Abstract
Purpose
To compare the anatomic and functional outcome of two variants of the inverted internal limiting membrane (I-ILM) flap technique for idiopathic macular holes (IMH) larger than 400 µm.
Methods
Twenty-seven consecutive patients undergoing PPV for IMH were randomly assigned to different variants of I-ILM technique: the Cover group included 14 patients in which the I-ILM was folded upside-down over the MH as a single layer while the Fill group enrolled 13 patients in which the I-ILM was folded within the MH in multiple layers.
Results
MH closed in 12/14 Cover and in 13/13 Fill eyes (84.6 vs. 100%, p = 0.14; n.s.). Vision at 1 month was Snellen 0.44 ± 0.17 vs. 0.28 ± 0.21 (p = 0.05) and 0.48 ± 0.20 vs. 0.37 ± 0.25 (n.s.) at 3 months. IS/OS line interruption width was 463 ± 385 vs. 602 ± 210 µm, respectively, at 1 month (n.s.) and 602 ± 210 vs. 563 ± 209 µm at 3 months (n.s.). The Cover group showed outer retina cystic changes more often (p < 0.01). MH over 700 µm closed in 0/2 and in 2/2 cases, respectively, in the Cover and Fill groups (0.045).
Conclusions
Cover and Fill I-ILM techniques allowed similar closure rates and post-operative vision at 3 months. The Cover group showed better anatomical restoration and vision at 1 month while the Fill technique might be more efficient in closing larger MHs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The visionary work of Kelly and Wendel [1] originated idiopathic macular hole (IMH) surgery in 1991. Ever since, surgery and instrumentation greatly refined to reach today’s 90% closure rate [2]. In 2010, Michalewska [3] introduced the inverted internal limiting membrane (ILM) flap technique, improving success rates of larger IMHs.
As the procedure gained acceptance, indications widened [4, 5] and alternatives were proposed [6]. The original technique is based on ILM peeling centripetally up to the MH rim and folding it upside-down on top of the MH (we named it the “Cover” technique) while one of the most widespread variation is based on folding multiple ILM layers within the MH defect [7] (a variant we named “Fill” technique).
The success rate of the original technique is reported but less is known about its variants and if there is any difference in terms of functional and anatomical results. The use of autologous tissue (the ILM) to “bridge” or “plug” the MH also poses unanswered questions regarding its purported role of simple scaffold, sealant, or glue.
In order to evaluate if and to what extent variations of the same technique differ in terms of vision and microstructural restoring capability, we conducted a study on patients randomly assigned to the Cover or Fill technique.
Materials and methods
Patient selection
Twenty-seven consecutive patients undergoing pars plana vitrectomy (PPV) for idiopathic MH were randomly assigned to Cover or Fill I-ILM technique. Every other prospectively eligible patient was assigned to Cover or Fill technique. There were only two senior surgeons involved (TR and AG).
Included patients had idiopathic MH greater than 400 µm of less than 6-month duration. Patients with myopia greater than 6 diopters, history of trauma, macular edema of any origin, recurrent or non-closing MH, previous ocular surgery other than uncomplicated phacoemulsification, diagnosis of glaucoma and/or other chronic ocular diseases were excluded.
All patients underwent complete eye examination with patent and manifest refraction, best-corrected visual acuity (BCVA) using EDTRS charts, anterior and dilated posterior segment, and SD-OCT (Spectralis Heidelberg Engineering, Germany) imaging pre-operatively, at 1 and 3 months after surgery. All OCT scans included horizontal and vertical MH diameter, IS/OS line interruption width and foveal thickness. Patients with incomplete charts or insufficient OCT quality were excluded. OCT readers were masked to surgical technique.
A senior retina specialist (CC) masked to group randomization and surgical technique (but not to pre- or post-surgery status analyzed all SD-OCT scans. Macular holes were considered closed if there was evidence of whatever tissue bridging the pre-operative MH, regardless to retinal layer integrity. IS/OS line interruption width was measured on a high-quality horizontal scan placing a horizontal caliper to bridge the IS/OS line interruption. If the IS/OS line presented multiple areas of disruption (like a dashed line), the interruption width was considered the line bridging the outermost sections of continuous IS/OS line.
The study followed the tenets of the Helsinki Declaration and received IRB approval.
Surgical technique
Surgical technique included a standard three-port 25G PPV, with posterior vitreous detachment induction, vitreous base vitrectomy, and ILM staining with 0.25 g/l brilliant blue-G (Brilliant Peel TM, Geuder, Germany). All phakic patients underwent combined phacoemulsification with in-the-bag IOL implant; no patients had capsular bag ruptures and/or dislocation.
Depending on group assignment, inverted ILM flap creation and apposition varied as follows:
-
1)
in the Cover group patients, the ILM was peeled centripetally all the way up to the MH rim and the hinged ILM flap folded upside-down on top of the MH in order to bridge the entire retinal defect with a single layer (see Fig. 1a).
Fig. 1 a Schematic drawing of the Cover technique. The ILM is peeled up to the MH rim and folded upside-down on top of it to bridge the entire MH gap. No attempt to fill the MH volume defect is made. b Schematic drawing of the Fill technique: the ILM is peeled up to the MH rim and folded inside it. Multiple layers of folded ILM can be seen within the MH section. Compare to Fig. 2
-
2)
in the Fill group the ILM was folded in multiple layers and deliberately “stuffed” or “packed” within the MH defect using a forceps (see Fig. 1b).
Gas tamponade was invariantly sulfur hexafluoride 20% (SF6; Micromed, Rome, Italy). All patients were instructed to position themselves face down for 3–4 h a day during the first 3 post-operative days.
Main outcome measures
Best-corrected visual acuity (BCVA), MH status (open, flat open, or closed) and IS/OS line interruption width at time 0 (pre-operative), 1 month and 3 months after surgery. Presence of hypo-reflective areas interpreted as cysts within the foveal region and of visible ILM layer(s) lining or filling the MH. Qualitative description of OCT images with particular regard to foveolar anatomical micro-structure completed results analysis.
Statistical analysis
Data were approached under the assumption of intention-to-treat analysis.
Analysis of variance with t test for repeated measures was used for continuous quantitative measures including BCVA (measured as Snellen fraction and then converted to logMAR for statistical purposes) and IS/OS line interruption width. Chi-square was used to test the significance of observed and expected MH closure, cystic changes, ILM remnants within the MH and foveal depression restoration. Pearson rho was used to evaluate the correlation between continuous variables such as MH and IS/OS line interruption width and logMAR visual acuity.
In all cases, p values less than 0.05 have been considered statistically significant.
Results
Cover groups included 14 patients and the Fill group included 13. Patients’ demographics and condition at baseline are listed in Table 1: the two groups did not differ significantly in terms of age, vision, MH width, and IS/OS line interruption.
Table 2 summarizes surgical outcome: overall success rate was 11/13 (84.6%) in the Cover group and 13/13 (100%) in the Fill group, the difference being not significant. Larger MHs (>700 µm) closure rate was higher in the Fill group (0/2 Cover groups vs. 2/2 in the Fill group; p = 0.0455). There were no cases of failed flap construction.
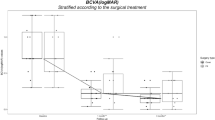
The Cover group showed a better BCVA at 1 month (0.44 vs. 0.28; p = 0.05) while IS/OS line interruption width at 1 month, BCVA, and IS/OS line interruption width at 3 months did not differ significantly between groups.
Both groups showed a significant BCVA improvement at 1 month compared to baseline (p > 0.001). Between 1 and 3 months after surgery, the Fill group (unlike the Cover group) showed a trend towards further improvement: 0.28 decimal improving to 0.37 Fill groups (not significant; n.s.) vs. 0.44 remaining stable at 0.44 (Table 2).
IS/OS line interruption width greatly reduced in both groups between baseline and 1 month after surgery (p < 0.01 for both). The Fill group showed a greater IS/OS line gap decrease between 1 and 3 months than the Cover group but neither was statistically significant (Table 2).
Cystic changes within the external retinal layers were significantly more prevalent in the Cover group (p < 0.01 both at 1 and 3 months) while the Fill group consistently showed remnants of the ILM within the MH, up to the 3-month follow-up visit (see Table 2; p = 0.02 and p < 0.001, respectively).
There was a significant correlation between IS/OS defect width and BCVA in both groups and at all points in time (baseline, 1 month, 3 months; p < 0.01 in all cases). Macular hole diameter at baseline was also significantly correlated to BCVA at 1 and 3 months (p < 0.005 in all cases).
Discussion
The introduction of inverted ILM flap technique in 2010 improved the closure rate and visual function for MHs greater than 400 µm, compared to ILM peeling alone [3].
Several modifications to the original technique (Fig. 1a) have been introduced, including the deliberate “filling” of the MH with folded ILM, a procedure also used in re-operations when a hinged flap cannot be obtained and free ILM patch is “stuffed” within the MH (Fig. 1b) [8–10].
We compared patients operated with Cover and Fill technique to evaluate if ILM apposition modality influenced anatomic closure pattern and functional outcome.
The two groups appeared well balanced at baseline in terms of age, MH diameter, vision, and IS/OS line interruption width (Table 1). The Fill group had a slightly higher proportion of MHs larger than 600 µm, although mean MH diameter was similar.
Both groups obtained a very high success rate, consistent with existing literature [3, 4]: MH closed in 13/13 the Fill group cases and 12/14 cases in the Cover group, the difference not being significant (Table 2). Likewise, both techniques resulted in significant vision improvement; the Cover group obtained a slightly higher vision at 1 month while there was no difference across groups at 3 months.
Foveal microstructural features differed between groups: the Cover technique resulted in a prompt reconstruction of the inner retinal layers (Fig. 2) and also in the presence of foveolar depression with residual outer retinal defects. The ILM lined the inner retinal profile sometimes reduplicating on top of closed MH but did not protrude within the previous MH. The Fill group eyes behaved differently: multiple and irregularly folded ILM layers perpendicular to the layered retinal structure were evident in all eyes and throughout the 3-month follow-up period (Fig. 3).
Cover technique. a Pre-operative OCT of patient #3 showing a fairly large MH with edematous rim and over 1,000 μ IS/OS line interruption width. b 1-month post-op OCT of the same patient shows MH closure with good restoration of foveal anatomy, very limited IS/OS line alteration is visible is this patient and the free ILM sheet is readily visible. c The same patient at 3-month post-op: the ILM folds remnants disappeared and the MH is closed. No residual IS/OS line interruption can be detected
Fill technique. a Pre-op OCT shows a large MH with edematous rim and deposits over the bare RPE within the MH. b 1-month post-op OCT shows multiple folded layers of ILM plugging the MH full-thickness, reaching the RPE layer. There are no cystic spaces and the ILM tissue with its layers perpendicular to retinal structure is readily visible. c Two months later, the ILM tissue is still visible full-thickness and discernible from retinal layers
Four types of MHs closure patterns have been previously categorized: U and V shaped, irregular, and flat open [11], the first one being the more functionally favorable. The introduction of inverted ILM flap introduces adjunctive closure patterns also described by Hayashi [12] that should be categorized (Figs. 2 and 3). Intriguingly, the presence of “intrusive” ILM tissue overtly interrupting inner retinal layers did not seem to jeopardize functional outcome in terms of Snellen visual acuity at least in the medium term, since vision in the Cover group was better at 1 month but similar at 3 months.
This data strengthens Wakabayashi et al.’s [13] observation that outer retinal layers integrity (i.e., IS/OS line gap width and external limiting membrane interruption) decides visual function more than inner retinal layer restoration [14]. No patients in either series showed serious adverse events and no case of retinal pigment epithelium atrophy seen, as previously reported [15]. It should be noted that our study only measured visual acuity and did not take into account metamorphopsias and foveolar differential sensitivity. Further testing in that regard is warranted to better characterize possible qualitative and quantitative difference among different surgical techniques.
Based on our anatomic and functional results, we believe the ILM acts differently according to surgical technique: in the Cover variant, the ILM bridges the MH, facilitating the inner retinal defect shrinkage and/or closure and allows better restoration of the retinal structure. The outer retina benefits less and takes longer to seal, leaving outer retinal cysts up to 3 months after surgery (Table 2; p = 0.0008). The closure of such outer retinal defects by means of the Cover technique would be a mere consequence of inner retinal apposition facilitated by ILM flap roofing the MH. Interestingly, Michalewska et al. [11] already reported the presence of post-operative outer retinal cysts in 2008 when ILM peeling alone was the gold standard.
In the Fill procedure (Figs. 1 and 3), the ILM acts as a filler, glue, and scaffold as the same time. The MH closes in the early post-operative period and no hypo-reflective areas are visible at 1 or 3 months, while the ILM folded within the MH remains visible throughout follow-up (Fig. 3). OCT scans of post-operative Fill group patients invariably show ILM tissue macroscopically altering the foveolar inner retinal layers while photoreceptor layer does not seem to be affected and the IS/OS line gap width is similar to the Cover group, probably justifying the same vision outcome at 3 months (Table 2).
Interestingly, the Fill group included 6/13 MHs larger than 600 µm and 2 MHs over 700 µm: they all closed (Fig. 4). The Cover group also had 2 MH greater than 700 µm that did not seal. Although barely significant, the higher success rate suggests an advantage of the Fill technique limited to this subgroup. It is conceivable that larger MHs close more promptly and efficiently when ILM becomes a filler more than a framework: the simple creation of a roof on top of the hole might not be enough to start endogenous sealing mechanism in MHs exceeding a critical span.
Pitfalls of the present study include the limited number of cases and relatively short follow-up. It nonetheless retains the strength of balanced groups at baseline and consistent surgical technique. Further studies on a larger scale are warranted to corroborate the suggested conclusion.
In summary, our study suggests that both inverted ILM flap variants can successfully close MHs greater than 400 µm with some difference in terms of micro-anatomical structure restoring. No significant adverse effects were registered in either series. The Fill technique could be more efficacious in closing larger MHs.
References
Kelly NE, Wendel RT (1991) Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol 109(5):654–9
Madi HA, Masri I, Steel DH (2016) Optimal management of idiopathic macular holes. Clin Ophthalmol 10:97–116
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J (2010) Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 117:2018–25
Kuriyama S, Hayashi H, Jingami Y, Kuramoto N, Akita J, Matsumoto M (2013) Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol 156:125–131
Michalewska Z, Nawrocki J (2013) Macular hole surgery in a patient who cannot maintain facedown positioning. Case Rep Ophthalmol 4:1–6
Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Adelman RA, Nawrocki J (2015) Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: a comparative study. Retina 35:1844–50
Lai CC, Chen YP, Wang NK, Chuang LH, Liu L, Chen KJ, Hwang YS, Wu WC, Chen TL (2015) Vitrectomy with internal limiting membrane repositioning and autologous blood for macular hole retinal detachment in highly myopic eyes. Ophthalmology 122:1889–98
Song Z, Li M, Liu J, Hu X, Hu Z, Chen D (2016) Viscoat-assisted inverted internal limiting membrane flap technique for large macular holes associated with high myopia. J Ophthalmol 6:8283062. doi:10.1155/2016/8283062
Chen Z, Zhao C, Ye JJ, Wang XQ, Sui RF (2016) Inverted internal limiting membrane flap technique for repair of large macular holes: a short-term follow-up of anatomical and functional outcomes. Chin Med J (Engl) 129:511–7
Gekka T, Watanabe A, Ohkuma Y, Arai K, Watanabe T, Tsuzuki A, Tsuneoka H (2015) Pedicle internal limiting membrane transposition flap technique for refractory macular hole. Ophthalmic Surg Lasers Imaging Retina 46:1045–6
Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J (2008) Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 246:823–30
Hayashi H, Kuriyama S (2014) Foveal microstructure in macular holes surgically closed by inverted internal limiting membrane flap technique. Retina 34:2444–50
Wakabayashi T, Fujiwara M, Sakaguchi H, Kusaka S, Oshima Y (2010) Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology 117:1815–24. doi:10.1016/j.ophtha.2010.01.017
Villate N, Lee JE, Venkatraman A, Smiddy WE (2005) Photoreceptor layer features in eyes with closed macular holes: optical coherence tomography findings and correlation with visual outcomes. Am J Ophthalmol 139:280–9
Imai H, Azumi A (2014) The expansion of RPE atrophy after the inverted ILM flap technique for a chronic large macular hole. Case Rep Ophthalmol 5:83–6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Financial disclosure
None of the other authors has any financial interest in the subject matter. The research for this paper was financially supported in part by the Ministry of Health and “Fondazione
Rights and permissions
About this article
Cite this article
Rossi, T., Gelso, A., Costagliola, C. et al. Macular hole closure patterns associated with different internal limiting membrane flap techniques. Graefes Arch Clin Exp Ophthalmol 255, 1073–1078 (2017). https://doi.org/10.1007/s00417-017-3598-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3598-9