Abstract
Purpose
To identify the functional outcome and evaluate the morphologic changes of patients with pachychoroid neovasculopathy (PNV) undergoing intravitreal anti-vascular endothelial growth factor (VEGF) combined with photodynamic therapy (PDT) at the 1-year follow-up.
Methods
We retrospectively studied all the treatment-naïve PNV patients who were scheduled to undergo combination therapy between September 2017 and November 2018. All the patients received three consecutive monthly injections of 0.5 mg/0.05 mL ranibizumab as loading doses. Full-dose PDT was performed within 1 week of the first injection. Retreatment was allowed if evidence of clinical deterioration or the presence of fluid on spectral-domain optical coherence tomography examination performed at the 1-month follow-up was noted. The best-corrected visual acuity (BCVA) was compared before treatment and at 3, 6, and 12 months after the initial treatment. Changes in the central foveal thickness (CFT), central choroidal thickness (CCT), and retreatment rate during the maintenance phase were also evaluated.
Results
Eleven eyes were enrolled in this study. Significantly, better BCVA was observed at 12 months than at baseline (P = 0.010). The mean CFT significantly decreased from 331 ± 93 to 237 ± 72 μm at 12 months (P < 0.001). The mean CCT also significantly decreased from 361 ± 74 to 310 ± 83 μm at 12 months (P < 0.001). The mean number of injections per eye was 3.9 ± 1.3 during the follow-up period. A total of 45.5% (5 /11) of the patients required retreatment during the maintenance phase.
Conclusion
Anti-VEGF combined with full-dose PDT was well tolerated and appeared to be effective treatment for patients with treatment-naïve PNV. Combination therapy might also reduce the treatment burden with fewer injections in patients with PNV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Choroidal neovascularization (CNV) is a severe complication that induces vision loss in chorioretinal diseases [1]. Type 1 NV is the most common subtype of neovascularization in age-related macular degeneration (AMD) and is characterized by pathologic angiogenesis below the retinal pigment epithelium (RPE) [2, 3]. Other conditions that are commonly associated with type 1 NV include the pachychoroid disease spectrum [4,5,6]. Pachychoroid neovasculopathy (PNV), included in the pachychoroid-related spectrum, is characterized by type 1 NV caused by a pachychoroid-driven process involving choroidal vascular hyperpermeability (CVH) manifested by thickened choroid and dilated choroidal vessels (pachyvessels) [7].
AMD is most frequently treated with anti-vascular endothelial growth factor (VEGF) agents that have demonstrated efficacy in improving visual acuity outcomes [8, 9]. The pathophysiology of PNV has been defined as type 1 NV overlying large choroidal vessels, often misinterpreted as AMD. Therefore, it is predicted that anti-VEGF agents would be useful for the treatment of PNV. In fact, many studies have reported the efficacy of intravitreal injection of anti-VEGF for PNV [10, 11]. However, the need for frequent visits and the burden of injections are issues that require resolution.
Photodynamic therapy (PDT) is known to decrease the choroidal thicknesses to suppress CVH [12]. Therefore, it is expected that anti-VEGF agents combined with PDT may be effective with reduced number of injections in patients with PNV. However, combined therapy for PNV have not been identified. The purpose of this report was to identify the functional outcome and assess morphologic changes of patients with PNV undergoing intravitreal anti-VEGF combined with PDT at the 1-year follow-up.
Patients and methods
We retrospectively reviewed the medical records of 11 eyes from 10 treatment-naïve Japanese patients with PNV treated with anti-VEGF combined with PDT at the Yokohama City University Medical Center between September 2017 and November 2018. This study design was approved by the institutional review board at the Yokohama City University Medical Center. It also followed the tenets of the Declaration of Helsinki.
The inclusion criteria were the presence of PNV determined by clinical, spectral-domain optical coherence tomography (SD-OCT), fluorescein angiography (FA), indocyanine green angiography (ICGA), and OCT angiography (OCTA) findings. PNV was defined as a form of type 1 NV, occurring over the areas of pachyvessels that exceeded the choroidal diameter seen in normal eyes, with exudative changes such as fluid (subretinal fluid, intraretinal fluid, and sub-RPE fluid), fibrin, and hemorrhage [6]. In areas overlying pachyvessels, attenuation of choriocapillaris and dilation of Haller vessels were observed even if central choroidal thickness (CCT) are less than 300 μm. All the patients had no polypoidal lesions before the treatment and also no history of central serous chorioretinopathy (CSC) in the past. Patients who had a history of previous treatment for PNV (i.e., laser photocoagulation, PDT, the intravitreal injection of anti-VEGF agents, or intravitreal steroids) were excluded from this study.
All eyes received three consecutive monthly intravitreal injections of 0.5 mg/0.05 mL ranibizumab (Lucentis®; Novartis Pharma AG, Basel, Switzerland, and Genentech, South San Francisco, CA, USA) combined with PDT as an induction treatment. Full-dose PDT was performed within 1 week of the first intravitreal injection. Verteporfin was administered over 10 min. Fifteen minutes after the intravenous infusion started, a 689-nm laser was applied for 83 s to deliver 50 J/cm2. The greatest linear dimension (GLD) was determined to cover the abnormality vascular network. During the maintenance phase, retreatment of anti-VEGF injection was allowed if recurrent fluid accumulation and fibrin on OCT imaging; clinically detectable hemorrhage; or visual acuity loss were seen. Single anti-VEGF combined with PDT was considered if persistent exudative findings were seen in spite of two consecutive monthly injections.
The main outcome measure was the best-corrected visual acuity (BCVA) between the pre- and postoperative BCVA at 3, 6, and 12 months after the initial treatment. The BCVA was converted to the logarithm of the minimum angle of resolution (logMAR) equivalent for the statistical analysis. The secondary outcome was the comparison of the change in the central foveal thickness (CFT) and central choroidal thickness (CCT) at baseline, 3, 6, and 12 months. The recurrence rate and mean number of injections during the follow-up periods were also analyzed. Digital simultaneous FA and ICGA (SPECTRALIS Product Family Version 5.3; Heidelberg Engineering, Germany) and SD-OCT (Heidelberg Spectralis HRA + OCT; Heidelberg Engineering, Germany) have been used to evaluate these changes.
The pre- and postoperative visual acuity was compared using one-way ANOVA. CFT and CCT were also evaluated using the one-way ANOVA. The statistical analyses were performed using the Ekuseru-Toukei 2012 (Social Survey Research Information, Tokyo, Japan). P value < 0.05 was considered to denote statistical significance.
Results
The baseline characteristics and clinical data for each patient before and after treatment are shown in Table 1. Of the 10 patients included in the series, 8 were men and 2 were women. The patient age ranged 61–82 years (mean age, 71.9 ± 6.7 years). The mean GLD was 2138 ± 674 μm.
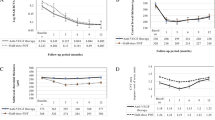
The mean logMAR visual acuity at the baseline was 0.12 ± 0.17. The mean logMAR BCVA values at 3, 6, and 12 months after the initial injection were 0.10 ± 0.16, 0.03 ± 0.18, and 0.01 ± 0.13, respectively. The postoperative BCVA at 12 months, but not at 3 and 6 months, showed a significant improvement, compared with the preoperative visual acuity (P = 1.000, P = 0.076, and P = 0.010 at 3, 6, and 12 months, respectively) (Fig. 1).
The mean baseline CFT was 331 ± 93 μm. The mean CFT at 3, 6, and 12 months after the initial treatment was 219 ± 95, 231 ± 89, and 237 ± 72 μm, respectively. The mean CFT at 3, 6, and 12 months showed significant decreasing, compared with those at baseline (P < 0.001, respectively) (Fig. 2).
The mean CCT at baseline was 361 ± 74 μm. The mean CCT at 3, 6, and 12 months after the initial injection was 286 ± 89, 301 ± 87, and 310 ± 83 μm, respectively. The mean CCT at 3, 6, and 12 months had also decreased significantly compared with those at baseline (P < 0.001, respectively) (Fig. 3).
In the maintenance phase, 5 of the 11 eyes (45.5%) exhibited recurrence during the maintenance phase. The mean number of injections per eye was 3.9 ± 1.3 during the follow-up period. Only 1 eye showed persistent fluid in spite of continuous injections; therefore, anti-VEGF was switched from ranibizumab to aflibercept, and PDT was additionally administered.
No incidence of serious ocular adverse effects, such as endophthalmitis, rhegmatogenous retinal detachment, or any nonocular adverse events, occurred. Figures 4 and 5 show the cases of PNV treated with anti-VEGF combined with PDT.
The case of a 76-year-old man who was no recurrence in the maintenance phase. a Color fundus photograph shows the area of RPE alteration in the macula. The best-corrected visual acuity (BCVA) was 20/40. b Early-phase fluorescein angiography reveals hyperfluorescent area corresponding to type 1 neovascularization (NV). c Early-phase indocyanine green angiography exhibits dilated choroidal vessels (white arrowhead). d Optical coherence tomography (OCT) at baseline shows type 1 NV with pachyvessels (yellow arrowheads). The choroidal thickness (CCT) was 420 μm. e OCT angiography (OCTA) shows the flow signal of NV clearly. Combined therapy using ranibizumab was performed. f One year after the initial treatment, OCT shows the decrease of CCT to 365 μm without exudative changes. g OCTA shows persistent flow signal of NV. The patient’s BCVA improved to 20/20
A 69-year-old man who required one additional treatment with ranibizumab due to the poor response. a Color funds photograph shows the area of RPE alteration in the macula. The best-corrected visual acuity (BCVA) was 20/16. b Early-phase fluorescein angiography demonstrates hyperfluorescent area corresponding to type 1 neovascularization (NV). c Late-phase indocyanine green angiography shows focal hyperfluorescent spots with choroidal vascular hyperpermeability. d Optical coherence tomography (OCT) at baseline shows type 1 NV, and choroidal thickness is 379 μm. Combined therapy using ranibizumab was performed. e Three months after the initial treatment, OCT shows the decrease of central choroidal thickness to 323 μm without exudative changes. The BCVA was maintained at 20/16. f Seven months after the initial treatment, subretinal fluid recurred, and additional ranibizumab was administered. g Twelve months after the initial treatment, OCT shows no exudative changes, and choroidal thickness was 358 μm. The patient’s BCVA was maintained at 20/16
Discussion
Our study demonstrated that ranibizumab combined with full-dose PDT was well tolerated and had efficacy in improving vision for treatment-naïve PNV during the 1-year follow-up examination. Furthermore, combined therapy showed improving exudative findings and reduced CCT with low rate of retreatment. There were few previous reports to investigate the functional outcome and morphologic changes of anti-VEGF combined with PDT in treatment-naïve patients with PNV [13].
The etiology of PNV has not been identified and has often mimicked AMD. However, patients with PNV are reported to have no evidence of AMD, such as soft drusen or fundus tessellation [7]. Furthermore, a recent report described that PNV was genetically different from neovascular AMD [14]. The current understanding of the pathogenesis of PNV involves the pachychoroid-related spectrum of diseases [4,5,6] includingCSC [15, 16] and polypoidal choroidal vasculopathy (PCV) [5, 7]. PNV occurs due to a pachychoroid-driven process involving choroidal congestion and CVH [7]. These changes can cause compression of the choriocapillaris, leading to a progression of type 1 NV through ischemic mechanism related to increased VEGF. Therefore, it is reasonable that anti-VEGF agents would be effective in suppressing type 1 NV due to PNV, resulting in improved exudative findings.
Furthermore, regarding PCV, part of the pachychoroid disease spectrum, Maruko et al. reported that PDT has reduced choroidal thickening [12]. The additional performance of PDT decreases the choroidal thickness, potentially leading to the suppression of CVH and mechanical pressure of pachyvessels to the RPE itself. Therefore, we expected the synergistic effect of anti-VEGF agents and PDT for PNV treatment.
Some patients with PNV need frequent anti-VEGF retreatment in the maintenance phase. A previous report has described that 64% (35 of 54 eyes) required additional treatment with anti-VEGF (ranibizumab and aflibercept) after the maintenance phase during the 12-month follow-up [10]. Another study has reported that 59% (13 of 22 eyes) needed additional treatment with anti-VEGF monotherapy [11]. In this study, 45.5% (5 of 11 eyes) showed that recurrence during the maintenance phase was lower than that in previous studies. The EVEREST II trial for PCV patients showed that the combined therapy of ranibizumab and PDT was superior to ranibizumab monotherapy in BCVA with fewer injections (4 versus 7 during 1 year) [17]. The Fujisan study in Japan also showed that initial PDT group led to significantly fewer additional ranibizumab treatments in the maintenance phase than later PDT group [18]. Combination therapy, especially using PDT as the initial treatment, may help reduce the treatment burden not only in patients with PCV but also in those with PNV.
The limitations of this study include its retrospectively nature and its small sample size. Furthermore, there was the lack of a control group of patients who had anti-VEGF monotherapy. The results of the current study require validation by further comparative studies involving a larger sample size. Finally, genetic differences between Japanese and Caucasian patients may underlie. Therefore, results in this study are possible to apply to a relatively homogenous Asian population; however, the same results may not apply to Caucasian patients with the same lesions.
In conclusion, ranibizumab combined with full-dose PDT was well tolerated and a highly effective treatment option in treatment-naïve patients with PNV. Combination therapy might also reduce the treatment burden with fewer injections in patients with PNV.
References
Wong WL, Su X, Li X et al (2014) Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2:e106–e116
Gass JD (1994) Biomicroscopic and histopathologic considerations regarding the feasibility of surgical excision of subfoveal neovascular membranes. Am J Ophthalmol 118:285–298
Grossniklaus HE, Gass JD (1998) Clinicopathologic correlations of surgically excised type 1 and type 2 submacular choroidal neovascular membranes. Am J Ophthalmol 126:59–69
Dansingani KK, Balaratnasingam C, Klufas MA et al (2015) Optical coherence tomography angiography of shallow irregular pigment epithelial detachments in pachychoroid spectrum disease. Am J Ophthalmol 160(1243–54):e2
Balaratnasingam C, Lee WK, Koizumi H et al (2016) Polypoidal choroidal vasculopathy: a distinct disease or manifestation of many? Retina 36:1–8
Dansingani KK, Balaratnasingam C, Naysan J et al (2016) En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina 36:499–516
Pang CE, Freund KB (2015) Pachychoroid neovasculopathy. Retina 35:1–9
Rosenfeld PJ, Brown DM, Heier JS et al (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355:1419–1431
Heier JS, Brown DM, Chong V et al (2012) Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 119:2537–2548
Jung BJ, Kim JY, Lee JH et al (2019) Intravitreal aflibercept and ranibizumab for pachychoroid neovasculopathy. Sci Rep 9:2055
Cho HJ, Jung SH, Cho S et al (2019) Intravitreal anti-vascular endothelial growth factor treatment for pachychoroid neovasculopathy. J Ocul Pharmacol Ther 35:174–181
Maruko I, Iida T, Sugano Y et al (2011) Subfoveal retinal and choroidal thickness after verteporfin photodynamic therapy for polypoidal choroidal vasculopathy. Am J Ophthalmol 151(594–603):e1
Matsumoto H, Mukai R, Kikuchi Y et al (2020) One-year outcomes of half-fluence photodynamic therapy combined with intravitreal injection of aflibercept for pachychoroid neovasculopathy without polypoidal lesions. Jpn J Ophthalmol 64:203–209
Miyake M, Ooto S, Yamashiro K et al (2015) Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep 5:16204
Warrow DJ, Hoang QV, Freund KB (2013) Pachychoroid pigment epitheliopathy. Retina 33:1659–1672
Fung AT, Yannuzzi LA, Freund KB (2012) Type 1 (sub-retinal pigment epithelial) neovascularization in central serous chorioretinopathy masquerading as neovascular age-related macular degeneration. Retina 32:1829–1837
Koh A, Lai TYY, Takahashi K et al (2017) Efficacy and safety of ranibizumab with or without verteporfin photodynamic therapy for polypoidal choroidal vasculopathy: a randomized clinical trial. JAMA Ophthalmol 135:1206–1213
Gomi F, Oshima Y, Mori R et al (2015) Initial versus delayed photodynamic therapy in combination with ranibizumab for treatment of polypoidal choroidal vasculopathy: the Fujisan study. Retina 35:1569–1576
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Yokohama City University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kitajima, Y., Maruyama-Inoue, M., Ito, A. et al. One-year outcome of combination therapy with intravitreal anti-vascular endothelial growth factor and photodynamic therapy in patients with pachychoroid neovasculopathy. Graefes Arch Clin Exp Ophthalmol 258, 1279–1285 (2020). https://doi.org/10.1007/s00417-020-04661-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04661-4