Abstract
Purpose
The purpose was to quantify and compare the severity of aniseikonia in patients undergoing vitrectomy for various retinal disorders.
Methods
We studied 357 patients with retinal disorders including epiretinal membrane (ERM), macular hole (MH), cystoid macular edema with branch / central retinal vein occlusion (BRVO-CME / CRVO-CME), diabetic macular edema (DME), macula-off rhegmatogenous retinal detachment (M-off RD), and macula-on RD (M-on RD) as well as 31 normal controls. The amount of aniseikonia was measured using the New Aniseikonia Test preoperatively and at 6 months postoperatively.
Results
Of all patients, 59% presented aniseikonia. Preoperative and postoperative mean aniseikonia were 4.0 ± 4.1% and 3.0 ± 3.6%, respectively. In particular, 68% of patients with ERM had macropsia, and approximately half of MH, RVO-CME, DME, and M-off RD patients had micropsia. Preoperative aniseikonia was significantly severe in ERM than in other disorders. Vitrectomy improved aniseikonia only in MH, while visual acuity was improved in all disorders except CRVO-CME.
Conclusion
More than half of the patients showed aniseikonia preoperatively. A majority of ERM patients exhibited macropsia, whereas MH, RVO-CME, DME, and macula-off RD patients presented micropsia. The aniseikonia score was greatest in ERM patients. In most retinal disorders, surgery significantly improved visual acuity, but not aniseikonia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aniseikonia is a difference of perceived image size between two eyes, and symptoms of aniseikonia, such as headache, asthenopia, photophobia, reading difficulty, nausea, vertigo, and dizziness, are various, and a sense of discomfort differs among individuals [1, 2]. Therefore, aniseikonia plays an important role in visual function and quality of life. Anisometropia, induced by a difference of spherical equivalent between two eyes, is relatively common in aniseikonic patients, and was reported in various pathological conditions including oblique astigmatism, aphakia, pseudophakia, and corneal refractive surgery [3–8]. In contrast, retinally induced aniseikonia is less-noted. Retinally induced aniseikonia may occur following stretching or compression of the retina, which changed the perceived image size due to space alteration among the photoreceptors [9]. Prior studies have investigated retinally induced aniseikonia in epiretinal membrane (ERM) [9–15], retinal detachment (RD) [15–20], age-related macular degeneration [21], macular edema [18], and central serous chorioretinopathy [22]. No reports so far, however, have addressed aniseikonia in patients with macular hole (MH), cystoid macular edema with retinal vein occlusion, and diabetic macular edema (DME). In addition, a comparison of aniseikonia and any postoperative changes in aniseikonia among these retinal disorders has not been documented.
In the present study, aniseikonia data from normal subjects and patients with various retinal disorders were assessed using the New Aniseikonia Test (Handaya, Tokyo, Japan). This study was aimed at comparing aniseikonia among retinal disorders and to make an evaluation the of the relationship between aniseikonia and visual function in each disorder.
Methods
The study population consisted of a series of 357 eyes of 357 patients who were diagnosed and treated with retinal disorders between August 2011 and December 2013 at Tsukuba University Hospital. The subjects were 204 male and 153 female patients, averaging 62.3 ± 11.0 years of age (mean ± standard deviation). This study included 81 patients with ERM, 80 patients with MH, 28 patients with cystoid macular edema with branch retinal vein occlusion (BRVO-CME), 12 patients with cystoid macular edema with central retinal vein occlusion (CRVO-CME), 20 patients with DME, 67 patients with macula-off rhegmatogenous RD (M-off RD), and 69 patients with macula-on rhegmatogenous RD (M-on RD), who all underwent vitrectomy. Thirty-one subjects served as normal controls (NC). We conducted this prospective, interventional, consecutive study in accordance with the Declaration of Helsinki and received approval from the institutional review committees of the University of Tsukuba Hospital. Signed informed consent was obtained from all study subjects. Exclusion criteria comprised eyes with ophthalmic disorders except for mild refractive errors and mild cataract, and a previous history of vitrectomy. Patients who showed anisometropia greater than 2.0 diopters before and/or six months after surgery were also excluded. Patients who had undergone vitrectomy for bilateral eyes within 6 months apart were also excluded.
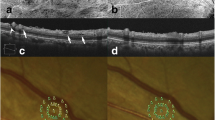
The examinations comprised measurements of the best-corrected visual acuity (BCVA), the severity of aniseikonia using the New Aniseikonia Test (NAT), fundus examinations with indirect ophthalmoscopy, and the retinal microstructure by spectral-domain optical coherence tomography (OCT) (Cirrus high-definition OCT; Carl Zeiss, Dublin, CA). All ophthalmological examinations were performed before and 6 months after surgery. The BCVA, measured by the Landolt Chart, was expressed as the logarithm of the minimum angle of resolution (logMAR).
The NAT, introduced in 1988 by Katsumi and his colleagues [3], is a simple method to quantify the amount of aniseikonia. The test consists of matched pairs of red/green semicircles with a target size of 4 cm, and allows for measurement from 1% to 24% of aniseikonia. Two semicircles with different sizes in each pair are placed in a consecutive manner with a difference in 1% increments. A subject who wears red/green spectacles views the plates so that the right eye can see either of the semicircles in every pair and the left eye can see the other one. The subject is asked to indicate the pair in which two semicircles seem to be the same size. The actual difference in the size of the halfmoons in the corresponding pair represents the percentage of the subject’s aniseikonia. Measurements were performed at a distance of around 40 cm in vertical as well as horizontal meridians, and the obtained mean values also were used to analyze data. Aniseikonia of 2% or greater was deemed macropsia, whereas that of +2% or less was considered micropsia. The examiners administering the NAT tests were experienced orthoptists and were masked to the fundus findings of the patients.
ERM was defined as a translucent membrane involving the fovea, with or without distortion of the inner retinal surface on biomicroscopy and OCT, and vitrectomy was indicated if patients complained of significant metamorphopsia and/or blurred vision. The indication for vitrectomy in MH included stage II - VI full-thickness macular hole on OCT. The indication for vitrectomy in BRVO and CRVO included persistent CME. DME was defined by clinically significant macular edema according to the ETDRS guidelines and diagnosed with slit-lamp biomicroscopy with foveal thickness of ≥ 300 μm as measured by OCT, and vitrectomy was indicated when ≥ 3 months had passed after at least one session of laser treatment. The indications for vitrectomy in RD included presence of causative horseshoe tears due to posterior vitreous detachment. In the patients with RD, preoperative aniseikonia evaluation was not performed, because of the rapid nature of its onset and significant disturbance of visual function.
Surgery consisting of 25-gauge transconjunctival sutureless vitrectomy under sub-Tenon local anesthesia was performed by three vitreoretinal surgeons (F.O., Y.O., Y.S.). When a clinically significant cataract was observed, we simultaneously conducted an operation for cataract. A core vitrectomy was performed with induction of posterior vitreous detachment if not already present. Peripheral retinal examination with scleral depression was performed to search for a retinal tear or dialysis in all cases. Fluid/gas exchange was performed if iatrogenic retinal tear or rhegmatogenous retinal detachment was identified intraoperatively. In patients with ERM, the membrane was removed from the macula with intraocular forceps. After the ERM was peeled, 0.1 - 0.2 ml of 0.025% brilliant blue G solution was applied to the macular area. Then, we completely peeled the remaining internal limiting membrane. In patients with MH, the inner limiting membrane was peeled off with the aid of brilliant blue G solution, followed by fluid/gas exchange. In patients with RD, surgical procedures comprised release of vitreous traction around the breaks, internal drainage of the subretinal fluid, total fluid/gas exchange using air or 20% SF6, and endolaser photocoagulation. For the subsequent 1-5 days, the patients kept a face-down position.
The mean scores and standard deviations were calculated for age, aniseikonia and BCVA in patients with retinal disorders and normal controls. The Paired t-test was performed to compare preoperative and postoperative results. The relationship between preoperative and postoperative parameters of visual function was examined with the Pearson’s correlation coefficient. Fisher’s protected least-significant difference (PLSD) was performed to compare age and aniseikonia among retinal disorders. All tests of association were considered statistically significant if p < 0.05. The analyses were carried out using StatView (version 5.0, SAS Inc., Cary, NC, USA).
Results
Table 1 summarizes the background data of normal controls and patients with retinal disorders. The patients in the RD group were significantly younger than those in the other groups (p < 0.05). Of the 357 patients, 64 were pseudophakic and 293 were phakic, 192 patients underwent cataract surgery combined with vitrectomy and 30 patients received scleral buckling surgery. Preoperative and 6-month postoperative absolute differences of spherical equivalent between both eyes were 0.57 ± 0.48 (range: 0.0 ∼ 1.9D) and 0.71 ± 0.51 (range: 0.0 ∼ 1.9D), respectively.
Preoperatively, 131 (59%) patients had aniseikonia (66 patients had micropsia, 65 had macropsia, and 90 had no aniseikonia) in all cases. The absolute value of aniseikonia was 4.0 ± 4.1%, and the degree of aniseikonia ranged from -21.5% to +19.5%. Figure 1 shows distribution of preoperative aniseikonia in each disorder. In ERM patients, 68% exhibited macropsia and only a few (2%) had micropsia. On the other hand, micropsia was observed in many of MH (48%), BRVO-CME (39%), CRVO-CME (50%), and DME (45%) patients and macropsia was rare. Postoperatively, 80 patients (22%) had micropsia, 179 (50%) had macropsia, and 98 (27%) had no aniseikonia in all cases. The absolute value of aniseikonia was 3.0 ± 3.6%, and the amount of aniseikonia ranged from -20.5% to +17%. The postoperative proportion of macropsia in ERM was 69%, which was comparable to the preoperative value. The proportion of micropsia in MH decreased from 48% to 18%, while that of BRVO-CME and CRVO-CME increased after surgery. In M-off RD patients, 48% showed micropsia, whereas 75% of M-on RD patients did not have any aniseikonia (Fig. 2).
Distribution of postoperative aniseikonia in retinal disorders. ERM = epiretinal membrane, MH = macular hole, BRVO-CME = cystoid macular edema with branch retinal vein occlusion, CRVO-CME = cystoid macular edema with central retinal vein occlusion, DME = diabetic macular edema, M-off RD = macula-off rhegmatogenous retinal detachment, M-on RD = macula-on rhegmatogenous retinal detachment
The box-and-whisker plots of the preoperative and postoperative aniseikonia in each group are displayed in Fig. 3. Significant differences in aniseikonia were found between NC and all retinal disorders except DME. Preoperative aniseikonia in ERM was significantly higher than that in other disorders. Preoperative aniseikonia in CRVO-CME was lower than that in DME (Fig. 3a). Postoperatively, significant differences in aniseikonia were found between NC and all retinal disorders except MH and M-on RD. Postoperative aniseikonia in ERM was significantly higher than that in other disorders. Significant differences were also seen among other disorders (Fig. 3b).
Box and whisker plots with the top and bottom boundary of the box indicating the 75th and 25th percentiles. Whiskers above and below the box indicate the 90th and tenth percentiles, respectively. a. Preoperative mean aniseikonia in retinal disorders. b. Postoperative mean aniseikonia in retinal disorders. NC = normal controls, ERM = epiretinal membrane, MH = macular hole, BRVO-CME = cystoid macular edema with branch retinal vein occlusion, CRVO-CME = cystoid macular edema with central retinal vein occlusion, DME = diabetic macular edema, M-off RD = macula-off rhegmatogenous retinal detachment, M-on RD = macula-on rhegmatogenous retinal detachment. * Significantly different in Fisher’s Protect Least Significant Difference (Fisher’s PLSD)
Vitrectomy significantly improved the absolute value of aniseikonia and BCVA in all cases. Subgroup analysis showed significant improvement of BCVA in all disorders except CRVO-CME. On the other hand, postoperative aniseikonia was significantly lower than the preoperative one only in MH, while no change was confirmed in other disorders (Table 2).
When scores of all the patients with retinal disorders were analyzed, the preoperative absolute value of mean aniseikonia correlated significantly with the postoperative absolute value of mean aniseikonia (r = 0.592, p < 0.0001, Fig. 4a) and changes in the absolute value of mean aniseikonia (r = 0.479, p < 0.0001, Fig. 4b). Subgroup analysis revealed preoperative aniseikonia correlated significantly with postoperative aniseikonia in every group except DME. In addition, preoperative aniseikonia correlated significantly with changes in aniseikonia in ERM, MH, and BRVO-CME (Table 3).
The preoperative absolute value of aniseikonia showed a significant correlation with preoperative BCVA in all cases (r = 0.252, p < 0.0001, Fig. 5a), while the postoperative absolute value of mean aniseikonia was associated with postoperative BCVA (r = 0.201, p < 0.0001, Fig. 5b). Subgroup analysis showed a significant correlation between preoperative aniseikonia and BCVA in ERM and MH. Postoperative aniseikonia was significantly associated with postoperative BCVA only in M-off RD (Table 4).
Discussion
In our present study, preoperative and postoperative aniseikonia was assessed with the NAT in patients with various retinal disorders and was compared with each other. In addition, we identified the characteristics of aniseikonia in each of the disorders.
Overall, more than half the retinal disorders accompanied aniseikonia. The absolute value of aniseikonia was 3.4%, and aniseikonia ranged from -21.5% to +19.5%. From a clinical perspective, symptoms were induced only when the percentage of aniseikonia reached more than 3–5% [23]. Nevertheless, discomfort levels tended to vary among different individuals based on their binocular fusion tolerance and stereopsis was able to tolerate up to 5% aniseikonia [10, 11]. Aniseikonia induces various symptoms such as headache, asthenopia, photophobia, reading difficulty, nausea, vertigo, and dizziness [1, 2]. Thus, it is probable that quality of life is impaired in patients with retinal disorders who exhibit severe aniseikonia.
The hypothesis of retinally induced aniseikonia may be associated with altered distribution of photoreceptors. If the photoreceptors are compressed closely, the object image stimulates a larger number of receptors and appears larger than it actually is (i.e., macropsia). Contrastingly, when the photoreceptors are stretched apart, the object image stimulates less receptors and tends to appear smaller (i.e., micropsia) [9]. As preoperative characteristics of aniseikonia in each disorder, macropsia was dominant in ERM, whereas micropsia was conspicuous in MH, BRVO-CME, CRVO-CME, and DME. Postoperatively, the distribution of aniseikonia was unchanged in ERM, BRVO-CME, CRVO-CME, and DME, while the proportion of micropsia decreased in MH (Fig. 2).
Macular contraction due to ERM distorts the distribution of photoreceptors. Thus, it is known that ERM is a representative disorder that exhibits macropsia. A majority of ERM patients presented macropsia in this study, which was consistent with the findings of previous reports [11–14]. In RVO-CME and DME, it was presumed that the retina was stretched due to outer retinal cyst and serous retinal detachment, resulting in micropsia. In the retinal structure of MH patients, serous retinal detachment and/or outer retinal cyst (fluid cuff) appeared during the forming process so that the photoreceptors were stretched apart. This was presumably a reason that many MH patients exhibited micropsia. Approximately half of M-off RD patients had micropsia and most of M-on RD patients had no aniseikonia. It was known that a major cause of micropsia in M-off RD was persistent and/or transient CME, subretinal fluid, and retinal displacement due to gas tamponade [19]. The postoperative scores in M-on RD were significantly lower than those in all the other disorders. The result was reasonable because there was no damage involving the macula. Of 69 patients with M-on RD, 13 (19%) had macropsia. Of the 13 macropsic eyes, ten had ERM but the other three eyes did not exhibit any abnormal morphologic change. In M-on RD patients, macropsia was caused by macular contraction due to ERM following surgery.
The severity of preoperative and postoperative aniseikonia showed a wide variation depending on the type of disease (Fig. 3). We found that preoperative aniseikonia in ERM was relatively high compared with other disorders. Postoperatively, no difference was observed among NC, MH, and M-on RD. In contrast, postoperative aniseikonia remained in ERM, RVO-CME, DME, and M-off RD. Previous studies reported that preoperative and postoperative aniseikonia (5.7 - 8.0 degrees of visual field angles) in ERM was 5.0% - 6.6% and 4.1% - 6.5%, respectively [12–14], and postoperative aniseikonia in RD was -2.3%[19]. These values were consistent with our results. However, subjects with ERM and RD partially overlapped in our previous reports [12, 19]. It can be considered that distortion of the distribution of photoreceptors due to macular contraction in ERM is greater than the distortion caused by retinal stretch in CME and/or serous retinal detachment so that aniseikonia scores tend to be higher in ERM.
The relationship between the severity of ERM and aniseikonia is unknown. However, a previous report on aniseikonia in ERM investigated preoperative aniseikonia was associated with thickness of the ganglion cell layer (GCL) and inner nuclear layer (INL), and postoperative aniseikonia had a significant correlation with central foveal thickness, GCL and INL thickness. In addition, Asaria et al. [24] reported that ERM patients with a longer duration of symptoms before surgery had worse stereopsis both preoperatively and postoperatively. Longer duration and severe ERM may be caused by deterioration in aniseikonia.
In our present study, there were four cases with CME (5%) and two cases with transient subretinal fluid (2%) caused by ERM. These cases had relatively small values of macropsia compared with typical ERM. Macropsia due to ERM may be offset by micropsia due to CME or subretinal fluid.
As shown in the results, vitrectomy significantly improved aniseikonia and visual acuity overall. Subgroup analysis showed visual acuity increased in all disorders except CRVO-CME, while aniseikonia improved only in MH. These results suggest that even after successful vitrectomy and improvement of visual acuity, abnormal distribution of photoreceptors cannot be restored. Therefore, it seems that aniseikonia testing is a highly sensitive measurement to evaluate visual function in patients with foveal disorders. In ERM, irregular traction of the retina is observed in various directions. As a result, even if the retina is restored to an almost normal condition by membrane peeling, the distribution of photoreceptors may not be restored. In contrast, as MH accompanies concentric and efferent movement of retinal photoreceptors, it is considered that the distribution of photoreceptors can be restored with comparative ease in MH by surgery. In addition, visual function is not impaired at an early stage of ERM, RVO-CME, and DME, so that the duration from onset to surgery tends to be relatively long. Irreversible photoreceptor cell loss and changes in cone-cell alignment were caused by prolonged macular traction in eyes with DME or BRVO [25, 26]. Therefore, a long disease duration often observed in ERM, RVO-CME, and DME may cause disruption of photoreceptor cells and result in a permanent change of cone cell alignment. Previous studies reported better recovery of visual acuity and better improvement of aniseikonia in ERM patients who had surgery at an earlier date [14]. Since visual acuity decreases quickly as soon as MH develops, the duration from onset to surgery tends to be short in MH. This might be a reason that aniseikonia was better improved in MH.
Overall, preoperative aniseikonia was significantly associated with postoperative aniseikonia as well as changes in aniseikonia. Subgroup analysis revealed that preoperative aniseikonia showed a correlation with postoperative metamorphopsia in all disorders except DME. It is suggested that surgical treatment should be considered as early as possible after a vitreoretinal disorder is recognized, so that vitrectomy can be performed to prevent further deterioration of the patient’s aniseikonia.
Overall, preoperative aniseikonia was significantly associated with preoperative visual acuity, and postoperative aniseikonia was significantly related to postoperative visual acuity. However, subgroup analysis revealed that preoperative aniseikonia showed a correlation with preoperative visual acuity only in ERM and MH, and postoperative aniseikonia was associated with postoperative visual acuity only in M-off RD. In these disorders, relatively good visual acuity was maintained compared with the remaining disorders. Thus, it was considered that aniseikonia was associated with visual acuity only when visual acuity was relatively good. An explanation for no association between aniseikonia and visual acuity in M-on RD was that visual acuity was unchanged and remained at a relatively high level before and after surgery. Regarding RVO-CME and DME, it was possible that we could not find any association, because the numbers of cases were small.
Retinally induced aniseikonia cannot be corrected fully with conventional optics because it is field-dependent aniseikonia [10]. Besides aniseikonia, the induction of postoperative anisophoria poses another problem. Wright et al. assessed binocularity in patients after successful RD surgery, and observed aniseikonia in 35% and diplopia in 18% [27]. Our study did not examine diplopia. It will be necessary to evaluate the relation between aniseikonia and binocularity in patients with retinal disorders in order to treat retinally induced aniseikonia. In addition, our hypothesis about retinally induced aniseikonia may be associated with altered distribution of photoreceptors. However, it is not possible to prove it, because the distribution of photoreceptors of the pathologic retina cannot be detected by OCT. It is therefore difficult to guess the amount of aniseikonia from OCT findings in retinal disorders.
Our study had several limitations. First, the sample size was rather small, especially patients with BRVO, CRVO, and DME. That may have influenced the aniseikonia results. Second, postoperative follow-up was short. Previous studies reported that visual acuity in patients with ERM improved more at 1-3 years postoperatively than at 6 months postoperatively [28]. In addition, visual acuity in patients with RD improved more even at 1 to 5 years postoperatively [29, 30]. Aniseikonia improved for the period between 7 and 45 months postoperatively in patients who experienced retinal detachment [18]. Thus, longer-term investigations of patients after vitrectomy might give somewhat different results regarding aniseikonia. Third, patient selection of BRVO-CME, CRVO-CME, and DME may be inadequate. In this study, vitrectomy was indicated to patients with persistent CME that was not resolved after administration of corticosteroid and/or anti-VEGF agents. Therefore, it was possible that we only selected patients with poor visual outcome. Future studies with a larger sample size, longer follow-up period, and appropriate patient selection will further facilitate our understanding of aniseikonia in patients with retinal disorders.
In conclusion, we investigated pre- and postoperative aniseikonia in various retinal disorders. More than half of the patients had aniseikonia. Macropsia was dominant in ERM, and micropsia was conspicuous in MH, RVO-CME, DME, and macula-off RD. Aniseikonia was most severe in ERM. Vitrectomy improved aniseikonia only in MH.
References
Berens C, Aniseikonia BRE (1963) A present appraisal and some practical considerations. Arch Ophthalmol 70:181–188
Kramer PW, Lubkin V, Pavlica M, Covin R (1999) Symptomatic aniseikonia in unilateral and bilateral pseudophakia. A projection space eikonometer study. Binocul Vis Strabismus Q 14:183–190
Katsumi O, Miyanaga Y, Hirose T et al (1988) Binocular function in unilateral aphakia. Correlation with aniseikonia and stereoacuity. Ophthalmology 95:1088–1093
Crone RA, Leuridan OM (1975) Unilateral aphakia and tolerance of aniseikonia. Ophthalmologica 171:258–263
Snead MP, Lea SH, Rubinstein MP et al (1991) Aniseikonia: a method of objective assessment in pseudophakia using geometric optics. Ophthalmic Physiol Opt 11:109–112
Häring G, Gronemeyer A, Hedderich J, de Decker W (1999) Stereoacuity and aniseikonia after unilateral and bilateral implantation of the Array refractive multifocal intraocular lens. J Cataract Refract Surg 25:1151–1156
Katsumi O, Miyajima H, Ogawa T, Hirose T (1992) Aniseikonia and stereoacuity in pseudophakic patients. Unilateral and bilateral cases. Ophthalmology 99:1270–1277
Gobin L, Rozema JJ, Tassignon MJ (2008) Predicting refractive aniseikonia after cataract surgery in anisometropia. J Cataract Refract Surg 34:1353–1361
Benegas NM, Egbert J, Engel WK, Kushner BJ (1999) Diplopia secondary to aniseikonia associated with macular disease. Arch Ophthalmol 117:896–899
de Wit GC, Muraki CS (2006) Field-dependent aniseikonia associated with an epiretinal membrane a case study. Ophthalmology 113:58–62
Ugarte M, Williamson TH (2005) Aniseikonia associated with epiretinal membranes. Br J Ophthalmol 89:1576–1580
Okamoto F, Sugiura Y, Okamoto Y et al (2014) Time course of changes in aniseikonia and foveal microstructure after vitrectomy for epiretinal membrane. Ophthalmology 121:2255–2260
Chung H, Son G, Hwang DJ et al (2015) Relationship Between Vertical and Horizontal Aniseikonia Scores and Vertical and Horizontal OCT Images in Idiopathic Epiretinal Membrane. Invest Ophthalmol Vis Sci 56:6542–6548
Han J, Han SH, Kim JH, Koh HJ (2016) Restoration of retinally induced aniseikonia in patients with epiretinal membrane after early vitrectomy. Retina 36:311–320
Rutstein RP (2012) Retinally induced aniseikonia: a case series. Optom Vis Sci 89:e50–55
Curtin BJ, Linksz A, Shafer DM (1959) Aniseikonia following retinal detachment. Am J Ophthalmol 47:468–471
Ugarte M, Williamson TH (2006) Horizontal and vertical micropsia following macula-off rhegmatogenous retinal-detachment surgical repair. Graefes Arch Clin Exp Ophthalmol 244:1545–1548
Sjöstrand J, Anderson C (1986) Micropsia and metamorphopsia in the re-attached macula following retinal detachment. Acta Ophthalmol (Copenh) 64:425–432
Okamoto F, Sugiura Y, Okamoto Y et al (2014) Aniseikonia and Foveal Microstructure after Retinal Detachment Surgery. Invest Ophthalmol Vis Sci 55:4880–4885
Lee HN, Lin KH, Tsai HY et al (2014) Aniseikonia following pneumatic retinopexy for rhegmatogenous retinal detachment. Am J Ophthalmol 158:1056–1061
Frisén L, Frisén M (1979) Micropsia and visual acuity in macular edema. A study of the neuro-retinal basis of visual acuity. Albrecht Von Graefes Arch Klin Exp Ophthalmol 210:69–77
Hisada H, Awaya S (1992) Aniseikonia of central serous chorioretinopathy. Nihon Ganka Gakkai Zasshi 96:369–374
de Wit GC (2008) Clinical usefulness of the Aniseikonia Inspector: a review. Binocul Vis Strabismus Q 23:207–214
Asaria R, Garnham L, Gregor ZJ, Sloper JJ (2008) A prospective study of binocular visual function before and after successful surgery to remove a unilateral epiretinal membrane. Ophthalmology 115:1930–1937
Murakami T, Tsujikawa A, Ohta M et al (2007) Photoreceptor status after resolved macular edema in branch retinal vein occlusion treated with tissue plasminogen activator. Am J Ophthalmol 143:171–173
Lardenoye CW, Probst K, DeLint PJ, Rothova A (2000) Photoreceptor function in eyes with macular edema. Invest Ophthalmol Vis Sci 41:4048–4053
Wright LA, Cleary M, Barrie T, Hammer HM (1999) Motility and binocularity outcomes in vitrectomy versus scleral buckling in retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol 237:1028–1032
Pesin SR, Olk RJ, Grand MG et al (1991) Vitrectomy for premacular fibroplasia: prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology 98:1109–1114
Oshima Y, Yamanishi S, Sawa M et al (2000) Two-year follow-up study comparing primary vitrectomy with scleral buckling for macula-off rhegmatogenous retinal detachment. Jpn J Ophthalmol 44:538–549
Chang SD, Kim IT (2000) Long-term visual recovery after scleral buckling procedure of rhegmatogenous retinal detachment involving the macula. Korean J Ophthalmol 14:20–26
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Okamoto, F., Sugiura, Y., Okamoto, Y. et al. Aniseikonia in various retinal disorders. Graefes Arch Clin Exp Ophthalmol 255, 1063–1071 (2017). https://doi.org/10.1007/s00417-017-3597-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3597-x