Abstract
Background
Some pseudophakic patients implanted with a monofocal intraocular lens (IOL) have good near visual acuity (VA) with their distance correction. The objective was to evaluate the prevalence of pseudo-accommodation in children after bilateral cataract surgery, without amblyopia, and to define its mechanisms.
Methods
Observational study that took place in a pediatric ophthalmology department, Paris, France. A total of 68 eyes were included, 40 from 23 children and 28 from 14 adults, with a corrected distance VA above 20/25 and a normal near VA (20/25) with +3 addition. Pseudo-accommodation was defined as a near VA better than 20/50 with the distance correction and without addition. Prevalence of pseudo-accommodation was calculated in each group. In order to determine the possible mechanisms of pseudo-accommodation in children, we compared children with pseudo-accommodation and adults without pseudo-accommodation regarding several parameters: refraction, axial length, corneal topography, aberrometry, pupillary diameter and IOL shift after cyclopentolate instillation.
Results
Among the children group, 36 (90 %) had pseudo-accommodation versus 2 (7 %) in the adult group. We found that spherical equivalent, implant power, corneal multifocality and corneal higher-order aberrations (mainly coma and trefoil) were significantly higher in the pseudo-accommodation group, while pupil diameter and implant shift were not significantly different.
Conclusions
Pseudo-accommodation has a high prevalence among non-amblyopic pseudophakic children. Several possible mechanisms have been found to explain pseudo-accommodation in children: a high power of the IOL and a small axial length, maximizing the effect of the IOL shift, corneal multifocality and corneal higher-order aberrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Some pseudophakic patients implanted with a monofocal intraocular lens (IOL) have good visual acuity (VA) at near and far with their distance correction. This phenomenon has been called “pseudo-accommodation” [1, 2]. The ocular parameters described to explain this apparent accommodation include astigmatism [3], pupil diameter [1, 4, 5], axial length [5], corneal multifocality [2] and aberrations [6], and myopia induced by the forward movement of the lens [5].
The importance of pseudo-accommodation decreases with age [7] and only 9 % of adults implanted with a monofocal lens have an uncorrected VA of 20/40 or better at distance and near [4]. This phenomenon seems to be more frequent in children, as shown in a recent study: 75 % of children who underwent bilateral cataract surgery had VA near and at distance greater than 20/40 without correction [8]. However, no study has tested the VA with solely distance correction, which seems interesting in order to assess the pseudophakic accommodation itself.
Furthermore, while mechanisms explaining the pseudo-accommodation have been fairly well studied in adults, this has not been the case in children [1–6].
Our first objective was to study the prevalence of pseudo-accommodation in pseudophakic children and pseudophakic adults in order to confirm its high prevalence in children compared to adults. The second objective was to understand the possible mechanisms of pseudo-accommodation in children, by comparing a children group with pseudo-accommodation and an adult group without pseudo-accommodation according to various clinical and paraclinical parameters.
Materials and methods
The study was retrospective and observational. It was approved by the institutional review board of our institution (Comité de Protection des Personnes Pitié-Salpêtrière, notice reference: CPP/132-13). Informed consent documents were signed by the parents of each patient.
The pediatric population was selected from a cohort of 88 children who underwent bilateral congenital or juvenile cataract surgery at the Fondation Ophtalmologique Adolphe de Rothschild between 2001 and 2014. We chose to select only bilateral cataracts in order to avoid as much as possible amblyopia, which is more common in unilateral cataracts [9–11]. The inclusion criteria were: children over 6 years at the time of examination, with a bilateral cataract operated on at least 6 months previously, with a corrected distance VA over 20/25 and a near VA of 20/25 with +3 addition. The surgery was performed by one of three surgeons (PLM, CE, PD). It consisted of clear corneal incision, anterior capsulorhexis, lens aspiration, posterior capsulotomy, anterior vitrectomy and implantation of an acrylic hydrophobic monofocal IOL in the posterior chamber. The IOL model was the surgeon’s choice. The power of the IOL was chosen after axial length (B-scan ultrasound) and keratometry measurements (Retinomax, Nikon®). The postoperative refractive target was hyperopia until 4 years and emmetropia after this age [12]. SRK T and Holladay formulas were used for IOL lens power calculation. Exclusion criteria were: per-operative and post-operative complications such as glaucoma, IOL shift, secondary proliferation or retinal detachment. Post-traumatic cataracts, uveitic cataracts and association with other ocular malformations (anterior segment dysgenesis, microphthalmia, persistent fetal vasculature) were not included.
The adult population was selected from a cohort of 140 patients older than 60 who had undergone surgery for bilateral age-related cataracts 6 to 12 months before. The intervention consisted of a standard phacoemulsification and placement of an acrylic hydrophobic monofocal IOL. Post-operative corrected distance VA had to be greater than 20/25 and near VA at 20/25.
For each patient included, medical history was noted as follows: age at the time of the study, age at surgery, preoperative axial length, preoperative mean keratometry (Km) and power and type of IOL implanted. All patients had measures of refraction (sphere, cylinder and spherical equivalent), corrected distance VA, near VA with distance correction, with and without a +3 addition, and slit-lamp biomicroscopy. The conditions of VA measurement were similar for all patients: Distance correction was measured objectively with an autorefractometer (Tonoref II®, Nidek) without dilatation. We tried to improve visual acuity at distance by adding +0.50 or −0.50. We kept the refraction corresponding to the best visual acuity at distance. The test at near distance was done with this same correction. The visual acuity at near distance was measured in the same conditions for all patients, children and adults. The optotype test chosen was the Parinaud scale, which is the most used text in France. The reading distance was measured at each exam at 35 cm with a ruler. Luminosity was the same. Those measures were performed by two examiners aware of the study objective. A series of additional tests was performed: axial length measurement (AL-Scan®, Nidek), corneal topography (ORB-Scan III®, Technolas), aberrometry (OPD-Scan II®, Nidek), pupillary diameter measurement (OPD-Scan II®, Nidek) and spectral domain optical coherence tomography (SD-OCT) of the anterior segment measuring the anterior chamber depth (OCT-Visante®, Zeiss). This measure was defined with a segment perpendicular to the IOL, passing through its center, from the anterior face of the IOL to the corneal endothelium. Three drops of cyclopentolate 0.5 % (Skiacol®, Alcon Laboratories) were then instilled into both eyes at 5-min intervals. Forty-five minutes later, measurement of near VA with distance correction was performed in the same conditions, with and without addition and a new depth chamber measurement with SD-OCT was performed under cyclopentolate. The shift of the implant between the two measurements was calculated.
Pseudo-accommodation was defined by a near VA measured with distance correction without addition of 20/50 or better. The 20/50 cut-off (P4 on scale) was chosen because the characters in textbooks and other books for children are equivalent to 20/80 or 20/100, but generally not less than 20/50. This threshold permitted a child to read optotypes easily in school books. The age of the children group was above 6 years, permitting assessment of the good feasibility of the reading test. If the patient could not read better than 20/50, the best near VA was measured. The group of children with pseudo-accommodation and the group of adults without pseudo-accommodation were compared on anamnestic factors (age, age at surgery, IOL power), spherical equivalent, axial length, pupillary diameter, minimal, maximal and mean keratometry (Kmin, Kmax, Km), multifocal corneal index (SimK), and corneal wavefront aberrations: total aberrations root mean square (RMS), higher order aberrations (HOAs) RMS, coma RMS, trefoil RMS, spherical aberration RMS, and Q factor. Results are given as mean ± standard deviation. Statistical analyses were based on the Levene test for normality and homogeneity of variance, and the nonparametric t test (Wilcoxon test). p values less than 0.05 were considered as significant.
Results
Patient characteristics
A total of 29 children were re-examined between November 2013 and March 2014. Twenty-three children (40 eyes) aged 9.8 ± 2.9 years fulfilled the study criteria and were included. They had undergone bilateral congenital or juvenile cataract surgery at the age of 3.6 ± 2.5 years. Distance VA was 20/20 in 85 % of the eyes.
The adults group consisted of 28 eyes of 14 patients aged 75.3 ± 7.6, examined 6 to 12 months after cataract surgery. Corrected distance VA was 20/20 for 82 % of them.
Patient characteristics are summarized in Table 1.
Prevalence of pseudo-accommodation in each group
In children, 36 of 40 eyes (90 %) had near VA of 20/50 or better with distance correction and without addition. After cycloplegia with cyclopentolate, among these 36 eyes, 23 (64 %) could still read 20/50 or better without addition. For the 4 eyes without pseudo-accommodation, near VA was 20/63 or 20/80.
In adults, 2 of 28 eyes (7 %) had near VA of 20/50 or better with distance correction and without addition. For the 26 others eyes, near VA was less than 20/100.
Possible mechanisms of pseudo-accommodation in children
The comparison of the two groups, “with pseudo-accommodation” (children, 36 eyes) and “without pseudo-accommodation” (adults, 26 eyes), exhibited several significant differences (Table 2).
The IOL power was significantly higher in the group with pseudo-accommodation (25.0 ± 3.5 D) than in the group without pseudo-accommodation (20.3 ± 3.6 D; p < 0.0001). The axial length was lower in the group with pseudo-accommodation (23.05 ± 1.21 mm) than in the group without pseudo-accommodation (24.10 ± 1.93 mm; p = 0.01). Furthermore, the type of IOL implanted was different: SN60WF and Asphina 509 M, which are aspherical IOLs, in adults, and SN60AT, SA60AT and MA60AC, which are spherical IOLs, in children.
Concerning refractive parameters, spherical equivalent, cylinder and sphere were significantly higher in absolute value in the group with pseudo-accommodation (p < 0.001). Astigmatism was within the rule in 72 % of eyes with pseudo-accommodation and in 10 % of eyes without pseudo-accommodation (p < 0.001). It was against the rule in 8 % of eyes with pseudo-accommodation and in 46 % of eyes without pseudo-accommodation (p < 0.05). Minimal and mean keratometry were steeper in the group without pseudo-accommodation (p = 0.007).
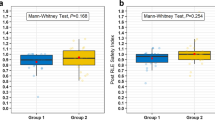
Concerning aberrometric parameters, SimK and Q factor, two indexes of corneal multifocality, were higher in the group with pseudo-accommodation (p < 0.007). In addition, the total aberration RMS, as well as HOAs RMS, trefoil RMS and coma RMS were significantly higher in the group with pseudo-accommodation (p < 0.0001). There was no significant difference concerning spherical aberration (Fig. 1).
Lastly, there was no significant difference for IOL shift and pupil diameter.
Discussion
In our study, the prevalence of pseudo-accommodation was higher in children than in adults. In the same conditions and with the same corrected distance VA, only 7 % of adults had pseudo-accommodation versus 90 % in children. Few data exist on the prevalence of the phenomenon of pseudo-accommodation in adults. Nanavaty et al. [4] mentioned a prevalence of 9 % of patients with distance and near VA greater than or equal to 20/40 in a series of 100 patients implanted with a monofocal lens. Concerning children, only Nihalani et al. [8] studied the prevalence of the phenomenon. In their study, among the children who underwent bilateral congenital cataract surgery, 75 % had uncorrected distance and near VA over 20/40. Several reasons can explain the higher prevalence of pseudo-accommodation in our study: amblyopia was excluded, 20/50 was chosen as cut-off and the testing conditions were different as patients were corrected for distance vision.
Interestingly, some patients (64 %) kept their pseudo-accommodation after cycloplegia. Pupillary diameter variations and IOL shift, therefore, cannot entirely explain their capacity to see well at near distance. Others factors, such as corneal multifocality or corneal aberrations, may play a role.
Comparing the two groups, “with pseudo-accommodation” and “without pseudo-accommodation”, we found several statistically significant factors, which may explain part of the mechanism of pseudo-accommodation.
First, IOL power was significantly larger and axial length smaller in the group with pseudo-accommodation. Yet, we know that the effect of IOL shift on the amplitude of accommodation depends on the IOL power and axial length [5]. In fact, for a given IOL shift, the greater the IOL power, the greater the amplitude of pseudo-accommodation. Then, even if IOL shift was not significantly different in the two groups, a similar shift would produce a more accommodative effect with an IOL of 25D than with an IOL of 20D. We cannot exclude the fact that some values were underestimated by imperfect cooperation of the patient when asked to look at near distances to measure the accommodative state, especially in children. We did not use pilocarpine for practical reasons because it would have required a second visit. For the measurements, we chose to use the anterior segment OCT, a non-contact method known as reliable for measuring the anterior chamber depth [13, 14]. Our results for the mean IOL shift between distance and near vision (41 ± 58 μm forward) were not different from those found in the literature [15, 16]. Most authors agree that this movement plays a minimal role in the pseudo-accommodation, which is consistent with our results [17–19]. In children, only Lesiewska Junk et al. [20] were able to find a positive correlation between the movement of the IOL and the amplitude of pseudo-accommodation; however, anterior chamber depth was measured by B ultrasound with the cooperation of the child, without the use of cycloplegia.
We did not find any significant difference of pupil diameter, but this is probably due to the age difference between both groups, as there is an induced miosis with age [21]. However, the reduction of pupil diameter for near vision is likely one of the mechanisms of pseudo-accommodation, by creating an increase of depth of focus, as shown by Nakazawa and Ohtsuki [1]. Moreover, we found that 36 % of the children who initially had pseudo-accommodation lost it after cyclopentolate, maybe because of the induced pupillary dilatation.
Low myopia with myopic astigmatism is known to provide good distance and near vision [3, 22, 23]. Although significant in our study, the differences found for spherical equivalent and astigmatism appear to play a minor role in the mechanisms of pseudo-accommodation, as patients were actually always tested with their distance correction. We attribute these differences to significant confounding factors, since in early childhood surgery, emmetropia is rarely achieved postoperatively, unlike in adults.
Finally, we showed that corneal multifocality was higher in the group with pseudo-accommodation, when measured with both Q factor and SimK. Corneal multifocality plays a role in the mechanism of pseudo-accommodation, as already shown by Fukuyama et al. [2] Oshika et al. [6] also found a significant correlation between apparent pseudo-accommodation and corneal multifocality, determined via topography by calculating the corneal refractive gradient (difference between Kmin and Kmax).
We also studied the role of corneal aberrations in pseudo-accommodation. Coma and trefoil were significantly higher in the group with pseudo-accommodation, unlike corneal spherical aberrations. Higher-order aberrations are known to play a role in pseudo-accommodation [24, 25]. Oshika et al. [6] also found a significant positive correlation between corneal coma aberration and pseudo-accommodation, but no correlation for spherical aberrations. Similarly, for Nishi et al. [26], a significant number of total comas with a low number of total spherical aberrations contribute to a larger amplitude of pseudo-accommodation. We did not find a significant difference for spherical aberration, maybe because of the type of IOL used in each group. Indeed, children received a spherical IOL and adults, an aspherical IOL. This may have been a confounding factor for our result concerning spherical aberration in each group.
The reason why coma and trefoil corneal aberrations appear to be more common in children than in adults after surgery remains unclear. According to Brunette et al. [27], the increase of corneal aberrations with age is not linear; the RMS error as a function of age was modeled by a second-order polynomial regression. It decreased progressively through childhood, adolescence and early adulthood, reached a minimum level during the fourth decade of life, then increased progressively with age, until age 82 [3]. Corneal aberrations, therefore, seem to be comparable in young children and senior adults. Furthermore, it is known that corneal aberrations increase after cataract surgery, due to keratotomy [28, 29]. Iseli et al. [30] showed that after cataract surgery with implantation, vertical and horizontal corneal coma and corneal spherical aberrations were significantly increased compared to normal eyes. However, because of a larger corneal incision and a more flexible cornea than in adults, it can be assumed that induced corneal aberrations are more important in children. Thus, overall, higher-order corneal aberrations, especially coma and trefoil, are more important in children after cataract surgery and could contribute to their pseudo-accommodation.
We found several confounders and bias that may have influenced the results. First, prevalence results are likely to be overestimated (90 %) in children because we chose to select only patients with good visual acuity at near and distance. Moreover, two examiners aware of the study objective, creating a measuring bias, performed visual acuity measurements. Finally, values concerning possible mechanisms were compared between the “pseudo-accommodation” group of children and the “non-accommodation” group of adults. The age is a confounding factor. We couldn’t compare children with pseudo-accommodation and without pseudo-accommodation because of too small a sample in the group without pseudo-accommodation.
Conclusion
Pseudo-accommodation in pseudophakic children has a remarkably high prevalence among non-amblyopic pseudophakic children. Several possible mechanisms contributing to pseudo-accommodation in children have been found: a high power of the IOL and a small axial length, maximizing the effect of the IOL shift, corneal multifocality and corneal higher-order aberrations, mainly coma and trefoil.
These results suggest that the optical correction of a pseudophakic child should be adapted to the degree of pseudo-accommodation and may not always include a 3-diopter addition, as is usually the case.
Several questions remain and would benefit from further longitudinal studies: What is the benefit of monofocal IOL compared with multifocal, and what will be the evolution of this pseudo-accommodation with age?
References
Nakazawa M, Ohtsuki K (1983) Apparent accommodation in pseudophakic eyes after implantation of posterior chamber intraocular lenses. Am J Ophthalmol 96:435–438
Fukuyama M, Oshika T, Amano S, Yoshitomi F (1999) Relationship between apparent accomodation and corneal multifocality in pseudophakic eyes. Ophthalmology 106:1178–1181
Huber C (1981) Planned myopic astigmatism as a substitute for accommodation in pseudophakia. J Am Intra-Ocul Implant Soc 7:244–249
Nanavaty MA, Vasavada AR, Patel AS et al (2006) Analysis of patients with good uncorrected distance and near vision after monofocal intraocular lens implantation. J Cataract Refract Surg 32:1091–1097. doi:10.1016/j.jcrs.2006.03.021
Nawa Y, Ueda T, Nakatsuka M et al (2003) Accommodation obtained per 1.0 mm forward movement of a posterior chamber intraocular lens. J Cataract Refract Surg 29:2069–2072
Oshika T, Mimura T, Tanaka S et al (2002) Apparent accommodation and corneal wavefront aberration in pseudophakic eyes. Invest Ophthalmol Vis Sci 43:2882–2886
Hayashi K, Hayashi H, Nakao F, Hayashi F (2003) Aging changes in apparent accommodation in eyes with a monofocal intraocular lens. Am J Ophthalmol 135:432–436
Nihalani BR, VanderVeen DK (2013) Uncorrected visual acuity in children with monofocal pseudophakia. J Cataract Refract Surg 39:419–424. doi:10.1016/j.jcrs.2012.09.021
Gouws P, Hussin HM, Markham RHC (2006) Long term results of primary posterior chamber intraocular lens implantation for congenital cataract in the first year of life. Br J Ophthalmol 90:975–978. doi:10.1136/bjo.2006.094656
Ledoux DM, Trivedi RH, Wilson ME, Payne JF (2007) Pediatric cataract extraction with intraocular lens implantation: visual acuity outcome when measured at age four years and older. J AAPOS 11:218–224. doi:10.1016/j.jaapos.2006.11.003
Chak M, Wade A, Rahi JS, British Congenital Cataract Interest Group (2006) Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British congenital cataract study. Invest Ophthalmol Vis Sci 47:4262–4269. doi:10.1167/iovs.05-1160
Enyedi LB, Peterseim MW, Freedman SF, Buckley EG (1998) Refractive changes after pediatric intraocular lens implantation. Am J Ophthalmol 126:772–781
Du C, Shen M, Li M et al (2012) Anterior segment biometry during accommodation imaged with ultralong scan depth optical coherence tomography. Ophthalmology 119:2479–2485. doi:10.1016/j.ophtha.2012.06.041
Chen Q, Leng L, Zhu D et al (2014) Fully automated biometry of in situ intraocular lenses using long scan depth spectral-domain optical coherence tomography. Eye Contact Lens 40:37–45. doi:10.1097/ICL.0000000000000005
Tsorbatzoglou A, Németh G, Széll N et al (2007) Anterior segment changes with age and during accommodation measured with partial coherence interferometry. J Cataract Refract Surg 33:1597–1601. doi:10.1016/j.jcrs.2007.05.021
Dhital A, Spalton DJ, Gala KB (2013) Comparison of near vision, intraocular lens movement, and depth of focus with accommodating and monofocal intraocular lenses. J Cataract Refract Surg 39:1872–1878
Findl O, Kiss B, Petternel V et al (2003) Intraocular lens movement caused by ciliary muscle contraction. J Cataract Refract Surg 29:669–676
Tsorbatzoglou A, Németh G, Máth J, Berta A (2006) Pseudophakic accommodation and pseudoaccommodation under physiological conditions measured with partial coherence interferometry. J Cataract Refract Surg 32:1345–1350. doi:10.1016/j.jcrs.2006.02.069
Legeais JM, Werner L, Werner L et al (1999) Pseudoaccommodation: BioComFold versus a foldable silicone intraocular lens. J Cataract Refract Surg 25:262–267
Lesiewska-Junk H, Kałuzny J (2000) Intraocular lens movement and accommodation in eyes of young patients. J Cataract Refract Surg 26:562–565
Nakamura K, Bissen-Miyajima H, Oki S, Onuma K (2009) Pupil sizes in different Japanese age groups and the implications for intraocular lens choice. J Cataract Refract Surg 35:134–138. doi:10.1016/j.jcrs.2008.10.020
Huber C (1981) Myopic astigmatism a substitute for accommodation in pseudophakia. Doc Ophthalmol 52:123–178
Datiles MB, Gancayco T (1990) Low myopia with low astigmatic correction gives cataract surgery patients good depth of focus. Ophthalmology 97:922–926
Nanavaty MA, Spalton DJ, Boyce J et al (2009) Wavefront aberrations, depth of focus, and contrast sensitivity with aspheric and spherical intraocular lenses: fellow-eye study. J Cataract Refract Surg 35:663–671. doi:10.1016/j.jcrs.2008.12.011
Cheng X, Bradley A, Thibos LN (2004) Predicting subjective judgment of best focus with objective image quality metrics. J Vis 4:310–321. doi:10.1167/4.4.7
Nishi T, Nawa Y, Ueda T et al (2006) Effect of total higher-order aberrations on accommodation in pseudophakic eyes. J Cataract Refract Surg 32:1643–1649. doi:10.1016/j.jcrs.2006.05.020
Brunette I, Bueno JM, Parent M et al (2003) Monochromatic aberrations as a function of age, from childhood to advanced age. Invest Ophthalmol Vis Sci 44:5438–5446
Ye H, Zhang K, Yang J, Lu Y (2014) Changes of corneal higher-order aberrations after cataract surgery. Optom Vis Sci 91(10):1244–50. doi:10.1097/OPX.0000000000000362
Marcos S, Rosales P, Llorente L, Jiménez-Alfaro I (2007) Change in corneal aberrations after cataract surgery with 2 types of aspherical intraocular lenses. J Cataract Refract Surg 33:217–226. doi:10.1016/j.jcrs.2006.10.021
Iseli HP, Jankov M, Bueeler M et al (2006) Corneal and total wavefront aberrations in phakic and pseudophakic eyes after implantation of monofocal foldable intraocular lenses. J Cataract Refract Surg 32:762–771. doi:10.1016/j.jcrs.2005.10.032
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Dénier, C., Dureau, P., Edelson, C. et al. Pseudo-accommodation in non-amblyopic children after bilateral cataract surgery and implantation with a monofocal intraocular lens: prevalence and possible mechanisms. Graefes Arch Clin Exp Ophthalmol 255, 407–412 (2017). https://doi.org/10.1007/s00417-016-3526-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3526-4