Abstract
Background
Pars plana vitrectomy (PPV) procedures are used for the surgical treatment of macular hole retinal detachment (MHRD) associated with high myopia. Re-detachment of the retina has been reported in MHRD associated with high myopia. Our aim was to evaluate the 1-year outcomes of vitrectomy, performed using an inverted internal limiting membrane (ILM) flap technique with gas tamponade, in five cases of MHRD associated with high myopia.
Methods
We performed a retrospective review of medical records of five consecutive cases of highly myopic MHRD. The following postoperative data were collected: refractive error, best-corrected visual acuity, intraocular pressure, ophthalmic fundus examination findings, ocular coherence tomography at 1, 3, 6, and 12 months postoperatively; duration of the follow-up period; and intra- and postoperative complications. The primary endpoint of the study was the rate of postoperative retinal reattachment and macular hole (MH) closure. Paired t-tests were conducted to evaluate postoperative changes.
Results
Mean visual acuity improved significantly (P = 0.008), with an improvement of ≥2 lines on LogMAR value gained in three of the five eyes. Retinal reattachment was maintained in all cases, with no cases of MH reopening identified over the mean follow-up period of 20.2 months. No complications were identified in any eye.
Conclusions
The inverted ILM flap technique and gas tamponade provided primary retinal reattachment and MH closure over the ≥12-month follow-up period.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since it was first described by Gonvers and Machemer, pars plana vitrectomy (PPV) procedures have been used in the surgical treatment of macular hole retinal detachment (MHRD) associated with high myopia [1]. However, some eyes require multiple surgeries to treat retinal redetachment after the initial surgery [1–12], despite variations in the PPV used, including posterior hyaloid peeling [3], internal limiting membrane (ILM) peeling [4–6, 8], macular buckling [7, 10], and endotamponade with gas [6] or silicone oil [11, 12]. The reason these surgical repairs are not always successful is related to the pathogenesis of the disease. MHRD associated with high myopia is thought to result from tangential and anteroposterior traction of the macula, combined with axial length (AL) elongation and atrophy of the retinal pigment epithelium (RPE). AL elongation in highly myopic eyes leads to an anatomical mismatch between the inner layer (sensory retina) and the outer layer (RPE-choroid-sclera) of the posterior eye globe [9, 13]. Because of this anatomical mismatch, tangential and anteroposterior traction of the posterior hyaloid membrane or internal limiting membrane causes a macular hole (MH). In cases of highly myopic eyes with a posterior staphyloma, the retina located at the posterior globe is detached by aqueous fluid passing through the opening of the MH [13]. Moreover, in these cases, the reattachment capacity of the posterior retina is insufficient due to atrophy of the RPE in the posterior staphyloma. In some cases with MHRD, a flat-open MH is identified on postoperative optical coherence tomography (OCT), indicative of a persistent MH despite retinal reattachment [5–11, 14]. Although initial repairs can successfully provide retinal attachment, the retina can subsequently detach again from the edge of the MH in the presence of flat-open MHs with a bare RPE resulting from RPE atrophy [5, 8, 15]. Closing the MH and relieving macular traction, therefore, seems to be essential to achieve retinal reattachment.
Recently, Michalewska et al. described the inverted internal limiting membrane (ILM) flap technique for the management of difficult-to-treat large MHs, including correction of the anatomical mismatch between the inner and outer layers of the posterior eye globe in MHRD [16–19]. The aim of our study was to evaluate the 1-year outcomes of vitrectomy, performed using an ILM flap technique with gas tamponade, in five cases of MHRD associated with high myopia.
Methods
Study design
We retrospectively reviewed the medical records of five consecutive eyes, contributed by five patients diagnosed with highly myopic MHRD, with an AL ≥26 mm, treated between August 2012 and August 2014 at Toho University Sakura Medical Centre, Chiba, Japan. All vitrectomy procedures were performed by one of the authors (T.M.) using the inverted ILM flap technique and gas tamponade.
This study was approved by the Toho University Sakura Medical Centre institutional review board. Patients’ personal information was protected at all times during the study process. Prior to surgery, the risks and benefits of the procedure were reviewed with each patient, and written informed consent was obtained from all patients in accordance with the guidelines for Toho University Sakura Medical Centre.
The following preoperative information was obtained for analysis: sex; age; refractive error; best-corrected visual acuity (BCVA), using the Snellen chart; intraocular pressure (IOP); AL; findings of slit-lamp examination; and cross-sectional fundus imaging, obtained using two commercially available spectral-domain OCT systems (Optovue; Fremont, CA, USA; and Spectralis HRA + OCT; Heidelberg Engineering, Heidelberg, Germany). The following postoperative data were collected: refractive error; BCVA; IOP; ophthalmoscopic fundus examination findings; OCT imaging at 1, 3, 6, and 12 months postoperatively; duration of the follow-up period; and intra- and postoperative complications. To confirm retinal reattachment in the early postoperative phase, OCT images, through endotamponade gas, were obtained within a few days after surgery. The main endpoint of this study was the rate of postoperative retinal reattachment and MH closure. Retinal reattachment was defined as observation of complete absorption of subretinal fluid (SRF) on OCT imaging. MH closure was defined as integrity of the retinal layer in the macular area, without evidence of a bare RPE on OCT imaging.
Surgical procedure
All patients underwent retrobulbar anesthesia, using a mixture of 2% lidocaine and 0.25% bupivacaine. In three of five eyes, a pars plana lensectomy was performed for cataract extraction. In the other two eyes, phacoemulsification and intraocular lens implantation were performed. All eyes underwent core vitrectomy after opening using a standard 25-gauge 3-port system (Constellation; Alcon, Fort Worth, TX, USA). Vitrectomy was extended to the periphery under scleral depression. After completion of the peripheral vitrectomy, gentle drainage of the viscous submacular fluid was performed through the MH, using a soft-tip cannula. The presence of posterior vitreous detachment was observed after intravitreal triamcinolone injection in all eyes (40 mg/mL; Kenacoat-A, Bristol-Myers Squibb, Princeton, NJ, USA) [20]. Remnants of the posterior hyaloid surrounding the MH were completely removed with a soft-tip cannula from all surfaces of the detached retina. Staining with 0.025% brilliant blue G (BBG) was used to facilitate ILM peeling in the range of three papillary diameters. The ILM surrounding the MH was peeled using end-gripping forceps, while the ILM was anchored at the edge of the MH. The peeled ILM was trimmed with a vitreous cutter, leaving enough of the central part of the ILM to cover the MH. The surgeon was careful to leave the ILM flap attached at the edge of the MH in the subsequent surgical process.
Intraoperative cross-sectional fundus images were obtained using a microscope-integrated to the intraoperative OCT device (Rescan 700; Carl Zeiss Meditec, Oberkochen, Germany) after its installation at our institution (in one of five eyes) [21, 22]. Fluid in the vitreous cavity was exchanged with air at an IOP of 25 mmHg, without draining the SRF through the MH. Three vitrectomy ports were sutured with the remaining fluid under the submacular space. The air in the vitreous cavity was then exchanged with 12% C3F8 gas in four eyes and with 20% SF6 gas in one eye. All patients were instructed to maintain a facedown position for 10 to 14 days.
Statistical analysis
Values were reported as the mean, standard deviation (SD) and range. Paired t-tests were conducted to evaluate postoperative changes in measured outcomes, with BCVA converted to the logarithm of the minimum angle of resolution (logMAR) for analysis. A P-value of 0.05 was considered significant. All analyses were performed using Statcel software (version 2.0; Excel-toukei, Saitama, Japan).
Results
The study included five patients: two men and three women. Relevant preoperative characteristics and postoperative results at 12 months post-surgery are summarized in Table 1. The mean preoperative BCVA was 0.80 ± 0.40 logMAR (range, 0.40 to 1.40 logMAR). The mean visual acuity improved significantly to 0.48 ± 0.48 logMAR (range, 0.00 to 1.05 logMAR) postoperatively (P = 0.008). An improvement in visual acuity of ≥2 lines (logMAR) was gained in three of the five eyes. In all eyes, although posterior vitreous detachment had been identified preoperatively, remnants of the posterior hyaloid were identified with intraoperative triamcinolone injection.
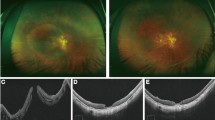
Intraoperative OCT images were obtained for Case 5 (Fig. 1). In this OCT image, the posterior retina appeared dome shaped, over the submacular fluid, with the ILM covering the MH (Video 1). OCT images acquired within a few days after surgery revealed MH closure and the disappearance of SRF. There was no incidence of MH reopening identified over the follow-up period. The mean follow-up duration was 20.2 months (range, 14 to 36 months). MH closure was confirmed by OCT at the final visit (Fig. 2) in all cases (100%). In addition, retinal reattachment was maintained over the follow-up period in all the cases (100%). No complications were identified.
Intraoperative optical coherence tomography images of Case 5 with macular hole retinal detachment. The OCT image in Fig. 1 (Top) was obtained at the time when the surgeon peeled the ILM, but left it attached at the edge of the MH. At this time, the peeled ILM extended toward the periphery. The images in Fig. 1 (Middle) were obtained at the time when the peeled ILM was trimmed with a vitreous cutter, but enough of the central part of the ILM was left to cover the MH. The trimmed ILM flap was spontaneously moved toward the center of the posterior pole. The OCT image in Fig. 1 (Bottom) was obtained after fluid-air exchange without draining the submacular fluid
Discussion
Since Gonvers et al. reported on the use of vitrectomy and gas tamponade for the surgical treatment of MHRD, the hole closure rate has remained unsatisfactory, although the rate of macular reattachment has improved over the years [1]. Ikuno et al. reported that a flat-open MH was detected on OCT in nine of 16 eyes after surgery for MHRD and that visual improvement was significantly associated with MH closure [14]. Therefore, the main purpose of surgical treatment for MHRD is to close the MH by filling the anatomical mismatch between the inner and outer layers of the posterior pole. We suggest that the inverted ILM flap technique should be considered to achieve this purpose [16].
Recently, successful outcomes of the inverted ILM flap technique for MHRD have been reported [17, 18]. However, these reports included cases that were followed for a comparatively short follow-up duration. By comparison, in this study, we report on the long-term outcomes (≥12 months) of a small number of cases of highly myopic MHRD treated with an ILM flap and gas tamponade procedure. In all eyes, retinal reattachment and MH closure were maintained over the 1-year follow-up period, with improvements in visual acuity of ≥2 lines (logMAR) achieved in three of the five eyes.
In one of the five eyes, intraoperative OCT findings revealed that coverage of the MH was successfully obtained using the inverted ILM flap according to the following procedural steps. First, the peeled ILM tends to lie towards the periphery before being trimmed. Second, after trimming, the peeled ILM assumes an erect position at the edge of the MH. Third, fluid-air exchange reduced the tension between the air and the remaining SRF over the opening of the MH and led to the inversion of the ILM flap, bridging the opening of the MH. In some cases of MHRD with a long disease duration, the SRF is commonly very viscous. In our study, the surgeon intentionally drained this pre-existing viscous SRF through the MH opening before ILM peeling. Okuda et al. reported residual SRF after surgery in three cases of MHRD [23], whereas our five cases showed rapid absorption of SRF after surgery. However, the non-viscous fluid remaining in the submacular space was intentionally retained to maintain the ILM flap at the edge of the MH opening. In one of the five eyes, intraoperative OCT imaging revealed a dome-shaped posterior retina from submacular fluid and an ILM flap that covered the MH opening. Furthermore, in all eyes, early postoperative OCT examination confirmed the disappearance of SRF within a few days after surgery, suggesting that SRF was not absorbed through the MH but via the RPE. Consequently, primary MH closure was observed in all eyes. We believe that our surgical procedures prompted reattachment in MHRD and MH closure.
Outcomes of the inverted ILM flap technique for patients with MHRD have recently been reported in different cases. Kuriyama et al. reported on four cases of MHRD treated using the PPV and inverted ILM flap technique [19]. Lai et al. reported that in 27 patients who underwent PPV with the inverted ILM flap technique, autologous blood application and C3F8 gas tamponade, 96% showed primary reattachment with a 96% MH closure rate [17]. Although the anatomical outcomes in their study were favorable overall, it is unknown which component of their surgical procedures contributed to the positive outcomes. The disadvantages of using autologous blood also need to be considered, which include endophthalmitis due to the additional extraocular manoeuver and the possibility of retinal toxicity from the autologous blood itself. Chen et al. performed a retrospective evaluation of outcomes for an inverted ILM flap technique compared to an ILM peeling technique [18]. Although a reattachment rate of 100% was identified for both techniques, a closure rate of the MH of 100% was reported for the ILM flap technique compared to 35% for the ILM peeling technique. Despite the short follow-up period of Chen et al.’s study (≤6 months), their findings do provide evidence of superior outcomes for the inverted ILM flap technique over the ILM peeling technique. These previous reports and our results support that the inverted ILM flap technique is more effective than standard vitrectomy with ILM peeling for the treatment of highly myopic MHRD.
With regards to visual outcomes, although the mean visual acuity improved significantly after surgery, some eyes showed only limited visual improvement. Even though the BBG that we used as a staining dye has been reported to have less retinal toxicity than ICG, a stained ILM flap in contact with the RPE at the MH opening may influence postoperative visual outcomes [8, 17, 18, 24]. Additionally, less visual improvement after surgery in case of highly myopic MHRD, with severe atrophy of the RPE or choroid, has previously been reported [9]. Greater damage to the photoreceptors of the detached retina in cases of MHRD with a long disease duration may lead to worse visual outcomes after surgery [25]. Though current treatments for MHRD focus on anatomical success, visual outcomes should be a further future goal.
The limitations of our study include its retrospective nature, small number of cases and lack of a control group. Further prospective studies should be conducted to evaluate differences between cases with and without visual improvement after vitrectomy with ILM flap.
In conclusion, we treated five eyes in five patients with highly myopic MHRD using vitrectomy with an inverted ILM flap technique and gas tamponade, obtaining primary retinal reattachment and MH closure in all cases. Retinal reattachment and MH closure were maintained in all eyes over the ≥12-month follow-up period. Moreover, the intraoperative process of the inverted ILM flap overlying the MH opening was revealed using a surgical microscope-integrated intraoperative OCT device.
References
Gonvers M, Machemer R (1982) A new approach to treating retinal detachment with macular hole. Am J Ophthalmol 94:468–472
Stirpe M, Michels RG (1990) Retinal detachment in highly myopic eyes due to macular holes and epiretinal traction. Retina 10:113–114
Oshima Y, Ikuno Y, Motokura M, Nakae K, Tano Y (1998) Complete epiretinal membrane separation in highly myopic eyes with retinal detachment resulting from a macular hole. Am J Ophthalmol 126:669–676. doi:10.1016/S0002-9394(98)00180-9
Kadonosono K, Yazama F, Itoh N, Uchio E, Nakamura S, Akura J, Sawada H, Ohno S (2001) Treatment of retinal detachment resulting from myopic macular hole with internal limiting membrane removal. Am J Ophthalmol 131:203–207. doi:10.1016/S0002-9394(00)00728-5
Ichibe M, Yoshizawa T, Murakami K, Ohta M, Oya Y, Yamamoto S, Funaki S, Funaki H, Ozawa Y, Baba E, Abe H (2003) Surgical management of retinal detachment associated with myopic macular hole: anatomic and functional status of the macula. Am J Ophthalmol 136:277–284. doi:10.1016/S0002-9394(03)00186-7
Uemoto R, Saito Y, Sato S, Imaizumi A, Tanaka M, Nakae K (2003) Better success of retinal reattachment with long-standing gas tamponade in highly myopic eyes. Graefes Arch Clin Exp Ophthalmol 241:792–796. doi:10.1007/s00417-003-0750-5
Ando F, Ohba N, Touura K, Hirose H (2007) Anatomical and visual outcomes after episcleral macular buckling compared with those after pars plana vitrectomy for retinal detachment caused by macular hole in highly myopic eyes. Retina 27:37–44. doi:10.1097/01.iae.0000256660.48993.9e
Oie Y, Emi K, Takaoka G, Ikeda T (2007) Effect of indocyanine green staining in peeling of internal limiting membrane for retinal detachment resulting from macular hole in myopic eyes. Ophthalmology 114:303–306. doi:10.1016/j.ophtha.2006.07.052
Nakanishi H, Kuriyama S, Saito I, Okada M, Kita M, Kurimoto Y, Kimura H, Takagi H, Yoshimura N (2008) Prognostic factor analysis in pars plana vitrectomy for retinal detachment attributable to macular hole in high myopia: a multicenter study. Am J Ophthalmol 146:198–204. doi:10.1016/j.ajo.2008.04.022
Alkabes M, Bures-Jelstrup A, Salinas C, Medeiros MD, Rios J, Corcostegui B, Mateo C (2014) Macular buckling for previously untreated and recurrent retinal detachment due to high myopic macular hole: a 12-month comparative study. Graefes Arch Clin Exp Ophthalmol 252:571–581. doi:10.1007/s00417-013-2497
Arias L, Caminal JM, Rubio MJ, Cobos E, Garcia-Bru P, Filloy A, Padron N, Mejia K (2015) Autofluorescence and axial length as prognostic factors for outcomes of macular hole retinal detachment surgery in high myopia. Retina 35:423–428. doi:10.1097/IAE.0000000000000335
Nishimura A, Kimura M, Saito Y, Sugiyama K (2011) Efficacy of primary silicone oil tamponade for the treatment of retinal detachment caused by macular hole in high myopia. Am J Ophthalmol 151:148–155. doi:10.1016/j.ajo.2010.07.023
Morita H, Ideta H, Ito K, Yonemoto J, Sasaki K, Tanaka S (1991) Causative factors of retinal detachment in macular holes. Retina 11:281–284
Ikuno Y, Sayanagi K, Oshima T, Gomi F, Kusaka S, Kamei M, Ohji M, Fuhikado T, Tano Y (2003) Optical coherence tomographic findings of macular holes and retinal detachment after vitrectomy in highly myopic eyes. Am J Ophthalmol 136:477–481. doi:10.1016/S0002-9394(03)00269-1
Seike C, Kusaka S, Sakagami K, Ohashi Y (1997) Reopening of macular holes in highly myopic eyes with retinal detachments. Retina 117:2–6. doi:10.1016/j.ophtha.2010.02.011
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J (2010) Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 117:2018–2025. doi:10.1016/j.ophtha.2010.02.011
Lai CC, Chen YP, Wang NK, Chuang LH, Liu L, Chen KJ, Hwang YS, Wu WC, Chen TL (2015) Vitrectomy with internal limiting membrane repositioning and autologous blood for macular hole retinal detachment in highly myopic eyes. Ophthalmology 122:1889–1898. doi:10.1016/j.ophtha.2015.05.040
Chen SN, Yang CM (2016) Inverted internal limiting membrane insertion for macular hole-associated retinal detachment in high myopia. Am J Ophthalmol 162:99–106.e1. doi:10.1016/j.ajo.2015.11.013
Kuriyama S, Hayashi H, Jingami Y, Kuramoto N, Akita J, Matsumoto M (2013) Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol 156:125–131.e1. doi:10.1016/j.ajo.2013.02.014
Yamamoto N, Ozaki N, Murakami K (2004) Triamcinolone acetonide facilitates removal of the epiretinal membrane and separation of the residual vitreous cortex in highly myopic eyes with retinal detachment due to a macular hole. Ophthalmologica 218:248–256. doi:10.1159/000078615
Ehlers JP, Kaiser PK, Srivastava SK (2014) Intraoperative optical coherence tomography using the RESCAN 700: preliminary results from the DISCOVER study. Br J Ophthalmol 98:1329–1332. doi:10.1136/bjophthalmol-2014-305294
Pfau M, Michels S, Binder S, Becker MD (2015) Clinical experience with the first commercially available intraoperative optical coherence tomography system. Ophthalmic Surg Lasers Imaging Retin 46:1001–1008. doi:10.3928/23258160-20151027-03
Okuda T, Higashide T, Kobayashi K, Ikuno Y, Sugiyama K (2016) Macular hole closure over residual subretinal fluid by an inverted internal limiting membrane flap technique in patients with macular hole retinal detachment in high myopia. Retin Cases Brief Rep 10:140–144. doi:10.1097/ICB.0000000000000205
Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T, Kubota T, Ishibashi T (2006) Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G-assisted membrane peeling. Retina 26:631–636. doi:10.1097/01.iae.0000236469.71443.aa
Shao Q, Xia H, Heussen FM, Ouyang Y, Sun X, Fan Y (2015) Postoperative anatomical and functional outcomes of different stages of high myopia macular hole. BMC Ophthalmol 15:93. doi:10.1186/s12886-015-0098-8
Acknowledgements
This research was not support by funding from the public, commercial, or not-for-profit sectors. The authors have no financial disclosures to report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
For this type of study formal consent is not required.
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
This intraoperative OCT video was recorded after fluid-air exchange without draining the SRF through the MH. In this video, the posterior retina appeared dome shaped, over the submacular fluid, with the ILM covering the MH. (MP4 6060 kb)
Rights and permissions
About this article
Cite this article
Kinoshita, T., Onoda, Y. & Maeno, T. Long-term surgical outcomes of the inverted internal limiting membrane flap technique in highly myopic macular hole retinal detachment. Graefes Arch Clin Exp Ophthalmol 255, 1101–1106 (2017). https://doi.org/10.1007/s00417-017-3614-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3614-0