Abstract
Purpose
To evaluate whether cellular migration or enlargement is the main mechanism of initial endothelial cell recovery following cataract surgery.
Methods
A prospective observational study, of 24 patients aged 50–80 years who were diagnosed with moderate cataract and received uncomplicated cataract surgery with a 2.75 mm temporal clear corneal incision, was performed in Seoul National University Bundang Hospital. Endothelial cell density (ECD) and area (ECA) were obtained in central and four paracentral (superior, inferior, nasal, and temporal) areas using non-contact specular microscopy. ECD, ECA, ECD% (ECD% = ECD in each area/the sum total of ECD in five areas), and the coefficient of variation of ECA (CV) in each location were investigated pre- and 1 day, 1 week, and 4 weeks postoperatively.
Results
ECD significantly decreased 1 day, 1 week, and 4 weeks postoperatively (p = 0.010, 0.015, and 0.003 respectively), and ECA increased (p = 0.008, 0.013, and 0.002 respectively) in only the temporal area. Postoperative ECD% decreased, and CV increased in only the temporal area significantly, when compared to preoperative values. There were no significant postoperative changes of ECD, ECA, ECD%, and CV in other areas.
Conclusions
Postoperative changes of ECD, ECA, ECD%, and CV were limited to the temporal area adjacent to the primary corneal incision. Cellular enlargement, rather than migration, may have the major effect on early endothelial cell recovery after cataract surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A lot of studies have examined the changes of endothelial cell density (ECD) in a central cornea after cataract surgery up to now [1–4]. It is widely known that damage to corneal endothelium is recovered by cellular migration and enlargement [5]. However, the mechanisms involved in endothelial recovery have not been fully determined. Recovery mechanism for corneal endothelial cell (CEC) have been studied for several decades, and most subjects of in-vivo studies about the CEC recovery mechanism following endothelial damages have been animals, including rabbit, rat, and monkey [6–9]. The human CEC recovery mechanism has been studied mostly in vitro or ex vivo because human in-vivo study is very difficult to perform [10–17]. Human in-vivo studies concerning the CEC recovery mechanism following endothelial damage have been rare. Hughes et al. showed the rise in central ECD after toxic endothelial injury, which might represent cellular migration from a less affected area [14], and Jacobi et al. provided evidence to support the hypothesis that the grafted endothelial cells migrated onto the host tissue after Descemet membrane endothelial keratoplasty [18].
To our knowledge, there has been no human in-vivo study for evaluating a main endothelial cell recovery pattern after cataract surgery. Perhaps the main recovery pattern would be cellular migration or enlargement. We hypothesized that ECD% (ECD% = ECD in each area/the sum total of ECD in central, superior, inferior, nasal, and temporal areas) would change postoperatively in all areas, if endothelial cell recovery is mainly done by cellular migration. In contrast, the change of ECD and ECD% would be localized and endothelial cell area (ECA) would be increased in the most damaged areas, if enlargement was the main contributory factor (Fig. 1). In the present study, we investigated the change of ECD, ECA, and ECD% in central and four paracentral areas after cataract surgery. Analyzing the change of ECD, ECA, and ECD% in each area may be helpful to understand a main pattern in early CEC recovery after cataract surgery.
The hypothesis about the early corneal endothelial cell recovery pattern following cataract surgery: cellular migration or enlargement. (Assumption of main ultrasonic damage in temporal paracentral area). ECD endothelial cell density, ECA endothelial cell area, C central area in endothelium, S superior paracentral area in endothelium, I inferior paracentral area in endothelium, N nasal paracentral area in endothelium, T temporal paracentral area in endothelium. CN = ECD in C; SN = ECD in S; IN = ECD in I; NN = ECD in N; TN = ECD in T. Total = CN + SN + IN + NN + TN. ECDC% = CN/Total(%); ECDS% = SN/Total(%); ECDI% = IN/Total(%); ECDN% = NN/Total(%); ECDT% = TN/Total(%)
Methods
This prospective observational study was conducted at the Seoul National University Bundang Hospital from November 2008 to April 2009. Patients aged 50 to 80 years diagnosed with moderate cataract were enrolled. Exclusion criteria were as follows: (1) previous corneal disease, corneal trauma, or intraocular surgery, (2) glaucoma or uveitis, (3) pseudoexfoliation syndrome, (4) use of contact lenses, (5) intraoperative complications (posterior capsule rupture with or without vitreous loss), and (6) diabetes mellitus. The institutional review board of Seoul National University Bundang Hospital approved the study protocol (IRB number: B-0909/083-020), and the protocol complied with the tenets of the Declaration of Helsinki. After obtaining informed consent, each patient received a standard preoperative ocular examination. Cataracts were graded according to the Lens Opacities Classification System III (LOCS III) [18]. In total, 24 eyes (13 right and 11 left) of 24 patients (nine men and 15 women) aged 68.1 ± 10.0 (SD) years (range 51 to 80 years) underwent surgery. The mean nuclear opalescence grade was 2.29 ± 0.53, and mean CDE was 7.07 ± 4.14.
Surgeries were performed using the Infiniti vision system (Alcon Laboratories, Inc., USA) by a single experienced surgeon (J.YH.). All patients received 0.5 % proparacaine hydrochloride topical anesthesia preoperatively. A 2.75-mm clear corneal incision was made on the temporal side. A side incision was made 90° clockwise to the main incision. A routine phaco-chop technique with torsional mode was used at 80 % amplitude, 400 mmHg vacuum limit, and a 40 ml/min aspiration flow rate. A single-piece hydrophobic foldable intraocular lens (SN60WF, Alcon, USA) was implanted into the capsular bag. No sutures were required on the corneal wound. Cumulative dissipated energy (CDE) was measured intraoperatively. Viscoat (3 % sodium hyaluronate and 4 % chondroitin sulfate, Alcon, US) was used as viscoelastic material.
The endothelial cell images were obtained from noncontact specular microscopy (Noncon Robo SP-8000 noncontact specular microscope, Konan, Japan) by a single experienced examiner. ECD and ECA were also calculated with the Konan computer-assisted analysis program using the center method by a same examiner [19]. As many as possible of the endothelial cells in the obtained image were counted. Before examination, it was checked that patients’ head positions were not tilted. Endothelial cells in central and four paracentral locations 3 mm away (superior, inferior, nasal, and temporal) were examined by consistently changing the microscope fixation target. Paracentral ECD measurement through changing the fixation target was built into the Robo SP-8000 machine. All specular microscopic examinations were performed between 09:00 AM and 16:00 PM.
Ciprofloxacin (Cravit®) and 0.1 % prednisolone acetate (Flarex®) were prescribed for 3 weeks postoperatively. The patients were examined with specular microscopy preoperatively and 1 day, 1 week, and 4 weeks postoperatively. ECD% was calculated by dividing ECD in each area by the sum total of ECD in central, superior, inferior, nasal, and temporal areas. ECDC%, ECDS%, ECDI%, ECDN%, and ECDT% were defined as ECD% in central, superior, inferior, nasal, and temporal paracentral areas respectively. The coefficients of variation (CV) of ECA in each area were also investigated pre- and postoperatively for analyses of corneal endothelial dysfunction and variations of ECA. The examiner was masked to the patient’s time point.
Data were analyzed using SPSS 18.0 software (SPSS Inc, Chicago, IL, USA). Comparison between each division was performed using one-way ANOVA. The postoperative changes in each division were evaluated using repeated measures ANOVA and paired t test; p < 0.05 was considered statistically significant. The significant p value limit was modified according to Bonferroni’s correction method to address problems caused by multiple comparisons.
Results
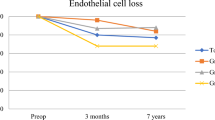
Table 1 summarizes the preoperative mean ECD and ECA. There were no significant differences of ECD and ECA in the central and four paracentral areas. ECD% was most in the superior and least in the inferior paracentral area. The sums of ECD at postoperative 1 day, 1 week, and 4 weeks were significantly decreased when compared with the preoperative value (Fig. 2). A preoperative sum of ECD was 12,854 ± 2145 cells/mm2, and postoperative 1 day, 1 week, and 4 weeks sums of ECD were 12,305 ± 1847, 12,209 ± 1858, and 11,988 ± 1812 respectively (p = 0.014, 0.001, 0.002, repeated measures ANOVA) Fig. 3 illustrated the changes of the ECD and ECA according to area postoperatively. ECD was decreased and ECA was increased significantly in only the temporal area according to time progression (ECD: p = 0.010, 0.015, 0.003; ECA: p = 0.008, 0.013, 0.002; postoperative 1 day, 1 week, and 4 weeks respectively, repeated measures ANOVA), but there were no significant changes in other area. The changes of ECD% according to area are illustrated in Fig. 4. Postoperative ECD% and CV showed significant change in only temporal area. ECDT% in postoperative 4 weeks significantly decreased (p = 0.010), but there were also no significant changes in ECDC%, ECDS%, ECDI%, and ECDN% postoperatively. CV in postoperative 1 day and 4 weeks also significantly increased in only temporal area (p = 0.003, p = 0.001), but there were no significant CV differences in other areas.
The changes of ECD (a) and ECA (b) according to area in postoperative period. Significant changes were only observed in the temporal paracentral area. Asterisk statistically significant (repeated measures ANOVA). ECD endothelial cell density, ECA endothelial cell area, Preop preoperative, Postop postoperative
The changes of ECD% (a), and coefficient of variation (CV) (b) according to area in postoperative period. Significant changes were only observed in the temporal area. Asterisk statistically significant (repeated measures ANOVA). ECD% = the proportion of ECD in each area to the sum total of ECD in central, superior, inferior, nasal, and temporal paracentral areas. Total = the sum total of ECD in central, superior, inferior, nasal, and temporal paracentral areas. ECDC% = CN/Total(%); ECDS% = SN/Total(%); ECDI% = IN/Total(%); ECDN% = NN/Total(%); ECDT% = TN/Total(%). Preop preoperative, Postop postoperative
Discussion
The purpose of this study was to investigate which of cellular migration or enlargement have the major effect on early CEC recovery after cataract surgery, using analysis of ECD, ECA, ECD%, and CV changes in central and four paracentral areas. Postoperative ECD, ECD% decreased and ECA and CV increased in only the temporal area, when compared to preoperative values. There were no significant changes in other areas. These results well coincided with our hypothesis (Fig. 1) about cellular enlargement from neighboring cells, and suggest that cellular enlargement may have the major effect on early CEC recovery after cataract surgery.
Once the endothelial single layer has formed, the endothelial cells do not normally replicate in vivo at a rate sufficient to replace dead or injured cells [19]. This relative lack of cell division results in a gradual decrease in ECD throughout life [19]. Several studies have reported endothelial cell damage after cataract extraction [14, 20–30]. It has been thought that endothelial damage following cataract surgery in humans would be recovered by migration or enlargement. To our knowledge, there has been no study to investigatewhich mechanism (cellular migration or enlargement) has the major effect on early CEC recovery after cataract surgery in humans. A lot of results from animal in-vivo studies and human in-vitro studies seem to have made people think that cellular migration or enlargement can be taken for granted as recovery patterns after cataract surgery in humans [6–16]. Because it is uncertain which of migration or enlargement have the major effect on early CEC recovery after cataract surgery in humans, this study could be meaningful as a human in-vivo study.
We observed a significant decrease in ECD and increase in ECA after surgery only in the temporal paracentral area, contrary to the expectation that central endothelial cell damage would happen mainly because the center is main site of phacoemulsification damage. These findings seem to be related with endothelial wound by temporal clear corneal incision and the in-and-out movement of surgical instruments through main incision. The result showed no statistically significant postoperative ECD decrease in the center. This can be attributed to the low CDE value used compared to the previous torsional phacoemulsification studies [2, 3, 30–32]. We enrolled patients with moderate cataracts, and the surgery was performed with the phaco-chop technique using dispersive OVD to minimize CDE and endotheilal cell damage. Instead, the sum total of ECD in five areas was significantly decreased postoperatively, and this is similar to the endothelial changes following cataract surgery found in several studies [2, 8, 20, 22, 27, 28, 33–36].
Ling et al. showed that central ECD had decreased by 25 % and CV had increased by 60 % at 4 weeks after wounding in cat eyes, but central ECD had been recovered at 18 months after wounding [37]. Huang et al. also showed that ECA and CV were significantly increased at 6 weeks after damaging cat eyes [38]. These findings correspond with our results, and support the supposition that enlargement may be a major factor in early CEC recovery. Though several in-vitro studies have revealed molecular biologic findings in corneal endothelial cell migration [13, 39–41], this does not mean that migration is a main pattern in early CEC recovery. Instead, cellular migration seems to act on CEC recovery in the long term.
Recently, a renewal zone, in the periphery of the human corneal endothelium, where endothelial cells divided very slowly and migrated toward the center but probably showed fragility, was introduced [42]. The study suggested the existence of endothelial stem cells or transient amplifying cells similar to limbal epithelial stem cells. On the basis of this finding, our results may reflect that corneal endothelial stem cells were damaged by temporal corneal incision and repetitive phaco-tip movement, which may consequently hinder endothelial cell migration from the periphery to the temporal paracentral area, and cellular enlargement may thus have the major effect on CEC recovery.
There are several notable limitations of the present study. The sample size is small, and the follow-up period is short. Our results cannot be considered direct evidence about cellular enlargement in the early CEC recovery, and may be limited in the moderate cataract and phaco-chop technique. Fluid turnover and the direction of the infusion flow were not considered. Intraobserver variability also could affect our results. However, preoperative variability was maximally controlled by using the same machine and by a single experienced surgeon and examiner. Because the estimate for the repeatability of specular microscopy was reported to be about ±8.2 % [29], and temporal ECD change in our study exceeded this range (more than 10 %, data not shown); the results in this study do not appear to show intraobserver variability. All patients’ data had a normal distribution, which also ensured that postoperative ECD changes were meaningful. The majority of endothelial repair occurs within 1 month after cataract surgery [43]; therefore, the short follow-up period is unlikely to be a critical limitation.
In conclusion, the postoperative change of ECD, ECD%, ECA, and CV after cataract surgery is limited to the temporal area only, adjacent to the main corneal incision. This revealed that cellular enlargement may have the major effect on early CEC recovery after cataract surgery.
References
Vajpayee RB, Kumar A, Dada T, Titiyal JS, Sharma N, Dada VK (2000) Phaco-chop versus stop-and-chop nucleotomy for phacoemulsification. J Cataract Refract Surg 26:1638–1641
Liu Y, Zeng M, Liu X, Luo L, Yuan Z, Xia Y, Zeng Y (2007) Torsional mode versus conventional ultrasound mode phacoemulsification: randomized comparative clinical study. J Cataract Refract Surg 33:287–292
Zeng M, Liu X, Liu Y, Xia Y, Luo L, Yuan Z, Zeng Y (2008) Torsional ultrasound modality for hard nucleus phacoemulsification cataract extraction. Br J Ophthalmol 92:1092–1096
Storr-Paulsen A, Norregaard JC, Ahmed S, Storr-Paulsen T, Pedersen TH (2008) Endothelial cell damage after cataract surgery: divide-and-conquer versus phaco-chop technique. J Cataract Refract Surg 34:996–1000
Krachmer JH, Mannis MJ, Holland EJ (2010) Cornea. In: Nishida T, Saika S (eds) Cornea and sclera — anatomy and physiology, 3rd edn. Elsevier Mosby, Philadelphia, pp 4–24
Ichijima H, Petroll WM, Jester JV, Barry PA, Andrews PM, Dai M, Cavanagh HD (1993) In vivo confocal microscopic studies of endothelial wound healing in rabbit cornea. Cornea 12:369–378
Tuft SJ, Williams KA, Coster DJ (1986) Endothelial repair in the rat cornea. Invest Ophthalmol Vis Sci 27:1199–1204
Matsuda M, Sawa M, Edelhauser HF, Bartels SP, Neufeld AH, Kenyon KR (1985) Cellular migration and morphology in corneal endothelial wound repair. Invest Ophthalmol Vis Sci 26:443–449
Matsubara M, Tanishima T (1982) Wound-healing of the corneal endothelium in the monkey: a morphometric study. Jpn J Ophthalmol 26:264–273
Yamaguchi M, Ebihara N, Shima N, Kimoto M, Funaki T, Yokoo S, Murakami A, Yamagami S (2011) Adhesion, migration, and proliferation of cultured human corneal endothelial cells by laminin-5. Invest Ophthalmol Vis Sci 52:679–684
Nakahara M, Okumura N, Kay EP, Hagiya M, Imagawa K, Hosoda Y, Kinoshita S, Koizumi N (2013) Corneal endothelial expansion promoted by human bone marrow mesenchymal stem cell-derived conditioned medium. PLoS One 8, e69009
Patel SV, Bachman LA, Hann CR, Bahler CK, Fautsch MP (2009) Human corneal endothelial cell transplantation in a human ex vivo model. Invest Ophthalmol Vis Sci 50:2123–2131
Joko T, Shiraishi A, Akune Y, Tokumaru S, Kobayashi T, Miyata K, Ohashi Y (2013) Involvement of P38MAPK in human corneal endothelial cell migration induced by TGF-beta(2). Exp Eye Res 108:23–32
Hughes EH, Pretorius M, Eleftheriadis H, Liu CS (2007) Long-term recovery of the human corneal endothelium after toxic injury by benzalkonium chloride. Br J Ophthalmol 91:1460–1463
Schilling-Schon A, Pleyer U, Hartmann C, Rieck PW (2000) The role of endogenous growth factors to support corneal endothelial migration after wounding in vitro. Exp Eye Res 71:583–589
Regis-Pacheco LF, Binder PS (2014) What happens to the corneal transplant endothelium after penetrating keratoplasty? Cornea 33:587–596
Jacobi C, Zhivov A, Korbmacher J, Falke K, Guthoff R, Schlötzer-Schrehardt U, Cursiefen C, Kruse FE (2011) Evidence of endothelial cell migration after Descemet membrane endothelial keratoplasty. Am J Ophthalmol 152:537–542
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY (1993) The lens opacities classification system III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 111:831–836
Joyce NC (2005) Cell cycle status in human corneal endothelium. Exp Eye Res 81:629–638
Bourne WM, McLaren JW (2004) Clinical responses of the corneal endothelium. Exp Eye Res 78:561–572
Dick HB, Kohnen T, Jacobi FK, Jacobi KW (1996) Long-term endothelial cell loss following phacoemulsification through a temporal clear corneal incision. J Cataract Refract Surg 22:63–71
Diaz-Valle D, del Castillo B, Sanchez JM, Castillo A, Sayagues O, Moriche M (1998) Endothelial damage with cataract surgery techniques. J Cataract Refract Surg 24:951–955
Walkow T, Anders N, Klebe S (2000) Endothelial cell loss after phacoemulsification: relation to preoperative and intraoperative parameters. J Cataract Refract Surg 26:727–732
Beltrame G, Salvetat ML, Driussi G, Chizzolini M (2002) Effect of incision size and site on corneal endothelial changes in cataract surgery. J Cataract Refract Surg 28:118–125
Inoue K, Tokuda Y, Inoue Y, Amano S, Oshika T, Inoue J (2002) Corneal endothelial cell morphology in patients undergoing cataract surgery. Cornea 21:360–363
Ravalico G, Botteri E, Baccara F (2003) Long-term endothelial changes after implantation of anterior chamber intraocular lenses in cataract surgery. J Cataract Refract Surg 29:1918–1923
Bourne RR, Minassian DC, Dart JK, Rosen P, Kaushal S, Wingate N (2004) Effect of cataract surgery on the corneal endothelium: modern phacoemulsification compared with extracapsular cataract surgery. Ophthalmology 111:679–685
Lee JS, Lee JE, Choi HY, Oum BS, Cho BM (2005) Corneal endothelial cell change after phacoemulsification relative to the severity of diabetic retinopathy. J Cataract Refract Surg 31:742–749
McCarey BE, Edelhauser HF, Lynn MJ (2008) Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures, surgical devices and new intraocular drugs and solutions. Cornea 27:1–16
Gonen T, Sever O, Horozoglu F, Yasar M, Keskinbora KH (2012) Endothelial cell loss: biaxial small-incision torsional phacoemulsification versus biaxial small-incision longitudinal phacoemulsification. J Cataract Refract Surg 38:1918–1924
Vasavada AR, Vasavada V, Vasavada VA, Praveen MR, Johar SR, Gajjar D, Arora AI (2012) Comparison of the effect of torsional and microburst longitudinal ultrasound on clear corneal incisions during phacoemulsification. J Cataract Refract Surg 38:833–839
Assaf A, Roshdy MM (2013) Comparative analysis of corneal morphological changes after transversal and torsional phacoemulsification through 2.2 mm corneal incision. Clin Ophthalmol 7:55–61
Schultz RO, Glasser DB, Matsuda M, Yee RW, Edelhauser HF (1986) Response of the corneal endothelium to cataract surgery. Arch Ophthalmol 104:1164–1169
Werblin TP (1993) Long-term endothelial cell loss following phacoemulsification: model for evaluating endothelial damage after intraocular surgery. Refract Corneal Surg 9:29–35
Dick B, Kohnen T, Jacobi KW (1995) Endothelial cell loss after phacoemulsification and 3.5 vs. 5 mm corneal tunnel incision. Ophthalmologe 92:476–483
Mathys KC, Cohen KL, Armstrong BD (2007) Determining factors for corneal endothelial cell loss by using bimanual microincision phacoemulsification and power modulation. Cornea 26:1049–1055
Ling T, Vannas A, Holden B (1988) Long-term changes in corneal endothelial morphology following wounding in the cat. Invest Ophthalmol Vis Sci 29:1407–1412
Huang P, Nelson L, Bourne W (1989) The morphology and function of healing cat corneal endothelium. Invest Ophthalmol Vis Sci 30:1794–1801
Treffers WF (1982) Human corneal endothelial wound repair. In vitro and in vivo. Ophthalmology 89:605–613
Rieck PW, Cholidis S, Hartmann C (2001) Intracellular signaling pathway of FGF-2-modulated corneal endothelial cell migration during wound healing in vitro. Exp Eye Res 73:639–650
Lee JG, Kay EP (2006) FGF-2-induced wound healing in corneal endothelial cells requires Cdc42 activation and Rho inactivation through the phosphatidylinositol 3-kinase pathway. Invest Ophthalmol Vis Sci 47:1376–1386
He Z, Campolmi N, Gain P, Ha Thi BM, Dumollard JM, Duband S, Peoc’h M, Piselli S, Garraud O, Thuret G (2012) Revisited microanatomy of the corneal endothelial periphery: new evidence for continuous centripetal migration of endothelial cells in humans. Stem Cells 30:2523–2534
Price N, Jacobs P, Cheng H (1982) Rate of endothelial cell loss in the early postoperative period after cataract surgery. Br J Ophthalmol 66:709–713
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, DH., Wee, W.R. & Hyon, J.Y. The pattern of early corneal endothelial cell recovery following cataract surgery: cellular migration or enlargement?. Graefes Arch Clin Exp Ophthalmol 253, 2211–2216 (2015). https://doi.org/10.1007/s00417-015-3100-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3100-5