Abstract
Purpose
Worldwide, the most frequent cause of visual impairment is uncorrected refractive error. This analysis focused on the distribution and associations of refractive, corneal and ocular residual astigmatism.
Methods
As part of the Gutenberg Health study, a population-based cross-sectional study was conducted in the general population of Germany. A comprehensive ophthalmological examination including refraction, tonometry, and Scheimpflug imaging of the anterior cornea (Pachycam) was performed. In addition to the magnitude and type (with-the-rule, against-the-rule, oblique) of the refractive or corneal astigmatism, we calculated the vector components (J0, J45) of both astigmatisms and calculated the ocular residual astigmatism. We performed multiple quantile regression analysis to evaluate the factors associated with refractive, corneal and ocular residual astigmatisms.
Results
A total of 13,558 subjects (49% female) with a mean age of 54.0 years (range 35–74 years) were included in this study. The prevalence of refractive astigmatism (>1.0D) was 13.0% in right eyes and 12.0% in left eyes, and 85% of these subjects wore spectacles. The distribution of refractive astigmatism showed a two-peak distribution with high astigmatism for with-the-rule and against-the-rule astigmatism. The associated factors were corneal curvature, age and sex for the different astigmatisms (p < 0.001).
Conclusions
We analyzed the prevalence of different astigmatisms within a European population. We confirmed a shift with aging from with-the-rule to against-the-rule astigmatism to refractive and corneal astigmatism. Astigmatism has a large impact on visual perception; more than 85% of people with astigmatism over one diopter wore glasses for distance vision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, the most frequent cause of visual impairment is uncorrected refractive error [1]. The three most common reasons are myopia, hyperopia and astigmatism, which show different distributions in various ethnic groups [2, 3]. In an astigmatic eye, light is focused on two focal lines in different planes. For instance, the image is sharply focused on the retina in the horizontal orientation, but not in the vertical direction, requiring cylindrical rather than spherical correction. As a result, a low amount of astigmatism is known to improve uncorrected reading ability due to increased pseudo-accommodation in pseudophakic eyes, especially in the case of against-the-rule astigmatism [4, 5]. Oblique orientations or increased amount of astigmatism decrease reading ability [6]. With increasing astigmatism, vision is reduced in all viewing distances, whereas other forms of refractive error can be at least partially balanced by accommodation of viewing distance.
It is known from previous studies that the prevalence of refractive and corneal astigmatism increases with age [7, 8]. Additionally, a change in the astigmatic axis from with-the-rule to against-the rule astigmatism occurs mainly based on corneal changes, as analyzed in Asian populations [8, 9], whereas so far little is known about the prevalence of astigmatism and associated factors in Caucasians.
To fill this gap, this study analyzed the distribution of refractive and corneal astigmatism, in amount and orientation, in different age decades within a Caucasian population. Furthermore, we aimed to analyze the factors associated with different forms of astigmatism, including refractive, corneal and ocular-residual astigmatism, and to evaluate the underlying form for the shift in orientation over the years.
Materials and methods
The Gutenberg Health Study (GHS) is a prospective, population-based, observational cohort study conducted in the Rhine-Main region in Midwestern Germany that examined a total of 15,010 participants. This study sample was recruited from the GHS and included subjects with an age of 35 to 74 years at the time of examination between April 2007 and March 2012. The sample was randomly drawn from local governmental registry offices. The response rate was 60%. The cohort was stratified by gender, residence and decade of age. More details of the study setup are described in Höhn et al. [10]. As part of the individual examination, a comprehensive ophthalmological work-up, including slit-lamp examination, was conducted. Objective refraction (Humphrey Automated Refractor/Keratometer (HARK) 599, Carl Zeiss Meditec AG, Jena, Germany) and corneal Scheimpflug imaging (Pachycam, Oculus, Wetzlar, Germany) were completed to analyze the refractive and corneal status of the participants. Noncontact tonometry (Nidek NT-2000, Nidec Co, Japan) was performed to measure intraocular pressure.
This study was approved by the Ethics Committee of the state chamber of physicians of Rhineland-Palatinate and by local and federal data safety commissioners. In accord with the tenets of the Declaration of Helsinki, written informed consent was obtained from all participants prior to entering the study.
Exclusion criteria
Participants with previous intraocular or corneal surgery were excluded from this study analysis. For this analysis, 13,558 subjects (13,521 right eyes and 13,527 left eyes) were included.
Data collection
Three different types of astigmatism were investigated: refractive astigmatism (RA), corneal astigmatism (CA) and ocular-residual astigmatism (ORA). Analyses of astigmatism were conducted using negative cylinder power as a distinct variable. Refractive astigmatism was defined as astigmatism of the total eye, measured by objective refraction. Corneal astigmatism describes the astigmatic curvature of the cornea examined by Scheimpflug imaging, while ocular-residual astigmatism was calculated based on vector analysis and displays astigmatism not being caused by corneal astigmatism. Refractive and corneal astigmatism were decomposed into vector components using the power vector approach proposed by Thibos et al. [11]. This conversion of cylinder power and axis into its constituent vector components reflects both astigmatic characteristics and allows for the calculation of the ocular-residual astigmatism and its axis. Refractive and corneal astigmatism were decomposed into power vectors using the following formulas:
where α is the cylindrical axis and C is the negative cylinder power.
J0 represents the power vector matching the cylinder power of the vertical (90°) and horizontal (180°) meridians. Positive values correspond to with-the-rule (WTR) astigmatism, whereas negative values reflect against-the-rule (ATR) astigmatism. J45 is the power vector corresponding to the cylinder power of the oblique meridians (45° and 135°).
For determination of ocular-residual astigmatism, the difference in refractive and corneal astigmatism was calculated using the power vectors. The cylinder power of ocular-residual astigmatism was then computed using the following formula:
Cyl power = −2 * \( \sqrt[]{{J_0}^2+{J_{45}}^2} \).
Statistical analysis
The data were processed using statistical analysis software (R version 3.1.1 [2014–07-10]). Median, interquantile range, minimum and maximum were calculated for all primary and secondary variables. Mean and standard deviation were computed for variables exhibiting approximately normal distribution. Spearman Rank-correlation coefficients were computed for associations of vector components and for comparing right and left eyes. The orientation of astigmatism was grouped for 180° +/− 30° as with-the-rule astigmatism (WTR), for 90° +/− 30° as against-the-rule astigmatism (ATR), whereas 45° +/− 15° and 135° +/− 15° were regarded as oblique astigmatism.
First, the age-specific prevalence of refractive, corneal and residual ocular astigmatism was calculated. The age/sex-distribution of the German population from the year 2014 was used to estimate the overall standardized prevalence [12].
Multiple quantile regression was performed to evaluate associated factors due to skewed distribution of dependent variables. In the first model, age, sex and residence (urban/rural) were included as independent variables; the dependent variable was the amount of refractive, corneal or ocular residual astigmatism for the different statistical analyses. In the second model, age, sex, residence, refraction, corneal curvature (power of the steep axis), central corneal thickness and intraocular pressure were included as independent variables. In a binary logistic regression model, associated factors were investigated using refractive astigmatism as the dependent variable (more than −1.0 diopters of astigmatism), and age, sex, residence, refraction, corneal curvature, central corneal thickness and intraocular pressure as independent variables. Right and left eyes were analyzed separately, and the results were compared.
We performed a sensitivity analysis and excluded all eyes with corneal pathologies as observed in slit-lamp examination of the anterior segment. The previously reported regression models were carried out and results were compared.
This study was performed as an explorative study to analyze the prevalence of refractive, corneal and ocular residual astigmatism and the factors associated with these conditions. All p-values should be regarded as continuous parameters that reflect the level of evidence and are therefore reported exactly.
Results
This study included 13,558 subjects (13,521 right eyes and 13,527 left eyes) with a mean age of 54.0 +/− 9.0 years (range 35 to 74 years). A total of 1142 subjects were excluded as they had undergone previous ocular surgery, and data on 310 subjects were missing. Within this study population, 49.3% were women. The subjects with missing data did not differ from the included subjects with respect to age and sex.
Refractive astigmatism ranged from −8.00 to 0 diopters with a median of −0.50 diopter in both the right and left eyes. The prevalence in our study cohort was 13.0% (95% confidence interval (CI): 11.4% to 14.7%) for a refractive astigmatism of larger than −1.0 diopters in the right eyes and 12.0% (95%-CI: 10.5% to 13.7%) in the left eyes. Spectacle use for distance vision increased with refractive astigmatism and was higher in women than in men (Table 1). For corneal astigmatism larger than −1.0 diopters, the prevalence was 36.2% (95%-CI: 34.8% to 37.6%) for the right eyes and 36.9% (95%-CI: 35.5% to 38.3%) for the left eyes.
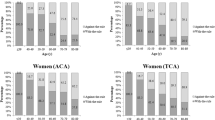
Corneal astigmatism was characterized by a median of −0.60 diopters in the right eyes and −0.70 diopters in the left eyes, with a minimum of −7.80 -and −7.60 diopters, respectively. The median ocular residual astigmatism was slightly lower, with −0.56 diopters in the right eyes and −0.58 diopters in the left eyes. Other refractive parameters are given in Table 1. The distribution of refractive astigmatism showed an accumulation of high astigmatism (more than −1 D) for with-the-rule (180° +/− 30°) and against-the-rule (90° +/− 30°), whereas higher corneal astigmatism (more than −1 D) mainly occurred in the with-the-rule position and higher ocular residual astigmatism (more than -1D) in the against-the-rule position (Fig. 1). Refractive astigmatism increased with aging (Fig. 2).
Comparing the right and left eyes, there was a moderate to high correlation in the amount of refractive astigmatism (r = 0.53, p < 0.001), the amount of corneal astigmatism (r = 0.59, p < 0.001) and the amount of ocular residual astigmatism (r = 0.41, p < 0.001). The astigmatism orientations, classified as with-the-rule, oblique or against-the-rule astigmatism, were similar in both eyes, as described in Table 2.
Regarding the vector components (J0 and J45), J0 served as an indicator of the amount of WTR or ATR astigmatism and was highly correlated between both eyes for refractive astigmatism (r = 0.67, p < 0.001), corneal astigmatism (r = 0.72, p < 0.001) and ocular residual astigmatism (r = 0.49, p < 0.001). J45 was an indicator of the amount of oblique astigmatism and showed a lower correlation between both eyes (refractive astigmatism: r = −0.37, <0.001; corneal astigmatism r = −0.45, <0.001; ocular residual astigmatism r = −0.29, p < 0.05). Interestingly, the J0 vector component of refractive and corneal astigmatism showed a negative correlation with age (refractive astigmatism: OD: r = − 0.25, p < 0.05, OS: r = −0.24, p < 0.05; corneal astigmatism: OD: r = − 0.23, p < 0.05, OS: r = − 0.23, p < 0.05), whereas the J45 vector component was not associated with age. This reflects the shift of with-the-rule astigmatism to against-the-rule astigmatism in both refractive and corneal astigmatism.
The factors associated with refractive astigmatism were examined by multiple quantile regression. The first model showed age and sex as factors associated with refractive astigmatism, whereas residence (rural/urban) was not associated with refractive astigmatism. Women had a slightly lower rate of refractive astigmatism (estimate of median in diopters for right eyes: 0.03, p = 0.005; for left eyes: 0.04, p < 0.001), and refractive astigmatism slightly increased with age (estimate for median per 10 years of age: −0.05 for right eyes and −0.05 for left eyes, p < 0.001). The second analysis model revealed sex and sphere as positively associated factors, whereas age and corneal power were negatively associated (Table 3).
Similar associated factors were found for analysis of corneal astigmatism, but with a different direction of association. The first model showed age (estimate in right eyes: 0.05, in left eyes: 0.06, p < 0.001) and sex (estimate in right eyes: −0.10, in left eyes: −0.06, p < 0.001) as factors associated with corneal astigmatism, whereas residence was not associated. The second analysis model showed age and IOP as positively associated factors, whereas sex and corneal power were negatively associated (Table 4).
Regarding ocular residual astigmatism, the first quantile regression model showed sex (estimate for right eyes: −0.05, for left eyes: −0.04, p < 0.001) and age (estimate in both eyes about −0.015, p < 0.001) as negatively associated factors. The second model revealed sex, corneal power and central corneal thickness as negatively associated factors (Table 5).
Logistic binary regression analysis of a high refractive astigmatism (larger than −1.0 diopters) revealed sex, sphere and corneal curvature as associated factors. Women had a refractive astigmatism of larger than −1.0 diopters with an OR = 0.7, p < 0.001. Each positive diopter of refraction was associated with a decrease in high refractive astigmatism with an OR = 0.9, p < 0.001, whereas a high corneal refractive power was associated with an increase in refractive astigmatism (Table 6).
Sensitivity analysis, excluding eyes with corneal pathologies (237 eyes), showed comparable findings for quantile regression analysis on refractive astigmatism, corneal astigmatism and ocular-residual astigmatism in the different models.
Discussion
This is the largest study within a European population analyzing the prevalence of different astigmatisms. Our study has shown that refractive astigmatism is prevalent in Europeans; 12.5% of the eyes studied had astigmatisms greater than one diopter. The impact of astigmatism on visual impairment is large; more than 85% of subjects with a refractive astigmatism of more than −1.0 diopter or larger wore glasses for distance vision. In addition, our study has demonstrated that refractive astigmatism is distributed in a two-peak fashion: one peak is at 180° (with-the-rule astigmatism), with astigmatism values up to –8.0 diopters, and the other peak is at 90° (against-the-rule astigmatism), with astigmatism values up to −7.75 diopters. Interestingly, these two peaks overlap with the distribution of anterior corneal and ocular residual astigmatism; anterior corneal astigmatism showed a peak in its distribution at 180°, and ocular residual astigmatism had a peak at 90°. Refractive astigmatism slightly correlated with age and increased by 0.05 diopters with each decade.
As previously shown in Asian and Australian populations [7, 9, 13,14,15], we found a statistically significant relationship between age and the orientation of refractive astigmatism, indicating a shift from with-the-rule astigmatism to against-the-rule astigmatism. Sanfilippo et al. published that this shift occurs after the age of 50 years in individuals with a previously relatively stable refractive astigmatism [7], and we were able to demonstrate this relationship over the entire study population with an age range of 35 years to 74 years. This may occur due to ocular changes summarized as either changes in the anterior corneal or in ocular residual astigmatism. Vector analysis of anterior corneal astigmatism showed a negative correlation between the straight vector and age indicating a shift from with-the-rule to against-the-rule astigmatism. In addition, the distribution of ocular residual astigmatism showed high astigmatic values for against-the-rule astigmatism, in contrast to the distribution of anterior corneal astigmatism. This leads to the assumption that the different components of ocular residual astigmatism [16], especially, (posterior corneal surface, lens, retinal surface) are of greater importance in high against-the-rule astigmatism and may gain importance during aging.
In our analysis, we evaluated factors associated with high refractive astigmatism (< −1.0 diopter). This analysis revealed that sex, refraction and corneal curvature are associated factors. These results indicate that women have a smaller probability of having visual impairment from high refractive astigmatism, whereas myopia and a steep anterior cornea are associated with an increased refractive astigmatism. Furthermore, data from the meta-analysis of genome-wide analysis studies have led to several putative loci (VAX2, PDGFRA) for astigmatism [17, 18] that are distinctly different from those for myopia and hyperopia [19]. Further research analyzing genetic associations with corneal astigmatism or vector components may lead to additional loci.
Although our study is a representative sample for the Rhine-Main region in Germany with an age range over three decades and a sample size of 15,010 subjects, its nature as a cross-sectional study may be considered to be a limitation. We will analyze age-dependent changes in a follow-up to this study. Second, we were not able to further analyze different aspects of ocular residual astigmatism and, therefore, were not able to distinguish between changes in the posterior cornea or in the lens. Third, as in previous studies, we did not measure cycloplegic refraction, which is a major limitation of our study, and our measurements may not reflect true refractive and residual astigmatism. Associations between refraction and astigmatism might be attenuated. Nevertheless, because myopic refraction is associated with increased refractive astigmatism, this might be of lesser importance. In addition, so far, we could not measure axial length and could not incorporate this factor into our analysis. To compensate for this, we incorporated refraction and corneal power in the multiple quantile regression model reflecting both corneal properties and total refraction. Fifth, our study had an age restriction from 35 to 74 years. Therefore, we can describe characteristics during only this stage of life and not during childhood development, youth or early adulthood. The study sample is undergoing a 5-year follow-up assessment, and we therefore expect to be able to answer questions concerning additional age-dependent changes in the future.
In conclusion, our study is the largest population-based study in Europe evaluating the distribution of refractive, corneal and ocular residual astigmatism. The analysis revealed that age, sex, spherical refraction and corneal power are factors associated with refractive astigmatism, whereas corneal astigmatism was associated with age, sex, corneal power and intraocular pressure. Considering previous findings from Asian and Australian population-based studies, our study suggests that a shift from with-the-rule astigmatism to against-the-rule astigmatism in older persons may be universal in all ethnicities.
References
Pascolini D, Mariotti SP (2012) Global estimates of visual impairment: 2010. Br J Ophthalmol 96:614–618. doi:10.1136/bjophthalmol-2011-300539
Cheng CY, Hsu WM, Liu JH, Tsai SY, Chou P (2003) Refractive errors in an elderly Chinese population in Taiwan: the Shihpai eye study. Invest Ophthalmol Vis Sci 44:4630–4638
Wolfram C, Hohn R, Kottler U, Wild P, Blettner M, Buhren J, Pfeiffer N, Mirshahi A (2014) Prevalence of refractive errors in the European adult population: the Gutenberg health study (GHS). Br J Ophthalmol 98:857–861. doi:10.1136/bjophthalmol-2013-304228
Trindade F, Oliveira A, Frasson M (1997) Benefit of against-the-rule astigmatism to uncorrected near acuity. J Cataract Refract Surg 23:82–85
Verzella F, Calossi A (1993) Multifocal effect of against-the-rule myopic astigmatism in pseudophakic eyes. Refract Corneal Surg 9:58–61
Kobashi H, Kamiya K, Shimizu K, Kawamorita T, Uozato H (2012) Effect of axis orientation on visual performance in astigmatic eyes. J Cataract Refract Surg 38:1352–1359. doi:10.1016/j.jcrs.2012.03.032
Sanfilippo PG, Yazar S, Kearns L, Sherwin JC, Hewitt AW, Mackey DA (2015) Distribution of astigmatism as a function of age in an Australian population. Acta Ophthalmol doi. doi:10.1111/aos.12644
Liu YC, Chou P, Wojciechowski R, Lin PY, Liu CJ, Chen SJ, Liu JH, Hsu WM, Cheng CY (2011) Power vector analysis of refractive, corneal, and internal astigmatism in an elderly Chinese population: the Shihpai eye study. Invest Ophthalmol Vis Sci 52:9651–9657. doi:10.1167/iovs.11-7641
Leung TW, Lam AK, Deng L, Kee CS (2012) Characteristics of astigmatism as a function of age in a Hong Kong clinical population. Optom Vis Sci 89:984–992. doi:10.1097/OPX.0b013e31825da156
Hohn R, Kottler U, Peto T, Blettner M, Munzel T, Blankenberg S, Lackner KJ, Beutel M, Wild PS, Pfeiffer N (2015) The ophthalmic branch of the Gutenberg health study: study design, cohort profile and self-reported diseases. PLoS One 10:e0120476. doi:10.1371/journal.pone.0120476
Thibos LN, Wheeler W, Horner D (1997) Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci 74:367–375
Statistisches Bundesamt (2016) GENESIS-Online Datenbank. Ergebnisse auf Grundlage des Zensus 2011, Wiesbaden. https://www-genesis.destatis.de/genesis/online;jsessionid=2AACC96482E846FFEDD35D7DD5069560.tomcat_GO_2_3?sequenz=suche&selectionname=Bevölkerung. Accessed 25 May 2015
Attebo K, Ivers RQ, Mitchell P (1999) Refractive errors in an older population: the Blue Mountains eye study. Ophthalmology 106:1066–1072. doi:10.1016/s0161-6420(99)90251-8
Asano K, Nomura H, Iwano M, Ando F, Niino N, Shimokata H, Miyake Y (2005) Relationship between astigmatism and aging in middle-aged and elderly Japanese. Jpn J Ophthalmol 49:127–133. doi:10.1007/s10384-004-0152-1
Hashemi H, Khabazkhoob M, Yekta A, Jafarzadehpur E, Emamian MH, Shariati M, Fotouhi A (2012) High prevalence of astigmatism in the 40- to 64-year-old population of Shahroud, Iran. Clin Experiment Ophthalmol 40:247–254. doi:10.1111/j.1442-9071.2011.02635.x
Alpins NA (1997) New method of targeting vectors to treat astigmatism. J Cataract Refract Surg 23:65–75
Lopes MC, Hysi PG, Verhoeven VJ, Macgregor S, Hewitt AW, Montgomery GW, Cumberland P, Vingerling JR, Young TL, van Duijn CM, Oostra B, Uitterlinden AG, Rahi JS, Mackey DA, Klaver CC, Andrew T, Hammond CJ (2013) Identification of a candidate gene for astigmatism. Invest Ophthalmol Vis Sci 54:1260–1267. doi:10.1167/iovs.12-10463
Fan Q, Zhou X, Khor CC, Cheng CY, Goh LK, Sim X, Tay WT, Li YJ, Ong RT, Suo C, Cornes B, Ikram MK, Chia KS, Seielstad M, Liu J, Vithana E, Young TL, Tai ES, Wong TY, Aung T, Teo YY, Saw SM (2011) Genome-wide meta-analysis of five Asian cohorts identifies PDGFRA as a susceptibility locus for corneal astigmatism. PLoS Genet 7:e1002402. doi:10.1371/journal.pgen.1002402
Simpson CL, Wojciechowski R, Oexle K, Murgia F, Portas L, Li X, Verhoeven VJ, Vitart V, Schache M, Hosseini SM, Hysi PG, Raffel LJ, Cotch MF, Chew E, Klein BE, Klein R, Wong TY, van Duijn CM, Mitchell P, Saw SM, Fossarello M, Wang JJ, Polasek O, Campbell H, Rudan I, Oostra BA, Uitterlinden AG, Hofman A, Rivadeneira F, Amin N, Karssen LC, Vingerling JR, Doring A, Bettecken T, Bencic G, Gieger C, Wichmann HE, Wilson JF, Venturini C, Fleck B, Cumberland PM, Rahi JS, Hammond CJ, Hayward C, Wright AF, Paterson AD, Baird PN, Klaver CC, Rotter JI, Pirastu M, Meitinger T, Bailey-Wilson JE, Stambolian D (2014) Genome-wide meta-analysis of myopia and hyperopia provides evidence for replication of 11 loci. PLoS One 9:e107110. doi:10.1371/journal.pone.0107110
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a conflict of interest with the study.
Financial support
“The Gutenberg Health Study is funded through the government of Rheinland-Pfalz („Stiftung Rheinland-Pfalz für Innovation“, contract AZ 961-386261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg-University of Mainz, and its contract with Boehringer Ingelheim, PHILIPS Medical Systems and Novartis Pharma, including an unrestricted grant for the Gutenberg Health Study. PSW and KAP are funded by the Federal Ministry of Education and Research (BMBF 01EO1003). Funders were involved in the development of the study design as scientific consultants. However, they played no role in data collection, analysis, decision to publish, or preparation of the manuscript.
Informed consent
This study was approved by the Ethics Committee of the state chamber of physicians of Rhineland-Palatinate and by local and federal data safety commissioners. In accord with the tenets of the Declaration of Helsinki, written informed consent was obtained from all participants prior to entering the study.
Rights and permissions
About this article
Cite this article
Schuster, A.KG., Pfeiffer, N., Schulz, A. et al. Refractive, corneal and ocular residual astigmatism: distribution in a German population and age-dependency - the Gutenberg health study. Graefes Arch Clin Exp Ophthalmol 255, 2493–2501 (2017). https://doi.org/10.1007/s00417-017-3775-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3775-x