Abstract
Purpose
To determine the influence of different lighting conditions on perceived visual function in patients of different age, gender, race, and in various ophthalmic diseases.
Methods
A prospective study. A survey given to patients seen in general ophthalmic and retina clinics. Patients were asked four questions: Is your vision better, worse, or the same in (1) bright light vs dim light, (2) indoors or outdoors, (3) beginning or end of the day, and (4) sunny or cloudy day? Parameters tested were age, race, gender, visual acuity, and a variety of ophthalmic conditions. Multivariable models for each question were fit using multinomial regression. Association was considered significant if p < 0.05.
Results
A total of 722 patients were enrolled in the study. Patients with lower vision (LogMAR ≥ 0.3) were more likely to indicate they either had better vision indoors or outdoors compared with better vision patients (LogMAR < 0.1). Patients with pseudophakia were also more likely to indicate they had better vision on a cloudy day (OR = 1.9). White patients had double the odds of selecting bright light compared with others. Males were less likely than females to indicate better vision indoors (OR = 0.62). There were no significant associations with age-related macular degeneration (AMD) in the multivariable model.
Conclusions
Most patients did not note any difference in lighting conditions, and although there is explanatory rational for some of the findings in this study, those questions concerning lighting conditions or time of day are not useful for screening of disease. Gender and ethnicity were found to have associations with lighting preferences which needs to be further studied.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
There is known effect of ocular disease on the visual acuity and luminance tolerance. Data by Sloan et al showed that the relationship of visual acuity vs luminance has a much higher slope in the normal patient with normal macula and fixation; the greater the luminance, the sharper the visual acuity. When extramacular fixation is tested, the slope is flatter, and those patients need more light to achieve a better visual acuity [1].
When the slope of acuity with changing luminance is studied in patients with significant impairment of foveal vision, the tests measure the function of some relatively normal parafoveal area rather than that of the impaired fovea [2]. Eccentric vision is associated with a smaller rate of change of acuity with increasing luminance. This change is similar to the one observed in the normal para-central retina [2]. As a result, these patients require very high light intensities to obtain their best visual acuity [2].
Contrast sensitivity is also affected by luminance and is important for visual function in various diseases [3,4,5,6,7,8]. The contrast of the target quantifies its relative difference in luminance from the background. It may be specified as the Weber contrast. The contrast sensitivity itself therefore is also a derivative of luminance [9]. Reducing the luminance causes the contrast sensitivity to decrease, although the visual acuity may remain the same [10].
In clinic settings, many patients have extrafoveal fixation and lower contrast sensitivity. We wondered if there was clinical utility in asking patients how their vision was affected by different lighting conditions and time of day. The purpose of this study was to evaluate patients in real-life setting, with regards to light preference using four questions.
Methods
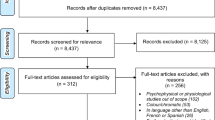
This prospective observational study was conducted at the University of Louisville after approval by the University of Louisville Institutional Review Board. The study adhered to the tenets of the Declaration of Helsinki and complied with Health Insurance Portability and Accountability Act guidelines. Informed consent to participate in the study was obtained from all patients. Patients were recruited at the Kentucky Lions Eye Retina clinic from December 20th, 2014 to November 20th, 2015. The participants completed a voluntary survey consisting of four principle questions: (1) Do you see better in (a) bright light, (b) dim light, (c) no difference; (2) Do you see better in (a) indoors, (b) outdoors, (c) no difference; (3) Do you have better vision at the (a) beginning of day, (b) end of day, (c) no difference; (4) Do you have better vision on a (a) sunny day, (b) cloudy day, (c) no difference. Demographic parameters were collected in each survey including age, race and gender, visual acuity, and all applicable ophthalmic diagnosis as (cataract, pseudophakia, primary open angle glaucoma, dry age macular degeneration (AMD), exudative AMD, branch retinal vein occlusion, central retinal vein occlusion, choroidal neovascular membrane, macular hole, diabetes without retinopathy, non-proliferative diabetic retinopathy by stage, proliferative diabetic retinopathy, macular hole, epiretinal membrane, and refractive status) were marked for each patient by the physician. Each demographic parameter and ophthalmic disease was analyzed individually against each other and each of the four questions. Patients were excluded from the study if their visual acuity was lower than Finger count vision.
Statistical methods
Bi-variable associations between responses to each question (Q1–Q4) and patient covariates were assessed using Chi-squared tests and Fisher’s exact test. To account for potential confounding in bi-variable associations, multivariable models for each question were fit using multinomial regression. Age, gender, and race were included in each multivariable model, along with variables having a bi-variable association of unadjusted p < 0.05 with the corresponding question. Multiple imputation with imputation-corrected standard errors was used to account for missing values in multivariable models, following recommended procedures and guidelines using the aregImpute function in R package Hmisc [11, 12] and the MIcombine function in R package mitools [13]. Sensitivity analysis was performed by removing subjects with missing values prior to fitting multivariable models. Odds ratios (OR), 95% confidence intervals (CI), and p values were reported from the multinomial regression models. For each question, response probabilities for choices A and B were compared with choice C (no preference, baseline category). P values for bi-variable associations were adjusted for multiple comparisons using the false discovery rate (FDR) [14], and an FDR value of 0.1 was used as the discovery threshold (corresponding to an expected 10% of reported discoveries being null). Analyses were conducted using R version 4.0.0.
Results
A total of 722 surveys were completed, consisting of 435 females and 285 males. A total of 594 of the patients completing the study were White, while 103 were African American or other. Mean age of the sample was 71.6 years, with a standard deviation of 16.1, a median of 75, and an inter-quartile range of 63 (25th percentile) to 84 (75th percentile). Four hundred and forty-eight of the patients were pseudophakic and 282 had age-related macular degeneration (AMD); of those, 207 had exudative AMD and 75 patients had dry AMD. Two hundred and twenty-one patients had cataract. Of those, 182 had nuclear sclerosis, 22 patients had cortical cataracts, and 17 had posterior subcapsular cataracts. One hundred and sixteen of the patients were diabetics; of them, 99 patients with diabetic retinopathy. Fifty-seven patients had epiretinal membrane (ERM), and 38 patients had retinal vein occlusions. Thirty-three patients had macular hole. Combined, 553 patients (76.5%) had at least one ophthalmic disease (cataract NS, exudative AMD, dry AMD, POAG, ERM, RD, or DR), while 165 (22.8%) had 2 and 37 (5.1%) had 3 co-occurring ophthalmic diseases. The number and percent of missing values for covariates were 2 (0.3%) for age, 25 (3.5%) for race, 3 (0.4%) for gender, and 129 (17.8%) for vision (LogMAR). Full descriptive statistics for the sample are provided in Table 1.
Bi-variable results are displayed in Tables 2, 3, 4, and 5 corresponding to questions 1–4. Question 1 (better vision in (a) bright light, (b) dim light, (c) no difference) had a notable association with race, with 50% of White patients preferring a more lit environment vs a third of the African American patients (FDR p = 0.08). Patients with exudative AMD also preferred a more lit environment than patients with non-exudative AMD (57% vs. 46%, FDR p = 0.08). However, patients with an epiretinal membrane preferred dimmer light than patients with no ERM (28% vs. 17%, FDR p = 0.08). There was no association of light strength and dry AMD, primary open angle glaucoma (POAG), retinal detachment (RD), diabetic retinopathy, age, gender, and lens status.
Question 2 asked whether vision was better (a) indoors, (b) outdoors, (c) no difference. Patients with cataract (NS) had better vision outdoors (natural light, 27%) vs. indoors (artificial light, 17%), compared with those without cataracts (21% and 27%, respectively, FDR p = 0.08). A greater percentage of females preferred indoor lighting (28%) compared with males (19%) (FDR p = 0.07). However, over 50% of both males and females stated “no difference” when answering this question. Fifty-nine percent of patients with good vision (better than 20/40) stated no preference for indoor vs. outdoor lighting, while patients with reduced vision had stronger opinions for preferring either indoor (30.5%) or outdoor (29.9%) lighting, compared with no preference (39.7%) (FDR p = 0.009).
Question 3 asked whether the vision was better at the: (a) beginning of day, (b) end of day, (c) no difference. No associations with FDR p value < 0.1 were discovered. However, some evidence of association between vision preference at beginning vs. end of the day and retinal detachment surgery (FDR p = 0.19) and primary open angle glaucoma (FDR p = 0.15). More patients with glaucoma had better vision at the beginning of the day than patients with no glaucoma (38% vs. 19%, respectively). More patients with glaucoma had better vision at the end of the day than patients with no glaucoma. The same preference for end of the day was noted for patients s/p retinal detachment surgery (34% vs. 19% for those without surgery). However, 50% of the glaucoma patients and 59% of the retinal detachment patients had no preference.
Question 4 asked whether the vision was better on a (a) sunny day, (b) cloudy day, or (c) no difference. Pseudophakic patients preferred cloudy days compared with phakic patients (31% vs. 22%, respectively), with phakic patients more likely to choose no difference (50% vs. 37%, respectively, FDR p = 0.04). Patients with better vision (> 20/40) were less likely to notice a difference in sunny and cloudy days (FDR p = 0.07). Exudative AMD patients preferred a sunny day more than non AMD patients (36% vs. 28%, FDR p = 0.08).
Results from the multivariable multinomial models are given in Table 6. Multiple imputation was used to fill-in missing values, with 10 imputations and imputation-corrected standard errors. For question 1, White patients had nearly double the odds of selecting bright light (option A), compared with (c) no difference) compared with African American/other race (OR = 1.90, 95% CI 1.16–3.13). Patients’ age > 75 years had reduced odds of preferring dim light compared with no difference, relative to patients ≤ 75 years (OR = 0.55, 95% CI 0.33–0.91). Patients with ERM had reduced odds (OR = 0.54, 95% CI 0.28–1.05) of selecting bright light compared with no difference. Patients with exudative AMD had increased odds of selecting either bright light (OR = 1.5, 95% CI 0.97–2.32) or dim light (OR = 1.82, 95% CI 1.00–3.32) compared with no difference. For question 2, patients with lower vision (LogMAR ≥ 0.3) were more likely to indicate they either had better vision indoors (OR = 2.43, 95% CI 1.41–4.19 compared with LogMAR < 0.1) or outdoors (OR = 3.1, 95% CI 1.85–5.17 compared with LogMAR < 0.1) compared with indicating no difference. Patients with cataracts were less likely to indicate they had better vision indoors (OR = 0.53, 95% CI 0.33–0.85). Patients age ≥ 75 years were less likely to indicate better vision indoors (OR = 0.63, 95% CI 0.42–0.95) or outdoors (OR = 0.48, 95% CI 0.32–0.74) compared with patients age < 75 years. Males were less likely than females to indicate better vision indoors (OR = 0.62, 95% CI 0.42–0.92) compared with indicating no difference. For question 3, patients with either POAG (OR = 3.04, 95% CI 1.45–6.35) or RD (OR = 1.89, 95% CI 0.97–3.7) were more likely to indicate they had better vision at the beginning of the day compared with no difference. Patients aged > 75 years were somewhat less likely to indicate they had better vision at the beginning of the day compared with no difference (OR = 0.66, 95% CI 0.44–0.99). For question 4, patients with lower vision (LogMAR ≥ 0.3) were more likely to indicate they had better vision on a cloudy day vs. no difference (OR = 2.05, 95% CI 1.17–3.59), compared with patients with good vision (LogMAR < 0.1). Patients with pseudophakia were also more likely to indicate they had better vision on a cloudy day (OR = 1.91, 95% CI 1.24–2.9), as were males (OR = 1.46 relative to females, 95% CI 1.01–2.13). Exudative AMD did not exhibit a strong association in the multivariable model.
Discussion
Studies of the acuity-luminance function are reported for patients with reduced acuity resulting from optic nerve lesions, retinal lesions of various sorts, and suppression amblyopias [2]. The findings in all those groups can be attributed almost completely to the use of parafoveal or paramacular regions of the retina [2]. The eccentric viewing area is associated with a reduced rate of change of visual acuity with increasing luminance similar to the finding observed in the normal paracentral retina [2]. In patients with retinal pathology involving the macular area, the acuity-luminance graph may be shifted to the right, and as a result, these patients require very high lighting intensities to obtain their best visual acuity [2].
Patients with AMD and macular scarring have varying response to increasing luminance, and vision may improve significantly in some [2]. This correlates with our finding that patients with wet AMD preferred a more lit environment than patients with dry AMD or no AMD, and also correlates with our finding that patients with exudative AMD were more likely to prefer sunnier days or cloudy days (compared with no preference), relative to those without exudative AMD in bi-variable analysis. In multivariable analysis, after adjusting for covariates, there is stronger evidence of a meaningful association between exudative AMD and question 1 (indoor vs. outdoor lighting) compared with question 4 (sunny vs. cloudy days). This can partly be explained by strong associations between question 4 and other covariates (gender, vision, pseudophakia) and in turn the associations between those variables and exudative AMD (all p < 0.001, except for gender which had p = 0.26).
Patients with poorer visual acuity had a stronger preference for indoor or outdoor lighting (question 1, compared with no difference) and sunny or cloudy days (question 2, relative to no difference), while patients with better visual function were more likely to indicate no preference in the bi-variable analysis across all four questions. This finding of some lower vision patients preferring more cloudy days in the multivariable analysis is surprising, as one would expect those patients to use more light to increase their best visual acuity. However, this subgroup of patients was equally distributed between their preference to sunny, cloudy, or no preference. Therefore, this finding should be read with caution.
Although glaucoma is an asymptomatic disease in an early stage, it appears that glaucoma patients do report complaints related to visual performance under extreme luminance conditions [15]. However, in this study, we did not find that those patients needed more light than other patients tested at the retina clinic. The luminance needed in glaucoma patients is secondary to the involvement of the macula, and patients with no involvement of the macula need less luminance than patients with involvement of the macula [16]. Therefore, it well may be that the glaucoma in this study was not severe, or macula involving in this study, and did not affect luminance needs. Also, 25/38 (66%) of the patients in this study with glaucoma had a co-occurring ophthalmic disease. A greater percentage of patients with retinal detachment and glaucoma reported having better vision towards the end of the day compared with those without those conditions. However, 50% of the glaucoma patients and 59% of the retinal detachment patients noted no difference.
Our finding that women preferring indoor lighting and men preferring outdoor lighting in the bi-variable analysis is in agreement with the study by Chellappa et al which observed a significant sex difference for light preference, such that men preferred brighter light, while the opposite was observed for women [17]. Interestingly, for blue light, the stimulus-response curve in men is different than in women, suggesting a higher sensitivity to the blue spectrum of light [18]. The underlying factors for a sex-related differential sensitivity to light remain to be fully established [17]. In the multivariable analysis, males had 40% reduced odds of preferring indoor lighting compared with no preference, relative to females. However, over 50% of both sexes actually mentioned no difference regarding this question. Fifty percent of White patients preferring a more lit environment vs a third of the African American patients. We did not find any literature regarding racial preferences in light settings. These findings are yet to be studied.
Many retinal diseases including epiretinal membranes, diabetic retinopathy, AMD, glaucoma and cataracts cause a reduced contrast sensitivity [3,4,5,6,7,8]. It has been shown that a decrease in luminance causes a decrease in contrast sensitivity. Reducing the luminance by 100 lumens caused the contrast sensitivity to decrease by 8-fold although the visual acuity remained the same [10]. Although patients with epiretinal membranes were found to be more likely to prefer dim environment (relative to no preference) compared with those without ERM, most patients with epiretinal membranes still preferred a lit environment. It may be that some patients with epiretinal membrane preferred low luminance settings to decrease the contrast sensitivity in the eye with the epiretinal membrane and avoid the distortion it causes. Or that the contrast sensitivity in eyes with epiretinal membrane is low to begin with; therefore, the increased lighting conditions do not help.
The finding that some patients with cataract prefer outdoor lighting, and patients with pseudophakia prefer cloudy days may be related to an increased amount of light perceived by the pseudophakic patients. Lens extraction may reverse the increase in stray light, which is considered an independent source of symptoms [19]. Stray light is a possible source of unwanted visual phenomena related to patients with implanted intraocular lenses (IOLs). Recent studies reported little difference in retinal stray light between patients with monofocal IOLs and patients with multifocal IOLs [20]. Stray light is an independent source of symptoms, and it should be measured clinically independently from visual acuity-associated symptoms [21].
Although there were some significant differences between the groups, a large number of patients did not feel that different lighting conditions affected their vision. Although there is an explanatory rational for some of the findings in this study, as pseudophakic patients preferring more cloudy days, some differences such as those seen in ethnicity and gender need to be further studied. None of the questions about lighting conditions could be strongly connected with one specific disease or condition. This study is not free of limitations, as many patients (22.8%) had more than one condition. Also, this is subjective data, and patients can perceive light differently. Moreover, as mentioned, one third of the patients or more were not sure of the effect of the different lighting conditions. Missing values were present, especially for visual acuity (17.8%). Our multivariable analysis accounted for missing values using recommended multiple imputation techniques [11]. Sensitivity analysis using case-wise deletion of patients with missing information (Supplemental Table 1) indicates no substantive differences from the multiple imputation results.
In conclusion, there were differences noted in various ocular conditions and perceiving light; as expected, the difference was mostly noted in relation to lens status. Exudative AMD did not exhibit a strong association in the multivariable model. However, differences in light preference were noted in gender and ethnicity, and those are to be further explored. Of note, many patients were unsure of their light preference and further studies, such as longitudinal studies, are needed to further define the relationship of lighting condition in ophthalmic disease.
References
Sloan LL (1968) The photopic acuity-luminance function with special reference to parafoveal vision. Vis Res 8:901–911
Sloan LL (1969) Variation of acuity with luminance in ocular diseases and anomalies. Doc Ophthalmol 26:384–393
Liu L, Wang Y, Liu J, Liu W (2018) Retinal-image quality and contrast sensitivity function in eyes with epiretinal membrane: a cross-sectional observational clinical study. BMC Ophthalmol 18:290
Safi H, Safi S, Hafezi-Moghadam A, Ahmadieh H (2018) Early detection of diabetic retinopathy. Surv Ophthalmol 63:601–608
Ortiz C, Jiménez JR, Pérez-Ocón F, Castro JJ, González-Anera R (2010) Retinal-image quality and contrast-sensitivity function in age-related macular degeneration. Curr Eye Res 35:757–761
Gupta L, Cvintal V, Delvadia R, Sun Y et al (2017) SPARCS and Pelli-Robson contrast sensitivity testing in normal controls and patients with cataract. Eye (Lond) 31:753–761
Wolkstein M, Atkin A, Bodis-Wollner I (1980) Contrast sensitivity in retinal disease. Ophthalmology 87:1140–1149
Fatehi N, Nowroozizadeh S, Henry S, Coleman AL, Caprioli J, Nouri-Mahdavi K (2017) Association of structural and functional measures with contrast sensitivity in glaucoma. Am J Ophthalmol 178:129–139
Pelli DG, Bex P (2013) Measuring contrast sensitivity. Vis Res 90:10–14
Rabin J (1994) Luminance effects on visual acuity and small letter contrast sensitivity. Optom Vis Sci 71:685–688
Clark TG, Altman DG (2003) Developing a prognostic model in the presence of missing data: an ovarian cancer case study. J Clin Epidemiol 56:28–37
Harrell FE (2020). Hmisc: Harrell Miscellaneous. R package version 4.4-0. https://CRAN.R-project.org/package=Hmisc. Accessed 10 Sept 2020
Lumley T (2019). mitools: tools for multiple imputation of missing data. R package version 2.4. https://CRAN.R-project.org/package=mitools. Accessed 10 Sept 2020
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 57:289–300
Bierings RAJM, van Sonderen FLP, Jansonius NM (2018) Visual complaints of patients with glaucoma and controls under optimal and extreme luminance conditions. Acta Ophthalmol 96:288–294
Blumberg DM, Liebmann JM, Hirji SH, Hood DC (2019) Diffuse macular damage in mild to moderate glaucoma is associated with decreased visual function scores under low luminance conditions. Am J Ophthalmol 208:415–420
Chellappa SL, Steiner R, Oelhafen P, Cajochen C (2017) Sex differences in light sensitivity impact on brightness perception, vigilant attention and sleep in humans. Sci Rep 7:14215
Cowan RL, Frederick BB, Rainey M, Levin JM et al (2000) Sex differences in response to red and blue light in human primary visual cortex: a bold fMRI study. Psychiatry Res 100:129–138
Van Den Berg TJ, Van Rijn LJ, Michael R, Heine C et al (2007) Straylight effects with aging and lens extraction. Am J Ophthalmol 144:358–363
Cerviño A, Hosking SL, Montés-Micó R, Alió JL (2008) Retinal straylight in patients with monofocal and multifocal intraocular lenses. J Cataract Refract Surg 34:441–446
Ferrer-Blasco T, Montés-Micó R, Cerviño A, Alfonso JF (2009) Light scatter and disability glare after intraocular lens implantation. Arch Ophthalmol 127:576–580
Funding
Supported by an unrestricted grant from Research to Prevent Blindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the University of Louisville IRB.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Fleissig, E., Appenbrick, E., Brock, G. et al. Lighting conditions and perceived visual function in ophthalmic conditions. Graefes Arch Clin Exp Ophthalmol 259, 723–732 (2021). https://doi.org/10.1007/s00417-020-04960-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04960-w