Abstract
Purpose
To evaluate a visual acuity test (VAT) with unexpected optotypes to detect malingering.
Methods
We tested two groups. Group 1 consisted of 20 individuals with normal best corrected visual acuity (BCVA). Group 2 included participants with ocular diseases and reduced BCVA. All subjects underwent a VAT proposed by Gräf and Roesen to assess suspected malingering. This test used 36 charts with one Landolt-C per page. The first 20 optotypes were Landolt-Cs, while at positions 21, 26, 30, and 34 closed rings were presented. The testing distance was adapted to 50% of the test person’s visual acuity. The test person was requested to name the gap direction of the Landolt-C within 3 s. The complete testing conversation was recorded digitally to determine response latency for each optotype from the audio tracks.
Results
The average response time was 0.46 s in group 1 and 0.45 s in group 2 for the first 20 Landolt-Cs. In both groups the response time was significantly extended (p < 0.05) for the first closed ring compared to the mean of the first 20 Landolt-Cs, (group 1: 2.9 s; group 2: 2.3 s). The following three closed rings had also longer response times. However, these differences were not significant.
Conclusions
Our results suggest that the proposed test may be helpful to evaluate ocular malingering. The testing procedure appeared to be feasible and showed good repeatability. The fast training effect may be a limitation for malingering detection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
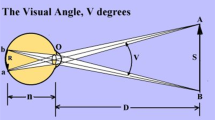
Testing visual acuity (VA) is a major medical assessment in ophthalmology. VA is tested by presenting optotypes at a standardized distance from the person whose vision is being tested. For maximum contrast, optotypes are usually black test symbols against a white background. Common optotypes for adults are Snellen letters, Landolt-C and Sloan letters in ETDRS charts. The main disadvantage of all these tests is that the examiner must rely on the patient’s compliance, which might be subject to individual manipulation. If VA does not correlate with the morphological and other objective findings, it can be necessary to check the validity of VA statements. It is not easy to discriminate disease that is morphologically not apparent such as occult macular dystrophy [1] from malingering as a possible reason for an obvious VA reduction. Malingering patients try to create or exaggerate symptoms in order to pretend being sick or sicker than they are. Common reasons for malingering are financial compensation, social privileges, or receiving attention by their environment. It is, therefore, not surprising that visual loss was the most frequent feigned symptom (74%) in a retrospective analysis of 344 ophthalmological independent medical examinations (IME) for detecting malingering [2]. A patient who is malingering may attempt to receive a fast diagnosis to achieve optimal therapy or prevent not being taken seriously.
Clinical assessment of malingering presents a challenge for ophthalmologists. Procedures to objectify visual testing are reported such as stochastic tests [3], optokinetic tests for example ophthalmoscopy by Kotowski [4], Teller Acuity Cards [5], imaging (i.e. OCT), electrophysiological diagnostics, spatial orientation, perimetry [6], and visual evoked potentials [7]. Most of these methods require specialized technical equipment. To assess visual malingering without the need for expensive examination devices, Gräf & Roesen proposed a practical acuity test with unexpected visual stimuli [8, 9]. In a VA test with 32 Landolt-Cs they included four additional closed rings of the same size. The test person’s responses were documented in a written response sheet and the voice was recorded in digital audio files. In their first report two volunteers showed longer reaction times for the closed ring compared to the Landolt-Cs [8]. In the second study the authors included 20 pseudomalingerers and 15 patients believed to be true malingerers [9]. It is obvious that any kind of malingering strategy can confound both the responses to the Landolt-C and the reaction induced by a surprise component. However, we found no normative study that determined standard values for non-malingering healthy subjects. Therefore, the aims of our study were the evaluation of this VA test in non-malingering individuals to assess normal values which characterize surprise and to test the applicability of this test in clinical routine.
Material and methods
The data in this study were collected from 40 volunteers. They were divided into two groups. Group 1 consisted of 20 subjects (12 women, 8 men) with normal BCVA (≥1.0). Group 2 included 20 patients (12 women, 8 men) with reduced BCVA (0.2–0.63). Vision loss was caused by age-related macular degeneration, cataracts, retinal detachment, uveitis, and keratitis. The participants were not selected by age or sex, but by VA and the presence of ocular disease. They were informed about the purpose and assessments of the study and gave their written informed consent. Local ethics committee approval was obtained to carry out this evaluation. The testing procedure was performed as proposed by Gräf & Roesen [8, 9]. All 36 optotypes were presented on pages (spiral-pad, EN ISO 216/DIN A4 210 mm × 297 mm) (Fig. 1) with one optotype per page. According to DIN 58220/EN ISO 8596 (German Industry Norms DIN 1998) Landolt-Cs were chosen for the test [10]. All Landolt-Cs had the same dimensions, where the diameter was 14.5 mm. The stroke width and the size of the gap were equal to one fifth of the diameter. This size corresponds to VA level 0.1 at a distance of 1.0 m. To perform the test at the VA level 0.32 (0.5 logMAR) the test distance had to be 3.2 m, for example. The first 20 Landolt-Cs were opened at top, bottom, left, or right. Beginning with the 21st optotype, four closed rings were inserted between the Landolt-Cs on page 21, 26, 30, and 34. This testing procedure offered each test person a habituation period with the first 20 Landolt-Cs, while the first closed ring (optotype number 21) was regarded as an unexpected optotype. To compare differences between the response time to closed rings and Landolt-Cs all responses were documented in written form and recorded digitally. A response sheet as proposed in the original paper [8, 9] was used for written documentation (Fig. 1). We performed the digital audio recording with a microphone (Philips SBC ME570) and a free-ware audio-program (Audacity, version 2.0.2) on a common laptop. The technical setup was intentionally kept as simple as possible to offer a feasible testing procedure. The VA of each test person was determined by decimal progression chart (DEC) with Landolt-Cs [11, 12] before using Gräf and Roesen’s test. The optotypes in their study were presented at a distance that corresponded to 50% of the VA from the DEC or presumed true acuity, respectively. For example the test distance was set to 5 m (corresponding to VA level 0.5) for a subject with VA 1.0. Reducing the test distance is essential to make sure that the test person can easily identify the optotypes. All test persons had to indicate the direction of the Landolt-C’s gap within 3 s and were instructed to respond to every optotype, if necessary by guessing the direction. Test conditions and procedures were equal for both groups. To avoid bias caused by illumination, reflections and scattered light, all evaluations were performed in the same examination room. For illumination a mix of moderate daylight (windows half covered) in addition to fluorescent tubes was chosen. This kind of illumination appeared to be the most practical way of avoiding unfavorable light effects on the test pad. We detected no reflections from any position in front of the spiral pad. The optotypes on the pad were consecutively numbered. The examiner announced the respective number to highlight the start of the presentation in the audio track. Response latency was defined by the time between optotype presentation and the corresponding response in the digital audio track (Fig. 2).
Screenshot of digital documentation with the free audio recorder Audacity. The response latency was determined by this procedure: a) identification of examiner’s voice, b) identification of test person’s voice, c) indicating the period between question and response, and d) the software calculated and displayed the length of period c, which was taken as response latency in seconds
Response times of the four closed rings at position 21, 26, 30, and 34 were compared with the mean answering time of the first 20 Landolt-Cs using non-parametric tests (Wilcoxon-Test).p-values <0.05 were considered statistically significant.
To assess individual scatter of the response times we compared the response time at position 21 (first closed ring) with the maximum response time for positions 6 to 20.
Gräf and Roesen proposed to document physical or verbal reactions indicating indecision or hesitation in a checkbox below each optotype (Fig. 1) [8, 9]. We found no signs of indecisive behavior or hesitation in the responses of all participants.
Results
The response times of the closed rings were longer compared to the first 20 Landolt-Cs. Table 1 presents an overview of the test statistics. Response times to the first closed ring were significantly longer, whereas the following three closed rings showed longer response times without statistical significance. These results appeared in group 1, and were consistently confirmed in group 2.
A detailed overview of the response times of all optotypes is given in Fig. 3 for group1. It remained at a constant level for Landolt-Cs throughout the entire testing period. The results of group 2 are shown in Fig. 4. In this group the response times of the first five Landolt-Cs were longer, while all other Landolt-Cs had constant levels similar to group 1.
Box plot of individual response times of group 1: healthy subjects with normal visual acuity (n = 20). The increased reaction times to the closed rings at positions 21, 26, 30, and 34 are highlighted by gray bars. Maximum at position 21 (20 s) is not shown. Boxes indicate interquartile range (IQR) and median, whiskers indicate 1.5 IQR, circles represent outliers >1.5 IQR, asterisks identify far outliers >3 IQR
Box plot of individual response times of group 2: subjects with ocular diseases and reduced visual acuity (n = 20). The increased reaction times to the closed rings at positions 21, 26, 30, and 34 are highlighted by gray bars. Boxes indicate interquartile range (IQR) and median, whiskers indicate 1.5 IQR, circles represent outliers >1.5 IQR, asterisks identify far outliers >3 IQR
A detailed overview of individual results is shown in Table 2. The number of cases with response times at position 21 exceeding the maximum of response times for positions 6 to 20 was 16 (80%) in group 1 and 14 (70%) in group 2.
Discussion
In our study we analyzed a VA test to identify malingering with closed rings as unexpected optotypes proposed by Gräf and Roesen [8, 9]. We performed the test in two groups: volunteers with normal BCVA (group 1) and co-operative patients with reduced BCVA (group 2). The aim of our analysis was to determine normative values for response times of closed rings by examining non-malingering subjects. In addition, we determined clinical feasibility of the testing procedure. Regarding the times to respond to closed rings we found differences compared to Landolt-Cs. The response time was significantly increased for the first closed ring (Table 1). The following three closed rings had also longer times compared to Landolt-Cs, but without statistical significance. We assume that this result was caused by a rapid training effect: the first closed ring surprised the subjects, whereas the following closed rings can be regarded as less unexpected. While the mean response time to the first closed ring was significantly increased, five of the subjects in each group had normal individual response times. This shows that the test can be false negative, particularly when exclusively focusing on the response time. On the other hand it is very likely that an increased time to respond signifies surprise.
To assess the variability of individual responses we compared the response time at position 21 (first closed ring) with the maximum response time for positions 6 to 20. Assuming that response times exceeding the maximum at positions 6 to 20 can be considered conspicuous we were able to identify 16 cases in group 1 and 14 cases in group 2 with substantial latency at the first position where a closed ring was presented. The possible presence of false positive responses has to be considered. A false positive result would be extended reaction time for position 21 despite factual inability to recognize the optotypes. The likelihood of false positives was around 0.06 (1/17) in this setting. It remained uncertain, if a single latency can give enough evidence to definitely prove malingering. Consequently, we agree with Gräf and Roesen that the patients’ reactions to the unexpected optotypes and the amount of correct and false responses have to be included in the test evaluation.
Gräf and Roesen instructed 19 volunteers to pretend malingering. They reported that 14 malingerers were detected with their test [9]. Verbal reactions (“What’s that?”) or physical abnormalities (raised eyebrows) uncovered malingering in 10 individuals. In contrast to those results physical or verbal signs of hesitation were absent in all participants of our study. This might be explained by the fact that surprise is a complex phenomenon. Latencies and behavioral responses largely depend on knowledge of the test, expectation, personality, and intelligence. These characteristics are subject to individual variation.
To evaluate the test feasibility and performance in a clinical environment we not only included normal vision volunteers but also patients with reduced VA. In both groups the test showed good reliability and repeatability. The only difference was a short adaptation period in the patients group, where the response times of the first five Landolt-Cs at the beginning of the test were longer but without being significant. However, this fact illustrates that it might be difficult to discriminate false positive time values from increased response times caused by surprise. Initial adaption was also reported from Gräf & Roesen [9]. They suggested to add one additional Landolt-C at the beginning of the test and to exclude it from the analysis. Our results suggest that this method is not sufficient because of larger individual variations in the patients who needed up to the first three optotypes to adapt.
A further aspect remains unclear in the original paper [8, 9]. The authors regarded the reaction to the first closed ring conspicuous if it was longer than any previous latency. This was the case in six of 19 pseudomalingerers compared to 15 subjects in group 1 and 10 in group 2 of our study. The following closed rings at positions 26, 30, and 34 were not considered in the analysis – meaning that their presentation was in fact not necessary. In our study, besides the 16 (group 1) and 14 (group 2) subjects with response times greater than maximum response times (scenario using response times at positions 6 to 20), we found one more subject meeting this criteria at least once for closed rings at positions 26, 30, and 34 (data not shown). Hence, increased response times at these positions could be used as additional information for strengthening conclusions about potential malingering and for improving sensitivity and/or specificity of the test. It should be mentioned that post hoc changes in evaluation criteria are not legitimate in a clinical setting.
In Gräf & Roesen’s study response latencies of patients believed to be malingerers were only estimated by the examiner by counting silently [9]. Estimating time intervals is subject to intra-observer variation which might have biased the results. Regarding response times it is not possible to compare our results with the original study because statistical data about latencies was not reported in their publication [9]. It is however very likely that our study on well cooperative individuals is not representative of the clinical situation in which response latencies might follow a different distribution and scatter of the response latencies is probably larger.
The concept of unexpectedness can be considered as a potential limitation of the test. Once published, the test principle using closed rings is not only available for examiners but also for malingerers. In our study we have already shown, how fast non-malingering subjects adapt to unexpected optotypes. Consequently, it is not very unlikely that malingerers might get access to the test characteristics and try to use this knowledge for further manipulation.
In our study the examiner announced each optotype number to indicate optotype presentation in the audio track. Variations between the examiner’s announcement and the turning of the page might be a potential source of bias. However, we were not able to find any relevant delays between the presenter’s voice and the turning of the page in the audio track.
Our study provides information that may help to better interpret a VA test to determine malingering with unexpected optotypes. The results of our present study suggest that the test proposed by Gräf and Roesen [8, 9] can be a valuable piece of the puzzle for the evaluation of malingering in VA testing. However, a real proof of malingering remains uncertain.
References
Kathol RG, Cox TA, Corbett JJ, Thompson HS (1983) Functional visual-loss – follow-up of 42 cases. Arch Ophthalmol 101:729–735
Schutz JS, Mavrakanas NA (2009) The value of the ophthalmological independent medical examination: analysis of 344 cases. Br J Ophthalmol 93:1371–1375. https://doi.org/10.1136/bjo.2009.160614
Roland J, Hirsch U, Heinrich SP, Bach M, Graef M (2010) A stochastic test for validity control of visual acuity statements. Ophthalmologe 107:47–54. https://doi.org/10.1007/s00347-009-1928-y
Kotowski H (1966) New device for the objective determination of visual acuity. Klin Monatsbl Augenheilkd 149:397–401
Teller DY, Morse R, Borton R, Regal D (1974) Visual-acuity for vertical and diagonal gratings in human infants. Vis Res 14:1433–1439. https://doi.org/10.1016/0042-6989(74)90018-2
Wilhelm H, Neitzel J, Wilhelm B, Beuel S, Ludtke H, Kretschmann U, Zrenner E (2000) Pupil perimetry using M-sequence stimulation technique. Invest Ophthalmol Vis Sci 41:1229–1238
Xu S, Meyer D, Yoser S, Mathews D, Elfervig JL (2001) Pattern visual evoked potential in the diagnosis of functional visual loss. Ophthalmology 108:76–80
Graf MH, Roesen J (2001) The airtight Landolt-C - a handy test in the diagnosis of suspected ocular malingering. Klin Monatsbl Augenheilkd 218:435–437. https://doi.org/10.1055/s-2001-16258
Graf MH, Roesen J (2002) Ocular malingering: a surprising visual acuity test. Arch Ophthalmol 120:756–760
Wesemann W, Schiefer U, Bach M (2010) New DIN norms for determination of visual acuity. Ophthalmologe 107:821–826
Bach M, Kommerell G (1998) Determining visual acuity using European normal values: scientific principles and possibilities for automatic measurement. Klin Monatsbl Augenheilkd 212:190–195
Loumann Knudsen L (2003) Visual acuity testing in diabetic subjects: the decimal progression chart versus the Freiburg visual acuity test. Graefes Arch Clin Exp Ophthalmol 241(8):615–618
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kröger, N., Jürgens, C., Kohlmann, T. et al. Evaluation of a visual acuity test using closed Landolt-Cs to determine malingering. Graefes Arch Clin Exp Ophthalmol 255, 2459–2465 (2017). https://doi.org/10.1007/s00417-017-3820-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3820-9