Abstract
Introduction
Characteristics of ophthalmia neonatorum (ON) amongst paediatric ophthalmologists remain unclear. The purpose of this current study is to examine the incidence, diagnosis, treatment, and prophylaxis of ON cases presenting to members of the American Association of Paediatric Ophthalmology and Strabismus (AAPOS).
Methods
An email containing a web link to a survey was sent to all members of AAPOS. The questionnaire examined the incidence of ON, etiology, diagnostic methods, treatment, and prophylaxis of the disease in different countries around the world.
Results
Two hundred and ninety-one ophthalmologists answered the questionnaire. Most were from North America (52.94 %). One hundred and seventy-six (60.69 %) ophthalmologists encountered 0–5 cases of ON per year. The most common pathogens causing ON was Chlamydia trachomatis (35.37 %). Two hundred and forty-two (85.21 %) treat empirically when encountering ON during the first 10 days of life and 205 (75.09 %) after the first 10 days of life. In both cases, erythromycin was the most common first line of treatment. Two hundred and twenty-two (78.72 %) ophthalmologists replied that prophylactic treatment is required in their country. The most common agent for prophylaxis was erythromycin ointment (71.50 %).
Conclusions
We found that the incidence of ON per year per practitioner is 0–5 cases, the most common etiology is C. trachomatis, and most infants receive prophylaxis and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ophthalmia neonatorum (ON), also known as neonatal conjunctivitis, is defined as an acute, mucopurulent conjunctivitis, which presents in the first 4 weeks of life [1]. The incidence of the disease ranges between 1.6 and 12 % in different studies and geographical locations [2, 3]. Presentation may vary from eyelid swelling and conjunctival hyperemia to chemosis, serous, or purulent discharge [2, 3].
Prior to 1880, ON was the primary cause of neonatal blindness (60–73 %), and the term ON was used only for cases of conjunctivitis due to Neisseria gonorrhoeae (N. gonorrhoeae) [4]. In 1881, Credé introduced ocular prophylaxis for ON which consisted of instilling a drop of 2 % silver nitrate solution into each eye at birth. [5] This simple treatment resulted in a dramatic reduction in the incidence of ON due to N. gonorrhoeae from 10 to 0.3 % [5].
ON can also be caused by bacterial infections (Chlamydia trachomatis, N. gonorrhoeae, Haemophilus species, Streptococcus pneumonia, etc.), viral infections (adenovirus or herpes simplex virus), or chemical substances (following treatment with silver nitrate prophylaxis or secondary to prophylaxis with other agents such as erythromycin or tetracycline) [6–8]. While chemical conjunctivitis usually presents within the first 24 h and is a self-limiting condition [9] bacterial and viral conjunctivitis occur later and require treatment [7].
For most non-sexually transmitted bacterial conjunctivitis, the treatment includes different topical antibiotics according to physician preference. In cases of ON caused by Chlamydia trachomatis (C. trachomatis) and N. gonorrhoeae, the treatment includes topical and systemic antibiotics [2, 3, 10]. Treatment for conjunctivitis caused by herpes simplex includes systemic acyclovir in addition to topical anti-viral ophthalmic solution [11].
Over the years, prophylaxis and treatment for sexually transmitted bacterial conjunctivitis evolved to include different antibiotics. Most women in the developed world are screened for C. trachomatis and N. gonorrhoeae towards the end of pregnancy, and, if infected, appropriate treatment is initiated prior to delivery.
Prophylaxis for infants at risk of developing ON is accomplished by a wide range of agents including topical tetracycline ointment 1 %, erythromycin ointment 0.5 %, povidone iodone solution 2.5 %, aminoglycosides, macrolids, fluroquinolone, chloramphenicol, or fucidic acid. The use of silver nitrate 1 % in neonates was discontinued due to the chemical conjunctivitis associated with this preparation [10]. Moreover, the agent is no longer manufactured.
The purpose of this study was to establish the worldwide incidence of ON and current opinion on appropriate ON diagnosis, treatment, and prophylaxis amongst pediatric ophthalmologists who are members of the American Association of Paediatric Ophthalmology and Strabismus (AAPOS).
Methods
Survey population and questionnaire
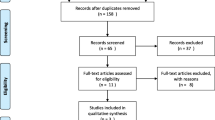
Email correspondence to all members of AAPOS was sent though International Peaditric Ophthalmology and Strabismus Council (IPOSC) secretariat, between February and April 2015. The email included a web link to a survey (created on www.surveymonkey.com), explanation for the purpose of the study, and a contact email and phone number that allowed the respondents to seek further clarification if needed. Follow-up emails were sent on several occasions in April 2015 to those who had not yet responded. The questionnaire included 20 questions (Supplementary Methods), which examined the incidence of ON, etiology, diagnostic methods, treatment, and prophylaxis of the disease in different countries around the world.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest.
As a retrospective study, formal consent is not required.
Statistical analysis
Statistical analysis, including distribution, was performed with JMP Statistical Discovery Software 7.0 (SAS Institute, Cary, NC, USA). The overall significance level was set to an alpha of 0.05.
Results
Two hundred and ninety-one ophthalmologists (out of 449 ophthalmologists) who were members of AAPOS answered the questionnaire. Forty-six (15.8 %) had practiced pediatric ophthalmology for less than 5 years, 48 (16.49 %) for 5-10 years, and 197 (67.70 %) for over 10 years.
The distribution of regions practicing ophthalmology around the world are summarised in Fig. 1.
Incidence and etiology
One hundred and seventy-six (60.69 %) ophthalmologists encountered 0–5 cases of ON per year, 43 (14.83 %) ophthalmologists did not encounter even one case of ON per year. The distribution of answers for those replied was No observed cases of ON: North America-36, Europe-1, Africa-1, Far East-2, Central America-1, and Middle East-1; 0-5 cases of ON per year: North America-103, South America-9, Central America-1, Central Asia-5, Far East-1, Africa-4, Middle East-15, Australia-4, Europe-34; 15–20: Far East-1, Central Asia-2, Europe-1, Middle East-2, and South America-1; More than 20: Central Asia-1, Europe-5, Far East-1, Middle East-4. Some did not specify where they practice.
The most common pathogens causing ON were C. trachomatis (35.37 %), S. aureus (19.65 %), and S. epidermidis (10.92 %). All etiological pathogens are presented in Fig. 2. The distribution for those who replied was C. trachomatis: South America-4, Central Asia-1, North America-36, Europe-28, Far East-1, Australia-4, and Middle East-5.
S. Aureus: South America-5, Central Asia-1, North America-27, Europe-4, Africa-3, Far East-3, and Middle East-1.
S. Epidermidis: South America-1, North America-9, Europe-5, Far East-2, Central America-2, and Middle East- 3
Some did not specify where they practice.
Diagnosis
One hundred and eighty-five (65.84 %) ophthalmologists order a Gram stain routinely for each patient with ON. The distribution for those who ordered a Gram stain was South America-8, Central America-1, Central Asia-6, North America- 100, Europe-42, Africa-5, Far East-5, Australia-4, and the Middle East-11. No Gram stain performed: South America-6, Central America-1, Central Asia-6, North America-44, Europe-15, Africa-3, Far East-5, and Middle East-16. Some did not specify where they practice.
Two hundred and two (72.40 %) routinely request for antibiotic sensitivity for each patient with a positive bacterial culture. One hundred and seventy-three (61.79 %) routinely test for C. trachomatis. The distribution for those who replied was Yes: South America-4, Australia-4, Central Asia-1, North America-111, Europe-37, Far East-2, and Middle East-10; No: South America-9, Central Asia-10, North America-35, Central America-2, Europe-17, Africa-8, Far East-8, and Middle East-17
Some did not specify where they practice.
Treatment
Two hundred and forty-two (85.21 %) treat empirically when encountering ON during the first 10 days of life. All first-line treatments are summarised in Fig. 3. The distribution for those who replied was Erythromycin: South America-2, Central Asia-1, North America-64, Europe-16, Africa-, Far East-2, and the Middle East-2. Fluoroquinolones: South America-3, Central Asia-5, North America- 33, Europe-4, Africa-1, Far East-4, and the Middle East-7. Aminoglycosides: South America-2, Central Asia-2, North America-6, Australia-1, Europe-7, Africa-4, Far East-1, and the Middle East-6. Some did not specify where they practice.
Two hundred and five (75.09 %) treat empirically when they encounter ON after the first 10 days of life. All first-line empirical treatments are summarised in Fig. 4.
Two hundred and sixteen (84.71 %) prescribe topical medications in addition to systemic treatment for ON caused by N. gonorrhoeae. The distribution for those who replied was Yes: Central America-1, Australia-3, Central Asia-9, North America-110, Europe-46, Africa-7, Far East-9, and Middle East-19; No: Central America-1, North America-20, Australia-1, Europe-8, Far East-1, and Middle East-3. Some did not specify where they practice.
The topical agents used for treatment of N. gonorrhoeae include: fluoroquinolones (46.5 %), aminoglycosides (22.5 %), polymyxin B sulfate–trimethoprim solution (15.0 %), macrolides (9.6 %), chloramphenicol (5.3 %), and fucidic acid (1.1 %). The distribution for those who replied was Fluoroquinolones: South America-3, Australia-, Central Asia-5, North America-44, Europe-15, Africa-4, Far East-5, and Middle East-10, Aminoglycosides: Central America-1, South America-1, Australia-1, Central Asia-3, North America-22, Europe-9, Africa-3, Far East-1, and Middle East-1. Polymyxin B sulfate–trimethoprim solution: Central Asia-1, North America-21, Europe-4, and Middle East-2.
Macrolides: South America-3, Australia-1, North America-11, Europe-3. Chloramphenicol: Australia-1, Central Asia-, North America-1, Europe-6, Africa-1, and Middle East-1. Fucidic acid: North America-1. Some did not specify where they practice.
One hundred and eighty-four (76.67 %) prescribe systemic antibiotics for C. trachomatis.
One hundred and forty-seven (63.64 %) prescribe topical medications in addition to systemic therapy for ON caused by C. trachomatis. First-line treatments for C. trachomatis are summarised in Fig. 5.
One hundred and fifty-five (64.65 %) also routinely refer to a pediatrician to rule out pneumonitis.
The distribution for those who answered yes was South America-9, Central America-1, Central Asia-5, Australia-1, North America-84, Europe-36, Africa-2, Far East-6, and Middle East-10. No: South America-2, Australia-3, Central America-1, Central Asia-4, North America-42, Europe-12, Africa-6, Far East-5, and the Middle East-9. Some did not specify where they practice.
Prophylaxis
Two hundred and twenty-two (78.72 %) ophthalmologists replied that prophylactic treatment is required in their country, whereas 60 (21.28 %) answered that prophylactic treatment is not recommended in their country.
The distribution for those who answered was Yes: South America-14, Central Asia-7, North America-146, Central America-2, Europe-17, Africa-3, Far East-7, and the Middle East-23. No: Central Asia-4, North America-4, Europe-37, Africa-5, Australia-4, Far East-3, and Middle East-3. Some did not specify where they came from.
The most common agents used in the hospitals for ON prophylaxis are summarised in Fig. 6.
One hundred and eighty (75.31 %) ophthalmologists routinely refer parents for testing and counseling for C. trachomatis and N. gonorrhoeae.
The most common agent for each location was South America-Povidone iodone, North America-Erythromycin ointment, Europe-Povidone iodone, Africa-Tetracycline, Far East-Erythromycin ointment, Middle East-Erythromycin ointment, and Central Asia-Not specific (the use of aminoglycosides, fluoroquinolones, povidone iodone, polymyxin B sulfate–trimethoprim solution).
Discussion
Although ON is less common than in the past, it remains a blinding disease in developed countries and a significant cause of ocular morbidity, blindness, and even death in developing areas. This survey summarises the incidence, etiology, diagnosis, treatment, and prophylaxis from several regions of the world. The survey attracted good representation from North America, Europe, and the Middle East, but poorer representation from Africa, Australia, the Far East, and South America; however, this may reflect the lower number of paediatric ophthalmologists practicing in those areas.
Most ophthalmologists responding to the questionnaire were very experienced, with over 10 years of clinical practice in pediatric ophthalmology, which increases the validity of this study.
The incidence of ON reported in the literature is 1.6–12 % [1, 2]. In this survey the majority replied that they treat only 1–5 cases per year, which is a very low rate. We assume that this it is because most ophthalmologists who answered the questionnaire practice in developed countries, where this disease is less common. Another explanation could be that, in some cases, the disease is treated by pediatricians, not ophthalmologists. The actual incidence of ON is unknown, due to under-reporting in the developing world. More comprehensive studies in those countries could help determine the actual incidence of this disease.
The primary etiologies of ON in decreasing order are: chemical inflammation, bacterial infection, and viral infection [12]. The organisms causing ON are usually acquired from the infected birth canal of the mother or as an infection from the immediate surroundings [13]. Since Crédé popularized prophylaxis in the 1884, the epidemiology of ON has changed dramatically in the developed world [14]. N. gonorrheae is no longer the most common bacterial infection in ON in the developed world, but presently C. trachomatis accounts for up to 40 % of all cases of ON in North America [3, 15]. Therefore, it was not surprising to find that the most common etiology in this survey was C. trachomatis in North America, Europe, Australia, and the Middle East. But S. aureus was the common pathogen in South America and the Far East. Clinical manifestations of C. trachomatis occur after the first week of life and vary from mild hyperemia with a watery discharge to severe mucopurulent discharge and chemosis. Fortunately, complications of ocular morbidity and blindness are rare [16].
ON is essentially a clinical diagnosis. However, the differentiation between various types of infections can be difficult clinically and requires lab tests and cultures in order to determine the pathogen [17, 18]. In our study, most ophthalmologists send conjunctival scrapings for Gram staining, cultures, and test for C. trachomatis and antibiotic sensitivity; this practice is less common in the Middle East. However, until the results of the cultures are obtained, most ophthalmologists treat ON empirically with erythromycin topically or by intravenous administration or both during and after the first 10 days of life. Erythromycin is the most common antibiotic probably by virtue of its safety.
World Health Organization (WHO) treatment recommendations for ON due to C. trachomatis include oral erythromycin, while topical erythromycin is recommended as an adjunct therapy. The purpose of the systemic therapy is to decrease the risk for pneumonitis and also prevent the relapse of conjunctivitis [16, 19, 20]. Most of the ophthalmologists that replied to the questionnaire stated that they adhere to those recommendations. ON due to N. gonorrheae should include, according to WHO recommendations, hospitalization, frequent irrigation of the conjunctiva and intravenous, or intramuscular administration of ceftriaxone or penicillin [21, 22]. In all countries where paediatric ophthalmologists replied to this question this was the common practice.
Since the beginning of the twenty-first century, there has been an increasing debate regarding the necessity of prophylaxis treatment for ON. Those opposed to the treatment claim that the incidence of sexually transmitted infections has declined, treatment and awareness of ON has improved, and prophylaxis carries a risk of developing antibiotic resistance. It is reported that in Scandinavian countries, it is not common to give prophylaxis [14, 20, 23]. The ophthalmologists who support prophylactic treatment claim that current evidence supports this practice.
In our study 78.9 % of the ophthalmologists answered that prophylactic treatment is currently recommended in their country. However, we believe that the debate about prophylactic treatment will increase in coming years with the increase in resistance to antibiotics.
There are some limitations of this study. Firstly, AAPOS members do not represent all paediatric ophthalmologists; secondly, not all AAPOS members responded; and thirdly, most of the paediatric ophthalmologists were from North America, leading to a potential bias.
We speculate there will be a change in treatment and prophylaxis of the disease with the increase in resistance to antibiotics; ON is a preventable cause of childhood blindness and prophylaxis has definitely had a huge impact on infant loss of vision. At present, in our opinion, due to advanced prenatal care and treatment of sexually transmitted disease in the developed world, prophylaxis is no longer required; however, in developing countries, and in areas of deprived socioeconomic status within developed countries, prophylactic treatment of ON should still remain standard practice. It remains to be determined if the possibility that a less expensive treatment, such a povidone iodine, can replace common antibiotic treatment is yet to be established. In some countries the cost of preparation of povidone iodine is similar to that of standard antibiotics. Furthermore, some practitioners object to its colour; therefore, is it difficult to popularise. Others propose that due to its colour one can determine that the drop entered the cul de sac of the eye. Despite the facts that wide use of this preparation would render it inexpensive and, most importantly, it is not susceptible to resistance, unlike standard antibiotics.
In conclusion, we summarise the incidence, etiology, diagnosis, treatment, and prophylaxis of ON in countries where paediatric ophthalmologists are members of AAPOS. We found that the incidence of ON per year in most regions is 0–5, the most common etiology is C. trachomatis, and most infants receive prophylaxis and treatment.
References
Normann EK, Bakken O, Peltola J, Andreasson B, Buhl S, Sigg P, Nielsen K (2002) Treatment of acute neonatal bacterial conjunctivitis: a comparison of fucidic acid to chloramphenicol eye drops. Acta Ophthalmol Scand 80(2):183–187
Teoh DL, Reynolds S (2003) Diagnosis and management of pediatric conjunctivitis. Pediatr Emerg Care 19(1):48–55
Wagner RS, Aquino M (2008) Pediatric ocular inflammation. Immunol Allergy Clin N Am 28(1):169–188. doi:10.1016/j.iac.2007.12.003, vii
Zuppa AA, D’Andrea V, Catenazzi P, Scorrano A, Romagnoli C (2011) Ophthalmia neonatorum: what kind of prophylaxis? J Matern Fetal Neonatal Med 24(6):769–773. doi:10.3109/14767058.2010.531326
Woods CR (2005) Gonococcal infections in neonates and young children. Semin Pediatr Infect Dis 16(4):258–270. doi:10.1053/j.spid.2005.06.006
de Toledo AR, Chandler JW (1992) Conjunctivitis of the newborn. Infect Dis Clin N Am 6(4):807–813
Zanoni D, Isenberg SJ, Apt L (1992) A comparison of silver nitrate with erythromycin for prophylaxis against ophthalmia neonatorum. Clin Pediatr (Phila) 31(5):295–298
Nishida H, Risemberg HM (1975) Silver nitrate ophthalmic solution and chemical conjunctivities. Pediatrics 56(3):368–373
Chandler JW, Rapoza PA (1990) Ophthalmia neonatorum. Int Ophthalmol Clin 30(1):36–38
Thanathanee O, O’Brien TP (2011) Conjunctivitis: systematic approach to diagnosis and therapy. Curr Infect Dis Rep 13(2):141–148. doi:10.1007/s11908-011-0167-y
Whitley R, Arvin A, Prober C, Burchett S, Corey L, Powell D, Plotkin S, Starr S, Alford C, Connor J et al (1991) A controlled trial comparing vidarabine with acyclovir in neonatal herpes simplex virus infection. Infectious diseases collaborative antiviral study group. N Engl J Med 324(7):444–449. doi:10.1056/NEJM199102143240703
Molgaard IL, Nielsen PB, Kaern J (1984) A study of the incidence of neonatal conjunctivitis and of its bacterial causes including chlamydia trachomatis. Clinical examination, culture and cytology of tear fluid. Acta Ophthalmol (Copenh) 62(3):461–471
Mohile M, Deorari AK, Satpathy G, Sharma A, Singh M (2002) Microbiological study of neonatal conjunctivitis with special reference to chlamydia trachomatis. Indian J Ophthalmol 50(4):295–299
Schaller UC, Klauss V (2001) Is Crede’s prophylaxis for ophthalmia neonatorum still valid? Bull World Health Organ 79(3):262–263
Moore DL, MacDonald NE, Canadian Paediatric Society ID, Immunization C (2015) Preventing ophthalmia neonatorum. Paediatr Child Health 20(2):93–96
Hammerschlag MR (2011) Chlamydial and Gonococcal infections in infants and children. Clin Infect Dis 53(Suppl 3):S99–102. doi:10.1093/cid/cir699
Gigliotti F, Williams WT, Hayden FG, Hendley JO, Benjamin J, Dickens M, Gleason C, Perriello VA, Wood J (1981) Etiology of acute conjunctivitis in children. J Pediatr 98(4):531–536
Leibowitz HW, Pratt MV, Flagstad IJ, Berrospi AR, Kundsin R (1976) Human conjunctivitis. I. Diagnostic evaluation. Arch Ophthalmol 94(10):1747–1749
Hammerschlag MR, Gelling M, Roblin PM, Kutlin A, Jule JE (1998) Treatment of neonatal chlamydial conjunctivitis with azithromycin. Pediatr Infect Dis J 17(11):1049–1050
Pichichero ME (2011) Bacterial conjunctivitis in children: antibacterial treatment options in an era of increasing drug resistance. Clin Pediatr (Phila) 50(1):7–13. doi:10.1177/0009922810379045
Haase DA, Nash RA, Nsanze H, D’Costa LJ, Fransen L, Piot P, Brunham RC (1986) Single-dose Ceftriaxone therapy of Gonococcal ophthalmia neonatorum. Sex Transm Dis 13(1):53–55
Hoosen AA, Kharsany AB, Ison CA (2002) Single low-dose Ceftriaxone for the treatment of Gonococcal ophthalmia--implications for the national programme for the syndromic management of sexually transmitted diseases. S Afr Med J 92(3):238–240
Meyer D (2014) Ophthalmia neonatorum prophylaxis and the 21st century antimicrobial resistance challenge. Middle East Afr J Ophthalmol 21(3):203–204. doi:10.4103/0974-9233.134667
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
For this type of study formal consent is not required.
Additional information
Ofira Zloto and Almutez Gharaibeh contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
ON Survey- A questionnaire included 20 questions which examined the incidence of ON, etiology, diagnostic methods, treatment and prophylaxis of the disease. (DOCX 16.5 kb)
Rights and permissions
About this article
Cite this article
Zloto, O., Gharaibeh, A., Mezer, E. et al. Ophthalmia neonatorum treatment and prophylaxis: IPOSC global study. Graefes Arch Clin Exp Ophthalmol 254, 577–582 (2016). https://doi.org/10.1007/s00417-016-3274-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3274-5