Abstract
Purpose
To investigate, using the Dynamic Vessel Analyzer (DVA), the retinal vascular changes that may occur after vitrectomy for idiopathic epiretinal membrane (ERM).
Methods
Twenty-six eyes of 13 patients affected by unilateral idiopathic ERM were prospectively analyzed. 13 fellow eyes were used as control. The static (central retinal artery and vein equivalents) and dynamic (after flicker light stimulus) DVA analysis was performed at baseline (1 day before surgery) and 6 months after vitrectomy.
Results
The static DVA analysis did not highlight any significant change between investigational eyes and controls at baseline and 6 months after surgery. The DVA dynamic analysis showed similar arterial flicker response between cases and controls at baseline (p = 0.3396), but disclosed a significant reduction of the arterial flicker response after surgery in the study eyes compared to fellow eyes (p = 0.0024).
No significant changes were appreciated in the venous flicker response after surgery between cases and controls, both at baseline (p = 0.3450) and at the follow-up examination (p = 0.4214).
Conclusions
The physiological flicker-induced vasoconstriction is reduced after vitrectomy in arteries. The oxygen saturation change occurring after vitrectomy might have a role in the vascular tone modification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An intact vitreous gel is essential to a healthy human eye. Beyond its role in oculogenesis [1], the vitreous has the important biophysical property of metabolism and regulation of intraocular oxygen tension [2, 3]. A high concentration of vitreal ascorbate metabolizes the free oxygen passively released from the highly vascularized retinal tissue [4, 5] and, by way of this ascorbate-dependent oxygen consumption, a gradient is established from the posterior segment (higher concentration) to the lens (lower concentration) [3].
The active role of oxygen in endothelial activity and vasoconstriction is known from the vascular physiology, and has been also investigated in the retinal vasculature [6–8]. Since the normal oxygen gradient in the vitreous cavity is neutralized by the circulation of fluid after vitrectomy [3], it could be reasonable to question whether this oxygen level change may have some influence on the retinal microvasculature.
For this purpose, we used the Dynamic Vessel Analyzer (DVA, Imedos Systems, Jena, Germany), a commercially available tool for the functional study of retinal vasculature. The DVA assesses the retinal vessel diameter by analyzing the brightness profile of the vessel, using video sequences obtained with a conventional fundus camera. Besides this static analysis, the DVA includes also a functional vascular assessment, structured on a visual provocation system with flickering light. It has been fully documented that this kind of stimulus increases the retinal vessel caliber, the retinal blood flow and the optic nerve head blood flow in humans [9, 10]. Therefore, stimulation with flicker light has been used as a provocation test to investigate the regulation of vascular tone and the endothelium physiology.
The DVA technology has been extensively used in different ocular and non-ocular pathologies [11–14], and in several physiology studies [6–8], but it has never been employed to investigate the vascular changes occurring after vitreous removal. Hence, the purpose of this pilot study is to investigate the retinal vascular changes that may occur after vitrectomy, particularly for idiopathic epiretinal membranes (ERMs).
Methods
Study participants
In this prospective study, all the institutional patients affected by idiopathic ERM were screened from January 2015 to December 2015 at the Vitreoretinal Surgery Service of the Department of Ophthalmology, University Vita-Salute, San Raffaele Hospital.
Inclusion criteria were: age ≥18 years, axial length between 22.5–24.5 mm (measured with IOL Master, Zeiss), and a diagnosis of unilateral idiopathic ERM. The diagnosis was obtained with biomicroscopy and was confirmed with spectral-domain optical coherence tomography (SD-OCT).
Exclusion criteria were: ERM secondary to any ocular disease (e.g. diabetic retinopathy, uveitis, retinal vein occlusion, retinal dystrophies, etc.), glaucoma, history of head or ocular trauma, previous anterior segment (e.g. cataract surgery) or posterior segment surgery, including retinal laser photocoagulation. Patients with any optical media opacity (cornea or lens) that could interfere with a good quality imaging acquisition, with any concomitant systemic cardiovascular diseases (stroke, coronary artery disease, arterial hypertension, etc.) or with any known cardiovascular risk factor (diabetes, obesity, dyslipidemia) were not enrolled. Fellow eyes were considered as controls, hence subjects with any vitreoretinal interface disorder or presenting any of the exclusion criteria in the fellow eye were excluded from the study.
Study design
Visits were conducted the day before surgery (baseline) and at the 6-month postoperative visit. The complete ophthalmologic evaluation included ocular and general medical history, best-corrected visual acuity (BCVA), metamorphopsia assessment (with Amsler grid test), applanation tonometry, slit-lamp examination, fundus biomicroscopy, SD-OCT examination, and static and dynamic analysis with DVA. BCVA was measured with the Early Treatment Diabetic Retinopathy Study charts, and converted into the logarithm of the minimal angle of resolution (LogMAR) for the sake of statistical analysis. SD-OCT images were performed using the Spectralis OCT device (Heidelberg Engineering, Heidelberg, Germany) with automated evaluation of central foveal thickness (CFT), and the analysis of the retinal vascular changes was performed by the DVA machine (Imedos, Jena, Germany).
We tested whether a difference between study eyes and controls was present after surgery in each of the following variables: vessel (respectively arterial and venous) caliber, central equivalent (respectively arterial and venous), and flicker response vasodilation (respectively arterial and venous). Considering the pilot nature of the research, and the absence of any previous available reference in literature, we studied a certain convenience sample of patients, based on 1-year subject availability. The alternative hypothesis H1 was that there was a difference in the three different studied variables (each for artery and vein). The study was designed with a power of 0.85, with an effect size of 0.8.
Surgical procedure
Twenty-five gauge transconjunctival three-port pars plana sutureless vitrectomies with ERM and internal limiting membrane (ILM) peeling was successfully performed in all cases by a single experienced vitreoretinal surgeon (MC). Internal limiting membrane peeling was obtained with the pinch technique, grasping the ILM nearby the macula with macular forceps and providing a round maculorrhexis. Internal limiting membrane peeling was removed in all patients with Brilliant Blue® staining (Fluoron GmbH – Germany). Concurrent phacoemulsification with in-the-bag IOL implantation was performed in selected cases.
DVA analysis
The DVA acquisition module includes a mydriatic conventional fundus camera (FF450plus; Carl Zeiss GmbH, Jena, Germany), a digital high-resolution charged-coupled device (CCD) color camera, and a CCD video camera. The acquisition system is connected to the analysis software.
Essentially, the DVA assesses the retinal vessel diameter by analyzing the brightness profile of the vessel. The light source of the fundus camera is reflected by both the retina and the retinal vessels, and is then delivered through the observation pathway to a CCD-measuring video camera. The acquired information is then analyzed and simultaneously recorded by a video recorder, in order to allow the session to be re-evaluated a second time.
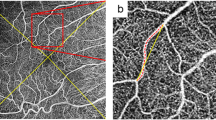
The DVA examination includes both static and dynamic analysis. The static analysis enables an automatic definition of the central retinal artery and vein equivalents (CRAE and CRVE), and the calculation of the artero-venous ratio (AVR). All arterioles and venules coursing through an area of 1/2 to 1 optic disc diameter away from the optic disc margin were manually identified and automatically measured (Fig. 1). Data were then summarized, where CRAE and CRVE represent the average caliber of arterioles and venules of the eye.
Static analysis performed with the Dynamic Vessel Analyzer. Optic disc-centered red-free fundus photography, taken with the Dynamic Vessel Analyzer. All arterioles (red segments) and venules (blue segments) coursing through an area of 1/2 to 1 optic disc diameter away from the optic disc margin are manually identified and automatically measured by the embedded software. Summarized data indicate the central retinal artery and the central retinal vein equivalents
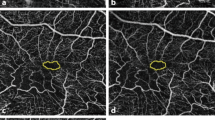
The DVA includes also a dynamic vascular assessment, structured on a visual provocation system. There is compelling evidence that visual stimulation with flickering light increases retinal vessel diameter, retinal blood flow and optic nerve head blood flow in humans [9, 10]. Therefore, stimulation with flicker light has been extensively used as physiological provocation stimulus to investigate the regulation of vascular tone [15]. The DVA flicker system is based on an optoelectronic shutter device inserted into the fundus camera, which interrupts the illumination light over the entire 30° visual field of the retinal camera. This produces a rectangular wave flicker with a bright-to-dark contrast ratio of 25:1. The flicker frequency is 12.5 Hz, which is in the range of the maximal excitation flicker frequency for retinal vessels in humans [9]. After flicker stimulus cessation, arteriolar diameters decrease below baseline, reaching a minimum diameter approximately 10–40 seconds after the cessation [16]. The exact time-course and the reason of this decrease are unclear. A steady illumination of 80 seconds was left between the 3 different cycles of flicker stimulation. The dynamic analysis outputs are the average of the vessel (artery and vein) caliber throughout the examination, and the relative dilation value (expressed in percentage; Fig. 2). Regarding the arterial analysis, since vessel dilation is physiologically followed by a relative constriction, we considered for calculations the entire caliber range between the maximum dilation and maximum constriction. Considering the vein inability to constrict, only the dilation range was used in the analysis.
Dynamic analysis graphs of artery and vein, before and after surgery. The graphs report the vascular response to flicker light stimulus of the sample subject. The pre-surgical and post-surgical graphs are shown for the arterial vessels (A and B respectively), and for the corresponding venous vessels (C and D). The complete cycle of 120 seconds (steady state-flicker stimulus-steady state) is plotted on X-axis, while the percentage relative vessel diameter is plotted on Y-axis. The dashed lines represent the threshold values for healthy individuals, automatically given by the embedded database. The time interval between the first and the second arrowhead indicates the flicker light duration, where vessel dilation is remarkable. The interval between the second and the third arrowhead is the time interval for the vessel to return into basal condition, where a mild relative constriction is evident. A loss of the relative dilation capacity is evident in the post-surgical arterial vessel (B), while no apparent difference appears in the venous vessel (D)
The DVA was performed in both eyes, examining in all subjects the supero-temporal vascular bundle (artery and vein; Fig. 3). In case of a normal unremarkable status of the fellow eye, the obtained data were used as a control. Pupil dilation was obtained using only 1% tropicamide solution eye-drops, in order to avoid any possible interference with the retinal vascular muscle tone and contraction. Patients were invited to rest while seated for at least 30 minutes before examination, to obtain a stable basal muscular vascular tone. Any vasoactive drugs, such as caffeine and nicotine, were avoided during the whole day of data registration. Two trained examiners (LI and GF) performed the DVA analysis.
Statistical analysis
Statistical analyses were performed using GraphPad Prism version 5.00 for Mac (GraphPad Software, San Diego, CA, USA). The Wilcoxon signed rank test was used to compare the outcome measures. The Spearman rank correlation test was used to assess the correlation between variables. We adjusted p values for multiplicity both with Bonferroni and with Holm procedures. The latter works under the same assumptions of Bonferroni adjustment. In all analyses, p values <0.05 were considered significant.
Results
We analyzed a total of 26 eyes of 13 patients (8 females, 5 males, average age at baseline 68.4 ± 7.7 years) fulfilling the inclusion/exclusion criteria. Thirteen eyes affected by idiopathic ERM were considered study eyes, and the 13 fellow eyes were used as controls.
All patients had disturbing metamorphopsia, which was reflected in distorted and non-uniform lines in the Amsler grid test. Average symptoms duration was 8.4 ± 2.1 months before surgery. All patients reported a post-surgical subjective reduction of metamorphopsia.
Surgery was successfully carried out in all the 13 enrolled eyes. No patient required a vitreous substitute at the end of surgery. No other procedures, such as laser endophotocoagulation, were performed in any of the studied cases.
BCVA increased from the baseline value of 0.58 ± 0.13 LogMAR to 0.28 ± 0.08 LogMAR at 6-month follow-up examination (p < 0.0001). The mean CFT changed from 439 ± 49 μm at baseline to 319 ± 31 μm at the 6-month postoperative visit (p = 0.002).
The DVA static analysis (CRAE, CRVE, AVR) did not highlight any significant change between study eyes and control eyes (Table 1). The baseline average AVR turned out to be similar between cases and controls, both at baseline (p = 0.9590) and at the follow-up examination (p = 0.7380). The same results were achieved also for CRAE, both at baseline (p = 0.3560) and at the follow-up examination (p = 0.5214), and for CRVE (p = 0.0905, and p = 0.1119, at baseline and at the follow-up examination, respectively).
The DVA dynamic analysis disclosed a significant reduction of the arterial flicker response after surgery in the study eyes compared to fellow eyes (p = 0.0024). The arterial flicker response was similar between cases and controls at baseline (p = 0.33; Table 2, Fig. 4).
No significant changes were appreciated in the venous flicker response after surgery between cases and controls, both at baseline (p = 0.3450) and at the follow-up examination (p = 0.4214; Table 2, Fig. 4).
Despite this significant change in the relative response to flicker light, the average arterial caliber remained unchanged after surgery, and turned out to be similar between cases and controls, both at baseline (p = 0.1837) and at the follow-up examination (p = 0.0960; Table 3, Fig. 5). The same results were achieved also for veins, both at baseline (p = 0.1422) and at the follow-up examination (p = 0.8339; Table 3, Fig. 5).
Bonferroni and Holm adjustments disclosed identical results, and are showed in the Tables 1, 2 and 3. Both procedures highlighted that the p value of arterial flicker response after surgery in study eyes compared to fellow eyes remained the only significant result (p = 0.0336).
For a further in-depth investigation, we analyzed the caliber difference of each study eye versus its respective control. For this purpose, we averaged each algebraic difference between the vessel caliber of the study eye and its fellow eye (in this order), and hence compared the results with the 6-month post-surgical visit. This analysis disclosed a significant increase in the difference between study eyes compared to fellow eyes, from the baseline value of −3 ± 17 μm to −12 ± 16 μm (p = 0.0140). The same procedure for the vein vessels did not achieve a statistically significant difference, from +5 ± 25 μm to −4 ± 25 μm (p = 0.3594).
The post-surgical arterial calibers did not correlate with average CFT (p = 0.7631), venous caliber (p = 0.9127), and BCVA (p = 0.9287).
Discussion
The retinal microvasculature provides a unique window to study the state of the local and systemic microcirculatory apparatus.
In the present study, we investigated the retinal vascular changes occurring after vitreous removal, using the technology of DVA. We analyzed only eyes with idiopathic ERM, as it is unanimously considered to be primarily a non-vascular disorder. The choice was done to minimize the influence of any other basal vascular condition that could have biased the results.
The DVA is a commercially available tool for the assessment of retinal vessel diameter in relation to time. The included software enables the operator to investigate two different aspects of microcirculation: a static analysis, which studies the basal vessel status (CRAE, CRVE and AVR), and a dynamic analysis, that explores the relative vessel variations by way of an additional visual provocation system (flickering light). Visual stimulation with flickering light increases retinal vessel diameter, and retinal and optic nerve head blood flow in humans [9]. More specifically, the retinal blood flow (and its response to flicker light stimulation) is selectively coupled with the local activity of the inner retina [10, 17, 18].
In healthy humans, the inhibition of nitric oxide (NO) causes an attenuation of the flicker light-induced vasodilation [19]. As a consequence, the regulation of retinal vascular tone (and flicker light-induced vasodilation) is dependent on NO release. The mediating effects of NO were further supported by the finding of flicker response attenuation in selected patients with known endothelial dysfunction, such as diabetes [20]. Furthermore, this decreased response was found to be deteriorated with increasing stages of retinopathy [21]. In another experimental human model, pO2 increasing by means of inhalation of 100% oxygen was found to induce a remarkable vasoconstriction in retinal vessels, particularly in all retinal quadrants [6–8].
Therefore, stimulation with flicker light has been used as physiological provocation to investigate the regulation of vascular tone and activity, both in healthy and pathologic subjects. The in-vivo registration of a dynamic vascular change after modification of vascular mediators (including NO and O2) revealed some of the mechanism underlying the vasoconstrictive response.
By means of dynamic analysis, in our study, we registered a significant reduction of the arterial vasoactivity 6 months after vitreous removal, compared to the fellow eyes. Despite the average arterial vessel caliber not being modified after surgery, we noted that an intra-subject case-to-control comparison disclosed a significant mild reduction of the vascular arterial caliber. No differences were noted in the venous vessels, which remained stable throughout the investigation.
Two theories about the vascular changes occurring after vitrectomy for idiopathic ERMs may be formulated. The first hypothesis suggests that the ERM itself might engender some morphological abnormalities on the inner retina, therefore altering the macular microcirculation and vasoactivity. Indeed, Kadonosono et al. found significant changes of capillary blood flow velocity in the perifoveal areas between normal subjects and eyes with ERMs [22, 23]. Furthermore, they found this pattern to be reversible, since the blood flow has been showed to increase after surgical removal of the ERM [22–25]. We acknowledge this hypothesis may be solid, but we disclose that the vascular markers (along the vascular arcades) that we used for static and dynamic analysis were far away from the macular area. Despite it being impossible to demonstrate that the measured vessels were not involved by the ERM, it is reasonable to think that they were loosely tightened by the epiretinal fibrosis.
The second hypothesis proposes that that vitreous removal, such as that after macular surgery, modifies oxygenation in the vitreous cavity. Vitrectomy significantly increases intraocular oxygen tension during and for prolonged periods after surgery [3]. According to previous data about hyperoxygenation [7], it could be reasonably hypothesized that this oxygen saturation change might have a role in the retinal oxygenation and in the vascular tone modification.
Despite a direct molecular connection between these two aspects not being demonstrated in our study, we speculate that this state of reduced vasoactivity may be attributable to the hyperoxic state of the vitreous cavity after vitrectomy. The whole vascular system might undergo a local chemioregulation that could lead to this new basal state.
Our static analysis did not find any significant change after surgery, highlighting the fact that the average CRAE, CRVE and AVR were similar. These apparently contrasting conclusions agree with our dynamic analysis results, since the vascular changes occurring after vitreous removal appear to be a dynamic change (reduced vasoactivity), more than a mere vascular caliber modification.
Our study has several limitations, mainly due to the small sample size and the short follow-up. We also acknowledge that, owing to the study design, the inclusion of patients from those who underwent serial observations might have influenced the results, since we enrolled only eyes with idiopathic ERMs and not with other diseases. Moreover, while the reproducibility of DVA in healthy subjects has been demonstrated [26], there are no conclusive data in literature regarding the reproducibility in pathologic subjects. On the other hand, strengths of our study are the accurate eye selection (idiopathic ERM only in subjects without vascular comorbidity), and control with fellow eyes. The use of fellow eye as controls enabled us to reduce the possibility that any potential external factor (that is concurrently affecting both eyes) could have biased the results: indeed, observations had a higher chance to be due to the tested variable.
Despite these limitations, to our best knowledge, this is the first study to selectively investigate the retinal vascular changes after vitreoretinal surgery for idiopathic ERM using DVA. Even though our conclusions are speculative, we believe our work supports the debate about the crucial role of the vitreous body in different retinal diseases. Furthermore, it emphasizes the possible positive role of vitrectomy for treating some ischemic retinal diseases, such as diabetic retinopathy. Other unknown factors should be certainly considered to understand the correct pathophysiology, and should be considered for a comprehensive analysis of this clinical aspect.
References
Sebag J (1998) Vitreous: from biochemistry to clinical relevance. In: Tasman W, Jaeger EA (eds) Duane’s foundations of clinical ophthalmology. Lippincott Williams & Wilkins, Philadelphia, pp 1–21
Holekamp NM (2010) The vitreous gel: more than meets the eye. Am J Ophthalmol 149(1):32–6
Beebe DC, Shui Y-B, Siegfried CJ, Holekamp NM, Bai F (2014) Preserve the (intraocular) environment: the importance of maintaining normal oxygen gradients in the eye. Jpn J Ophthalmol 58(3):225–31
Duarte TL, Lunec J (2005) Review: When is an antioxidant not an antioxidant? A review of novel actions and reactions of vitamin C. Free Radic Res 39(7):671–86
Shui Y-B, Holekamp NM, Kramer BC, Crowley JR, Wilkins MA, Chu F, Malone PE, Mangers SJ, Hou JH, Siegfried CJ, Beebe DC (2009) The gel state of the vitreous and ascorbate-dependent oxygen consumption: relationship to the etiology of nuclear cataracts. Arch Ophthalmol 127(4):475–82
Palkovits S, Told R, Schmidl D, Boltz A, Napora KJ, Lasta M, Kaya S, Werkmeister RM, Popa-Cherecheanu A, Garhöfer G, Schmetterer L (2014) Regulation of retinal oxygen metabolism in humans during graded hypoxia. Am J Physiol Heart Circ Physiol 307(10):H1412–H1418
Palkovits S, Lasta M, Told R, Schmidl D, Boltz A, Napora KJ, Werkmeister RM, Popa-Cherecheanu A, Garhöfer G, Schmetterer L (2014) Retinal oxygen metabolism during normoxia and hyperoxia in healthy subjects. Invest Ophthalmol Vis Sci 55(8):4707–13
Palkovits S, Told R, Boltz A, Schmidl D, Popa Cherecheanu A, Schmetterer L, Garhöfer G (2014) Effect of increased oxygen tension on flicker-induced vasodilatation in the human retina. J Cereb Blood Flow Metab 34(12):1914–8
Riva CE, Logean E, Falsini B (2005) Visually evoked hemodynamical response and assessment of neurovascular coupling in the optic nerve and retina. Prog Retin Eye Res 24(2):183–215
Falsini B, Riva CE, Logean E (2002) Flicker-evoked changes in human optic nerve blood flow: relationship with retinal neural activity. Invest Ophthalmol Vis Sci 43(7):2309–16
Lim M, Sasongko MB, Ikram MK, Lamoureux E, Wang JJ, Wong TY, Cheung CY (2013) Systemic associations of dynamic retinal vessel analysis: a review of current literature. Microcirculation 20(3):257–68
Corvi F, La Spina C, Benatti L, Querques L, Lattanzio R, Bandello F, Querques G (2015) Impact of Intravitreal Ranibizumab on Vessel Functionality in Patients With Retinal Vein Occlusion. Am J Ophthalmol 160(1):45–52.e1
Corvi F, Querques G, La Spina C, Lattanzio R, Bandello F (2015) Dynamic and Static Retinal Vessel Analyses in Patients with Macular Edema Secondary to Retinal Vein Occlusion. Retina 35(10):2052–9
La Spina C, Corvi F, Bandello F, Querques G (2016) Static characteristics and dynamic functionality of retinal vessels in longer eyes with or without pathologic myopia. Graefes Arch Clin Exp Ophthalmol 254(5):827–34
Garhöfer G, Bek T, Boehm AG, Gherghel D, Grunwald J, Jeppesen P, Kergoat H, Kotliar K, Lanzl I, Lovasik JV, Nagel E, Vilser W, Orgul S, Schmetterer L, Ocular Blood Flow Research Association (2010) Use of the retinal vessel analyzer in ocular blood flow research. Acta Ophthalmol 88(7):717–22
Polak K, Schmetterer L, Riva CE (2002) Influence of flicker frequency on flicker-induced changes of retinal vessel diameter. Invest Ophthalmol Vis Sci 43(8):2721–6
Metea MR, Newman EA (2007) Signalling within the neurovascular unit in the mammalian retina. Exp Physiol 92(4):635–40
Ames A, Li YY, Heher EC, Kimble CR (1992) Energy metabolism of rabbit retina as related to function: high cost of Na + transport. J Neurosci 12(3):840–53
Dorner GT, Garhofer G, Kiss B, Polska E, Polak K, Riva CE, Schmetterer L (2003) Nitric oxide regulates retinal vascular tone in humans. Am J Physiol Heart Circ Physiol 285(2):H631–6
Mandecka A, Dawczynski J, Blum M, Müller N, Kloos C, Wolf G, Vilser W, Hoyer H, Müller UA (2007) Influence of flickering light on the retinal vessels in diabetic patients. Diabetes Care 30(12):3048–52
Lim LS, Ling LH, Ong PG, Foulds W, Tai ES, Wong E, Lee SY, Wong D, Cheung CM, Wong TY (2014) Dynamic responses in retinal vessel caliber with flicker light stimulation in eyes with diabetic retinopathy. Invest Ophthalmol Vis Sci 55(8):5207–13
Kadonosono K, Itoh N, Nomura E, Ohno S (1999) Perifoveal microcirculation in eyes with epiretinal membranes. Br J Ophthalmol 83(12):1329–31
Kadonosono K, Itoh N, Nomura E, Ohno S (1999) Capillary blood flow velocity in patients with idiopathic epiretinal membranes. Retina 19(6):536–9
Yagi T, Sakata K, Funatsu H, Hori S (2012) Evaluation of perifoveal capillary blood flow velocity before and after vitreous surgery for epiretinal membrane. Graefes Arch Clin Exp Ophthalmol 250(3):459–60
Yagi T, Sakata K, Funatsu H, Noma H, Yamamoto K, Hori S (2012) Macular microcirculation in patients with epiretinal membrane before and after surgery. Graefes Arch Clin Exp Ophthalmol 250(6):931–4
Polak K, Dorner G, Kiss B, Polska E, Findl O, Rainer G, Eichler HG, Schmetterer L (2000) Evaluation of the Zeiss retinal vessel analyser. Br J Ophthalmol 84(11):1285–90
Acknowledgements
The Authors wish to thank Prof Alessandro Ambrosi, PhD of the Vita-Salute University in Milano for his support in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Iuliano, L., Fogliato, G., Querques, G. et al. Retinal vascular changes after vitrectomy for idiopathic epiretinal membrane: a pilot study with dynamic vessel analysis. Graefes Arch Clin Exp Ophthalmol 255, 1325–1332 (2017). https://doi.org/10.1007/s00417-017-3643-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3643-8