Abstract
Purpose
The purpose was to evaluate indications and clinical outcomes in paediatric corneal keratoplasty.
Methods
Fifty-four eyes of 43 patients who underwent corneal keratoplasty from the 1st of January 2010 through the 31st of December 2013 at the Bambino Gesù Children’s Hospital in Rome, Italy, were retrospectively evaluated. To assess the effect of age on graft failure rate, the recipient age was considered as a dichotomous variable (≤5 or >5 years) and a 2X2 table was developed, using the chi-square test for testing the statistical significance. Furthermore, two separate subgroup analyses were conducted on patients of ≤5 years and those of >5 years, to evaluate the effect of penetrating keratoplasty (PK) or deep anterior lamellar keratoplasty (DALK) on the graft failure rate. The level of statistical significance was set at p < 0.05
Results
Mean recipient age was 8.9 ± 5.7 [SD] years. Mean follow-up time was 22.8 months. Main preoperative diagnoses were keratoconus (37 %) and congenital glaucoma (20 %). Patients ≤5 years showed a higher percentage of graft failure (p = 0.0008). PK and DALK did not show statistically significant differences regarding the graft failure in both subgroups (p = 0.15 for ≤5 years group and p = 0.27 for >5 years group, respectively). However, across groups DALK provided a lower rate of graft failure.
Conclusions
Our findings suggest that children older than 5 years show a significantly better graft outcome and that DALK seems to offer greatest benefits in terms of failure risk in paediatric patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Paediatric keratoplasty still represents a very challenging surgery, and it is generally performed when corneal opacification induces a visual deprivation [1]. This condition requires a fast and effective treatment to prevent amblyopia in the youngest patients; however, mainly for these patients, the follow-up is not favourable. Indeed, Penetrating Keratoplasty (PK), actually the “gold standard” in paediatric corneal keratoplasty surgery, has shown a prognosis for graft survival of approximately 50–60 %, [2, 3] mainly due to endothelial rejection [4]. It has been reported that Deep Anterior Lamellar Keratoplasty (DALK), a lamellar transplantation surgical technique indicated for corneal diseases not affecting the endothelium, could improve the graft survival in a subset of children with stromal pathology by preventing endothelial rejection [5].
Anwar and Teichmann [6] introduced the big-bubble technique in DALK to facilitate pre-Descemet plane dissection, where air is injected into the deep stroma in the attempt to achieve a large air bubble between the Descemet membrane and the stroma. However, big-bubble DALK’s diffusion is limited because of its steep learning curve and surgical complexity [7] and up to now few papers have been published about big-bubble technique in children [8, 9].
Several parameters have to be considered in paediatric keratoplasty: [10] pre-operative evaluation, intraoperative problems such as low corneal and scleral rigidity, increased fibrin reaction, and positive vitreous pressure; the need of frequent examinations under general anaesthesia for postoperative follow-up evaluations; frequent loosening of sutures necessitating replacement or early removal; increased risk of rejection and infections; the difficulties related to repeated refractive error assessments, and the management of amblyopia.
In a recent review of paediatric keratoplasty, Vanathi et al. [10] reported that poor prognostic indicators are concomitant infantile glaucoma and corneal vascularization, active inflammation or infection, combined procedures, and previous graft failure.
In this paper we review all paediatric procedures performed at the Bambino Gesù Children’s Hospital in Rome, Italy, over a period of 4 years, reporting indications and clinical outcomes. This is the first large series analysis in Italy on paediatric corneal keratoplasty.
Materials and methods
The clinical charts of fifty-four eyes of 43 patients (33 males and 10 females) who underwent corneal keratoplasty from 1 January 2010 through 31 December 2013 were retrospectively retrieved. For this data analysis formal consent is not required, whereas informed consent for the surgical procedure was obtained from all individual participants included in the study. All the operations were performed under general anaesthesia in the operating room. Mean follow-up period was 22.8 months (range 1–45 months).
Patients underwent PK or DALK as a function of pre-operative diagnosis. DALK with the big-bubble technique was performed in all cases in which corneal endothelium appeared healthy. PK was performed in all other cases of congenital, traumatic, or acquired non-traumatic diseases [11, 12]. Some patients were randomized to undergo PK (four eyes) and DALK (eight eyes) assisted by IntraLase 60 KHz femtosecond laser (IntraLase FS Laser, Abbott Medical Optics, Inc.) [13, 14]. Pre-operative diagnoses, recipient age, type of keratoplasty, and post-operative follow-up data [Visual Acuity (VA, Snellen feet), complications, and cause of graft failure] were recorded. Visual Acuity was defined as the best visual acuity measured at the last examination. In children with insufficient verbal or cognitive skills, the ability to fixate on and follow visual targets was recorded. Complications were defined as vascularization (any vessel ingrowth into the corneal transplant without distinction between the numbers of quadrants affected, superficial and deep vessels, or single and multiple vessel leashes), glaucoma (the intraocular pressure was considered abnormal if over 22 mmHg, recorded by applanation or air-puff tonometry), and inflammation (intraocular reaction with or without corneal infiltrates). Graft clarity was evaluated on slit lamp, and a clear graft was defined as a clear central stroma without epithelial or stromal oedema. Graft failure was defined as the irreversible loss of optical clarity with or without vascularized scarring, with onset date of corneal clouding selected as time point of graft failure. Survival time of failed grafts was defined as the time between the date of surgery and recorded date of failure.
Postoperative treatment regimen involved topical corticosteroid along with antibiotics and lubricants. Topical steroids were given more frequently in the initial postoperative period and gradually tapered and changed to weaker steroids such as fluoromethalone in 3–6 months.
Statistics
To assess the effect of age on graft failure rate, the recipient age was considered as a dichotomous variable (≤5 or >5 years) and a 2X2 table was developed, using the chi-square test for testing the statistical significance. The effect of preoperative disease and surgical technique on the graft failure rate was tested using the chi-square test and the same approach of analysis: first developing a contingency table with all the enrolled eyes put together, then conducting two subgroup analyses with patients of ≤5 years and those of >5 years analyzed separately. The preoperative diseases were grouped in three subgroups: congenital (including glaucoma and sclerocornea), acquired traumatic diseases (including previous failed surgery and penetrating trauma) and acquired non-traumatic diseases (including keratoconus and all the other conditions). To evaluate the survival time of failed grafts, the Kaplan-Meier estimate for PK and DALK groups was plotted. The level of statistical significance was set at p < 0.05, and all statistical analyses were performed with SPSS ver 21.0 (SPSS inc., Chicago, IL.).
Results
Pre-operative diagnosis
Table 1 shows the pre-operative diagnoses, Table 2 the distribution of the preoperative diseases by age group and table 3 the distribution of preoperative disease condition and its effect on graft failure for the whole sample and by age groups (≤5 years or > 5 years). Twenty eyes (37 %) were affected by keratoconus, 11 (20 %) by congenital glaucoma with corneal decompensation, six (11 %) by secondary leukoma, four (7 %) by corneal opacity following penetrating trauma, two (4 %) by secondary ulcer with tectonic indication, two (4 %) by secondary glaucoma with corneal decompensation, and one (2 %) each, respectively, by sclerocornea, secondary limbus stem deficit with corneal scars, limbal dermoid and blood cornea adsorption after vitrectomy. Five eyes (9 %) underwent keratoplasty after a previous failed surgery. Therefore, more than half of keratoplasty (57 %) was due to keratoconus (37 %) or congenital glaucoma (20 %).
Vascularization was preoperatively observed in 17 patients (31 %): 14 (82 %) affected by congenital glaucoma, two (12 %) by ulcer and one (6 %) by leukoma. Thirteen patients were affected by glaucoma and under topical treatment.
Recipient age
Mean age of patients was 8.9 ± 5.7 [SD] years (range, 1 to 17 years). Mean age of patients treated with PK and DALK was respectively 6.9 ± 5.2 and 11.8 ± 5.0 years.
Table 1 reports mean recipient age by pre-operative diagnosis. All patients affected by keratoconus were over eight years of age, whereas within the group of eighteen patients with ≤5 years, ten were affected by congenital glaucoma.
Type of keratoplasty
Thirty-two eyes (60 %) underwent PK, while 22 (40 %) underwent DALK. In general, PK was performed on younger children, while DALK on older patients mainly for keratoconus (82 %) (table 1).
Regrafts
Five eyes (9 %) underwent keratoplasty after previous failed surgery. The initial diagnosis was congenital glaucoma in three eyes (60 %), keratitis and penetrating trauma, respectively, in one eye (20 %). One of the three eyes affected by congenital glaucoma had already been grafted twice; therefore, only one patient showed an acquired non-traumatic disease.
Post-operative follow-up
At the final follow-up examination, visual acuity could be recorded in 57 % of eyes (31 of 54 eyes); in 52 % of these, VA was measured by means of the ability to fixate on and follow visual targets. In residual 43 % VA could not be measurable due to young age and/or insufficient cognitive skills of patients.
Of all those patients whose VA could be measured with a minimal follow-up of 18 months (with at least 8 months after complete suture removal), 12 had undergone big-bubble DALK (mean VA 20/25) and three had undergone PK (mean VA 20/50). The PK group of patients with recordable vision was reduced because of the younger mean age of patients treated with this procedure. Consequently, in these patients amblyopia mainly affected VA recovery.
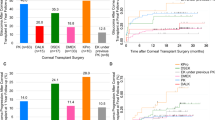
Graft failure was recorded in 59 % of PK and 27 % of DALK eyes (19 and six, respectively) occurring in the first two post-operative years.
One patient presented the Urrets Zavalia syndrome one day after big-bubble DALK.
One patient showed a 3 day post-operative traumatic massive intraocular bleeding.
No active inflammation was observed.
The most common cause of failure was endothelial rejection with corneal swelling and marked corneal thickness increase. Graft failure occurred in fifteen of seventeen eyes with preoperative recipient bed vascularization.
At the last follow-up clear grafts were observed respectively in 16 DALK (73 %) and 13 PK (41 %) patients.
The present study did not analyze separately the outcomes achieved using mechanical trephine or femtosecond laser, but it is limited to the analysis of clinical outcomes as a function of the surgical technique performed (PK or DALK).
Effect of age, surgical procedure and preoperative diseases on graft failure
When considering the effect of recipient age on the graft failure rate of the whole sample, patients with ≤5 years, showed a higher percentage of failure than older ones (p = 0.0008) (Table 4).
When considering the effect of surgical technique on the graft failure rate of the whole sample, eyes that underwent DALK procedure have shown a statistically significant lower rate of graft failure than the PK eyes (p = 0.02) (Table 4).
However, when subgroup analysis was conducted separately for patients of ≤5 and of >5 years, despite the DALK group showing lower rate of graft failure in both age groups (50 vs 82 % and 22 vs 39 %), no statistically significant differences emerged between DALK and PK (p = 0.15 for ≤5 years group and p = 0.27 for >5 years group, respectively) (Table 4).
In Table 3, the effect of preoperative disease on the graft failure rate is reported. Congenital disease, mainly glaucoma (ten out of 12 eyes) have shown higher rate of graft failure, followed by acquired traumatic disease and acquired non-traumatic disease (mainly keratoconus), which have shown the lower rate of failure. A statistically significant effect of the preoperative diseases has been noted only when considering the whole sample and the eyes of patients older than 5 years. Preoperative disease condition seemed not influence the failure rate of eyes younger than or equal to 5 years.
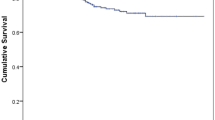
The Kaplan-Meier plot of the survival rates is displayed in Fig. 1. DALK eyes have shown a longer survival time than PK eyes (588 vs 406 mean days), and the difference has been statistically significant (Wilcoxon test: p = 0.0255).
Kaplan- Meier survival curve of corneal grafts failure in function on the surgical technique shows significant differences between deep anterior lamellar keratoplasty (DALK) and penetrating keratoplasty (PK) (Wilcoxon test: p = 0.0255). The mean survival time of the grafts were 588.455 days for eyes that underwent DALK and 406.594 days for eyes that underwent PK (p = 0.02, log-rank test)
Discussion
Indications for paediatric keratoplasty differ worldwide according to the diverse corneal disease [15]. Congenital corneal opacity and corneal dystrophies appear in developed countries with the major indications for paediatric PK, [16] actually the “gold standard” in paediatric keratoplasty. However, the graft survival is approximately 50–60 %, [2, 3] mainly because of endothelial rejection due to the high immunologic response of paediatric patients [4].
Here, we report indications and clinical outcomes of a consecutive series of paediatric keratoplasty performed over 4 years at the Bambino Gesù Children’s Hospital in Rome, Italy. These data collect more than 80 % of all Italian paediatric keratoplasties performed in this period (unpublished data) and, up to now, this is the first Italian report about paediatric keratoplasty outcomes.
Recent advances in surgical technique and post-operative management have moderately improved PK results, [3] allowing keratoplasty even in very young patients [10]. Early grafting can be necessary to prevent deep amblyopia in case of corneal dense opacity, despite poor outcomes, and is generally associated with the youngest age [10, 17].
Considering the high rate of intra-operative complications [7] and the limited number of paediatric keratoplasty performed in eyes with healthy endothelium, to date only small case series of paediatric big-bubble DALK have been reported [8, 9, 14].
Several authors reported clinical outcomes in paediatric PK or DALK, [2–4, 8–10, 14, 15, 17] but few papers simultaneously analysed and compared the two procedures.
Our data show that the majority of patients were affected by acquired non-traumatic diseases (59 %), mainly by keratoconus. In accordance with other authors [2, 10], we observed the best graft survival in acquired non-traumatic diseases where amblyopia, however, limited the visual outcome [18], whereas the worst prognosis appears related to congenital diseases, mainly congenital glaucoma, although a comparison among different studies in the literature appears difficult due to the high heterogeneity of samples and follow-up, typical of paediatric populations. In our study patients younger than 5 years show worse outcome. This difference may partially depend on the pre-operative corneal conditions.
Congenital glaucoma in PK and pre-operative vascularization both in PK and DALK seem to represent the main pre-operative risk factors for keratoplasty failure. This finding is consistent with those reported in other studies [10, 15, 17]. New therapeutic approaches concerning pre- and post-operative corneal blood vessels treatment [19, 20] could improve clinical outcomes.
Trauma represents a specific childhood-correlated postoperative risk factor after keratoplasty. Younger patients can be more exposed to traumatic accidents with consequent wound dehiscence or intraocular bleeding. Lamellar keratoplasty presents more resistance against wound dehiscence than penetrating keratoplasty, and it is recommended for such patients [21].
The best age to perform the surgery is still a matter open to discussion. In some studies, the age of patients at the time of surgery significantly influenced the graft survival [4, 22], whereas in others this correlation was not statistically significant [3, 17].
In our study, when we grouped patients by age, children older than 5 years have shown a statistically significant better graft outcome than younger ones. Similarly, Aasuri et al. [4], Hong et al. [22] and Lowe et al. [23] have shown a worse graft survival for children younger than 5 years. A more active immune system has long been suggested as the main reason for the increased rate of rejection observed in younger recipients [24]. Recently Scwartzkopff et al. [25] reported an animal model of keratoplasty that mimics the faster graft failure in children. They observed that CD161 + NK/NKT cells may be key players in corneal graft rejection in young patients, although additional developmental disorders generally represent poor prognostic
factors, suggesting an involvement of the innate immune system in this process [22]. Our findings confirm the main role of immunology in the higher graft failure rate observed in children since a preoperative disease condition seems not influence the failure rate of eyes younger than or equal to 5 years.
Then, in our opinion, the surgeons should always consider the risk-benefit profile of paediatric corneal transplantation before proceeding.
However, considering how the recipient age has affected the graft failure rate in our sample, it must be noted that patients younger than 5 years old were affected by congenital glaucoma or acquired diseases (different from keratoconus), whereas children older than 5 were mainly affected by keratoconus. The different prevalence of keratoconus, which usually provides better surgical results, could have introduced a selection bias, and overestimated the favorable outcome in younger patients.
In order to explore whether DALK procedure can provide advantages over PK surgery, we first analyzed the differences in the whole sample and then in two subgroups of patients of ≤5 and >5 years of age, respectively. DALK procedure have shown a better graft failure outcome in the first comparison but in both subgroup analyses no statistically significant differences were found between PK and DALK; nevertheless, in both subgroups the percentage of graft failure was reduced in patients treated with DALK procedure.
In the analysis involving younger patients (≤5 years) the DALK group included only four cases, and this could have reduced the power of the statistical analysis, whereas in the >5 year subgroup the cases treated were 18 for PK and DALK with more comparable pre-operative clinical corneal conditions. Our data, therefore, suggest that DALK could also improve clinical outcomes and decrease the graft failure percentage [5] in child populations. However, the extensive corneal involvement, mainly observed in congenital diseases, does not recommend DALK as the usual “first surgical option” in paediatric keratoplasty to prevent deprivation deep amblyopia.
We decided to statistically evaluate the effect of age and surgery technique on graft failure, despite the analysis presenting some limitations and, consequently, suggesting a cautious interpretation of the results. Specifically, the diseases included in the compared groups were different and, thus, greater homogeneity of the pre-operative conditions should be required to obtain reliable results less affected by selection bias. Such limitations and the relatively brief follow-up, however, are the same limits of other similar studies due to the special features of paediatric patients [2, 3, 9].
In conclusion, our paper presents a large series of paediatric keratoplasties and might suggest the need for multicentre studies to improve surgical strategy, better management of risk factors to improve graft survival, and specific visual rehabilitation pathways to improve visual outcomes.
References
Colby K (2008) Changing times for pediatric keratoplasty. J AAPOS 12:223–224
Hovlykke M, Hjortdal J, Ehlers N, Nielsen K (2013) Clinical results of 40 years of pediatric keratoplasty in a single university eye clinic. Acta Ophthalmol. doi:10.1111/aos.12198x
Huang C, O’Hara M, Mannis MJ (2009) Primary pediatric keratoplasty: indications and outcomes. Cornea 28:1003–1008
Aasuri MK, Garg P, Gokhle N, Gupta S (2000) Penetrating keratoplasty in children. Cornea 19:140–144
Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM (2011) Deep Anterior lamellar keratoplasty as an alternative to penetrating keratoplasty. Ophthalmology 118:209–218
Anwar M, Teichmann KD (2002) Big-bubble technique to bare Descemet’s membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 28:398–403
Han DC, Mehta JS, Por YM, Htoon HM, Tan DTH (2009) Comparison of outcomes of lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol 148:744–751
Harding SA, Nishal KK, Upponi-Patil A, Fowler DJ (2010) Indications and outcomes of deep anterior lamellar keratoplasty in children. Ophthalmology 117:2191–2195
Ashar JN, Pahuja S, Ramappa M, Vaddavalli PK, Chaurasia S, Garg P (2013) Deep anterior lamellar keratoplasty in children. Am J Ophthalmol 155:570–574
Vanathi M, Panda A, Vengayil S, Chaudhuri Z, Dada T (2009) Pediatric keratoplasty. Surv Ophthalmol 54:245–271
Stulting RD (1993) Penetrating keratoplasty in children. In: Brightbill FS (ed) Corneal surgery: theory, technique and tissue, 2nd edn. Mosby, St Louis, pp 374–385
Stulting RD, Sumers KD, Cavanagh HD (1984) Penetrating keratoplasty in children. Ophthalmology 91:1222–1230
Farid M, Pirouzian A, Steinert RF (2013) Femtosecond laser keratoplasty. Int Ophthalmol Clin 53:55–54
Buzzonetti L, Petrocelli G, Valente P (2012) Big-bubble deep anterior lamellar keratoplasty assisted by femtosecond laser in children. Cornea 31:1083–1086
Rong Low J, Anshu A, Tan ACS, Htoon HM, Tan DTH (2014) The outcomes of primary pediatric keratoplasty in Singapore. Am J Ophthalmol 158:496–502
Limaiem R, Chebil A, Baba A, Ben Youssef N, Mghaieth F, Ei ML (2011) Pediatric penetrating Keratoplasty: indications and outcomes. Transplant Proc 43:649–651
Al-Ghamdi A, Al-Rajhi A, Wagoner MD (2007) Primary pediatric keratoplasty: indications, graft survival, and visual outcome. J AAPOS 11:41–47
Ganekal S, Gangangouda C, Dorairaj S, Jhanji V (2011) Early outcomes of primary pediatric keratoplasty in patients with acquired, atraumatic corneal pathology. J AAPOS 15:353–355
Koenig Y, Bock F, Kruse FE, Stock K, Cursiefen C (2012) Angiogressiove pretreatment of mature corneal blood vessels before keratoplasty: fine needle vessel coagulation combined with anti VEGFs. Cornea 8:887–892
Papathanassiou M, Theodoropoulou S, Analitis A, Tzonou A, Theodossiadis PG (2013) Vascular endothelial growth factor inhibitors for treatment of corneal neovascularization: a meta-analysis. Cornea 4:435–444
Foroutan AR, Gheibi GH, Joshaghani M, Ahadian A, Foroutan P (2009) Traumatic wound dehiscence and lens extrusion after penetrating keratoplasty. Cornea 28:1097–1099
Hong JX, Xu JJ, Sheng MJ, Liu Y, Zhu L (2008) Pediatric penetrating keratoplasty in Shanghai: a retrospective multiple centre study from 2003 to 2007. Chin Med J (Engl) 121:1911–1914
Lowe MT, Keane MC, Coster DJ, Williams KA (2011) The outcome of corneal transplantation in infants, children, and adolescents. Ophthalmology 118:492–497
Alldredge OC, Krachmer JH (1981) Clinical types of corneal transplant rejection. their manifestations, frequency, preoperative correlates, and treatment. Arch Ophthalmol 99:599–604
Scwartzkopff J, Berger M, Bimbaum F, Bohringer D, Reinhard T (2009) Accelerated corneal graft rejection in baby rats. Br J Ophthalmol 94:1062e–1066e
Acknowledgments
The authors have no financial or proprietary interests in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The following sentence: “For this data analysis formal consent is not required, whereas informed consent for the surgical procedure was obtained from all individual participants included in the study” has been added.
Rights and permissions
About this article
Cite this article
Buzzonetti, L., Ardia, R., Petroni, S. et al. Four years of corneal keratoplasty in Italian paediatric patients: indications and clinical outcomes. Graefes Arch Clin Exp Ophthalmol 254, 2239–2245 (2016). https://doi.org/10.1007/s00417-016-3447-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3447-2