Abstract
Purpose
To determine the amount and characteristics of dynamic torsional misalignment of eyes during excimer ablation in laser in-situ keratomileusis (LASIK).
Methods
Retrospective trial for evaluation of dynamic intraoperative torsional misalignment of 179 eyes that underwent LASIK for correction of myopia and/or astigmatism. Patients were treated with the Keracor 217z excimer laser implementing 25 Hz dynamic eye tracker ACE 100 (both Technolas Perfect Vision, Munich, Germany). From dynamic torsional misalignments, temporal power spectra were obtained by Fourier analysis up to a frequency of 12.5 Hz and an amplitude of ±15° from initial torsional status (limited by the tracking system). The f90, f95, and f99 criteria were defined as the frequency below which 90 %, 95 %, and 99 % of misalignments occur. A Wilcoxon rank sum test was performed to detect differences of f90, f95, and f99 in groups’ gender, age, and eye (if both eyes underwent surgery at same day). Multiple regression analysis (MRA) was performed to evaluate possible preoperative predictors of f90, f95, and f99.
Results
Fourier analysis showed a dominance of high-frequency, low-power dynamic torsional misalignment. Mean f95 threshold of rotational movements was 4.89±2.12 Hz (median 4.54, ranging from 0.44 to 9.23 Hz). Wilcoxon rank sum test showed no differences in f90, f95, and f99 between groups' gender, age, and eye. MRA revealed age, gender, and optical zone as preoperative predictors on intraoperative f90, f95, and f99.
Conclusions
Dynamic intraoperative torsional misalignments of eyes undergoing LASIK are dominated by low-frequency (slow), high-power (large) movements, with 95 % being slower than 4.89Hz regarding the spectrum analyzed (0–12.5Hz, ±15°). Movements can be predicted preoperatively by eye treated, patients’ gender, and age in pre-LASIK diagnostics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Decentration of ablation patterns in laser refractive surgery caused by differences in the eye position between time of diagnostics, laser alignment, and laser ablation may account for inducing aberrations or postoperative over- and undercorrection to a certain degree [1]. Relevant eye movements that may lead to decentration or misalignment are, on the one hand, fixational movements such as tremor and micro-saccades or slow and large eye drifts [2, 3]. On the other hand, several investigators also confirm the occurrence of static preoperative torsional misalignment induced by shifting the patient from seated to supine position, monocular occlusion or head roll [4–8]. As head movements also have an influence on the eye’s position during laser refractive surgery, the current eye tracking systems available in refractive lasers systems do not solely analyze eye movements, but misalignments in general, which also includes head-movement induced misalignments.
The occurrence of dynamic intraoperative torsional misalignment has been proven [9–11]. The influence of static preoperative and dynamic intraoperative lateral decentration on visual outcome has been described before [1]. Different publications focus on the description of static and dynamic torsional misalignment [5–7, 12], its negative influence on astigmatism correction or higher-order aberrations [11, 13, 14], or confirm the visual benefit gained by its compensation. [11, 13, 15, 16] However, those trials did not look at the dynamic characteristics of the torsional misalignment occurring during laser refractive surgery; instead, they evaluated the maximum, minimum, and mean values only.
The aim of this trial was to determine the amount and characteristics of dynamic torsional misalignment using a large patient cohort and a commercially-available iris-recognition-enabled dynamic eye tracker. Temporal power spectra as described by Porter et al. (2005) [12] were calculated to define a threshold frequency below which the majority of dynamic torsional misalignments occur. Using this frequency as a dependent variable, a multiple regression analysis was performed to evaluate predictors of intraoperative dynamic torsional misalignment. Possible predictors including (1) manifest sphere, cylinder, and spherical equivalent, (2) age, (3) optical zone size, and ablation depth were evaluated. Furthermore, differences of f95 in the groups’ eye and gender were analyzed, using a Wilcoxon rank sum test. The overall significance threshold for these analyses was p = 0.05.
Material and methods
This retrospective evaluation of clinical data includes 179 eyes (for patient data see Table 1) which were treated for myopia or myopic astigmatism with LASIK using a femtosecond laser for flap creation (Intralase FS60, Abbot Medical Optics, Santa Anna, CA, USA) including dynamic torsional misalignment tracking during excimer ablation, using the ACE 100 eyetracker implemented in the Keracor 217z excimer laser system (both Technolas Perfect Vision, Munich, Germany). Lateral tracking was always activated. All treatments were aimed at the correction of myopia or myopic astigmatism. All patients signed written consent for the applied treatment. Ethics committee approval was not needed due to the retrospective character of the trial. For all treatments, the suitability for treatment with LASIK according to the safety and quality standards of the German Commission of Refractive Surgery (KRC) was required [17]. In detail, the inclusion criteria were: myopia ≤10.0 D in the steepest meridian, astigmatism ≤5.0 D, residual stromal thickness ≥250 μm, and an age of ≥18 years. A further inclusion criterion for this trial was successful dynamic torsional misalignment tracking for 100 % of ablation. Exclusion criteria were: preoperative corneal thickness ≤500 μm, progressive corneal diseases, forme fruste keratoconus, cataract, glaucoma, or macular degeneration. No additional measurements were performed in addition to the common femtosecond-LASIK practice of our institution. All laser refractive procedures were performed by the same surgeon (TK). Right eyes were always treated prior to the left eye; both eyes underwent surgery on the same day within approximately 20 minutes.
Tracking of dynamic torsional misalignment
The resolution dimension of dynamic torsional misalignment measurement is 0.1° within a range of ±15° from the initial torsional status of the eye at the beginning of the tracking procedure (according to the manufacturer). The dynamic torsional misalignment tracking system works with a repetition rate of 25 Hz, the laser itself with 100 Hz. Thus, approximately every fourth laser spot is aligned by the eye tracker and was used for the analysis of movements. The analysis of the torsional movements of the laser with 25 Hz indirectly reflects the dynamic torsional misalignments.
Using a custom-written MATLAB program (MATLAB 7.0; The MathWorks Inc., Natick, MA, USA), the temporal power spectra of dynamic torsional misalignment were calculated by the laser movements to determine the frequency below which the majority of rotational eye movements occurred. The temporal power spectrum is a simple way to quantify the size of eye movements as a function of frequency, as previously described by Porter et al. (2005) [12]. Fourier analysis was performed respecting the Nyquist–Shannon sampling theorem, thus only frequencies up to 25Hz/2=12.5Hz were analyzed [18]. Fast dynamic torsional misalignments are represented by high temporal frequencies, slow dynamic torsional misalignments by low temporal frequencies. Small-amplitude movements have a low power and large-amplitude movements a larger power, respectively [12]. In this trial, a 95 % threshold was chosen as a criterion (f95) to define the majority of eye movements.
Statistics
The Shapiro–Wilk test was performed to detect parametric distribution of f90, f95, and f99 in the study population. The Wilcoxon rank sum test was performed to detect significant differences between groups, as data were nonparametric. Male versus female, patients older than median versus patients younger than median (35 years), and eyes treated first versus eyes treated second if both procedures were performed at same day. Finally, the influence of factors shots, spherical equivalent, age, gender, optical zone size and ablation depth of f90, f95, and f99 were evaluated using a multiple regression analysis. This was possible despite the nonparametric distribution of the variables because for linear regression only normality for error terms is necessary and this was met. An overall significance level of p = 0.05 was chosen. All statistic analyses were performed with SPSS 13.0 software. (SSPS Inc, Chicago, IL, USA)
Results
Analysis of dynamic torsional misalignment
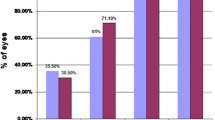
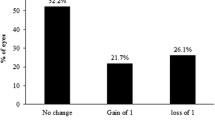
Figures 1 and 2 show exemplary results of the same patient’s right and left eye. This patient displayed large inter-eye differences. At first, the total amount of misalignment was larger in the left eye than in the right eye (Fig. 1a,b). Since this systematic difference has no influence on the analysis of dynamic torsional misalignment characteristics it could be omitted. The second effect was a difference in power of dynamic torsional misalignment. The reason for this difference remains unclear; increasing nervousness or restlessness of the patient might lead to the increasing ration of dynamic torsional misalignment. The left (second treated) eye shows more high-power movements (Fig. 1a,b, Fig. 2a,b). The low-power movements superimposing the high-power movements (Fig. 1a,b) are similar in both eyes (Fig. 2a,b). Analysis of the relationship between power and frequency of torsion with Fourier analysis (Fig. 2a,b) shows that the amplitude of torsion decreases with increasing frequency. The cumulative power spectrum (Fig. 2c,d) represents the cumulative percentage of torsional frequencies. In the patient’s left eye, low-frequency and thus high-power movements take a larger percentage of all dynamic torsional movements than in the right eye, where the high-frequency and thus low-power movements dominate. The cumulative percentage increases much faster in the left eye compared to the right eye. The graph of the Fourier analyses for the entire series (Fig. 3a) shows that the amplitude of dynamic torsional movements decreases with increasing frequency. Additionally, a second smaller peak in movement amplitudes occurs for high frequencies. We have no coherent explanation for this peak. It might reflect an actual increase in amplitude for small-frequency movements. It might also be an artefact of the analysis method. The median f95 criterion was 4.54, ranging from 0.44 to 9.23 Hz. The mean f95 criteria was 4.89°±2.12Hz.
Analysis of prediction of f90, f95, and f99
Shapiro–Wilk testing indicated nonparametric distribution of f90, f95, and f99 (Table 1). The Wilcoxon rank sum test indicated no differences of f90, f95, and f99 between groups formed by gender, age, and eye (Table 2).
Regression analysis for determination of possible influencing variables on f90, f95, and f99 included: ablation depth, age, optical zone size, gender, shots, and spherical equivalent (Table 3). Although R-squared was relatively low in MRA of f90, f95, and f99, a significant impact on all of them was shown by age, gender, and optical zone, with female gender, higher age, and increase in optical zone promoting an increase in f90, f95, and f99 (Table 4).
Discussion
Our trial aims to describe the characteristics of dynamic cyclotorsional misalignment during LASIK beyond the often used maximum torsion or mean torsion values, as these can only describe worst case or mean misalignment. In particular, the use of maxima leads to an overestimation of the impact of these misalignments on postoperative results.
Fourier analysis offers a way to split these dynamic torsional misalignments into single components, frequency and amplitude, which can be a further option for calculating their impact on ablation precision more precisely. Our analysis shows that slow but large torsional misalignments (high amplitude, low frequency) dominate the dynamic torsional error. These errors are potentially of bigger influence on ablation precision than are fast and small (low-amplitude and high-frequency) movements. Large and fast torsional misalignments did not occur within the range of analyzed frequency.
The magnitude of static torsional misalignment, as well as its influence on postoperative vision, has been described before and was thus not the topic of this paper. [4–8, 16, 19]
To describe the impact of dynamic torsional eye movements on ablation precision during refractive corneal excimer surgery, such as photorefractive keratectomy or laser in-situ keratomileusis (LASIK), the knowledge of two factors is required. First, the torsional position of the eye at any moment during ablation. Second, the exact intended position of the laser spot at each moment. By combining these two factors, the impact of dynamic torsional misalignment of ablation precision can be calculated. This paper focuses on the basics of the first parameter, as it describes the characteristics of dynamic torsional misalignment during LASIK in a real patient cohort. Fourier analysis is used to decompose the dynamic process to its basic components: amplitude and frequency.
Age, gender, and optical zone had a significant impact on f90, f95, and f99. An increase in optical zone has the highest impact on f90, f95, and f99 and promotes their increase significantly. Similarly, female gender and higher age promote increase of f90, f95, and f99 significantly. Therefore, these variables can be considered as predictors in contrast to shots and spherical equivalent.
Our findings can help producers of eye-tracking systems to further adjust their systems in order to compensate for patients’ eye movements. Furthermore, we think it is critical to discuss with patients that misalignment was higher in the second treated eye when getting informed consent.
Voluntary fixation leads to a reduction of microsaccades from an average of 85 Hz [20] to frequencies as low as 0.5 Hz [21]. In LASIK, patients are asked to voluntarily fixate as well, so the mean torsional misalignment of about 2–3° described by most authors seems to appear to be a reasonable range. In accordance with these findings, we did show that 95 % of all dynamic torsional misalignments during LASIK were slower than 4.89° ± 2.12Hz. Significantly faster dynamic torsional misalignments are also, according to the frequency trend shown in Fig. 3a, not to be expected. The faster the torsional misalignments get, the smaller they get. Due to the limits of the tracking system, however, faster and at the same time much larger torsional misalignments cannot be excluded completely.
References
Mrochen M, Eldine MS, Kaemmerer M, Seiler T, Hütz W (2001) Improvement in photorefractive corneal laser surgery results using an active eye-tracking system. J Cataract Refract Surg 27:1000–1006
Rolfs M (2009) Microsaccades: small steps on a long way. Vision Res 49:2415–2441
Ditchburn RW, Foley-Fisher JA (1967) Assembled data in eye movements. Opt Acta 14:113–118
Park SH, Kim M, Joo C-K (2009) Measurement of pupil centroid shift and cyclotorsional displacement using iris registration. Ophthalmologica 223:166–171
Chernyak DA (2004) Cyclotorsional eye motion occurring between wavefront measurement and refractive surgery. J Cataract Refract Surg 30:633–638
Ciccio AE, Durrie DS, Stahl JE, Schwendeman F (2005) Ocular cyclotorsion during customized laser ablation. J Refract Surg 21:S772–S774
Swami AU, Steinert RF, Osborne WE, White AA (2002) Rotational malposition during laser in situ keratomileusis. Am J Ophthalmol 133:561–562
Kohnen T, Kühne C, Cichocki M, Strenger A (2007) Cyclorotation of the eye in wavefront-guided LASIK using a static eyetracker with iris recognition. Ophthalmologe 104:60–65
Chang J (2008) Cyclotorsion during laser in situ keratomileusis. J Cataract Refract Surg 34:1720–1726
Febbraro J-L, Koch DD, Khan HN, Saad A, Gatinel D (2010) Detection of static cyclotorsion and compensation for dynamic cyclotorsion in laser in situ keratomileusis. J Cataract Refract Surg 36:1718–1723
Waring GO (2009) One-kilohertz eye tracker and active intraoperative torsion detection in the NIDEK CXIII and Quest excimer lasers. J Refract Surg 25:S931–S933
Porter J, Yoon G, MacRae S, Pan G, Twietmeyer T, Cox IG, Williams DR (2005) Surgeon offsets and dynamic eye movements in laser refractive surgery. J Cataract Refract Surg 31:2058–2066
Wang L, Koch DD (2008) Residual higher-order aberrations caused by clinically measured cyclotorsional misalignment or decentration during wavefront-guided excimer laser corneal ablation. J Cataract Refract Surg 34:2057–2062
Tjon-Fo-Sang MJ, de Faber J-THN, Kingma C, Beekhuis WH (2002) Cyclotorsion: a possible cause of residual astigmatism in refractive surgery. J Cataract Refract Surg 28:599–602
Arba-Mosquera S, Merayo-Lloves J, de Ortueta D (2008) Clinical effects of pure cyclotorsional errors during refractive surgery. Invest Ophthalmol Vis Sci 49:4828–4836
Ghosh S, Couper TA, Lamoureux E, Jhanji V, Taylor HR, Vajpayee RB (2008) Evaluation of iris recognition system for wavefront-guided laser in situ keratomileusis for myopic astigmatism. J Cataract Refract Surg 34:215–221
Kohnen T, Knorz MC, Neuhann T, German Ophthalmological Society, Professional Association of German Ophthalmologists (2007) Evaluation and quality assurance of refractive surgery procedures by the German Ophthalmological Society and the Professional Association of German Ophthalmologists. Ophthalmologe 104:719–726
Shannon CE (1949) Communication in the presence of noise. Proc IRE 37:10–21
Kim H, Joo C-K (2008) Ocular cyclotorsion according to body position and flap creation before laser in situ keratomileusis. J Cataract Refract Surg 34:557–561
Bolger C, Bojanic S, Sheahan NF, Coakley D, Malone JF (1999) Dominant frequency content of ocular microtremor from normal subjects. Vision Res 39:1911–1915
Steinman RM, Cunitz RJ, Timberlake GT, Herman M (1967) Voluntary control of microsaccades during maintained monocular fixation. Science 155:1577–1579
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
Financial Disclosure
MS and JB: None. TK: Consultant for Abbott, Alcon, Carl Zeiss, Geuder, Oculus, Rayner, Schwind, TearLab, Thieme Compliance and Ziemer; receives a research grant from Abbott, Alcon, Carl Zeiss, Rayner, Oculus and Schwind.
Rights and permissions
About this article
Cite this article
Shajari, M., Bühren, J. & Kohnen, T. Dynamic torsional misalignment of eyes during laser in-situ keratomileusis. Graefes Arch Clin Exp Ophthalmol 254, 911–916 (2016). https://doi.org/10.1007/s00417-016-3309-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3309-y