Abstract
Purpose
The purpose was to investigate the impact of ultraviolet light corneal collagen crosslinking (UV-CXL) on the success rate and clinical outcome of subsequent deep anterior lamellar keratoplasty (DALK) in eyes with keratoconus (KC).
Methods
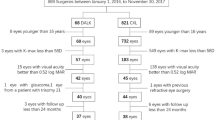
Medical records of 101 consecutive eyes with KC scheduled for big-bubble DALK surgery were screened retrospectively for details of previously performed UV-CXL, as well as intra- and postoperative complications of DALK surgery. Main outcome measures were intraoperative success rates (big-bubble formation, conversion to penetrating keratoplasty (PK)), postoperative complications, best corrected visual acuity (BCVA), endothelial cell density (ECD), and central corneal thickness (CCT) within 18 months of follow-up.
Results
Out of the 101 KC eyes, eight eyes (7.9%) had a history of previous UV-CXL. Surgical failure, defined as conversion to PK due to macroperforation, occurred in 17 eyes (16.8%) of 93 eyes without and in none with previous UV-CXL (P < .001). Failure to achieve a big-bubble occurred in 37 eyes (40.2%) without previous UV-CXL and in two eyes (25%) with previous UV-CXL. Microperforations of Descemet’s membrane were observed in ten eyes (20.7%) without and in 14 eyes (15.2%) with previous UV-CXL (P = .16). No significant differences could be detected for either the postoperative complication rate (P ≥ .18) or the clinical outcome parameters at 18 months follow-up, including BCVA, ECD and CCT (P ≥ .08) for eyes with or without UV-CXL.
Conclusions
In DALK surgery, prior UV-CXL does not seem to affect the rate of intra- or postoperative complications, the success rate, or its clinical outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Treatment of keratoconus (KC) has become much more diverse in recent years [20]. Additions to established conservative standard therapies, such as the adjustment of rigid contact lenses, include ultraviolet light corneal collagen crosslinking with riboflavin (UV-CXL), big-bubble deep anterior lamellar keratoplasty (DALK) and intracorneal ring segments (ICRS) [20, 21, 32].
KC eyes are typically marked by corneal thinning and an increase in the anterior and/or posterior curvatures of the cornea leading to high myopia and irregular astigmatism. The effect of riboflavin/UV-A corneal crosslinking is based on the ability to form additional crosslinking bonds between stromal proteins [3, 11]. The aim of this treatment is to arrest the progression of keratoconus, and thereby prevent further deterioration in vision and the need for corneal transplantation [18, 28]. In humans, Wollensak et al. in 2003 were the first to successfully apply UV-CXL [31], and on April 18, 2016 it received FDA approval.
Historically, UV-CXL has been regarded as suitable only for mild to moderate cases, but its application in more advanced stages of KC is growing [6, 20, 21]. While an increase of anterior stromal stiffness has been reported in various studies, a satisfactory investigation of the elasticity and viscoelasticity of the stromal depth has not yet been done [3, 4, 11, 12, 20, 21, 25]. This is of importance in eyes with advanced KC, which underwent UV-CXL, but nonetheless experienced progression of ectasia, insufficient BCVA, or contact lens intolerance. Traditionally, full thickness penetrating keratoplasty (PK) has been the standard of care for advanced keratoconus (KC) [20, 27]. Since the introduction of deep anterior lamellar keratoplasty (DALK) with the complete removal of the recipient’s corneal stroma in 1997, there has been a steady increase in its adoption during the last years [7, 9, 22, 29]. In fact, the American Academy of Ophthalmology (AAO) recently suggested that DALK is a safer technique as compared to PK [22].
Nonetheless, there is only little evidence regarding the effect of previous UV-CXL on the success and outcome of subsequent DALK [15]. Therefore, the purpose of the present study is to evaluate the success rate of DALK using the big-bubble technique in eyes with a history of previous UV-CXL as compared to untreated KC eyes.
Patients and methods
In this retrospective, nonrandomized, single-center cohort study, we reviewed clinical records of patients with KC who were scheduled for DALK surgery at the Department of Ophthalmology, University of Cologne, Cologne, Germany between 1 July 2011 and 31 December 2015. Patient data were collected in the Cologne DALK database.
Medical history of KC eyes was reviewed for previously performed UV-CXL according to the Dresden protocol as reported before [31]. The success rate of DALK surgery and conversion rate to penetrating keratoplasty (PK), as well as further intraoperative complications and clinical outcome parameters were collected for eyes with and without previous UV-CXL. This nonrandomized, clinical study was approved by the institutional review board (15-301) and was conducted in adherence to the tenets of the Declaration of Helsinki.
Inclusion and exclusion criteria
Deep anterior lamellar keratoplasty (DALK) was only performed if visual acuity could no longer be corrected by means of contact lenses or contact lens were not tolerated and BCVA without contact lens was insufficient.
All eyes with keratoconus requiring corneal transplantation and that were scheduled for big-bubble DALK surgery were consecutively included in this study.
Exclusion criteria for recipient eyes were a history of any keratoplasty in the past, other diseases leading to corneal ectasia including pellucid marginal degeneration, Terrien Marginal Degeneration, and ectasia after refractive surgery (such as Laser-in-situ-Keratomileusis (LASIK) or radial keratotomy). Furthermore, pseudophakic eyes, eyes with known history of severe ocular trauma, recurrent keratitis of unknown origin, uveitis, significant immunosuppression, Steven-Johnson syndrome or graft-versus-host-disease were excluded.
For statistical analysis concerning BCVA, partial exclusion criteria were visual acuity limiting factors, such as amblyopia. Furthermore, patients with severe mental retardation, such as Down syndrome, were excluded.
Donor preparation and surgical technique
All patients underwent surgery under general anesthesia and under steady state conditions in the eye hospital. DALK was performed in a standardized fashion using the big-bubble technique as described previously [1, 2] by two experienced corneal surgeons (C.C., B.O.B.). If big-bubble DALK could not be performed successfully, the micro-bubble incision technique was applied [24], or the Descemet membrane (DM) was manually dissected by separation of the adherent recipient corneal stroma with a knife. In case of intraoperative macroperforation of recipient’s DM, the surgery was converted to perforating keratoplasty. If intraoperative microperforation of DM occurred, whenever possible, the corneal transplantation was completed as DALK. If necessary, the anterior chamber was then filled with air to support the postoperative attachment of DM to the DALK graft.
From donor lenticules, DM was peeled off with fine, nontoothed forceps and the corresponding tissue was punched with a 7–8 mm trephine, usually using the DM for DMEK in split-cornea transplantation [13, 14]. Afterwards, the donor lenticule was secured with 10-0 monofilament nylon by 16 interrupted sutures or two 8-bite double-running diagonal cross-stitch sutures.
Conversion rate to perforating keratoplasty and intraoperative complications
Intraoperative complications were recorded and categorized as follows: Unsuccessful application of the big-bubble technique requiring use of either the micro-bubble DALK incision technique or manual dissection, microperforation or macroperforation of DM with or without conversion to PK.
Postoperative course
All patients received routine postoperative management in the form of topical prednisolone acetate 1% in tapering doses over several months and topical antibiotic drops (fluoroquinolones) for 1 to 2 weeks. The steroid medication was continuously tapered to one time a day after 4 months and discontinued after 1 year. Half of the sutures were removed 12 months after DALK, and the remaining sutures after 18 months.
Clinical information and collected data of recipients
Directly prior to surgery and 3 months after total removal of corneal sutures (17.4 ± 3.6 months postoperatively), standardized eye examinations, including best corrected visual acuity (BCVA) with manifest subjective refraction (trial glasses in a trial frame), central corneal thickness (Orbscan, Bausch & Lomb, Berlin, Germany), endothelial cell density (Tomey EM-3000 Specular Microscope, Tomey, Erlangen, Germany) were performed, as well as slit lamp examination and funduscopy. Postoperative complications were recorded and categorized as follows: For postoperative DM detachment, both the number of conservatively managed detachments and the number of patients in which intra-cameral air injection (re-bubbling) was required, the loosening of sutures during the postoperative course, persistent epithelial defects, interface opacifications, DM folds at 18 months follow-up, primary graft failure and graft rejections during the follow-up period.
Statistical analyses
Descriptive data for keratoconus eyes scheduled for DALK and corresponding donor tissues were collected in Microsoft Excel 2000 for Windows and analysed using SPSS (version 22.0 for Windows; SPSS, Inc., Chicago, IL). For statistical significance testing for interval scale parameters, Student’s t-test and the chi-square test were used for ordinal scale parameters. Differences regarding the intraoperative complication rate between the two surgeons were determined by means of the Mann-Whitney U test. BCVA was analysed in the logarithm of the minimum angle of resolution (logMAR) equivalent units. The level of significance was defined as P < .05.
Results
Demographic data of recipient eyes scheduled for DALK surgery
One hundred and one eyes of 101 patients with KC (mean age 40.5 ± 14.5 years; 79 males, 22 females) scheduled for big-bubble DALK were included. Thereof, eight eyes (7.9%; mean age 43.3 ± 17.4 years; six males, two females) had a history of UV-CXL, which was performed 5 ± 1.8 years prior to DALK surgery (range, 2–7 years).
Intra- and postoperative complications in eyes with previous UV-CXL undergoing DALK
In two (25.0%) of eight eyes with UV-CXL, big-bubble formation failed and the micro-bubble incision technique was applied for lamellar dissection. Microperforation of Descemet’s membrane (DM) occurred in two eyes (25.0%), but no macroperforation (0%). DALK surgery could be performed successfully in all eight eyes (100%) with a history of UV-CXL, and in no eyes (0%) conversion to penetrating keratoplasty (PK) was required.
Out of the eight eyes with UV-CXL, five were available for clinical outcome analysis and recording of postoperative complications. Three eyes were excluded for clinical outcome analysis because total suture removal and final examination at 18 months had not been performed yet.
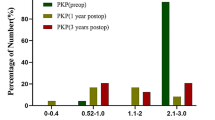
Mean ± SD best corrected visual acuity (BCVA) in eyes with UV-CXL was 0.60 ± 0.52 logMAR prior to DALK, and 0.13 ± 0.06 logMAR at the final examination. The mean ± SD central corneal thickness (CCT) was 469.0 ± 48.7 μm prior to corneal transplantation, and 597.5 ± 5.0 μm at 18 months.
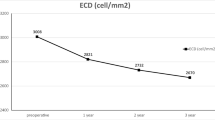
Endothelial cell density (ECD) was 2628 ± 181 cells/mm2 preoperatively, and at 18 months postoperatively 2505 ± 151.3 cells/mm2.
In the postoperative course, one eye (20.0%) showed loosened sutures during the observation period, but resuturing was not required. Re-bubbling was performed in one eye (20.0%) with postoperative DM detachment during the first postoperative week. Persistent epithelial defect occurred in one eye (20.0%) and responded to subsequent medical treatment. There was no case of primary graft failure or stromal graft rejection (Table 1).
Intra- and postoperative complications in eyes without previous UV-CXL undergoing DALK
In 37 eyes (40.2%) of the 93 without a history of UV-CXL, big-bubble formation failed and the micro-bubble incision technique was applied to separate the corneal stroma. Macroperforation of DM during surgery occurred in 19 eyes (20.7%), and microperforation in 14 eyes (15.2%). DALK surgery could be performed in 76 eyes (81.7%), while in 17 eyes (18.3%) conversion to PK was required due to macroperforation.
All DALKs were performed by two experienced surgeons (C.C., B.O.B.). The first surgeon performed 72 DALKs (71.3%), and thereof seven eyes with previously performed UV-CXL. The second surgeon performed 29 DALKs (28.7%), and thereof one case with history of UV-CXL. Regarding the intraoperative complication rate no statistical difference could be observed (P ≥ .051).
Of the eyes that did not undergo UV-CXL, 48 were available for the analysis of clinical outcome and postoperative complications.
Mean ± SD BCVA was 0.94 ± 0.42 logMAR prior to DALK, and 0.25 ± 0.11 logMAR at the final examination. Mean ± SD CCT was 390.8 ± 66.4 μm prior to corneal transplantation, and 577.4 ± 53.8 μm at 18 months.
Endothelial cell density preoperatively was 2398.9 ± 345.7 cells/mm2, and at 18 months postoperatively was 2025 ± 542.9 cells/mm2.
Twelve eyes (25.0%) showed loosened sutures during the observation period, but resuturing was required in only two eyes (4.2%). In 5 eyes (10.4%), DM detachment occurred. In four of these eyes (80.0%), re-bubbling was performed, while in one eye (20%) DM detachment was managed conservatively. A poor ocular surface leading to persistent epithelial defect was seen in six eyes (12.5%). Five of six responded to medical treatment or a bandage contact lens. In one of six eyes, amniotic membrane transplantation and tarsorrhaphy was necessary when ulcerative keratitis was diagnosed. Response to this treatment could be observed. There was no case of primary graft failure or stromal graft rejection, respectively (Table 1).
Impact of UV-CXL on the outcome of DALK surgery
DALK was performed successfully in 100% of UV-CXL eyes, whereas conversion to PK was required in 18.3% of the eyes without UV-CXL (P < .001). Occurrence of microperforation of DM showed no association with a history of UV-CXL (P = .16).
The clinical outcome was comparable within both groups (Fig. 1) for all parameters including BCVA (P = .08), CCT (P = .66), and ECD (P = .24). Furthermore, postoperative complication rates did not show any significant association with previously performed UV-CXL (P ≥ .18).
Clinical outcome of deep anterior lamellar keratoplasty in eyes with and without previous ultraviolet corneal collagen crosslinking. Box plots for clinical outcome parameters at 18 months follow-up are shown for both groups (with and without previous ultraviolet corneal collagen crosslinking (UV-CXL)). Boxes represent first quartile, median and third quartile values; whiskers represent extreme values. Only eyes which underwent total removal of sutures and final examination at 18 months follow-up were included in the analysis of clinical outcome parameters. P values < .05 were considered statistically significant. Left: For best corrected visual acuity with manifest subjective refraction (trial glasses in a trial frame), middle: central corneal thickness, and right: endothelial cell density, no statistically significant differences could be revealed at 18 months (P ≥ .08)
Discussion
This study is the first to analyse the impact of previous ultraviolet corneal crosslinking (UV-CXL) on subsequent DALK surgery success in keratoconus patients. Our results may suggest there is no correlation between a history of UV-CXL and either intraoperative complication rate or clinical outcome in subsequent deep anterior lamellar keratoplasty. In fact, these pretreated corneas showed higher rates of success in big-bubble formation and higher rates of successful completion of DALK surgery.
DALK seems to be the superior approach for treating anterior corneal pathology in eyes with a healthy endothelium, as it eliminates the possibility of endothelial rejection that may result in graft failure [5, 19, 23, 24, 26]. One of the reasons for the hesitant application of DALK might be the simple fact that there are now fewer patients requiring keratoplasty in the first place due to effective prevention of the progression of keratoconus by UV-CXL [6, 20]. Another reason is certainly the more complex surgical technique, and the rate of cases in which an intraoperative change from DALK to perforating keratoplasty is required [10, 17, 20, 30]. Therefore, many surgeons may refrain from applying the DALK technique, especially in complicated or unpredictable cases, such as those with a history of UV-CXL. Our data suggest that DALK can be as safely and as satisfactorily performed after previous UV-CXL as compared to non-crosslinked eyes.
Due to the rapid adoption of UV-CXL in keratoconus patients worldwide, the number of patients with previously performed UV-CXL will increase significantly in future. Although > 90% of keratoconus patients benefit from the treatment, there are still patients suffering from KC progression despite UV-CXL, or who have insufficient BCVA and thus require corneal transplantation [8, 16, 20]. Therefore, our data are relevant to demonstrate that the rate of intra- and postoperative complications does not seem to increase after previously performed crosslinking. The reason may involve the depth of the layer in which big-bubble separation of DM from adherent stroma occurs, namely below the one where crosslinking is achieved. A more robust anterior stroma may in fact cause tissue characteristics that are beneficial for a successful air injection and big-bubble formation, thus explaining the apparently better rates of big-bubble formation observed in our study in precrosslinked eyes. In a porcine model, Dias et al. found increasing stiffness in the anterior stroma, but no significant changes at a stromal depth of 200 μm [11]. Therefore, they concluded that UV-CXL seems to be limited to the anterior stroma and does not extend to the deeper stromal region [11]. So far, comparable investigations on human corneas have been very limited [15]. Iovieno et al. reported about a series of patients who had UV-CXL and underwent the big-bubble technique for DALK for keratoconus progression. Our results are in line with the data of Iovieno et al. in that we can confirm that eyes that underwent UV-CXL should not be excluded for DALK [15].
Our clinical results indicate a good visual outcome, confirming that DALK can be considered a safe alternative to PK, independent of a history of UV-CXL in the recipient eyes. In particular, as a further finding, we can conclude that there is no association between previously performed UV-CXL and complication rate during and following DALK surgery. Unexpectedly, we observed that the intraoperative complication rate was even significantly lower in the UV-CXL eyes.
The major limitation of our study is the small number of included eyes with UV-CXL. Although the statistical power of our study may be low, evaluating the validity of our conclusions involves other factors, too. An increase in the number of cases will be difficult to achieve, because the number of patients needing a corneal transplantation despite having had UV-CXL is declining. Furthermore, we were not able to compare the exact numbers of injections or shape of bubbles during DALK surgery between eyes with and without a history of UV-CXL due to the retrospective design of our study. Thus, further prospective clinical studies are required to support our findings.
In summary, we could find no negative impact of previous UV-CXL on the complication rates and clinical outcome of DALK surgery. Our results may encourage surgeons to apply the DALK technique even in eyes with a history of previous UV-CXL.
References
Anwar M, Teichmann KD (2002) Big-bubble technique to bare Descemet’s membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 28:398–403
Anwar M, Teichmann KD (2002) Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet’s membrane. Cornea 21:374–383
Ashwin PT, McDonnell PJ (2010) Collagen cross-linkage: a comprehensive review and directions for future research. Br J Ophthalmol 94:965–970
Beshtawi IM, Akhtar R, Hillarby MC, O’Donnell C, Zhao X, Brahma A, Carley F, Derby B, Radhakrishnan H (2013) Biomechanical properties of human corneas following low- and high-intensity collagen cross-linking determined with scanning acoustic microscopy. Invest Ophthalmol Vis Sci 54:5273–5280
Borderie VM, Sandali O, Bullet J, Gaujoux T, Touzeau O, Laroche L (2012) Long-term results of deep anterior lamellar versus penetrating keratoplasty. Ophthalmology 119:249–255
Chan E, Snibson GR (2013) Current status of corneal collagen cross-linking for keratoconus: a review. Clin Exp Optom 96:155–164
Cohen AW, Goins KM, Sutphin JE, Wandling GR, Wagoner MD (2010) Penetrating keratoplasty versus deep anterior lamellar keratoplasty for the treatment of keratoconus. Int Ophthalmol 30:675–681
Craig JA, Mahon J, Yellowlees A, Barata T, Glanville J, Arber M, Mandava L, Powell J, Figueiredo F (2014) Epithelium-off photochemical corneal collagen cross-linkage using riboflavin and ultraviolet a for keratoconus and keratectasia: a systematic review and meta-analysis. Ocul Surf 12:202–214
Cursiefen C, Heindl LM (2011) Perspectives of deep anterior lamellar keratoplasty. Ophthalmologe 108:833–839
Cursiefen C, Schaub F, Bachmann B (2016) Update: Deep anterior lamellar keratoplasty (DALK) for keratoconus: when, how and why. Ophthalmologe 113:204–212
Dias J, Diakonis VF, Lorenzo M, Gonzalez F, Porras K, Douglas S, Avila M, Yoo SH, Ziebarth NM (2015) Corneal stromal elasticity and viscoelasticity assessed by atomic force microscopy after different cross linking protocols. Exp Eye Res 138:1–5
Goldich Y, Marcovich AL, Barkana Y, Avni I, Zadok D (2010) Safety of corneal collagen cross-linking with UV-A and riboflavin in progressive keratoconus. Cornea 29:409–411
Heindl LM, Riss S, Bachmann BO, Laaser K, Kruse FE, Cursiefen C (2011) Split cornea transplantation for 2 recipients: a new strategy to reduce corneal tissue cost and shortage. Ophthalmology 118:294–301
Heindl LM, Riss S, Laaser K, Bachmann BO, Kruse FE, Cursiefen C (2011) Split cornea transplantation for 2 recipients—review of the first 100 consecutive patients. Am J Ophthalmol 152:523–532
Iovieno A, Moramarco A, Coassin M, Baiocchi S, Caporossi A, Fontana L (2013) Big bubble DALK after CXL in keratoconic patients. J Refract Surg 29:801
Ivarsen A, Hjortdal J (2013) Collagen cross-linking for advanced progressive keratoconus. Cornea 32:903–906
Jhanji V, Sharma N, Vajpayee RB (2010) Intraoperative perforation of Descemet’s membrane during “big bubble” deep anterior lamellar keratoplasty. Int Ophthalmol 30:291–295
Kissner A, Spoerl E, Jung R, Spekl K, Pillunat LE, Raiskup F (2010) Pharmacological modification of the epithelial permeability by benzalkonium chloride in UVA/Riboflavin corneal collagen cross-linking. Curr Eye Res 35:715–721
Melles GR, Lander F, Rietveld FJ, Remeijer L, Beekhuis WH, Binder PS (1999) A new surgical technique for deep stromal, anterior lamellar keratoplasty. Br J Ophthalmol 83:327–333
Parker JS, van Dijk K, Melles GR (2015) Treatment options for advanced keratoconus: a review. Surv Ophthalmol 60:459–480
Pron G, Ieraci L, Kaulback K (2011) Collagen cross-linking using riboflavin and ultraviolet-a for corneal thinning disorders: an evidence-based analysis. Ont Health Technol Assess Ser 11:1–89
Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM (2011) Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty a report by the american academy of ophthalmology. Ophthalmology 118:209–218
Riss S, Heindl LM, Bachmann BO, Kruse FE, Cursiefen C (2012) Pentacam-based big bubble deep anterior lamellar keratoplasty in patients with keratoconus. Cornea 31:627–632
Riss S, Heindl LM, Bachmann BO, Kruse FE, Cursiefen C (2013) Microbubble incision as a new rescue technique for big-bubble deep anterior lamellar keratoplasty with failed bubble formation. Cornea 32:125–129
Schumacher S, Oeftiger L, Mrochen M (2011) Equivalence of biomechanical changes induced by rapid and standard corneal cross-linking, using riboflavin and ultraviolet radiation. Invest Ophthalmol Vis Sci 52:9048–9052
Senoo T (2001) Combined surgery with deep lamellar keratoplasty. Semin Ophthalmol 16:126–136
Shimazaki J (2000) The evolution of lamellar keratoplasty. Curr Opin Ophthalmol 11:217–223
Spoerl E, Wollensak G, Seiler T (2004) Increased resistance of crosslinked cornea against enzymatic digestion. Curr Eye Res 29:35–40
Sugita J, Kondo J (1997) Deep lamellar keratoplasty with complete removal of pathological stroma for vision improvement. Br J Ophthalmol 81:184–188
Unal M, Bilgin B, Yucel I, Akar Y, Apaydin C (2010) Conversion to deep anterior lamellar keratoplasty (DALK): learning curve with big-bubble technique. Ophthalmic Surg Lasers Imaging 41:642–650
Wollensak G, Spoerl E, Seiler T (2003) Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 135:620–627
Yeung SN, Lichtinger A, Ku JY, Kim P, Low SA, Rootman DS (2013) Intracorneal ring segment explantation after intracorneal ring segment implantation combined with same-day corneal collagen crosslinking in keratoconus. Cornea 32:1617–1620
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The German Research Foundation provided financial support in the form of the grant FOR 2240 “(Lymph) Angiogenesis And Cellular Immunity In Inflammatory Diseases Of The Eye” to C.C. and L.M.H. (www.for2240.de). The European Cooperation of Science and Technology (EU COST) provided financial support in the form of the grant BM1302 “Joining Forces in Corneal Regeneration” to B.O.B and C.C. (www.biocornea.eu). The sponsor had no role in design, conduct, or analysis of the study.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Schaub, F., Enders, P., Bachmann, B.O. et al. Effect of corneal collagen crosslinking on subsequent deep anterior lamellar keratoplasty (DALK) in keratoconus. Graefes Arch Clin Exp Ophthalmol 255, 811–816 (2017). https://doi.org/10.1007/s00417-017-3592-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3592-2