Abstract
Purpose
To explore a new classification scheme for acute ocular burns.
Methods
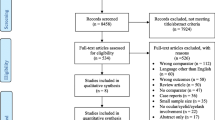
Medical records of 345 patients (450 eyes) with acute ocular burns treated at Shandong Eye Institute between January 2013 and January 2018 with a 12-month minimum follow-up were retrospectively reviewed. A total of 8 parameters in the acute phase were evaluated and graded on a scale from 0 to 3 according to their severity.
Results
The key factors affecting the prognosis of acute ocular burns were conjunctival involvement (386 eyes, 85.8%), corneal epithelial defect (349 eyes, 77.6%), and limbal ischemia (244 eyes, 54.2%). Visual acuity in 181/450 eyes (40.2%) was worse than 6/60. The injury severity of the cornea, limbus, bulbar conjunctiva, eyelid, and fornix and intraocular signs in the acute phase was significantly correlated with the logarithm of the minimum angle of resolution (logMAR) visual acuity (correlation coefficient [R] 0.481–0.933, P < 0.0001) and corneal opacification, neovascularization, and symblepharon scores in the stable phase (R 0.513–0.855, P < 0.0001). The mean total score for the 8 parameters in the acute phase was 5.34 ± 4.04 (range 0–14); higher scores indicated worse visual acuity (R = 0.899, P < 0.0001). The total score for acute-phase parameters was significantly correlated with that for the stable-phase parameters (R = 0.872, P < 0.0001).
Conclusions
The severity of acute-phase parameters is significantly correlated with the final visual outcome and prognosis. The new grading scheme can help clinicians more accurately analyze the degree of ocular burns, determine a reasonable treatment protocol, and rationally evaluate the prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ocular chemical and thermal burns constitute true ophthalmic emergencies and represent potentially blinding ocular injuries [1]. The reported prevalence of ocular chemical burns in developing countries ranges from approximately 1.25 to 4.4% [2, 3]. Chemical burns usually result from either alkaline or acidic agents. Thermal burns may be caused by accidents associated with firework explosions, boiling water, steam, or molten metal (primarily aluminum). Chemical and thermal injuries of the eye may result in extensive damage to the ocular surface, anterior segment, and posterior segment, leading to corneal opacification, ulcer perforation, corneal neovascularization, pterygium formation, symblepharon, and permanent vision loss [4, 5]. Acute interventions are directed at promoting ocular surface re-epithelialization, controlling the inflammatory response, preventing tissue melting, and reducing the incidence of complications, such as eye scarring and severe vision loss [6, 7].
The prognosis of ocular burns depends on the chemical and physical characteristics of the offending agent, its concentration and temperature, the duration of exposure, the impact force, and the extent of damage to corneal, limbal, and conjunctival tissues at the time of injury [4, 8]. Various prognostic classification schemes based on the extent of ocular damage are available [9]. The Roper-Hall classification system was originally proposed by Ballen [10] in 1964 and was later modified by Roper-Hall [11] in 1965 to provide prognostic guidelines based on the degree of corneal haze and the extent of limbal ischemia, which is currently the commonly used classification standard. Dua et al. [12] introduced a new modified classification system that not only considers the extent of limbal involvement in clock hours but also includes the percentage of conjunctival involvement.
The aim of this study was to initially explore a new classification scheme based on the clinical characteristics and treatment results of patients with acute ocular burns. This scheme more comprehensively considers the ocular surface state after ocular burns, including corneal, limbal, conjunctival, eyelid, and fornix involvement, intraocular hypertension, and anterior chamber inflammation, and facilitates a more detailed evaluation of patients with ocular burns to determine their prognosis.
Patients and methods
Patients
This study was approved by the Institutional Review Board of Shandong Eye Institute and adhered to the tenets of the Declaration of Helsinki. The medical records of patients with ocular chemical or thermal burns treated at our institution between January 2013 and January 2018 were reviewed retrospectively, and each patient completed a follow-up of at least 12 months. According to the medical records, data on the percentage of the corneal epithelial defect, the percentage of bulbar conjunctival involvement, clock hours of limbal ischemia, eyelid abnormalities, and fornix involvement (including intraocular hypertension and anterior chamber inflammation in the acute phase), as well as information corneal opacification, vascularization, and symblepharon in the stable phase, were collected to analyze the treatment methods and treatment outcomes of the patients.
Classification and grading of eye parameters
We considered 8 parameters, including corneal signs (the percentage of corneal epithelial defects and clock hours of limbal ischemia), conjunctival signs (the percentage of bulbar conjunctival involvement), eyelid signs (tarsal conjunctiva involvement and blepharon defects), fornix signs (fornix conjunctival involvement), and intraocular abnormalities (intraocular hypertension and anterior chamber inflammation), in the assessment of the clinical characteristics of ocular burns in the acute stage. Depending on the severity of the 8 parameters in the acute phase and the degree of corneal opacification, vascularization, and symblepharon in the stable phase, the 11 parameters were assigned scores of 0, 1, 2, and 3. Then, the scores for the acute-phase parameters and stable-phase parameters were added to obtain a total score of 0–14 in the acute phase and 0–9 in the stable phase. A higher score in the acute phase corresponded to more severely affected eyes.
Scoring criteria for acute-phase parameters (within 1 week after injury)
Corneal epithelial defect: The percentage of the corneal epithelial defect was scored from 0 to 3, where 0 = no epithelial defect, 1 = an epithelial defect area smaller than 50%, 2 = an epithelial defect area of 50–100%, and 3 = an epithelial defect area of 100%.
Limbal involvement: The clock hours of limbal involvement were graded from 0 to 3, where 0 = no limbal involvement, 1 = fewer than 9 clock hours of limbal were involvement, 2 = 9–12 clock hours of limbal involvement, and 3 = 12 clock hours of limbal involvement.
Bulbar conjunctival ischemia: The percentage of bulbar conjunctival involvement was graded from 0 to 3, where 0 = no bulbar conjunctival involvement, 1 = less than 50% bulbar conjunctival involvement, 2 = 50–100% bulbar conjunctival involvement, and 3 = 100% bulbar conjunctival involvement.
Eyelid, fornix, and intraocular parameters were graded as follows:
Eyelids: 0 = no tarsal conjunctival involvement and no blepharon defect, 1 = the presence of only one of the above two signs, and 2 = the presence of both of the above signs at the same time.
Fornix parameters: 0 = no fornix conjunctival ischemia and 1 = fornix conjunctival ischemia.
Intraocular parameters: 0 = no intraocular hypertension or anterior chamber inflammation, 1 = the presence of only one of the above two signs, and 2 = the presence of both of the above signs at the same time.
Scoring criteria for stable-phase parameters (more than half a year after injury)
Cornea opacification: The severity of corneal opacification was graded from 0 to 3 [13], where 0 = a clear cornea with clearly visible iris details, 1 = partial obscuration of the iris details, 2 = poor visibility of the iris details with a barely visible pupil margin, and 3 = completely obscured iris and pupil details (Fig. 1).
Corneal neovascularization: The extent of corneal neovascularization was scored from 0 to 3 [13, 14], where 0 = no neovascularization, 1 = confined to the limbus of the cornea, 2 = extending up to the margin of the pupil, and 3 = extending beyond the margin of the pupil into the central cornea (Fig. 1).
Symblepharon: The extent of symblepharon was scored from 0 to 3 [15], where 0 = no symblepharon, 1 = limited to the conjunctiva, 2 = extending to the limbus, and 3 = extending to the cornea (Fig. 1).
Visual acuity
We categorized 450 eyes from 345 patients according to their visual acuity in the stable phase. Visual acuity was 6/20 or better in group 1 (n = 167 eyes), worse than 6/20 and up to and including 6/60 in group 2 (n = 102 eyes), and worse than 6/60 in group 3 (n = 181 eyes). The visual acuity for counting fingers, hand movements, and light perception was converted to 0.004, 0.002, and 0.001 [16], respectively, and the results were converted to the logarithm of the minimum angle of resolution (logMAR) visual acuity for statistical analysis.
Treatment method
The treatments included medication and surgery. Medical treatment: The obvious first step for treating patients diagnosed within 24 h after injury is to immediately and thoroughly irrigate the ocular surface to remove the offending agent. Conjunctival sac secretions should be collected for bacterial culture and drug sensitivity testing to determine the status of conjunctival sac bacteria and to prevent infections in eyes with epithelial defects. Commonly used drugs include (1) drugs that promote ocular surface repair (autologous serum once per hour and deproteinized calf blood extract eye gel 4 times per day); (2) drugs that improve local microcirculation in the eye (the heparin solution of 1000–2000 units per ml is usually topically administered every15–30 min for 3–5 days, until the limbal blood vessels become dilated); (3) antibiotics that prevent infections (0.5% levofloxacin eye drops 4 times a day, ofloxacin eye ointment one night before bed.); and (4) one or more medications to reduce elevated intraocular pressure (IOP). Surgical treatment: amniotic membrane transplantation can be performed repeatedly in patients with conjunctival ischemia and corneal epithelial defects until the corneal epithelial defect area is repaired and conjunctival ischemia is improved. If the corneal epithelium fails to heal after multiple amniotic membrane transplantation attempts, since the stroma tends to break down or palpebral fissure dysraphism may occur, tarsorrhaphy is required to promote the recovery and stability of the ocular surface.
Grading
Acute ocular burns were classified into three grades according to the clinical characteristics of the acute stage (Table 1).
Grade I was defined as follows: Percentage of corneal epithelial defects less than 50% (a score less than 1), no limbal involvement (a score of 0), a percentage of bulbar conjunctival involvement less than 50% (a score less than 1), and no eyelid abnormalities, fornix involvement or intraocular abnormalities (a score of 0). Most of the treatment methods were drugs and bandage lenses or amniotic membrane transplantation. The cornea remained transparent during the stable period without neovascularization or symblepharon (a score of 0). Visual acuity was equal to 6/20 or better, and the prognosis was very good.
Grade II was defined as follows: Percentage of corneal epithelial defect less than 100% (a score less than 3), fewer than 12 clock hours of limbal involvement (a score less than 3), a percentage of bulbar conjunctival involvement less than 100% (a score less than 3), and no eyelid abnormalities, fornix involvement, or intraocular abnormalities (a score of 0). The most common treatment was amniotic membrane transplantation. During the stable period, the cornea was slightly cloudy, and neovascularization and symblepharon occurred in a few patients. Visual acuity was worse than 6/20 and up to and including 6/60, and the prognosis was good.
Grade III was defined as follows: A complete corneal epithelial defect, 100% bulbar conjunctival involvement, 12 clock hours of limbal involvement (a score of 3), eyelid abnormalities (less than or equal to a score of 2), fornix involvement (less than or equal to a score of 1), and intraocular abnormalities (less than or equal to a score of 2). The treatment was tarsorrhaphy. Most patients exhibited corneal opacity, neovascularization, and symblepharon (less than or equal to a score of 3) at the stable phase and had a poor prognosis with a visual acuity worse than 6/60.
Statistical analysis
All statistical analyses were carried out with SPSS software version 24.0 (SPSS, Inc., Chicago, IL). Normally distributed data are shown as the mean values ± standard deviations. Spearman’s correlation coefficients (2-tailed) were used to evaluate whether the scores of the acute-phase parameters were correlated with logMAR visual acuity and the stable-phase parameters. The correlations of the total score of the 8 acute-phase parameters with logMAR visual acuity and with the total score of stable-phase parameters were also evaluated. The chi-square test was used to compare the scores of all 8 parameters among the 3 groups. A P value ≤ 0.05 was considered statistically significant.
Results
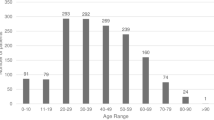
A total of 450 eyes of 345 patients with ocular burns, including 319 men (92.5%) and 26 women (7.5%), were enrolled in this study. The average age at injury and surgery was 42.23 ± 13.39 years (range, 1–73 years). Alkali burns were the most common ocular burns, which were noted in 222 eyes (49.34%), followed by thermal burns in 159 eyes (35.33%) and acid burns in 69 eyes (15.33%). Bilateral chemical injuries were observed in 105 patients (23.33%).
Acute-phase parameters
Corneal parameters: Among the 450 eyes examined, 223 eyes (49.6%) had a corneal epithelial defect area with scores of 2 and 3 (50–100% and 100%, respectively), and 244 eyes (54.2%) had different levels of limbal ischemia. Detailed information on the corneal parameters in the acute phase is summarized in Table 2.
Conjunctival parameters: Conjunctival involvement was scored as 2 and 3 (50–100 mm2 and 100 mm2, respectively) in 237 eyes (52.7%), and no ischemia was found in only 64 eyes (14.2%) (Table 2).
Eyelid, fornix, and intraocular parameters: Eyelid abnormalities were noted in 165 eyes (36.7%), including 110 eyes assigned a score of 1 and 55 eyes assigned a score of 2. A total of 154 eyes (34.2%) had fornix conjunctival ischemia. We found intraocular abnormalities in 85 eyes (18.9%), intraocular hypertension in 45 eyes (10%), and anterior chamber inflammation in 21 eyes (4.7%), with a score of 1 in 66 eyes and 2 in 19 eyes (Table 2).
Stable-phase parameters
Corneal opacification: Only 169 eyes (37.6%) had a clear cornea. Corneal neovascularization: No corneal neovascularization was observed in 334 eyes (74.2%). The score for corneal neovascularization was 1 in 15 eyes, 2 in 40 eyes (8.9%), and 3 in 61 eyes (13.6%). Symblepharon: No symblepharon was observed in 325 eyes (72.2%), and only 20 eyes (4.4%) had a score of 3 (Table 3).
Treatment method
Of the 450 eyes examined, 63 eyes (14%) were treated with medicine and bandage lenses, 250 eyes (55.6%) were treated with amniotic membrane transplantation, and 137 eyes (30.4%) were treated with amniotic membrane transplantation and tarsorrhaphy.
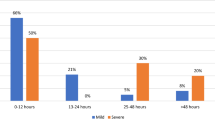
Visual acuity
Among the 450 eyes examined, only 167 eyes (37.1%) had a visual acuity equal to 6/20 or better, 102 eyes (22.7%) had a visual acuity worse than 6/20 and up to and including 6/60, and 181 eyes (40.2%) had a visual acuity worse than 6/60 (Table 4).
Correlations between visual acuity, stable-phase, and acute-phase parameters
We compared the acute-phase parameter score between the three groups of visual acuity (equal to 6/20 or better, worse than 6/20 and up to and including 6/60, and worse than 6/60) and the stable-phase parameter score and found that the score differences were statistically significant.
We estimated the correlation coefficient (R) between the visual acuity of the 450 eyes and the severity grade scored from 0 to 3. We found that all 8 acute-phase parameters were significantly correlated with logMAR visual acuity, with R ranging from 0.481 to 0.933 (P < 0.0001) (Table 5).
The scores for all the parameters in the acute phase were significantly correlated with those in the stable phase, with R ranging from 0.513 to 0.855 (P < 0.0001) (Table 6).
The correlations of visual acuity and total score of stable-phase parameters with the total score of acute-phase parameters
The mean total score for the 8 parameters in the acute phase was 5.34 ± 4.04 (range 0–14). The mean total score for the 3 parameters in the stable phase was 2.66 ± 2.90 (range 0–9). As shown in Table 4, eyes with a higher total score in the acute phase had poorer vision. The average scores for the acute-phase parameters in the three groups were as follows: group 1, 1.38 (range, 0–8); group 2, 4.64 (range, 1–9); and group 3, 9.39 (range, 4–14). The average scores for the stable-phase parameters in the three groups were as follows: group 1, 0.05 (range, 0–3); group 2, 2.06 (range, 1–7); and group 3, 5.42 (range, 1–9). Pearson’s analysis clearly demonstrated that the total score for the acute-phase parameters was significantly correlated with logMAR visual acuity (R = 0.899, P < 0.0001, Fig. 2a) and the total score for the stable-phase parameters (R = 0.872, P < 0.0001, Fig. 2b).
Scatterplots depicting the correlations of the total score for the acute-phase parameters with logMAR visual acuity and the total score for the stable-phase parameters. The total score for the 8 acute-phase parameters showed significant positive correlations with logMAR visual acuity (R = 0.899, P < 0.0001) (a) and the total score for the stable-phase parameters (R = 0.872, P < 0.0001) (b)
Discussion
Eye injuries are the leading cause of blindness in China, with chemical and thermal burns accounting for 7.7 to 18.0% of eye injuries [4]. With the development of the chemical industry, the number of chemical and thermal burns has increased each year [17]. Recent survey data from the USA show that from January 1, 2010, through December 31, 2013, a total of 144 149 chemical ocular burns were diagnosed at 900 emergency departments nationwide [18]. In this study, we analyzed the medical records of patients with chemical and thermal burns treated at the Shandong Eye Institute between January 2013 and January 2018. According to the clinical characteristics of the patients in the acute phase, a classification system was preliminarily explored to assess the severity of patient conditions more objectively, summarize treatment effects, and finally propose a grading method.
Various prognostic classification systems based on the extent of ocular damage are available to determine appropriate treatments and predict outcomes [9,10,11]. Roper-Hall’s [10] classification of acute ocular burns is based on the original classification of Ballen [9], and little difference exists between these classification methods. Roper-Hall [10] classified all patients with 50–100% limbal ischemia into one group (grade IV) and predicted a similar prognosis for all such patients. This classification immediately leads to the problem of classifying an eye, for example, with corneal clinical features of one grade and conjunctival clinical features of another grade. Conjunctival and limbal injuries are also difficult to grade. These difficulties have also led to inconsistent treatment success rates reported in the literature [19, 20]. Dua et al. [12] recognized the problem of assessing limbal damage and proposed a quasi-analog scale to incorporate intergrade variations. These authors demonstrated that not all burns with 50–100% limbal ischemia will have the same prognostic outcome and suggested classifying these patients into different grades for more appropriate treatment.
One question that must be addressed is whether to base the grade of a burn on the most severe clinical feature or on a combination of ocular surface clinical features. A combination of three physical parameters (corneal, limbal, and conjunctival parameters), each with three levels, requires 27 possible combinations to avoid crossover. To avoid this complexity and without evidence to indicate a difference in prognosis, grading an injury according to the most severe physical sign seems reasonable. Limbal stem cells are the source of corneal epithelial regeneration, and limbal ischemia can reflect the extent and severity of limbal stem cell injury and is the most important prognostic factor in ocular chemical or thermal injuries [21]. The presence of residual conjunctival epithelium in the eye is a better prognostic indicator than the complete loss of corneal, limbal, and conjunctival epithelium [11, 22]. In this study, we referred to Roper-Hall [10] and Dua’s [12] classifications of acute ocular burns and used corneal epithelial defects, limbal ischemia, and bulbous conjunctival involvement as the main parameters while increasing the importance of eyelid abnormalities, fornix involvement, intraocular pressure, and anterior chamber inflammation at the time of injury, which were divided into 8 physical parameters. We used a simple method to grade the severity of acute symptom parameters and scored these variables to reflect whether their involvement was mild, moderate, or severe.
In our study, conjunctival involvement (386 eyes; 85.8%), corneal epithelial defects (349 eyes; 77.6%), and limbal ischemia (244 eyes; 54.2%) were the key factors affecting the prognosis of acute ocular burns and significantly affecting the vision of patients (R > 0.481, P < 0.0001). These findings are consistent with those of previous studies [10, 11]. Eyelid abnormalities, including tarsal conjunctival ischemia, blepharon defects, and associated eyelid burns, can result in lid shortening, rigidity, and contractures, leading to exposure keratitis and mechanical damage to the cornea, which are usually associated with a poor prognosis. Fornix involvement represents fornix conjunctival ischemia. In this study, we suggested dividing the conjunctival surface into bulbar, tarsal, and fornix areas to include the total area of involvement. Chemicals that reach the trabecular meshwork result in elevated IOP, a compound effect that is easily overlooked [23]. The mechanism underlying this effect is acute injury leading to tissue damage, which then leads to aqueous outflow tract damage [23, 24]. Therefore, the IOP at the time of injury is closely related to the prognosis. The results of a recent study showed that within 24 h after the onset of chemical burns affecting the cornea, the initially released inflammatory cytokines (such as tumor necrosis factor α) can quickly reach the retina, resulting in ganglion cell apoptosis and other cell changes and increasing the damage to tissues in the eyes [25]. Hence, in this study, we included anterior chamber inflammation in the classification scheme to better predict the prognosis of patients.
In our study, an eye with 100% limbal and conjunctival involvement, was very likely to have a poor prognosis even with maximum intervention, and this finding differed from that with the Roper-Hall [10] classification, which predicts a similar prognosis for all patients with 50–100% limbal involvement and classified them into one group (grade IV). With the development of present management strategies, eyes with 50% or even 75% limbal involvement are very likely to have a good to fair prognosis. Furthermore, an ocular surface covered with conjunctival epithelium is in better condition than one with no epithelial cover. In eyes with total loss of the corneal epithelium and 100% limbal involvement, the presence of any surviving conjunctival epithelium is a prognostic indicator that is favorable compared with eyes with total loss of the corneal, limbal, and conjunctival epithelium. Therefore, the other 5 parameters, namely, tarsal conjunctiva involvement, blepharon defects, fornix conjunctival involvement, intraocular hypertension, and anterior chamber inflammation, although not the main criteria, were also important for the prognosis of acute ocular burns. In addition, our grading system also provides a standardized method for evaluating patients before corneal and ocular surface transplantation procedures. A purposeful approach to grading the severity of the preoperative condition of a patient may ultimately help predict long-term clinical outcomes for eyes postoperatively. In conclusion, our study analyzed the medical records of patients with ocular chemical or thermal burns at Shandong Eye Institute. According to the clinical characteristics at the time of injury, the extent of corneal epithelial defects, the percentage of bulbar conjunctival involvement, the clock hours of limbal ischemia, eyelid abnormalities, fornix involvement, intraocular hypertension, and anterior chamber inflammation, new grades for acute ocular burns were developed to determine accurate prognoses and treatment methods to provide a reference for clinicians.
References
Fish R, Davidson RS (2010) Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Curr Opin Ophthalmol 21:317–321
Xie YF, Tan YY, Tang S (2004) Epidemiology of 377 patients with chemical burns in Guangdong province. Burns 30:569–572
Hong JX, Qiu T, Wei AG, Sun XH, Xu JJ (2010) Clinical characteristics and visual outcome of severe ocular chemical injuries in Shanghai. Ophthalmology 117:2268–2272
Pfister RR (1983) Chemical injuries of the eye. Ophthalmology 90:1246–1253
Vajpayee RB, Shekhar H, Sharma N, Jhanji V (2013) Demographic and clinical profile of ocular chemical injuries in the pediatric age group. Ophthalmology 121:377–380
Gicquel JJ (2011) Management of ocular surface chemical burns. Br J Ophthalmol 95:159–161
Baradaran-Rafii A, Eslani M, Haq Z, Shirzadeh E, Huvard MJ, Djalili AR (2017) Current and upcoming therapies for ocular surface chemical injuries. Ocular Surface 15:48–64
Sharifipour F, Baradaranrafii A, Idani E, Zamani M, Bonyadi MHJ (2011) Oxygen therapy for acute ocular chemical or thermal burns: a pilot study. Am J Ophthalmol 151:823–828
Gupta N, Kalaivani M, Tandon R (2011) Comparison of prognostic value of Roper Hall and Dua classification systems in acute ocular burns. Br J Ophthalmol 95:194–198
Ballen PH (1964) Treatment of chemical burns of the eye. Eye Ear Nose Throat Mon 43:57–61
Roper-Hall MJ (1965) Thermal and chemical burns. Trans Ophthalmol Soc UK 85:631–653
Dua H, King A, Joseph A (2001) A new classification of ocular surface burns. Br J Ophthalmol 85:1379–1383
Sotozono C, Ang LPK, Koizumi N, Higashihara H, Ueta M, Inatomi T, Yokoi N, Kaido M, Dogru M, Shimazaki (2007) New grading system for the evaluation of chronic ocular manifestations in patients with Stevens–Johnson syndrome. Ophthalmology 114:1294–1302
Basu S, Mohan S, Bhalekar S, Singh V, Sangwan V (2018) Simple limbal epithelial transplantation (SLET) in failed cultivated limbal epithelial transplantation (CLET) for unilateral chronic ocular burns. Br J Ophthalmo bjophthalmol-2017-311506
Basu S, Sureka SP, Shanbhag SS, Kethiri AR, Singh V, Sangwan VS (2016) Simple limbal epithelial transplantation: long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology 123:1000–1010
Cheng J, Qi X, Zhao J, Zhai HL, Xie LX (2012) Comparison of penetrating keratoplasty and deep lamellar keratoplasty for macular corneal dystrophy and risk factors of recurrence. Ophthalmology 120:34–39
Li FM, Xie LX (2014) Chinese ophthalmology. Beijing, China
Haring RS, Sheffield ID, Channa R, Canner JK, Schneider EB (2016) Epidemiologic trends of chemical ocular burns in the United States. Jama Ophthalmol 134:1119–1124
Meller D, Pires RT, Mack RJ, Figueiredo F, Heiligenhaus A, Park WC, Prabhasawat P, John T, McLeod SD, Steuhl KP (2000) Amniotic membrane transplantation for acute chemical or thermal burns. Ophthalmology 107:980–989
Dua HS, Azuara-Blanco A (2000) Discussion on amniotic membrane transplantation for acute chemical or thermal burns. Ophthalmology 107:990
Le QH, Chen Y, Wang X, Li YM, Hong JX, Xu JJ (2011) Vision-related quality of life in patients with ocular chemical burns. Invest Ophthalmol Vis Sci 52:8951–8956
Westekemper H, Figueiredo FC, Siah WF, Wagner N, Steuhl KP, Meller D (2016) Clinical outcomes of amniotic membrane transplantation in the management of acute ocular chemical injury. Br J Ophthalmol 101:103–107
Lin MP, Ekşioğlu Ü, Mudumbai RC, Slabaugh MA, Chen PP (2012) Glaucoma in patients with ocular chemical burns. Am J Ophthalmol 154:481–485
Cabalag MS, Wasiak J, Syed Q, Paul E, Hall AJ, Cleland H (2014) Early and late complications of ocular burn injuries. J Plast Reconstr Aesthet Surg 68:356–361
Dohlman CH, Cade F, Regatieri CV, Zhou C, Lei F, Crnej A, Harissi-Dagher M, Robert MC, Papaliodis GN, Chen D, Aquavella JV (2018) Chemical burns of the eye: the role of retinal injury and new therapeutic possibilities. Cornea 37:248–251
Funding
This study was funded by the National Science Foundation of Shandong Province (ZR2017BH026).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, F., Cheng, J., Zhai, H. et al. Correlation analysis of the clinical features and prognosis of acute ocular burns—exploration of a new classification scheme. Graefes Arch Clin Exp Ophthalmol 258, 147–155 (2020). https://doi.org/10.1007/s00417-019-04525-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04525-6