine. Given the retrospective nature of this study, the requirement for informed consent was waived by the Research Ethics Board.
Patient
Inclusion criteria were as follows: age < 80 years old, a diagnosis of NTG according to a standardized set of criteria, as specified below*; follow-up for ≥ 5 years before and after trabeculectomy; fornix-based trabeculectomy performed by a single well-trained surgeon (SS); either a single or triple procedure performed; VF tests performed at least five times (once a year) before and after surgery, using a Humphrey visual field analyzer (Carl Zeiss Meditec, Jena, Germany) according to the standard 30–2 and 10–2 programs of the Swedish Interactive Threshold Algorithm (SITA) with reliability indices of the VF test as follows: fixation < 20%, false-positive rate < 15%, and false-negative rate < 15%; no systemic use of calcium-channel blockers or β-blockers for systemic diseases; no use of oral acetazolamide during follow-up; no history of any incisional or laser surgery pre-operatively or during follow-up; and no severe cataracts that might affect visual field test during the course.
*The diagnostic criteria for NTG were as follows: glaucomatous optic neuropathy and corresponding VF defects as determined by a Humphrey visual field analyzer; IOP by Goldmann applanation tonometry was defined without ocular hypotensive therapy that never exceeded 21 mmHg during the follow-up period, including 24-h fluctuation; a normal open angle on gonioscopy; and the absence of any other ocular or systemic diseases including brain that could cause changes in the optic nerve head and/or VF. The appearance of the optic disk was assessed by direct ophthalmoscopy, stereoscopic observation using a biomicroscope and appropriate lenses, and fundus photography.
Patient population
A total of 352 patients underwent trabeculectomy (with or without combined cataract surgery) during the study period. Of these, 56 were examined VF tests more than five times before and after surgery. Among those 56 patients, only 28 underwent reliable VF tests at least once a year. Thus, twenty-eight eyes of 28 NTG patients were included in this study.
Parameters evaluated pre- and postoperatively
IOP measurements
IOP measurements were performed during slit-lamp and fundus examination with the patient in a sitting position. Topical anesthesia was applied and a calibrated Goldmann applanation tonometer was used to measure IOP. All IOP measurements were performed during office hours by a single ophthalmologist.
Medication score
The medication score was defined as the number of components in the main anti-glaucoma medication.
Visual field deterioration rate (whole field analysis)
Regression analysis of mean deviation (MD) values for the 10–2 and 30–2 VF was used to calculate the overall rate of progression (MD slope: dB/year).
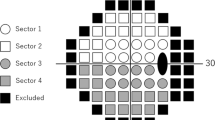
Visual field deterioration rate (sector analysis)
Regression analysis of total deviation (TD) values was performed for six sectors of the visual field. These six subfields consisted of the superior cecocentral field (Sector 1), inferior cecocentral field (Sector 2), superior paracentral field (Sector 3), inferior paracentral field (Sector 4), superior arcuate field (Sector 5), and inferior arcuate field (Sector 6) (Fig. 1). These subdivisions were based on a previous report [21]. Data from left eyes were converted to mirror images to correspond to right eye data for analysis.
Location of test points in each subfield for the right eye. The numbered regions represent the subfields and each square represents a test point. The black areas indicate the blind spot and were not included in analysis. Sector 1 represents superior cecocentral field; Sector 2, inferior cecocentral field; Sector 3, superior paracentral field; Sector 4, inferior paracentral field; Sector 5, superior arcuate field; and Sector 6, inferior arcuate field, respectively
Surgical indication and procedures
The surgery was indicated when the patient’s VF deteriorated even with maximum ophthalmic therapy for the patient. After instillation of local anesthetic into the Sub-Tenon’s space, a 5–6 mm fornix-based conjunctival incision was made along the limbus at the temporal side. Cauterization was then performed, and a single rectangular scleral flap (3 × 3 mm) was created. The area was soaked in 0.05% MMC for 1.5 min, then washout of residual MMC with 100 mL of balanced salt solution (BSS). A sclerocorneal block (vertical 0.5 × horizontal 2 mm) was then excised, followed by peripheral iridectomy, the placement of four 10–0 nylon scleral flap sutures (MANI, Utsunomiya, Japan), the adjustment of aqueous humor flow with an occasional additional suture, and the placement of a wing conjunctival suture. In cases in which the procedure was combined with cataract surgery, a clear corneal incision was made in the superior quadrant and the anterior chamber was filled with viscoelastic material (Viscoat 0.5 Ophthalmic Viscoelastic Substance (Alcon, Tokyo, Japan) and 1% Healon Ophthalmic Viscoelastic Substance (AMO, Tokyo, Japan)). Postoperative treatment after simple trabeculectomy consisted of four applications of 0.1% betamethasone and moxifloxacin ophthalmic solution; for combined surgery, diclofenac sodium ophthalmic solution was also applied. Laser suture lysis or bleb needling was performed at the surgeon’s discretion to increase the flow rate of aqueous humor if IOP was elevated after the surgery.
Analytical methods
The outcome measures were the rate of VF deterioration (dB/year) before and after surgery, mean IOP, and medication score. The IOP data recorded within 6 months after the surgery were excluded from analyses because this period of IOP instability commonly affects the VF. The Wilcoxon signed-rank test was used to compare the pre- and postoperative MD and TD slope values, mean IOP, and medication score. The same analysis was performed for the rate of deterioration of VF, separately for stand-alone and combined surgeries. All statistical analyses were performed using R software (version 3.4.3; The Foundation for Statistical Computing, Vienna, Austria). A two-sided P-value < 0.05 was considered statistically significant.
Results
The demographic data of the enrolled subjects are summarized in Table 1. A total of follow-up period was over 12 years. After initial fornix-based trabeculectomy with MMC, mean IOP significantly decreased from the preoperative value of 13.9 mmHg to 9.0 mmHg (P ≤ 0.01) with a decrease in the number of eye drops. The preoperative deterioration rate in the 10–2 VF of − 1.0 dB/year was significantly reduced to − 0.4 dB/year (Table 2).
The average TD value (dB) by sectorial analysis revealed that sensitivity significantly decreased in Sectors 2, 4, and 6 in the inferior hemifield. On the other hand, there was almost no change in Sectors 1, 3, and 5 in the superior hemifield (Fig. 2). In connection to this, the deterioration rates (dB/year) in Sector 1 and Sector 5 showed a significant decrease postoperatively. In addition, the rate of deterioration in Sector 3 showed a reduction with borderline significance. On the other hand, there were no significant changes in the rate of VF deterioration (i.e., deterioration rate did not slow down) in the inferior hemifield (Sectors 2, 4, and 6) (Fig. 3). The rate of deterioration of VF, separately for stand-alone and combined surgeries, was shown in Table 3. The rate of central visual field progression showed a significant delay even after when the procedure was divided into single and combined surgeries.
From 6 months after the surgery, bleb needling was performed in five eyes and no laser suture lysis was performed. No cases of significant visual acuity loss affected the examination of VF during the treatment.
Discussion
Fornix-based trabeculectomy in NTG patients with a mean IOP of 13.9 mmHg significantly reduced IOP while decreasing medication scores and we revealed that significant suppression of 10–2 VF progression was observed, indicating that this procedure had a positive effect on maintaining central visual function. Although only 28 of the patients were able to be followed up at least 10 years or more during the period, it is not easy to follow the long-term course of many cases in actual practice, as there are some cases in which the patient was transferred to another hospital or the course is unfavorable. For these reasons, it can be said that our cases were valuable to be evaluated as a cohort with stable postoperative observation. There is a report of trabeculectomy for NTG with similar preoperative IOP (≒13 mmHg), but the short preoperative observation period and small population size would be problematic [14, 22]. In addition to this, similar papers published so far are listed (Table 4) [14, 16,17,18,19, 22,23,24,25]. It should be noted that the surgical procedure, the surgeon, and the use of antimetabolites were not always uniform within the studies discussed.
While it is important to assess long-term IOP management, it is also necessary to confirm the resulting effect on visual function. If the effect on visual function is assessed by the speed of VF progression, it is said that an accurate judgment of progress cannot be made unless reliable VF test results (MD values) are collected at least five times [26]. This calculation requires a follow-up period of at least 3 years if the VF test is performed every 6 months. In this regard, one of the novelties of this study is that it included long-term preoperative IOP and VF data for 6.3 years almost as same as postoperative data for 6.0 years.
The long-term change in VF deterioration rate after trabeculectomy is an important issue, because the goal of the operation is to preserve visual function, not to lower IOP. However, to understand the basis of this preservation of function, we will consider the question of whether the reduction in IOP persists for a long period after the surgery. The success rate of trabeculectomy after 10 years has previously been reported as 44% (success in this study was defined as an IOP without treatment < 21 mmHg as well as no visual field loss, disk damage, or need for further surgical intervention) [27]. Other studies considering 15-year data have reported success rates ranging from 42% (success defined as maintaining the IOP < 21 mmHg, or at a 33% reduction from baseline if the preoperative IOP was < 21 mmHg) [28] to 85% (success defined as an IOP < 21 mmHg) [29]. Twenty-year follow-up studies have reported success rates of 57% (success defined as an IOP without treatment < 21 mmHg) [30] and 79% (success defined as an IOP < 21 mmHg) [31]. To maintain VF stability in Japanese NTG patients after trabeculectomy, it has been recommended to aim for a target IOP of 10 mmHg or less, or to lower the IOP by 20% from baseline [32]. Based on this information, the mean IOP of approximately 9 mmHg calculated from 6 years postoperatively in our study could be expected to be sufficient in terms of IOP management.
Maintaining the central VF is important for maintaining visual function. Previously they evaluated the relationship between visual disability and VF measurements in Japanese glaucoma patients [33]. They found that visual disability could be attributed primarily to lessening of retinal sensitivity in the inferior hemifield within 5° of fixation and to the visual acuity of the better eye; a small proportion of visual disability could be explained by visual acuity in the worse eye. Protecting the central VF is a high priority in clinical practice because there is a close relationship between preservation of the central VF and quality of life. Another researcher created a vision-related quality of life prediction system to identify the VF test points most associated with quality of life [34]. They investigated the importance of the integrated VF test points using the random forest method and found that the most important test points were concentrated along the horizontal meridian. Their study also identified VF test points that were particularly important regarding carrying out daily activities. Despite the importance of the central VF in quality of life as mentioned above, few studies have evaluated the 10–2 VF before and after trabeculectomy. This may be due to the small number of reports in which 10–2 VF can be routinely examined before and after surgery. Although it has been reported that central VF progression has been delayed after trabeculectomy [22], it seems that the number of patients included in their study was too small (6 eyes) to evaluate easily.
Some previous studies have reported that VF progression after trabeculectomy was significantly delayed except in the inferior cecocentral field [17, 18], and this is also consistent with our results. The reason for the lack of suppression in the lower VF may be that there is an element in the upper part of the optic disk (corresponding to the lower VF) that is barely dependent on IOP. Regarding our significant observation that VF progression in the inferior hemifield was not delayed despite sufficient IOP reduction, as has also been reported previously [17], further investigation and research is necessary. A potential contributing factor here could be the structural features of the optic nerve head in glaucoma. Since factors associated with the shape of the optic disk and central corneal thickness were reported to affect the superior hemifield defect [35], these parameters should be included in the future research.
One of the limitations of this study was that the number of patients was relatively small in spite of the retrospective nature because we only included cases with reliable VF results that were stably followed up for more than 5 years before and after surgery, that is, a total follow-up period was 10 years or more. In general, it is difficult to obtain stable data after surgery, as there is a lot of instability and transfer or drop out of the hospital. Also, cases that dropped out due to ocular complications raising the need for another intervention were excluded. Therefore, it is not possible to fully judge the extent of visual function preservation after trabeculectomy from our study alone. This should be investigated in future work.
Secondly, the dosage and the application time for MMC are usually individualized based on many factors. Accordingly, a consistently similar application for all eyes, young and old, with and without cataract surgery simply seemed to be unacceptable. However, in the similar studies listed in Table 4, the metabolic antagonists themselves were not standardized and there were multiple surgeons and other uncertainties. In this context, we believe that this retrospective study using a single metabolic antagonist by a single surgeon might include relatively little uncertainty. And lastly, one more important issue is combining data from patients undergoing both trabeculectomy alone and combined with cataract surgery. One may argue that concomitant cataract surgery indicates the presence of some degree of visually significant cataracts which may adversely affect VF indices. As shown in Table 3, when we divided the analysis into single and combined surgeries, both showed delayed progression of central VF deterioration. In the combined surgery, there were no areas where significant progression changes were observed in the sectoral analysis. The postoperative MD slope was calculated from the first postoperative VF (in 6 months after surgery), so the improvement in sensitivity caused by cataract surgery might not affect the slope of the MD slope. Obviously, a combined surgery tends to have less robust IOP reducing effect as compared to trabeculectomy alone. However, the main theme of the present study is not about the function of the bleb or IOP, but rather about the rate of VF progression. Therefore, we did not distinguish between successful and unsuccessful of glaucoma surgery based on postoperative IOP cutoff value or the site of VF deterioration. Originally, we only collected cases that had been followed for 5 years or more after surgery, which basically meant that all cases had a good postoperative course.
In conclusion, based on concrete preoperative data, a significant reduction in VF deterioration rate in the central VF could be obtained after fornix-based trabeculectomy in Japanese NTG patients with a mean IOP of 13.9 mmHg. Considering this result, central vision could be expected to be maintained for NTG patients with low IOP if the patient is managed without major problems after filtration surgery.
References
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S, Kuwayama Y, Mishima HK, Shimizu H, Tomita G, Inoue Y, Kitazawa Y (2004) The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology 111:1641–1648. https://doi.org/10.1016/j.ophtha.2004.03.029
Ernest PJ, Schouten JS, Beckers HJ, Hendrikse F, Prins MH, Webers CA (2013) An evidence-based review of prognostic factors for glaucomatous visual field progression. Ophthalmology 120:512–519. https://doi.org/10.1016/j.ophtha.2012.09.005
No authors listed (1998) Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol 126:487–497. https://doi.org/10.1016/S0002-9394(98)00223-2
Koseki N, Araie M, Yamagami J, Shirato S, Yamamoto S (1999) Effects of oral brovincamine on visual field damage in patients with normal-tension glaucoma with low-normal intraocular pressure. J Glaucoma 8:117–123
Tomita G, Araie M, Kitazawa Y, Tsukahara S (2004) A three-year prospective, randomized and open comparison between latanoprost and timolol in Japanese normal-tension glaucoma patients. Eye (Lond) 18:984–989. https://doi.org/10.1038/sj.eye.6701373
Araie M, Shirato S, Yamazaki Y, Kitazawa Y, Ohashi Y (2010) Visual field loss in patients with normal-tension glaucoma under topical nipradilol or timolol: subgroup and subfield analyses of the nipradilol-timolol study. Jpn J Ophthalmol 54:278–285. https://doi.org/10.1007/s10384-010-0815-z
De Moraes CG, Liebmann JM, Greenfield DS, Gardiner SK, Ritch R, Krupin T (2012) Risk factors for visual field progression in the low-pressure glaucoma treatment study. Am J Ophthalmol 154:702–711. https://doi.org/10.1016/j.ajo.2012.04.015
Sakata R, Aihara M, Murata H, Mayama C, Tomidokoro A, Iwase A, Araie M (2013) Contributing factors for progression of visual field loss in normal-tension glaucoma patients with medical treatment. J Glaucoma 22:250–254. https://doi.org/10.1097/IJG.0b013e31823298fb
Komori S, Ishida K, Yamamoto T (2014) Results of long-term monitoring of normal-tension glaucoma patients receiving medical therapy: results of an 18-year follow-up. Graefes Arch Clin Exp Ophthalmol 252:1963–1970. https://doi.org/10.1007/s00417-014-2767-3
Lee J, Kong M, Kim J, Kee C (2014) Comparison of visual field progression between relatively low and high intraocular pressure groups in normal tension glaucoma patients. J Glaucoma 23:553–560. https://doi.org/10.1097/IJG.0b013e31829484c6
Anderson DR, Drance SM, Schulzer M (2001) Natural history of normal-tension glaucoma. Ophthalmology 108:247–253. https://doi.org/10.1016/S0161-6420(00)00518-2
Heijl A, Bengtsson B, Hyman L, Leske MC (2009) Natural history of open-angle glaucoma. Ophthalmology 116:2271–2276. https://doi.org/10.1016/j.ophtha.2009.06.042
Sakata R, Yoshitomi T, Iwase A, Matsumoto C, Higashide T, Shirakashi M, Aihara M, Sugiyama K, Araie M (2019) Factors associated with progression of Japanese open-angle glaucoma with lower normal intraocular pressure. Ophthalmology 126:1107–1116. https://doi.org/10.1016/j.ophtha.2018.12.029
Iverson SM, Schultz SK, Shi W, Feuer WJ, Greenfield DS (2016) Effectiveness of single-digit IOP targets on decreasing global and localized visual field progression after filtration surgery in eyes with progressive normal-tension glaucoma. J Glaucoma 25:408–414. https://doi.org/10.1097/ijg.0000000000000240
Schultz SK, Iverson SM, Shi W, Greenfield DS (2016) Safety and efficacy of achieving single-digit intraocular pressure targets with filtration surgery in eyes with progressive normal-tension glaucoma. J Glaucoma 25:217–222. https://doi.org/10.1097/ijg.0000000000000145
Koseki N, Araie M, Shirato S, Yamamoto S (1997) Effect of trabeculectomy on visual field performance in central 30 degrees field in progressive normal-tension glaucoma. Ophthalmology 104:197–201. https://doi.org/10.1016/S0161-6420(97)30334-0
Shigeeda T, Tomidokoro A, Araie M, Koseki N, Yamamoto S (2002) Long-term follow-up of visual field progression after trabeculectomy in progressive normal-tension glaucoma. Ophthalmology 109:766–770. https://doi.org/10.1016/S0161-6420(01)01009-0
Mataki N, Murata H, Sawada A, Yamamoto T, Shigeeda T, Araie M (2014) Visual field progressive rate in normal tension glaucoma before and after trabeculectomy: a subfield-based analysis. Asia Pac J Ophthalmol (Phila) 3:263–266. https://doi.org/10.1097/apo.0000000000000020
Daugeliene L, Yamamoto T, Kitazawa Y (1998) Effect of trabeculectomy on visual field in progressive normal-tension glaucoma. Jpn J Ophthalmol 42:286–292. https://doi.org/10.1016/S0021-5155(98)00013-6
Koseki N, Araie M, Suzuki Y, Yamagami J (1995) Visual field damage proximal to fixation in normal- and high-tension glaucoma eyes. Jpn J Ophthalmol 39:274–283
Suzuki Y, Araie M, Ohashi Y (1993) Sectorization of the central 30 degrees visual field in glaucoma. Ophthalmology 100:69–75. https://doi.org/10.1016/S0161-6420(93)31691-X
Naito T, Fujiwara M, Miki T, Araki R, Fujiwara A, Shiode Y, Morizane Y, Nagayama M, Shiraga F (2017) Effect of trabeculectomy on visual field progression in Japanese progressive normal-tension glaucoma with intraocular pressure < 15 mmHg. PLoS ONE 12:e0184096. https://doi.org/10.1371/journal.pone.0184096
Folgar FA, de Moraes CG, Prata TS, Teng CC, Tello C, Ritch R, Liebmann JM (2010) Glaucoma surgery decreases the rates of localized and global visual field progression. Am J Ophthalmol 149:258-264.e252. https://doi.org/10.1016/j.ajo.2009.09.010
Bertrand V, Fieuws S, Stalmans I, Zeyen T (2014) Rates of visual field loss before and after trabeculectomy. Acta Ophthalmol 92:116–120. https://doi.org/10.1111/aos.12073
Baril C, Vianna JR, Shuba LM, Rafuse PE, Chauhan BC, Nicolela MT (2017) Rates of glaucomatous visual field change after trabeculectomy. Br J Ophthalmol 101:874–878. https://doi.org/10.1136/bjophthalmol-2016-308948
Chauhan BC, Garway-Heath DF, Goni FJ, Rossetti L, Bengtsson B, Viswanathan AC, Heijl A (2008) Practical recommendations for measuring rates of visual field change in glaucoma. Br J Ophthalmol 92:569–573. https://doi.org/10.1136/bjo.2007.135012
Diestelhorst M, Khalili MA, Krieglstein GK (1998) Trabeculectomy: a retrospective follow-up of 700 eyes. Int Ophthalmol 22:211–220. https://doi.org/10.1023/a:1006238624072
Wilensky JT, Chen TC (1996) Long-term results of trabeculectomy in eyes that were initially successful. Trans Am OphthalmolSoc 94:147–159. https://doi.org/10.1016/s0002-9394(14)70163-1
Molteno AC, Bosma NJ, Kittelson JM (1999) Otago glaucoma surgery outcome study: long-term results of trabeculectomy—1976 to 1995. Ophthalmology 106:1742–1750. https://doi.org/10.1016/s0161-6420(99)90351-2
Landers J, Martin K, Sarkies N, Bourne R, Watson P (2012) A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology 119:694–702. https://doi.org/10.1016/j.ophtha.2011.09.043
Bevin TH, Molteno AC, Herbison P (2008) Otago glaucoma surgery outcome study: long-term results of 841 trabeculectomies. Clin Exp Ophthalmol 36:731–737. https://doi.org/10.1111/j.1442-9071.2008.01896.x
Aoyama A, Ishida K, Sawada A, Yamamoto T (2010) Target intraocular pressure for stability of visual field loss progression in normal-tension glaucoma. Jpn J Ophthalmol 54:117–123. https://doi.org/10.1007/s10384-009-0779-z
Sumi I, Shirato S, Matsumoto S, Araie M (2003) The relationship between visual disability and visual field in patients with glaucoma. Ophthalmology 110:332–339. https://doi.org/10.1016/s0161-6420(02)01742-6
Murata H, Hirasawa H, Aoyama Y, Sugisaki K, Araie M, Mayama C, Aihara M, Asaoka R (2013) Identifying areas of the visual field important for quality of life in patients with glaucoma. PLoS ONE 8:e58695. https://doi.org/10.1371/journal.pone.0058695
Iwase A, Araie M (2019) Primary open-angle glaucoma with initial visual field damage in the superior and inferior hemifields: comparison in a population-based setting. J Glaucoma 28:493–497. https://doi.org/10.1097/ijg.0000000000001241
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Riverside Internal Medicine Cardiology Clinic (approval ID: RSC-1811RB01) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Given the retrospective nature of this study, the requirement for informed consent was waived by the Research Ethics Board.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakajima, K., Sakata, R., Ueda, K. et al. Central visual field change after fornix-based trabeculectomy in Japanese normal-tension glaucoma patients managed under 15 mmHg. Graefes Arch Clin Exp Ophthalmol 259, 2309–2316 (2021). https://doi.org/10.1007/s00417-021-05215-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05215-y