Abstract
Purpose
To evaluate and compare the rate and characteristics of vitreoretinal disorders in fellow eyes of lamellar macular holes (LMH) versus epiretinal membrane foveoschisis (ERMF).
Methods
Included patients in this retrospective study were divided into two groups based on spectral-domain optical coherence tomography (SD-OCT) features of their primary eye: LMH (group A) and ERMF (group B).
Results
Ninety-four patients were enrolled: 59 (62.8%) in group A and 35 (37.2%) in group B. Fellow eyes in group A had a higher rate of retinal detachment (8/59 [13.6%] vs. 0/35 [0%], P = 0.024), and full-thickness macular hole (FTMH) (11/59 [18.6%] vs. 2/35 [5.7%], P = 0.079), compared with fellow eyes in group B. In group A, 4/59 patients (6.8%) showed a bilateral LMH while none from group B had a LMH in their fellow eye (0/35 [0%]), P = 0.293. Additionally, epiretinal proliferation was noted in 30/59 (50.8%) fellow eyes in group A versus 3/35 (8.6%) fellow eyes in group B, P < 0.001. Longitudinal data were available for 80/94 patients. Over a mean follow-up of 37.4 ± 29.9 months, 1/48 (2.1%) fellow eyes from group A developed a FTMH and 2/48 (4.2%) developed a LMH, while no FTMH or LMH occurred in fellow eyes of group B.
Conclusions
Fellow eyes of LMH showed a high rate of macular and peripheral vitreoretinal disorders. In addition, epiretinal proliferation was detected in a higher number of fellow eyes of LMH versus ERMF. These findings suggest a bilateral process in eyes of patients with LMH.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lamellar macular hole (LMH) is a macular lesion characterized by a partial thickness foveal defect but its true definition is debated and its pathogenesis still remains poorly understood. The study and classification of LMH have been hampered by the lack of universal consensus on a definition, which has resulted in the conflation of several different macular diseases over the past several years [1,2,3]. Various propositions have been made regarding the pathophysiology of LMH including partial avulsion of the inner retinal layer during posterior vitreous detachment, sustained contraction of an epiretinal membrane (ERM), rupture of the inner cystic wall in eyes with chronic cystoid macular edema, and progressive retinal degenerative processes [3,4,5].
Recent advances in retinal imaging have provided new insights into our understanding of LMH. An international panel of vitreoretinal experts recently proposed an OCT-based definition of LMH [6]. This classification proposed three OCT-based clinical entities: lamellar macular hole, epiretinal membrane foveoschisis, and macular pseudohole. The required criteria for LMH were the presence of an irregular foveal contour, a foveal cavitation, and a true loss of retinal tissue. By contrast, the macular diseases characterized by the presence of intraretinal cleavage due to the contraction of an ERM were named “epiretinal membrane foveoschisis” (ERMF). While outer retinal layers (i.e., external limiting membrane and ellipsoidal zone) are usually preserved in ERMF, LMH are often associated with early ellipsoidal zone disruption and subsequent vision loss. Macular pseudohole was defined by the presence of a foveal sparring ERM and a steepened foveal profile. In this new classification, LMH is notably distinguished from other tractional-related macular diseases, while in the past LMH and ERMF were usually considered different subtypes of “lamellar macular holes” [3, 6].
In eyes with LMH, Pang and colleagues first described on OCT the presence of a thick and isoreflective epiretinal tissue, which they initially termed “lamellar hole–associated epiretinal proliferation” (LHEP) [7]. Further histopathological analyses differentiated it from ERM by the lack of contractile properties [8, 9]. More recently, this proliferation has been described in association with other retinal conditions than LMH, such as full-thickness macular hole and ERM formation [6, 10,11,12], and therefore, the more inclusive term “epiretinal proliferation” (ERP) was preferred to refer to this material [6]. The initial trigger leading to this proliferation remains unknown, and it is unclear if this ERP is the primary cause or a consequence of LMH.
Despite extensive investigation and research, the rate and characteristics of vitreoretinal disorders in fellow eyes of patients diagnosed with LMH have been minimally studied [13]. Such information may improve our understanding of LMH and ERP pathogenesis [14]. Thus, this study was designed to perform a retrospective fellow eye analysis, with the aim to characterize and compare the occurrence of vitreoretinal abnormalities in the fellow eyes of patients with LMH versus ERMF. We separately studied and compared fellow eyes of LMH and ERMF to evaluate the recent theories that these are separate clinical entities with potentially different clinical development, progression, and pathophysiology.
Methods
Design
This was a retrospective, consecutive, and observational study that adhered to the principles of the Declaration of Helsinki and to the regulations of the Health Insurance Portability and Accountability Act. This study was approved by the University of California Los Angeles Office of Human Research Protection (IRB#16-000574).
The clinical charts and spectral-domain optical coherence tomography (SD-OCT) scans of consecutive patients with a diagnosis of “lamellar macular hole”, between January 2014 and December 2018, at the Stein Eye Institute, University of California Los Angeles, were carefully reviewed and analyzed. Due to the lack of clear OCT definition of lamellar macular holes in the past, only patients under the care of one retina specialist (JPH) were included to get an accurate data collection. During the period under review, patients with a lamellar macular hole and an epiretinal membrane foveoschisis were respectively classified as “degenerative lamellar macular hole” and “tractional lamellar macular hole,” and both retrieved by searching patients with a diagnosis of “lamellar macular hole.”
Inclusion criteria were the presence of lamellar macular hole (LMH) or epiretinal membrane foveoschisis (ERMF) in at least one eye. The specific criteria for the definition of these two lesions subtypes were based on the “optical coherence tomography-based consensus definition for lamellar macular hole” and are described below [6]. Exclusion criteria were the presence in any eye of active choroidal neovascularization, active retinal vascular disease, and uninterpretable or poor-quality SD-OCT scans.
Study population
Included patients were retrospectively divided into two groups depending on the SD-OCT imaging features affecting the primary eye at baseline: group A (LMH) and group B (ERMF), as illustrated in Fig. 1. In case of bilateral lesions, the first symptomatic eye was the one considered the primary eye.
Classification of the primary eyes at baseline. Lamellar macular hole (left). Optical coherence tomography scan shows a foveal cavity characterized by an apparent loss of foveal tissue with a foveal cavity with undermined edges open to the vitreous cavity. Epiretinal proliferation is visible on the edges of the hole (solid arrowheads). Epiretinal membrane foveoschisis (right). Optical coherence tomography image shows a macular thickening and intraretinal cleavage at the level of the Henle fiber layer resulting from the contraction of an epiretinal membrane (empty arrowheads). Cystic spaces are visible between the membrane and the retina (white arrow)
Group A lesions (LMH) were defined by the presence of the following major inclusion criteria: (1) an irregular foveal contour, (2) the presence of foveal cavitation, and (3) an apparent loss of foveal tissue. Minor criteria for the diagnosis of LMH were (1) the presence of epiretinal proliferation, (2) the presence of a foveal bump, and (3) the presence of EZ disruption [6]. Group B included cases of epiretinal membrane foveoschisis (ERMF) illustrating an epiretinal membrane (ERM) and a cleavage at the level of the Henle fiber layer [2, 6].
The term “epiretinal proliferation” was defined on SD-OCT as a thick homogeneous layer of isoreflective and non-contractile epiretinal material typically bounded by a thin hyperreflective band [6, 7]. The term “epiretinal membrane” (ERM) corresponded to a thin hyperreflective line over the internal limiting membrane, with tractional properties, and frequently separated from the underlying retina by small hyporeflective spaces [6].
Baseline and last follow-up data
The patient’s presenting visit to the senior author (JPH) was deemed the baseline evaluation. History of vitreomacular surgery, rhegmatogenous retinal detachment (RRD), and retinal tear were collected. Examination at presentation and at the end of the follow-up period included best-corrected visual acuity (BCVA), intraocular pressure, and lens status assessment. Characteristics at baseline were studied for all included patients, while longitudinal data were analyzed for patients who had been evaluated by the senior author (JPH) at two different times with OCT examination between January 2014 and December 2018. Best-corrected visual acuity was measured on a Snellen chart and converted to a logarithm of the minimum angle of resolution (LogMAR) for statistical analysis.
Spectral-domain OCT imaging
In all cases, eye-tracked OCT images were obtained with the Spectralis SD-OCT device (Heidelberg Engineering GmbH, Heidelberg, Germany) at baseline and at the end of the follow-up and reviewed with the Heidelberg Eye Explorer (version 1.8.6.0) using the HRA/Spectralis Viewing Module (version 5.8.3.0). The Spectralis OCT imaging protocol included a 20 × 15-degree volume scan with 19 B-scans spaced 242 μm apart and a single high-definition 30-degree horizontal line. A high-density 15 × 10 degrees with 97 B-scans spaced 30 μm apart was also performed in selected eyes. Additionally, some patients were imaged with the RS-3000 Advance OCT (Nidek Co, Gamagori, Japan).
SD-OCT characteristics recorded in both eyes included the presence of macular posterior vitreous detachment (PVD), ERP, ERM, and disruption of EZ. Central foveal thickness (CFT) (defined as the thinnest vertical height from the bottom of the lesions to the inner retinal pigment epithelium [RPE] boundary) was measured using the caliper function of the Heidelberg device.
In fellow eyes, the presence of vitreomacular abnormalities including vitreomacular traction (VMT), ERMF, LMH, and FTMH was analyzed and recorded. In addition to the CFT, the central macular thickness (CMT), corresponding to the mean retinal thickness within the central 100-μm diameter area, was measured using the Spectralis Software, and boundary lines were manually adjusted when necessary.
CMT values were measured in fellow eyes, while not used in primary eyes analysis since this value was not consistent in LMH eyes due to their irregular foveal profile. Of note, full-thickness macular hole eyes were excluded from CFT and CMT measurements. All SD-OCT scans were carefully reviewed independently by two examiners (IC, NM). Discordant cases were adjudicated by a third retina specialist (JPH) until a consensus was reached.
Main outcome
The main outcome measurement was the fellow eye’s rate of vitreoretinal pathologies and macular SD-OCT abnormalities in group A versus group B.
Statistical analysis
Quantitative values were presented as mean ± standard deviation (SD), while qualitative values were listed as ratio and percentage. Normality of variable distribution was assessed through visual inspection (e.g., histograms and quantile-quantile plots) and with the Shapiro-Wilk test. The Mann-Whitney U test or the Student t test was used to compare continuous data between the two groups. The paired t test or the Wilcoxon’s signed-rank test was used to compare continuous variable changes. Qualitative variables were compared using the chi-square test or the Fisher exact test. A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using the XLSTAT software version 2018.1.49572 (Assinsoft, Paris, France).
Results
Population
After a comprehensive chart review of 123 patients, 94 patients (188 eyes), of which 65 (69.1%) were female and 29 (30.9%) were male, met the inclusion criteria and were enrolled in this study. Follow-up data were available for 80 of these 94 patients with a mean interval follow-up of 37.4 ± 29.9 months.
Primary eyes at baseline
Characteristics of the primary eyes at baseline are reported in Table 1. Degenerative LMH (group A) was diagnosed in 59 out of 94 (62.8%) eyes. Five out of 59 (8.5%) primary eyes in group A were noted to have a history of retinal detachment and 8 out of 59 (13.6%) eyes had a history of laser retinopexy treatment for retinal tear formation. History of pars plana vitrectomy for FTMH (1/59) or VMT (1/59) was noted in two out of 59 (3.4%) primary eyes.
Epiretinal membrane foveoschisis (group B) was noted in 35 out of 94 (37.2%) primary eyes, of which three (8.6%) eyes were previously treated by laser for retinal tear and no cases had a history of RRD or macular surgery.
Mean BCVA at baseline was significantly lower in primary eyes from group A (0.32 ± 0.33 LogMAR [20/41 Snellen equivalent]) versus group B (0.20 ± 0.29 LogMAR [20/31 Snellen equivalent], P = 0.013). An ERM was significantly more frequent in group B (35/35 equivalent to 100.0%) compared with group A (4/59 equivalent to 6.8%), P < 0.001, whereas ERP was significantly more frequent in group A (43/59 equivalent to 72.9%) versus group B (6/35, equivalent to 17.1%), P < 0.001. The primary eyes in group A also exhibited a higher rate of EZ disruption (P < 0.001), and a higher inner/outer hole diameter ratio (P < 0.001) versus primary eyes in group B.
Fellow eyes baseline data
The clinical characteristics of fellow eyes are summarized in Table 2. In group A, 8 out of 59 (13.6%) fellow eyes had a history of RRD and 6 out of 59 (10.2%) had a history of laser treatment for retinal tear. Remarkably, there were no cases of retinal detachment reported in fellow eyes from group B while 3 out of 35 (8.6%) fellow eyes in group B had laser retinopexy for retinal tear. This higher rate of fellow eye RRD in group A versus group B was statistically significant (P = 0.024).
In group A, 11 out of 59 (18.6%) fellow eyes had a FTMH, of which five were diagnosed at baseline and six underwent a surgery before baseline, whereas two out of 35 (5.7%) fellow eyes in group B were diagnosed with a FTMH at baseline (P = 0.079). At baseline, four out of 59 (6.8%) patients exhibited a bilateral LMH in group A while no case of LMH was reported in fellow eyes of group B (P = 0.293). In addition, a ERMF was noticed in two out of 59 (3.4%) fellow eyes in group A and in two out of 35 (5.7%) fellow eyes in group B, without significant difference (P = 0.627). Interestingly, ERP was identified in 30 out of 59 (50.8%) fellow eyes in group A versus 3 out of 35 (8.6%) fellow eyes in group B (P < 0.001) (Fig. 2).
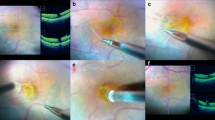
Epiretinal proliferation in fellow eyes of lamellar macular holes. Every row shows spectral-domain optical coherence tomography scans of both eyes from the same patient. Optical coherence tomography scans of the fellow eyes (left panel) show additional isoreflective material (white arrows) over the fovea, typically bounded by a thin hyperreflective line
Longitudinal data
Longitudinal data were available for 48 out of 59 (81.4%) patients in group A and 32 out of 35 (91.4%) patients in group B. No difference in follow-up duration between patients within the group A (40.2 ± 32.8 months; [range: 1.7–120.4 months]) and patients within the group B (33.1 ± 24.9 months [range: 2.8–114.5 months]) was found (P = 0.353). Longitudinal data of primary and fellow eyes are reported in Table 3.
Over the follow-up period, four out of 48 (8.3%) primary eyes in group A showed spontaneous conversion from LMH to FTMH while no case of FTMH occurred in primary eyes of group B. Two out of the 48 (4.2%) fellow eyes in group A developed a LMH during the follow-up period. Both of them had a complete posterior vitreous detachment and displayed ERP at baseline (Fig. 3). One out of 48 (2.1%) fellow eyes in group A with a history of vitrectomy for RRD developed a FTMH. No cases of LMH or FTMH occurred in fellow eyes of group B, and no cases of VMT were recorded in fellow eyes of groups A and B.
Development of a bilateral lamellar macular hole. Spectral-domain optical coherence tomography images showing the development of a lamellar macular hole (LMH) in the fellow eye of a patient with LMH. In the primary eye (left column), SD-OCT scans show a LMH with epiretinal proliferation (white arrowheads) and progressive increase of retinal cavitation (white arrows) over the follow-up. Optical coherence image (right column) of the fellow eye from January 2013 shows a discreet additional isoreflective material (white arrowhead), surrounded by a thin hyperreflective line, in the nasal side of the foveal area (top right). Twenty-eight months later, a LMH was visible with apparent loss of retinal tissue (white arrow), and an increase of epiretinal proliferation (white arrowhead) over the nasal surface of the fovea (middle right). After 38 months of follow-up, the retinal defect (white arrow) reached the external limiting membrane (bottom right)
Overall, at the last follow-up, 12 of 59 (20.3%) fellow eyes in group A had a FTMH versus two of 35 (5.7%) fellow eyes in group B (P = 0.054). Six of 59 (10.2%) patients had a bilateral LMH in group A, whereas no cases of LMH were identified in the 35 fellow eyes in group B (P = 0.081).
Discussion
Even though our ability to define the morphological features of LMH has tremendously improved during the past few years, our understanding of its pathogenesis and initial trigger has not yet been elucidated [2, 3, 6].
To aid our understanding of its pathogenesis, so far only one study has focused on the fellow eyes of LMH [13]. Nava and colleagues reported the presence of ERM in 74% of LMH fellow eyes, a bilateral LMH in three cases (9%) and the occurrence of one LMH in the fellow eye after 3 years of follow-up [13]. The authors concluded that the presence of LMH in one eye does not significantly increase the risk of developing the same disease in the fellow eye. However, they did not distinguish LMH from other tractional-related vitreomacular diseases (i.e., epiretinal membrane foveoschisis). Most of the presented cases in this report displayed, in their primary eyes, an ERM with intraretinal schisis more than a true loss of retinal tissue as seen in LMH. In the present study, LMH and ERMF eyes have been sorted within two different groups, in the light of the recent OCT-based consensus definition for LMH, to specifically study the rate of vitreoretinal disorders in the fellow eyes of LMH and to compare it with those of ERMF [6]. Our results demonstrated a high rate of vitreoretinal disorders in both eyes of patients with LMH, supporting the idea of a bilateral vitreoretinal condition in these patients.
Epiretinal proliferation has been studied in eyes with LMH and FTMH. On OCT, ERP appears as a thick, homogenous, isoreflective material over the ILM and often bounded by a thin hyperreflective line [6, 7]. Histological analysis in LMH demonstrated that this proliferation contains retinal glial cells, and especially Müller cells [9]. However, the exact pathogenesis of this proliferation remains poorly understood. Our current understanding is that this proliferation develops in LMH as a consequence of Müller cell activation and migration in response to the loss of retinal tissue [9, 15]. However, using SD-OCT, we found similar isoreflective material, in half of fellow eyes of LMH, without any other apparent retinal structural change (Fig. 3). Therefore, it may be speculated that Müller cell dysregulation and migration could actually be present in both eyes of some patients with LMH [10, 16].
Consistently with previous reports [3, 17], we noted that 72.9% of LMH (primary eyes) displayed ERP, but we also observed the presence of an additional isoreflective material over the fovea in 50.8% of their fellow eyes. Based on blue-light fundus autofluorescence (B-FAF) and SD-OCT imaging, Dell’Omo and colleagues described recently similar foveal abnormalities that they termed FATIAS, for “Foveal Abnormality associated with epiretinal Tissue of medium reflectivity and Increased blue-light fundus Autofluorescence Signal,” in 47 eyes without other significant retinal condition [18]. They defined FATIAS by the presence of an abnormal foveal contour and the presence of an additional tissue of medium reflectivity on SD-OCT, and an increase B-FAF signal at the fovea [18]. They hypothesized that this lesion might be secondary to a true loss of retinal tissue arising from the PVD, or a displacement of retinal tissue due to age-related vitreous change and an inherent weakness of the retina. We classified this additional medium reflectivity on SD-OCT tissue as ERP. Of note, B-FAF was not routinely performed in our practice, and therefore, we were not able to ensure that similar B-FAF changes were retrieved in fellow eyes with additional isoreflective material. Interestingly, Dell’Omo and colleagues also reported a high rate of vitreoretinal interface disorders in the fellow eyes of patients with the so-called FATIAS, including 11 FTMH and 3 LMH, supporting our observations.
The fellow eyes of LMH showed a high rate of severe vitreomacular diseases. In fact, out of 59 fellow eyes, 12 had a FTMH (20.3%) and six had a LMH (10.2%). This suggests that LMH patients likely present bilateral abnormal vitreomacular interface and/or an inherent foveal weakness. Thus, the ERP that we noted in fellow eyes of LMH may participate in the development of such macular lesions by modification of the posterior hyaloid adherence, or may reflect a dysfunction of Müller cells [19]. The glial cells and notably Müller cells are known to provide essential structural support and tensile strength to the retinal tissue [20, 21]. As a consequence, dysfunction of glial Müller cells may lead to a higher risk of LMH and/or FTMH due to a lack of retinal adhesiveness [20, 22]. This latter hypothesis is reinforced by the progression, over the follow-up period, of four LMH (in the primary eyes) to a FTMH, despite a previous posterior vitreous detachment, suggesting an inherent weakness of the retina [23,24,25].
Patients with LMH also showed a high rate of RRD and retinal tear in both eyes. Retinal detachment and retinal tear formation may cause a mechanical stimulus leading to dysregulation of astrocytes and activation of Müller cells [26, 27]. This Müller cell dysregulation might lead to ERP and/or LMH formation [26, 27]. Alternatively, it is possible that LMH patients have a primary dysregulation of Müller cells leading to ERP as well as an altered peripheral vitreoretinal interface predisposing to the development of retinal tear and RRD [20, 22]. The mean visual acuity of the LMH eyes was significantly lower compared with ERMF eyes. This may be explained by the higher rate of outer retinal layers disruption (e.g., EZ disruption) which has been reported to be one of the typical features of LMH [6, 17, 21]. However, the greater proportion of LMH eyes which had a history of RRD surgery or macular peeling surgery compared with ERMF eyes may also have contributed to this difference.
The limitations of this study included the retrospective nature of the analysis and the possibility of selection bias. Thus, the high rate of RRD we noted in patients with LMH may have been the result of ascertainment bias due to the selection of patients from an academic tertiary care clinic managed by a highly specialized vitreoretinal surgeon. However, no cases of RRD were reported in group B from the same population. Of note, the SD-OCT identification of ERP in the fellow eye was admittedly challenging and required high-quality imaging, as the abnormality was subtle to detect in certain cases. However, similar observations have recently been reported and correlated with B-FAF abnormalities [15, 18], and each SD-OCT scan has been carefully analyzed by at least two readers. The strengths of this study include the clear distinction between patients with LMH and patients with ERMF, the relatively large number of included patients, and the long follow-up period of time.
In conclusion, fellow eyes of LMH had a higher rate of macular and peripheral vitreoretinal abnormalities compared with fellow eyes of ERMF and illustrated isolated ERP with SD-OCT analysis. These findings reinforce the idea that LMH imply different pathogenesis than ERMF and provide evidence that patients with LMH may be predisposed to develop bilateral macular and peripheral vitreoretinal conditions.
Data availability
All de-identified and coded data of patients included in the study are available by request.
References
Haouchine B, Massin P, Tadayoni R et al (2004) Diagnosis of macular pseudoholes and lamellar macular holes by optical coherence tomography. Am J Ophthalmol 138:732–739
Gaudric A, Aloulou Y, Tadayoni R et al (2013) Macular pseudoholes with lamellar cleavage of their edge remain pseudoholes. Am J Ophthalmol 155:733–742
Govetto A, Dacquay Y, Farajzadeh M et al (2016) Lamellar macular hole: two distinct clinical entities? Am J Ophthalmol 164:99–109
Gass JD (1975) Lamellar macular hole: a complication of cystoid macular edema after cataract extraction: a clinicopathologic case report. Trans Am Ophthalmol Soc 73:231–250
Duker JS, Kaiser PK, Binder S et al (2013) The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619
Hubschman JP, Govetto A, Spaide RF et al (2020) Optical coherence tomography-based consensus definition for lamellar macular hole. Br J Ophthalmol https://doi.org/10.1136/bjophthalmol-2019-315432
Pang CE, Spaide RF, Freund KB (2014) Epiretinal proliferation seen in association with lamellar macular holes: a distinct clinical entity. Retina 34:1513–1523
Compera D, Entchev E, Haritoglou C et al (2015) Correlative microscopy of lamellar hole-associated epiretinal proliferation. J Ophthalmol 2015:1–8
Pang CE, Maberley DA, Freund KB et al (2016) Lamellar hole-associated epiretinal proliferation: a clinicopathologic correlation. Retina 36:1408–1412
Itoh Y, Levison AL, Kaiser PK et al (2016) Prevalence and characteristics of hyporeflective preretinal tissue in vitreomacular interface disorders. Br J Ophthalmol 100:399–404
Lai T-T, Yang C-M (2018) Lamellar hole-associated epiretinal proliferation in lamellar macular hole and full-thickness macular hole in high myopia. Retina 38:1316–1323
Takahashi H, Inoue M, Itoh Y et al (2018) Macular dehiscence-associated epiretinal proliferation in eyes with full-thickness macular hole. Retina 00:1–9
Nava U, Cereda MG, Bottoni F et al (2017) Long-term follow-up of fellow eye in patients with lamellar macular hole. Graefes Arch Clin Exp Ophthalmol 255:1485–1492
Ezra E, Wells JA, Gray RH et al (1998) Incidence of idiopathic full-thickness macular holes in fellow eyes. A 5-year prospective natural history study. Ophthalmology 105:353–359
Dell’Omo R, Vogt D, Schumann RG et al (2018) The relationship between blue-fundus autofluorescence and optical coherence tomography in eyes with lamellar macular holes. Invest Ophthalmol Vis Sci 59:3079–3087
Schumann RG, Eibl KH, Zhao F et al (2011) Immunocytochemical and ultrastructural evidence of glial cells and hyalocytes in internal limiting membrane specimens of idiopathic macular holes. Invest Ophthalmol Vis Sci 52:7822–7834
Pang CE, Spaide RF, Freund KB (2015) Comparing functional and morphologic characteristics of lamellar macular holes with and without lamellar hole-associated epiretinal proliferation. Retina 35:720–726
Dell’Omo R, De Turris S, Filipelli M et al (2019) Foveal abnormality associated with epiretinal tissue of medium reflectivity and increased blue-light fundus autofluorescence signal (FATIAS). Graefes Arch Clin Exp Ophthalmo 257:2601–2612. https://doi.org/10.1007/s00417-019-04451-7
Bringmann A, Wiedemann P (2009) Involvement of Müller glial cells in epiretinal membrane formation. Graefes Arch Clin Exp Ophthalmol 247:865–883
MacDonald RB, Randlett O, Oswald J et al (2015) Müller glia provide essential tensile strength to the developing retina. J Cell Biol 210:1075–1083
Govetto A, Bhavsar KV, Virgili G et al (2017) Tractional abnormalities of the central foveal bouquet in epiretinal membranes: clinical spectrum and pathophysiological perspectives. Am J Ophthalmol 184:167–180
Lu Y-B, Pannicke T, Wei E-Q et al (2013) Biomechanical properties of retinal glial cells: comparative and developmental data. Exp Eye Res 113:60–65
Fabian ID, Moisseiev E, Moisseiev J et al (2012) Macular hole after vitrectomy for primary rhegmatogenous retinal detachment. Retina 32:511–519
Compera D, Schumann RG, Cereda MG et al (2018) Progression of lamellar hole-associated epiretinal proliferation and retinal changes during long-term follow-up. Br J Ophthalmol 102:84–90
Smiddy WE (2008) Macular hole formation without vitreofoveal traction. Arch Ophthalmol 126:737–738
Luna G, Keeley PW, Reese BE et al (2016) Astrocyte structural reactivity and plasticity in models of retinal detachment. Exp Eye Res 150:4–21
Pfeiffer RL, Marc RE, Kondo M et al (2016) Müller cell metabolic chaos during retinal degeneration. Exp Eye Res 150:62–70
Funding
Supported by an unrestricted grant from Research to Prevent Blindness and the Hess Foundation, which had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jean-Pierre Hubschman: Alcon (C), Allergan (C), Bausch and Lomb (C), Novartis (C), and Carl Zeiss Meditec (C). David Sarraf: Amgen (C, F), Genetech-Roche (C, F), Heidelberg (F), Novartis (C, F), Optovue (C, F), Regeneron (F), Bayer (C, F), and Topcon (F) The following authors have no financial disclosures: Ismael Chehaibou, Niranjan Manoharan, Andrea Govetto, and Anibal Andrés Francone.
Ethics approval
This research study was conducted retrospectively from data obtained for clinical purposes. An IRB official waiver of ethical approval was granted from the University of California Los Angeles Office of Human Research Protection (IRB#16-000574).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not Applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of a topical collection on Macular Holes
Rights and permissions
About this article
Cite this article
Chehaibou, I., Manoharan, N., Govetto, A. et al. Comparison of vitreoretinal disorders in fellow eyes of lamellar macular holes versus epiretinal membrane foveoschisis. Graefes Arch Clin Exp Ophthalmol 258, 2611–2619 (2020). https://doi.org/10.1007/s00417-020-04950-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04950-y